ABSTRACT
The purpose of this case report was to describe a technique to modify the free gingival graft by perforations within the graft to guarantee a horizontal increase in the keratinized mucosa in the anteroinferior sector of a total edentulous mandible after osseointegration of previously placed dental implants in a hybrid prosthesis protocol. A 71-year-old male underwent free modified gingival graft surgery with perforations at the level of each implant. At 3 months, the mucosa appeared to be healthy and keratinized, especially at a horizontal level around the implants previously diagnosed with mucositis, providing the patient with satisfactory results. Finally, the hybrid prosthesis was cleaned and polished due to the presentation of a hard plate at the level of the abutments. Within the limitations of this case report, further research is needed to evaluate the long-term efficacy of this modification to the free gingival graft.
KEYWORDS: Free gingival graft, mucositis, punch technique
INTRODUCTION
The traditional morphology presented by the oral mucosa in relation to shape, color, and size plays a fundamental role in human biology, with these characteristics having an impact on the aesthetics of each patient. For example, gingival recession can lead to hypersensitivity, pain, and loss of teeth, among others.[1]
Therefore, it is important for peri-implant mucosa to be wide, thick, and well keratinized for the maintenance of the tissue surrounding a dental implant. Several techniques have been described to increase the amount of keratinized tissue, such as connective tissue graft and free epithelial graft, among others.[2]
Constructive techniques can improve oral mucosal tissue defects, and are, therefore, generally indicated before dental implant treatment as part of surgical and prosthetic planning. Preserving the architecture of dental implants is challenging, especially when the anatomical conditions of the patient limit correct rehabilitation of the implants placed.[3,4,5] All these techniques seek to maintain and preserve peri-implantar health,[5] especially in multiple prostheses retained on implants in total edentulous patients. However, the implants placed are not always successful and some fail when bacterial plaque causes microbial contamination, leading to mucositis or peri-implantitis and implant failure due to bone loss, inflammation, or exudate along the implant bone interface.[6,7,8,9,10]
Total edentulous patients who have a very extensive resorption of the jaws are generally candidates for rehabilitation with a hybrid prosthesis supported by dental implants, because it is a complete fixed prosthesis made of acrylic resin that is supported on dental implants. It returns the aesthetic, chewing, phonetic function, and provides lip support successfully.[3,4,5]
The objective of this case report was to present the management of peri-implant mucositis of multiple osseointegrated implants using a modified free gingival graft “punch technique” in a total edentulous area.
CASE REPORT
A 71-year-old man with a medical history of diabetes and controlled arterial hypertension, who attended the postgraduate department of the Universidad Peruana Cayetano Heredia, Lima, Peru, was treated. The patient was completely edentulous and wished to have a fixed prosthesis to eat properly. During the periodontal clinical evaluation, the patient was classified as Seibert Type II, presenting poor condition of upper and lower total prostheses due to atrophy in both jaws. The gingiva keratinized was horizontally inadequately attached <4 mm over the entire lower jaw with low-insertion mucosa [Figure 1].
Figure 1.
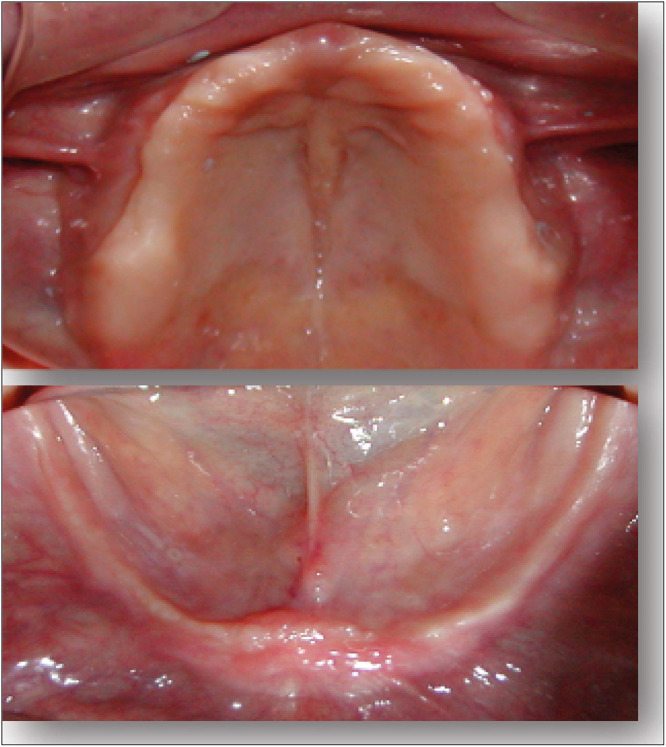
Edentulous ridges before implant placement
Previously, the patient was treated with a new conventional total prosthesis in only the upper jaw, whereas a hybrid prosthesis was planned in the lower jaw with the Branemark protocol of 5 implants [Figure 2]. The implants were conical, with textured internal connection (Implant AR Conexão, São Paulo, Brazil) of 4 × 15 mm at the teeth 31 and 33, and 4 × 13 mm at teeth 34, 42, and 44. This type of implant contains conventional TiGr4 titanium, and therefore, a double thread with an active apex and internal hexagon is indicated for multiple prostheses. All the implants were placed with a torque >40 N·cm [Figure 3]. According to the manufacturer's instructions, a conventional drilling technique was used and a control radiograph was taken [Figure 4].
Figure 2.
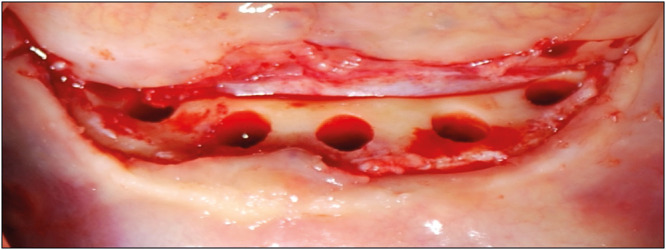
Crestal level flap and preparation for surgical drilling
Figure 3.

Placement of the five dental implants with their respective closing caps
Figure 4.
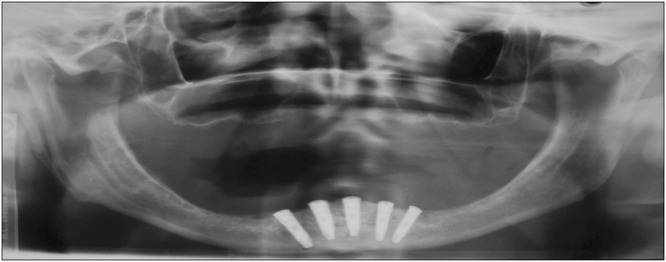
Panoramic control radiograph to observe the equidistance of the implants according to the Branemark protocol
After a 6-month osseointegration period, 3-mm cuff healing was placed, and 1 week later, 3-mm cuff microunit multiple code abutments (Code 136073) were placed at a torque of 20 N·cm, and the lower hybrid prosthesis was installed. It was performed through the second phase surgery where the connection of the dental implants was exposed, for which a full-thickness supracrestal flap was performed to place the transepithelial healing. Where, the local anesthesia was previously placed, and finally it was sutured with a simple technique with 3/0 Caliber Black Silk.
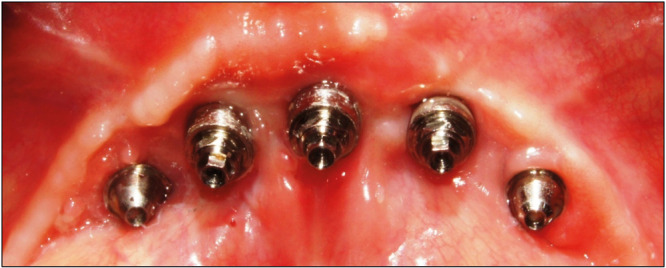
After approximately 8 months, the patient returned for follow-up maintenance, and clinical examination showed an inflammatory process around the implants. The hybrid prosthesis was removed, and generalized peri-implant mucositis was diagnosed [Figure 5].
Figure 5.
Diagnosis of peri-implant mucositis
On evaluation of the mucositis, a lack of hygiene was determined due to the pain caused by the absence of keratinized tissue. Therefore, a modified free gingival graft was planned [Figure 6] using the punch technique.[9] Perforations were made in the free gingival graft with the intention of guaranteeing a better adaptation of the graft on each one of the prosthetic abutments, and thus gaining keratinized gum. It was decided to obtain the palatal graft with dimensions of 24 × 8 × 3 mm (length/width/thickness) [Figure 7]. After compliance with the antisepsis protocol, the patient was anesthetized with 2% lidocaine, 1:100,000 (ATC class: n01bb02, Lima, Peru). A horizontal incision was made with 15C scalpel blade at the level of the bone crest of the area to be treated approximately 20 mm from the most distal implants on each side to its counterpart, and then a flap was made with Prichard type curettage (Hu-Friedy, Chicago, IL, USA).
Figure 6.
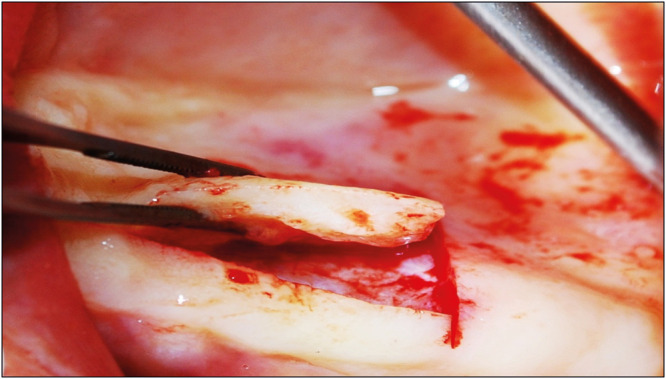
Obtaining the free epithelial graft from the palatal area
Figure 7.
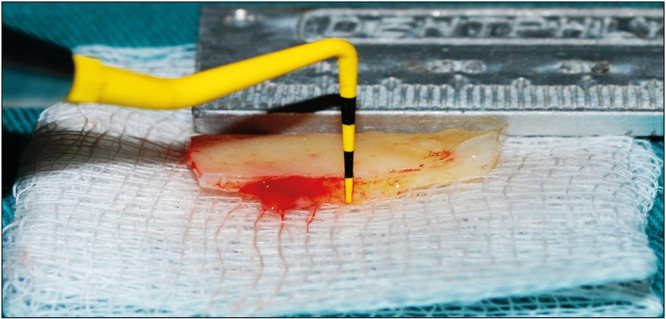
Free epithelial graft before placement in the recipient area
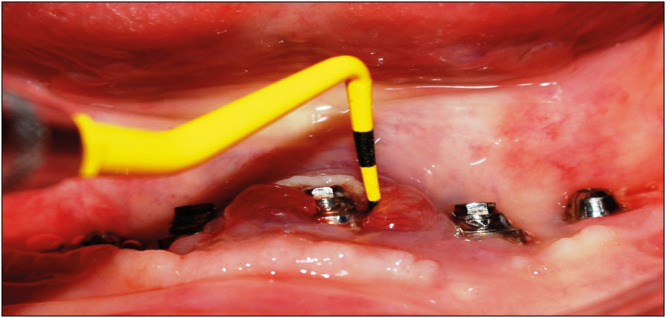
To place the free gingival graft previously removed from the donor area of the palate, holes were made on the graft using a 5-mm diameter trephine-type milling cutter [Figure 8]. The graft was then placed in the compromised implants and sutured using simple technique (Glicosorb polyglycolic acid) [Figure 9]. Compression was performed with sterile gauze moistened with saline solution to stabilize the surrounding tissues. A palatal plate was made to protect the donor area and provide patient comfort. Finally, the patient was medicated with chlorhexidine antiseptic mouthwash, an anxiolytic (Alpaz 0.25 mg, Xanax), and clindamycin 300 mg/8 h for 6 days, etoricoxib (Arcoxia) 120 mg/day for 5 days, and diclofenac sodium (Voltaren) 75 mg intramuscular injection for 1 day. The sutures were removed at 15 days, and the patient was periodically monitored [Figure 10]. After more than 6 months, a notable increase in keratinized tissue was evident around the implants that had previously presented mucositis. The hybrid prosthesis was then installed after polishing and cleaning the metal and acrylic structure to guarantee correct hygiene and maintenance of the peri-implant tissues [Figure 11].
Figure 8.
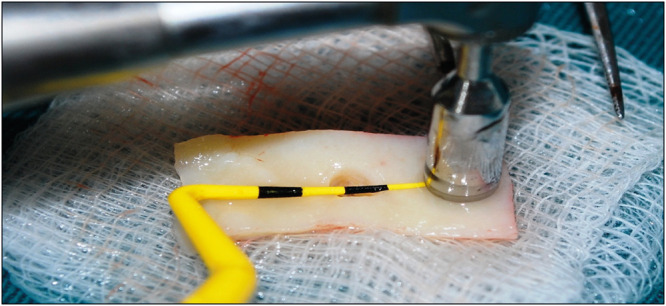
Perforation of the graft with the circular drill “punch technique”
Figure 9.
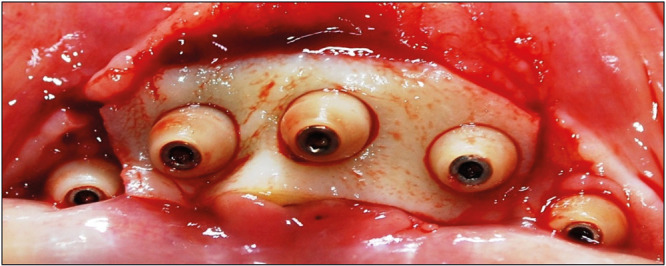
Insertion of the free epithelial graft in the recipient area to obtain sufficient quantity of keratinized gingiva
Figure 10.
Control of the grafted area showing significant gain of keratinized gum
Figure 11.

Control of the hybrid prosthesis in the maintenance phase showing peri-implant health at 6 months
DISCUSSION
The concept of a flapless surgical approach was introduced in the 1970s. This procedure uses a circular tissue punch to obtain a circumferential incision, to use this tissue in the grafts to be performed or at the implant site without any elevation of the surgical flap. In the flapless implant surgery approach, it is also important to enter the bone with a circular drill. This surgical technique has certain advantages such as tissue preservation, minimization of surgical trauma, and maintenance of soft tissue emergence profiles, although it can often reduce the width of keratinized tissue as the circular bur must reduce the space required.[11,12]
Taking into account the low quantity of keratinized gingiva at the level of future dental implants, corrective surgery using a free gingival graft modified by the “punch technique” was planned to obtain an increase in the horizontal keratinized gingiva after hybridization of the prosthesis on the implants. The clinical results obtained in this case report show the development of a keratinized epithelium around dental implants. Furthermore, radiographic analysis showed a preserved alveolar bone ridge without any peri-implant reabsorption process. This is especially important in cases affected by an inflammatory process. Currently, there is a controversy regarding the influence of keratinized gums on peri-implant health. Some studies have reported that optimal oral hygiene conditions of the marginal gum surrounding the implants are needed, although similar results have been reported when the attached gum was inadequate. On the contrary, other studies have reported an association between implant survival and the width of the keratinized gum,[13,14,15] similar to the results obtained in this case report and other studies. Healthy tissue is essential to preserve the aesthetics and chewing function around dental implants. In addition, gingival recessions can be prevented by avoiding exposing the threads of the implants as this usually provides a tight collar at the periphery of the implants, thereby preventing the development of mucositis or peri-implantitis.[9,15,16,17]
However, a free epithelial graft can often cause certain discomfort such as pain, second surgical wound in the donor area, inconsistent color, and some shrinkage of the surrounding texture, which can result in unsightly results.[18,19] Other studies have also shown that adequate width and length of the keratinized mucosa is very important to guarantee peri-implant health as it reduces the possibility of accumulating bacterial plaque, inflammation, recession, and gingival bleeding. Furthermore, sufficient vertical and horizontal thickness of the mucous tissue is essential for correct passive seating of the prostheses on the implants, to thereby prevent resorption at the level of the bone crest and provide a favorable environment for single and multiple prostheses.[18,19,20,21]
Finally, some limitations of this case report were that comparison of our results is difficult because there are few studies showing the effectiveness of free epithelial grafts with perforations using the punch technique. Although this technique has shown promising results, clinical studies with greater scientific rigor are needed to evaluate the benefits of this modified technique.
CONCLUSION
This case report shows that it is favorable to recover tissues surrounding the peri-implant space, thus optimizing the stability of the implants. Nonetheless, within the limitations of this case report, further studies on this modified surgical technique are needed to show its effectiveness and benefits for making adequate clinical decisions.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
AUTHOR CONTRIBUTIONS
Study conception was by FMT and JR; data collection by FMT and DAT; data acquisition and analysis by FMT, and JR; data interpretation by JR, SL, CMV, FM, and FMT, and manuscript writing by FMT, SL, FM, CMV, and DAT.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
Patients attended in the postgraduate service signed an informed consent before beginning any type of surgical or prosthetic treatment. The study respects the rights of the patient. The Declaration of Helsinki was followed.
PATIENT DECLARATION OF CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
DATA AVAILABILITY STATEMENT
The data or photos that support the study results are available from the author (Dr. Frank Mayta-Tovalino, e-mail: fmaytat@ucientifica.edu.pe) on request.
ACKNOWLEDGEMENTS
The authors wish to thank the Universidad Cientifica del Sur for all their unconditional support for preparing this case report.
REFERENCES
- 1.Menceva Z, Dimitrovski O, Popovska M, Spasovski S, Spirov V, Petrushevska G. Free gingival graft versus mucograft: Histological evaluation. Open Access Maced J Med Sci. 2018;6:675–9. doi: 10.3889/oamjms.2018.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nemcovsky CE, Artzi Z. Split palatal flap. II. A surgical approach for maxillary implant uncovering in cases with reduced keratinized tissue: Technique and clinical results. Int J Periodontics Restorative Dent. 1999;19:385–93. [PubMed] [Google Scholar]
- 3.Karaca Ç, Er N, Gülşahı A, Köseoğlu OT. Alveolar ridge preservation with a free gingival graft in the anterior maxilla: Volumetric evaluation in a randomized clinical trial. Int J Oral Maxillofac Surg. 2015;44:774–80. doi: 10.1016/j.ijom.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Azar DE. Dental implant uncovering techniques with emphasis on increasing keratinized mucosa. Compend Contin Educ Dent. 2015;36:290–2, 294, 296-7. [PubMed] [Google Scholar]
- 5.Kissa J, El Kholti W, Laalou Y, El Farouki M. Augmentation of keratinized gingiva around dental implants. J Stomatol Oral Maxillofac Surg. 2017;118:156–60. doi: 10.1016/j.jormas.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Stimmelmayr M, Stangl M, Edelhoff D, Beuer F. Clinical prospective study of a modified technique to extend the keratinized gingiva around implants in combination with ridge augmentation: One-year results. Int J Oral Maxillofac Implants. 2011;26:1094–101. [PubMed] [Google Scholar]
- 7.Adibrad M, Shahabuei M, Sahabi M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantol. 2009;35:232–7. doi: 10.1563/AAID-JOI-D-09-00035.1. [DOI] [PubMed] [Google Scholar]
- 8.Andreasi Bassi M, Andrisani C, Lopez MA, Gaudio RM, Lombardo L, Lauritano D. Modified connective tissue punch technique to increase the vestibular/buccal keratinized tissue on flapless implant surgery: A case series. J Biol Regul Homeost Agents. 2016;30:29–34. [PubMed] [Google Scholar]
- 9.Meijer HA, Batenburg HK, Raghoebar GM, Vissink A. Mandibular overdentures supported by two Branemark, IMZ or ITI implants: A 5-year prospective study. J Clin Periodontol. 2004;31:522–6. doi: 10.1111/j.1600-051X.2004.00510.x. [DOI] [PubMed] [Google Scholar]
- 10.Meijer HJ, Geertman ME, Raghoebar GM, Kwakman JM. Implant-retained mandibular overdentures: 6-year results of a multicenter clinical trial on 3 different implant systems. J Oral Maxillofac Surg. 2001;59:1260–8; 1269-70. doi: 10.1053/joms.2001.27512. [DOI] [PubMed] [Google Scholar]
- 11.Sclar AG. Guidelines for flapless surgery. J Oral Maxillofac Surg. 2007;65(7 Suppl 1):20–32. doi: 10.1016/j.joms.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Bayounis AM, Alzoman HA, Jansen JA, Babay N. Healing of peri-implant tissues after flapless and flapped implant installation. J Clin Periodontol. 2011;38:754–61. doi: 10.1111/j.1600-051X.2011.01735.x. [DOI] [PubMed] [Google Scholar]
- 13.Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995;6:131–8. doi: 10.1034/j.1600-0501.1995.060301.x. [DOI] [PubMed] [Google Scholar]
- 14.Chung DM, Oh TJ, Shotwell JL, Misch CE, Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77:1410–20. doi: 10.1902/jop.2006.050393. [DOI] [PubMed] [Google Scholar]
- 15.Bouri A, Jr, Bissada N, Al-Zahrani MS, Faddoul F, Nouneh I. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. 2008;23:323–6. [PubMed] [Google Scholar]
- 16.Marin DO, Leite AR, Nícoli LG, Marcantonio C, Compagnoni MA, Marcantonio E., Jr Free gingival graft to increase keratinized mucosa after placing of mandibular fixed implant-supported prosthesis. Case Rep Dent. 2017;2017:5796768. doi: 10.1155/2017/5796768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20:1170–7. doi: 10.1111/j.1600-0501.2009.01795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh SL, Masri RM, Williams DA, Ji C, Romberg E. Free gingival grafts for implants exhibiting lack of keratinized mucosa: A prospective controlled randomized clinical study. J Clin Periodontol. 2017;44:195–203. doi: 10.1111/jcpe.12660. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal C, Tarun Kumar AB, Mehta DS. Comparative evaluation of free gingival graft and alloderm(®) in enhancing the width of attached gingival: A clinical study. Contemp Clin Dent. 2015;6:483–8. doi: 10.4103/0976-237X.169838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mendoza-Azpur G, Gallo P, Mayta-Tovalino F, Alva R, Valdivia E. A case series of vertical ridge augmentation using a nonresorbable membrane: A multicenter study. Int J Periodontics Restorative Dent. 2018;38:811–6. doi: 10.11607/prd.3538. [DOI] [PubMed] [Google Scholar]
- 21.Imano MH, Cunha EJ, Storrer CLM, Deliberador TM. A modified free gingival graft technique for gaining vertical and horizontal soft tissue augmentation. J Indian Soc Periodontol. 2019;23:77–80. doi: 10.4103/jisp.jisp_156_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data or photos that support the study results are available from the author (Dr. Frank Mayta-Tovalino, e-mail: fmaytat@ucientifica.edu.pe) on request.


