Abstract
Introduction:
Vitamin C deficiency has been described in patients with sepsis. The post-cardiac arrest syndrome shares similarities to sepsis, however vitamin C levels in post-arrest patients have been incompletely characterized. We assessed vitamin C levels in a post-arrest population.
Methods:
This was a retrospective observational study at a tertiary care center. A convenience sample of post-arrest, sepsis, and healthy control patients was selected from prior studies. Vitamin C levels were measured from samples obtained within 6-hours of emergency department admission. A subset of cardiac arrest patients had vitamin C levels additionally measured at 24-hours later.
Results:
A total of 84 patients (34 healthy controls, 25 post-arrest, and 25 septic patients) were included. The median baseline vitamin C level in cardiac arrest patients was 0.33 mg/dL (0.05–0.83), as compared to 0.91mg/dL (0.69–1.48) in the healthy control group (p<0.01) and 0.28 mg/dL (0.11–0.59) in the septic group (p=0.36). Vitamin C levels for cardiac arrest patients fell between the two time points, but the change was not statistically significant (median decrease 0.26 mg/dL, p=0.08).
Conclusions:
Serum vitamin C levels were lower in post-arrest patients compared to controls and were similar to patients with sepsis. Future studies of vitamin C levels and supplementation following cardiac arrest may be warranted.
Keywords: Cardiac Arrest, Vitamin C, Ascorbic Acid, Sepsis, Out of Hospital, Post-cardiac arrest
Introduction:
Vitamin C has several functions. In addition to serving as an anti-oxidant and co-factor in catecholamine synthesis, it also has anti-inflammatory and immune-modulating properties.1,2 Vitamin C deficiency has been described in sepsis.3–5 and there is evidence that supplementation may help attenuate organ injury and improve mortality in sepsis victims.6–9
The post-cardiac arrest syndrome is characterized by brain injury, myocardial dysfunction, and systemic ischemia-reperfusion injury. The post-arrest systemic pathophysiologic cascade shares several features in common with sepsis such as mitochondrial dysfunction, generalized activation of coagulation and immunologic pathways, with resultant multi-organ failure and high rates of morbidity.10,11 To date, there has been a paucity of studies exploring vitamin C levels in post-arrest populations.
In this study we hypothesized that post-arrest patients would have significantly lower vitamin C levels than healthy controls and similar levels to septic patients.
Methods:
Study Design
This was a single center, retrospective, observational study performed at an academic tertiary care center. Vitamin C levels were measured in stored blood samples collected during two previously completed, multicenter prospective studies. The original studies, including blood collection and analysis plans, were approved by the Beth Israel Deaconess Medical Center Committee on Clinical Investigation (CCI)a.
Data Collection
Blood samples from cardiac arrest victims were collected during the Characterization of Mitochondrial Injury in Cardiac Arrest (COMICA) study.12 Sepsis samples were obtained from the Randomized Control Trial of Calcitriol in Sepsis.13 Control blood samples were obtained from healthy volunteers. Patients were included in the present sub-study if sufficient stored blood sample was available. Post-arrest samples were taken with 6-hours of return-of-spontaneous circulation (ROSC) and sepsis samples were taken within 6 hours of trial enrollment. All cardiac arrests occurred out-of-hospital. Twelve of the 25 post-arrest patients also had blood available from a time-point 24-hours after enrollment. All blood samples were centrifuged to remove cellular elements and then serum was stored frozen at −80°C. For complete details of the original study designs, blood collection protocols, cohort characteristics, and results please see the published manuscripts.12,13
Measurement of Vitamin C Levels
Vitamin C levels were measured using the Abcam ascorbic acid assay. In this assay, ascorbate oxidase was added to parallel samples. This removes any ascorbate present in the sample and leaves a background value which is subtracted from the total value to calculate the ascorbate concentration of the sample. The detection limit for this assay is 0.035 to 3.52 mg/dL of ascorbic acid. To ensure measurement accuracy, all samples were measured at least in duplicates of sample and sample background. Measures closest in value were averaged.
Statistical Analysis
Vitamin C levels were expressed as median (IQR) in milligrams/deciliter (mg/dL). Median vitamin C levels were compared between the 3 groups using the Kruskall-Wallis test with pairwise comparisons done via Mann-Whitney U test. Changes in vitamin C levels between time points in the post-cardiac arrest patients were compared using the Wilcoxon signed-rank test. A p-value < 0.05 was used to determine statistical significance. Data analysis was performed using STATA, version IC15. (College Station, Texas, StataCorp LP, United States)
Results:
Cohort Characteristics
There were 84 patients who had serum samples available for testing. Of these, 34 were healthy controls, 25 were post-cardiac arrest patients, and 25 were septic patients. Demographic data, comorbidities, the worst serum lactate over the first 24-hours after enrollment, and in-hospitality mortality for these patients can be found in Table 1.
Table I:
Demographics, co-morbidities, worst lactate, and in-hospital mortality for each of the 3 groups
| Healthy Control | Cardiac Arrest | Sepsis | |
|---|---|---|---|
| N (sample size) | 34 | 25 | 25 |
| Age (median, IQR) | 28.0 (25.5–33.5) | 68.0 (57.0–75.0) | 64.0 (56.0–71.0) |
| Gender (% female) | 76.5 | 40.0 | 40.0 |
| Race (% white) | 88.2 | 80.0 | 80.0 |
| Worst Lactate (within 24 hr of admission), median, IQR) | N/A | 6.6 (4.3–8.8) | 2.1 (1.5–3.0) |
| Comorbidities (% yes) | |||
| Diabetes Mellitus | 0.0 | 36.0 | 20.0 |
| Chronic Obstructive Pulmonary Disease | 0.0 | 20.0 | 24.0 |
| Congestive Heart Failure | 0.0 | 12.0 | 16.0 |
| Chronic Kidney Disease | 0.0 | 16.0 | 8.0 |
| Initial rhythm (% shockable) | N/A | 52.0 | N/A |
| Hospital Mortality (% died) | 0.0 | 56.0 | 20.0 |
Vitamin C Levels at Time 0
The median baseline vitamin C level in cardiac arrest patients was 0.33 mg/dL (0.05–0.83), as compared to 0.91mg/dL (0.69–1.48) in the healthy control group and 0.28mg/dL (0.11–0.59) in the septic group. Vitamin C levels were significantly lower in the cardiac arrest group than in the control group (p=<0.01). There was no significant difference in vitamin C levels between the cardiac arrest and sepsis patients (p=0.36). These data are shown in Figure 1.
Figure 1:
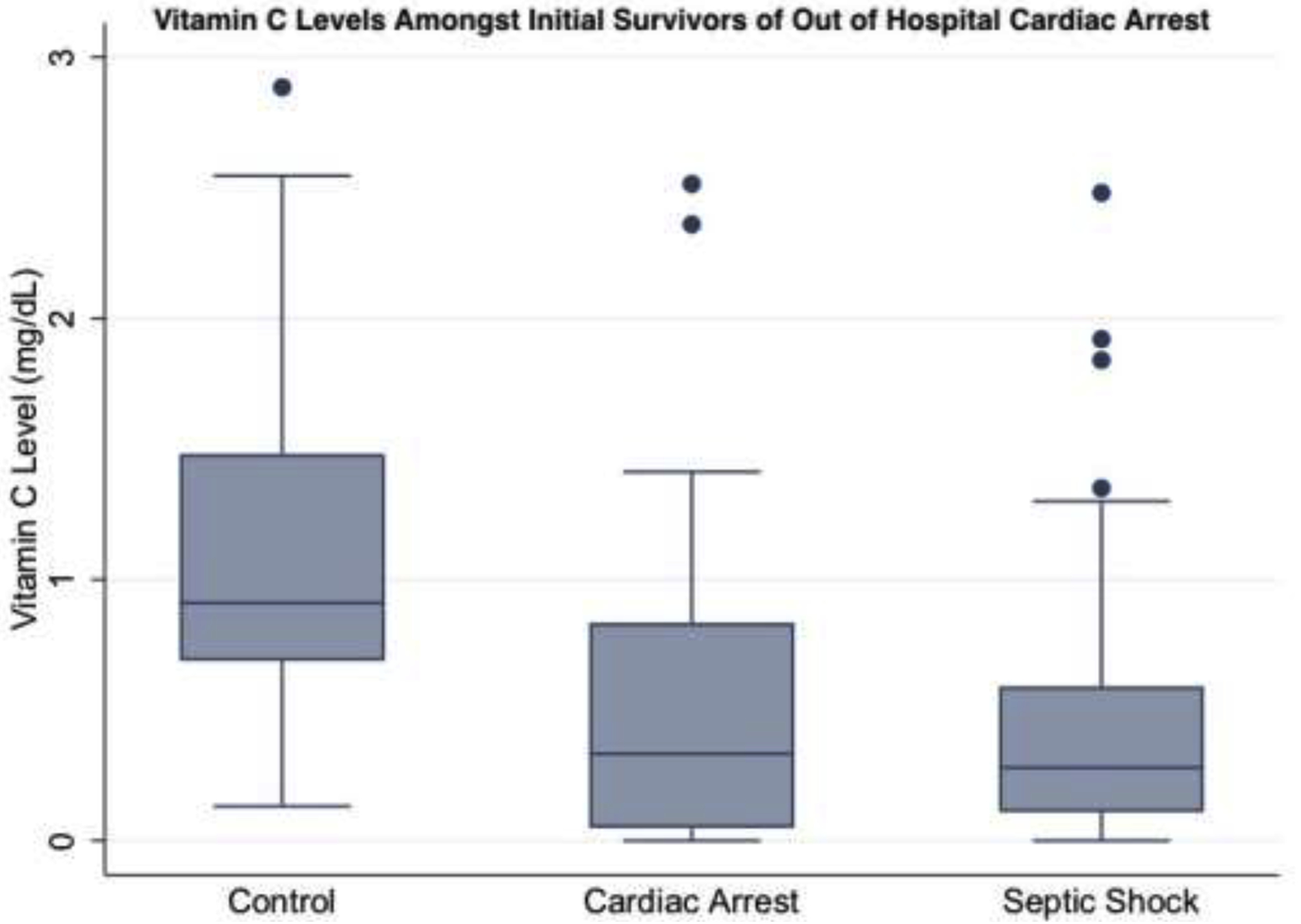
Median Vitamin C Levels in 3 Groups at Time 1 (0 Hours). This figure represents median (IQR) vitamin C levels for each of the 3 groups at time point 0. Levels were significantly lower in post-arrest and septic groups compared to healthy controls. Levels were similar between post-arrest and septic groups.
Vitamin C Levels in Post-Arrest Group Between 0 and 24 Hours
A total of 12 post-arrest patients had repeat plasma samples available for testing at 24-hours. The median vitamin C level among those patients at 24-hours was 0.07 mg/dL (0.01–0.19). Although lower than initial levels, this did not reach the a priori determined significance threshold of 0.05 (p=0.08). These data are shown in Figure 2.
Figure 2:
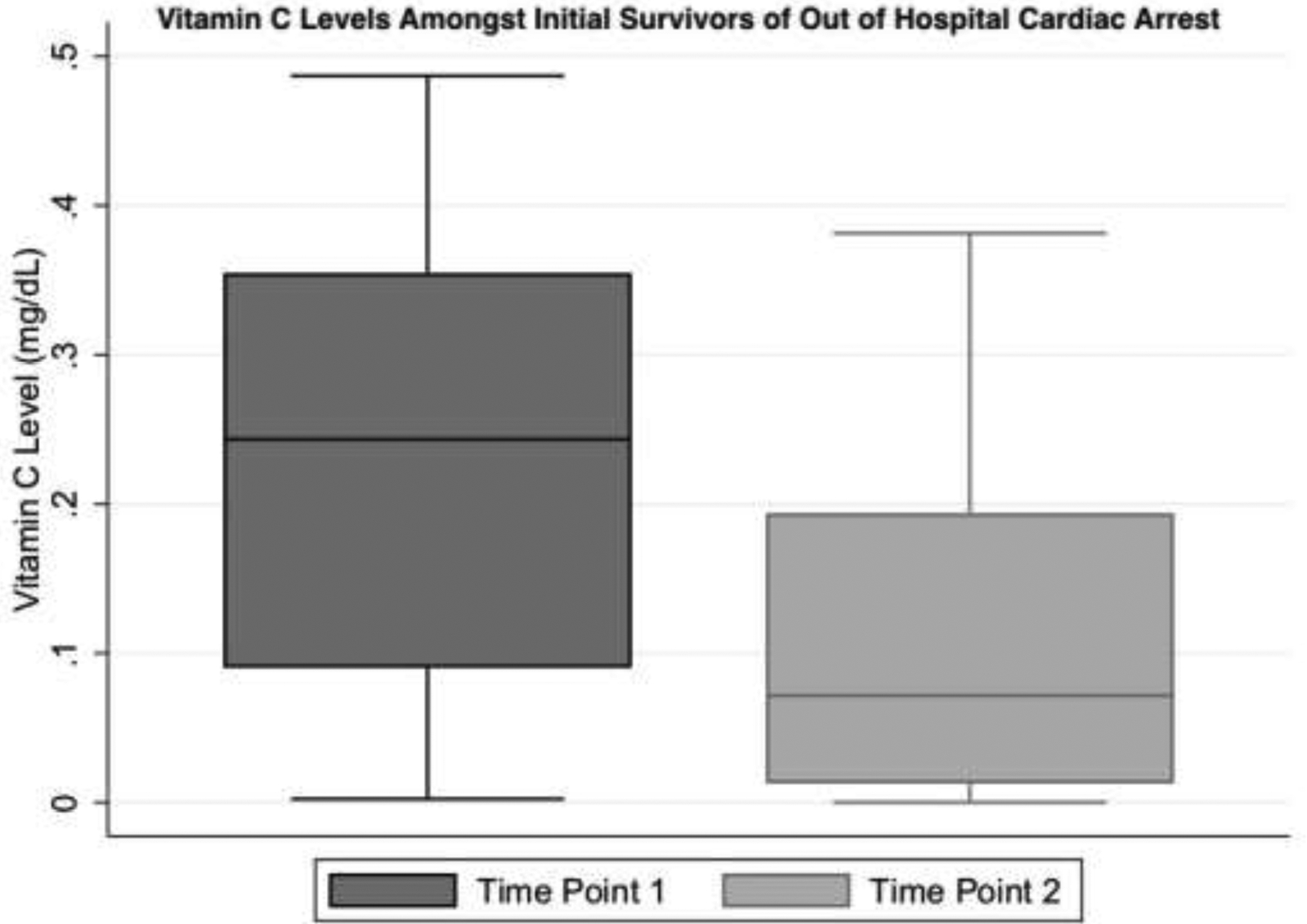
Vitamin C Levels in Post Arrest Patients at Time 1 and 2. This figure shows median (IQR) levels of vitamin C for the post-arrest group at time point 1 (~0–6 hours) and time point 2 (24 hours). At 24 hours, repeat vitamin C levels were trending downwards, nearing statistical significance.
Discussion:
In this study, serum vitamin C levels were lower in patients post-cardiac arrest as compared to healthy controls and were similar to those in septic patients. Over the next 24 hours, vitamin C levels in post-arrest patients trended downwards. Aside from an abstract from Grooth et al in 201414, we believe this is the first study to describe vitamin C levels in human subjects post-cardiac arrest.
Multiple studies have identified vitamin C deficiency in sepsis and septic shock patients5,7,14. While Fowler7 and Carr5 found mean vitamin C levels of 0.29 mg/dL and 0.27 mg/dL respectively, Grooth14 found a median level of 0.35 mg/dL. In this study, we found that vitamin C levels in a post-arrest population were decreased to a similar magnitude as those in a septic population. Vitamin C deficiency during critical illness may be due to increased metabolic demand. Both sepsis and the post-cardiac arrest syndrome generate significant oxidative stress10,11, which could result in excess metabolic consumption of vitamin C. The acute nature of out-of-hospital cardiac arrest suggests that poor oral intake/malnutrition is a less prominent contributor to post-arrest vitamin C deficiency. The processes by which vitamin C levels fall in critical illness are an important avenue of future investigation.
The large age difference between the healthy controls and the septic and cardiac arrest patients in this study could explain the increased rate of vitamin C deficiency we observed. However, while elderly patients are known to be higher risk for malnutrition, the 2003–2004 National Health and Nutrition Examination Survey (NHANES) conducted by the Centers for Disease Control found mean vitamin C levels were higher in patients > 60 years old compared to those 20–39 years old.15 Given this, we feel it is unlikely the difference we are seeing are solely due to age and more likely related to the underlying pathophysiology of their illness.
Supplementation of vitamin C has been studied in populations of critically ill septic patients with mixed outcomes.6–9,16 In the CITRUS-ALI trial, Fowler et al found no difference in the primary outcomes of modified SOFA scores and C-Reactive Protein levels in patients with severe sepsis who developed ARDS. However, secondary outcomes analysis showed statistically significant improvements in 28-day mortality and hospital-free days at 60-days.9 While the improvement in mortality is less dramatic than those reported by Marik and Kim6,16, it is encouraging that improvements in mortality were replicated in a larger scale trial. More recently, in the VITAMINS multicenter randomized trial comparing administration of hydrocortisone, vitamin C and thiamine combination to hydrocortisone alone in patients with septic shock, Fujii et al found no difference in the primary outcome of median time alive and free of vasopressors. This was a well-designed study, however, it should be noted it was underpowered to detect differences in mortality and the effects of vitamin C and thiamine were not assessed separately.17
To date, there have not been any studies examining the effect of supplemental vitamin C in human subjects post-cardiac arrest. However, two animal studies by Tsai et al demonstrated that, in rat models with induced ventricular fibrillation of 5 minutes prior to onset of CPR and defibrillation, supplementation of IV vitamin C was associated with decreased myocardial necrosis, improved myocardial function, increased ability to obtain ROSC, and improved survival and neurologic outcomes of mice at 72 hours post-arrest.18,19
There were several limitations to our study. First, the blood samples we used were several years old, although all were from approximately the same years and all were frozen at −80 Celsius which is generally protective. Second, we used colorimetry/fluorimetry to quantify vitamin C levels. Other investigators have used mass spectrometry, which may be more sensitive. Finally, we used a small, retrospective sample since this study was meant to be hypothesis generating.
Conclusions:
Vitamin C levels were lower in patients post-cardiac arrest compared to controls and were similar to patients with sepsis. These levels appeared to continue to decline over their first 24 hours of admission. Future study trending vitamin C levels post-cardiac arrest and supplementation of vitamin C to these patients with outcome-based measures is a reasonable next step.
Acknowledgements:
Special thanks to the Center for Resuscitation Science at Beth Israel Deaconess Medical Center for their contributions to this manuscript
Source of Funding: This study was supported by a grant from the Open Philanthropy Project. Dr. Moskowitz is supported by a grant from the National Institutes of Health (K23GM128005–01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
Abbreviations: CCI: Committee on Clinical Investigation; ED: Emergency Department; IQR: Inter-Quartile Range; IRB: Institutional Review Board; NHANES: National Health and Nutrition Examination Survey; ROSC: Return of Spontaneous Circulation;
References:
- 1.Carr AC, Maggini S. Vitamin C and Immune Function. Nutrients. 2017;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carr AC, Shaw GM, Fowler AA, Natarajan R. Ascorbate-dependent vasopressor synthesis: a rationale for vitamin C administration in severe sepsis and septic shock? Crit Care. 2015;19:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long CL, Maull KI, Krishnan RS, et al. Ascorbic acid dynamics in the seriously ill and injured. J Surg Res. 2003;109:144–8. [DOI] [PubMed] [Google Scholar]
- 4.Schorah CJ, Downing C, Piripitsi A, et al. Total vitamin C, ascorbic acid, and dehydroascorbic acid concentrations in plasma of critically ill patients. Am J Clin Nutr. 1996;63:760–5. [DOI] [PubMed] [Google Scholar]
- 5.Carr AC, Rosengrave PC, Bayer S, Chambers S, Mehrtens J, Shaw GM. Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes. Crit Care. 2017;21:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J. Hydrocortisone, Vitamin C, and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A Retrospective Before-After Study. Chest. 2017;151:1229–38. [DOI] [PubMed] [Google Scholar]
- 7.Fowler AA 3rd, Syed AA, Knowlson S, et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014;12:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zabet MH, Mohammadi M, Ramezani M, Khalili H. Effect of high-dose Ascorbic acid on vasopressor’s requirement in septic shock. J Res Pharm Pract. 2016;5:94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fowler AA 3rd, Truwit JD, Hite RD, et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients With Sepsis and Severe Acute Respiratory Failure: The CITRIS-ALI Randomized Clinical Trial. JAMA. 2019;322:1261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–83. [DOI] [PubMed] [Google Scholar]
- 11.Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation. 2002;106:562–8. [DOI] [PubMed] [Google Scholar]
- 12.Donnino MW, Liu X, Andersen LW, et al. Characterization of mitochondrial injury after cardiac arrest (COMICA). Resuscitation. 2017;113:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leaf DE, Raed A, Donnino MW, Ginde AA, Waikar SS. Randomized controlled trial of calcitriol in severe sepsis. Am J Respir Crit Care Med. 2014;190:533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grooth HJ S-dMA, Oudemans-van Straaten HM. Early plasma vitamin C concentration, organ dysfunction and ICU mortality. Intensive Care Med. 2014;40:Suppl 1:S199. [Google Scholar]
- 15.Schleicher RL, Carroll MD, Ford ES, Lacher DA. Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr. 2009;90:1252–63. [DOI] [PubMed] [Google Scholar]
- 16.Kim WY, Jo EJ, Eom JS, et al. Combined vitamin C, hydrocortisone, and thiamine therapy for patients with severe pneumonia who were admitted to the intensive care unit: Propensity score-based analysis of a before-after cohort study. J Crit Care. 2018;47:211–8. [DOI] [PubMed] [Google Scholar]
- 17.Fujii T, Udy AA, Deane AM, et al. Vitamin C, Hydrocortisone and Thiamine in Patients with Septic Shock (VITAMINS) trial: study protocol and statistical analysis plan. Crit Care Resusc. 2019;21:119–25. [PubMed] [Google Scholar]
- 18.Tsai MS, Huang CH, Tsai CY, et al. Combination of intravenous ascorbic acid administration and hypothermia after resuscitation improves myocardial function and survival in a ventricular fibrillation cardiac arrest model in the rat. Acad Emerg Med. 2014;21:257–65. [DOI] [PubMed] [Google Scholar]
- 19.Tsai MS, Huang CH, Tsai CY, et al. Ascorbic acid mitigates the myocardial injury after cardiac arrest and electrical shock. Intensive Care Med. 2011;37:2033–40. [DOI] [PubMed] [Google Scholar]


