Abstract
Objective:
To assess the association between preoperative opioid exposure and readmissions following elective surgery.
Summary Background Data:
Preoperative opioid use is common, but its effect on opioid-related, pain-related, respiratory-related and general readmissions following surgery is unknown.
Methods:
We analyzed claims data from a 20% national Medicare sample of patients ages ≥ 65 with Medicare Part D claims undergoing surgery between 1/1/2009 – 11/30/2016. We grouped patients by the dose, duration, recency, and continuity of preoperative opioid prescription fills. We used logistic regression to examine the association between prior opioid exposure and 30-day readmission, adjusted for patient risk factors and procedure type.
Results:
Of 373,991 patients, 168,579 (45%) filled a preoperative opioid prescription within 12 months of surgery, ranging from minimal to chronic high use. Preoperative opioid exposure was associated with higher rate of opioid-related readmissions, compared with naïve patients [low: aOR=1.63, 95% CI=1.26–2.12; high: aOR=3.70, 95% CI=2.71–5.04]. Preoperative opioid exposure was also associated with higher risk of pain-related readmissions [low: aOR=1.27, 95% CI=1.23–1.32; high: aOR=1.62, 95% CI=1.53–1.71] and respiratory-related readmissions [low: aOR=1.10, 95% CI=1.05–1.16; high: aOR=1.44, 95% CI=1.34–1.55]. Low, moderate, and high chronic preoperative opioid exposures were predictive of general readmissions (low: OR 1.09, 95% CI: 1.06–1.12); high: OR 1.23, 95% CI: 1.18–1.29).
Conclusions:
Higher levels of preoperative opioid exposure is associated with increased risk of readmissions after surgery. These findings emphasize the importance of screening patients for preoperative opioid exposure and creating risk mitigation strategies for patients.
INTRODUCTION
In 2017, the United States accounted for 99.2% of global consumption of hydrocodone, and was the main consumer country for hydromorphone and oxycodone. 1 According to a national survey in 2015, 37.8% of U.S. adults used prescription opioids in the previous 12 months, most commonly for pain relief.2 Opioid use is common among older patients, with one in three Medicare Part D beneficiaries receiving a prescription opioid in 2016.3 Troublingly, older individuals also experienced the largest increase in opioid-related deaths between 2001 and 2016.4 In addition to risk of overdose, opioid analgesics have serious side effects including respiratory depression, bladder dysfunction and hyperalgesia.5,6,7
Patients with pre-existing opioid use present a particular challenge to surgeons, who strive to balance appropriate pain control with avoiding adverse effects of postoperative opioids. Previous studies have found that postoperative pain is predictive of subsequent emergency department visits and increased healthcare utilization.8,9 Chronic opioid exposure is also associated with increased postoperative complications, readmission rates, and healthcare costs.10,11 However, it is unknown whether the degree of preoperative opioid exposure changes the risk of adverse events after surgery, such as readmissions. Moreover, preoperative opioid exposure is heterogeneous,12,13 and practical strategies to define risk based on clinically meaningful groups of preoperative opioid exposure are not well described. Understanding this relationship could help identify high-risk patients and potentially prevent adverse events. To date, there is little information regarding the nuances of preoperative opioid exposure, and their effect on postoperative outcomes, including details of dosage, timing, and continuity in preoperative opioid exposure.
Readmission rates are key quality metrics for stakeholders interested in optimizing the value of surgical care, as preventable readmissions represent missed care opportunities for interventions and the need for better preoperative screening. For example, one study found that 48% of readmissions after laparoscopic bariatric surgery were preventable, indicating a need for quality improvement.14 Recently, the Centers of Medicare and Medicaid Services (CMS), have provided financial incentives to decrease readmissions, improve quality of care, and lower costs.15,16,17 To better understand the effect of preoperative opioid exposure on postoperative readmissions, we used the previously described opioid exposure classifications to study the risk of 30-day hospital readmissions among Medicare beneficiaries ages 65 years of age and older undergoing major or minor elective surgery.18 We hypothesized that preoperative opioid exposure would be associated with increased risk of opioid-related, pain-related, respiratory-related, and general hospital readmissions 30 days after surgery.
METHODS
Data Source and Patient Cohort
In this retrospective observational study, we examined a 20% national sample of Medicare claims data to examine patients 65 years and older who underwent a surgical procedure from January 1, 2009 to November 30, 2016. This study was deemed exempt by the University of Michigan Human Research Protections Office.
As age has shown to increase risk of adverse effects from opioids,19,20 our cohort included patients aged 65 years and older who were continuously enrolled in Medicare Parts A, B, and D for 12 months before and 6 months after their surgical date. We selected 15 common elective procedures based on Current Procedural Terminology Fourth Edition (CPT-4) codes (Appendix I) and categorized them as major or minor procedures. Minor procedures included varicose vein removal, laparoscopic cholecystectomy, laparoscopic appendectomy, hemorrhoidectomy, thyroidectomy, transurethral prostate surgery, parathyroidectomy, and carpal tunnel. Major procedures included ventral incisional hernia repair, colectomy, reflux surgery, bariatric surgery, hysterectomy, total hip arthroplasty, and total knee arthroplasty. We excluded patients who had a length of stay greater than 30 days, and patients who were not discharged home.
Outcomes
We examined four outcomes: (1) 30-day opioid-related readmissions (e.g., adverse effects of opioids, opioid abuse, and opioid poisoning), (2) 30-day pain-related readmissions (e.g., postoperative pain, abdominal and bowel pain, and fibromyalgia), (3) 30-day respiratory-readmissions (e.g., acute respiratory failure, upper respiratory drug-induced interstitial lung disorders, and apnea), and (4) 30-day general readmissions. We queried claims data for inpatient and emergency department claims with a readmission date within 30 days after discharge. We identified opioid-related readmissions by matching diagnosis codes in the claims with the list in Appendix II.21 We identified pain-related readmissions using a previously described algorithm.22 For respiratory-readmissions, we reviewed related ICD-9 and ICD-10 diagnosis codes in Appendix III.
Explanatory Variable and other Patient Characteristics
The main explanatory variable was preoperative opioid exposure. Medicare Part D pharmacy claims were used to identify patients with preoperative opioid exposure, defined as filling at least one prescription during the year before surgery. Opioid prescriptions were selected based on generic name matched with National Drug Code. Total amount prescribed was calculated by taking the product of strength, quantity and a factor for converting different types of opioid to oral morphine equivalents (OMEs).23 For ease of interpretation, prescription size was also reported as number of tablets of 5/325mg hydrocodone-acetaminophen (one 5 mg hydrocodone tablet = 5 OME).
Preoperative opioid exposure was described using four attributes: dose, duration, recency, and continuity of use.18 Dose was defined as total OMEs of prescriptions filled in the year before the operation. Duration was the total number of months during which a patient filled an opioid prescription. Recency was defined as the number of months since the last opioid filled before the operation. Continuity was defined as the longest “streak” of months that a patient consecutively filled a prescription. We used previously described clustering analysis, a machine learning algorithm, to classify patients into groups of preoperative exposure.24,18
Patient demographic characteristics were age, sex, race/ethnicity, region of residence, and Medicaid eligibility. Patients were grouped into 5 age groups (65–69, 70–74, 75–79, 80–84, and 85+). Race/Ethnicity included White, Black, Hispanic and Others. There were nine geographic region of residences including East North Central, East South Central, Middle Atlantic, Mountain, New England, Pacific, South Atlantic, West North Central, and West South Central. Medicaid eligibility was based on the dual eligibility status in the month of surgery.
Charlson Comorbidity Index (CCI), tobacco use, mental health disorders, and pain disorders, were based on diagnosis codes in the claims during the year before surgery. CCI was categorized into different categories: 0, 1–2, 3–4, and ≥5. Patients who had a diagnosis of tobacco use (ICD-9-CM: 305.1, V15.82; ICD-10-CM: F17.***, Z87.891, Z72.0) were defined as smoker or history of smoking. Mental health disorders (adjustment, anxiety, mood, suicide or self-harm, disruptive, personality, psychosis, alcohol or other substance abuse disorders, and other mental health disorders) were based on the Clinical Classifications Software (CCS) for ICD-9-CM and ICD-10-CM.25 History of pain disorders (arthritis, back, neck, and other pain) were identified by ICD-9 and ICD-10 diagnosis codes (see Appendix IV). Additionally, we adjusted for any hospitalization and skilled nursing facility stay within 1 year before the patient’s surgical date. We also identified patients who concurrently filled a benzodiazepine and opioid prescription in the perioperative period, defined as 30 days prior to and 14 days after surgery.
Statistical Analysis
We used descriptive statistics to present demographic and clinical characteristics of the study cohort. We then used logistic regression models to estimate preoperative opioid exposure and the other factors associated with opioid-related readmissions, pain-related readmissions, respiratory-related readmissions, and general readmissions within 30 days after discharge. Multicollinearity was tested among all covariate. The model fit was evaluated using c-statistics. Cluster analysis was performed using R version 3.6.1, and all other analyses were performed using SAS version 9.4 and Stata version 15.1. Statistical significance was defined as p< 0.05 with 2-sided tests.
RESULTS
We identified 373,991 patients who underwent major or minor elective surgical procedures during the study period. The demographic and clinical profiles of the overall patient cohort are summarized in Table 1. In this cohort, 223,541 (60%) underwent a major procedure, and 150,449 (40%) underwent a minor procedure. In addition, 231,563 (62%) were female, 320,694 (86%) were Caucasian, and 20,950 (6%) were African-American. There were 14,771 (4%) patients who filled a benzodiazepine concurrently with their opioid prescription during the preoperative period. Finally, 205,412 (55%) patients were opioid-naïve, while 168,579 (45%) had filled an opioid prescription in the 12 months before surgery.
Table 1.
Patient Characteristics
| Characteristics | N | % |
|---|---|---|
| Total cases | 373,991 | |
| Age, y | ||
| 65–69 | 109094 | 29.17 |
| 70–74 | 108156 | 28.92 |
| 75–79 | 78288 | 20.93 |
| 80–84 | 48741 | 13.03 |
| ≥85 | 29712 | 7.94 |
| Gender | ||
| Male | 142428 | 38.08 |
| Female | 231563 | 61.92 |
| Race | ||
| White | 320694 | 85.75 |
| Black | 20950 | 5.6 |
| Hispanic | 20633 | 5.52 |
| Other | 9855 | 2.64 |
| Missing | 1859 | 0.5 |
| Resided in Metropolitan County | ||
| Yes | 278266 | 74.4 |
| No | 95318 | 25.49 |
| Missing | 407 | 0.11 |
| Division | ||
| East North Central | 39005 | 10.43 |
| East South Central | 18757 | 5.02 |
| Middle Atlantic | 34378 | 9.19 |
| Mountain | 30912 | 8.27 |
| New England | 51773 | 13.84 |
| Pacific | 16997 | 4.54 |
| South Atlantic | 77765 | 20.79 |
| West North Central | 29195 | 7.81 |
| West South Central | 36851 | 9.85 |
| Unknown | 38358 | 10.26 |
| Charlson Comorbidity Index | ||
| None (CCI 0) | 94751 | 25.34 |
| Mild (CCI 1, 2) | 141481 | 37.83 |
| Moderate (CCI 3, 4) | 77217 | 20.65 |
| Severe (CCI ≥5) | 60542 | 16.19 |
| Medicaid eligibility | 56628 | 15.14 |
| Any hospitalization in previous year | 78201 | 20.91 |
| Skilled nursing facility stay in previous year | 12483 | 3.34 |
| History of tobacco use | 56317 | 15.06 |
| Surgery Type | ||
| Major surgery | 223542 | 59.77 |
| Minor surgery | 150449 | 40.23 |
| Mental Health Disorders | ||
| Adjustment | 6579 | 1.76 |
| Anxiety | 46862 | 12.53 |
| Mood | 56450 | 15.09 |
| Suicide or self-harm | 590 | 0.16 |
| Disruptive | 1393 | 0.37 |
| Personality | 678 | 0.18 |
| Psychosis | 7183 | 1.92 |
| Alcohol or other substance use disorders | 9507 | 2.54 |
| Other Mental Health Disorders | 10101 | 2.7 |
| Pain Disorders | ||
| Arthritis | 311507 | 83.29 |
| Back | 149225 | 39.9 |
| Neck | 57661 | 15.42 |
| Other pain | 149055 | 39.86 |
| Opioid filled during preop period (365 to 31 days prior to admission) | ||
| Yes | 168579 | 45.08 |
| No (Opioid Naive) | 205412 | 54.92 |
| Opioid filled during periop period (30 days before admission to 14 days after discharge) | 266444 | 71.24 |
| Benzo and Opioid filled concurrently during periop period | 14771 | 3.95 |
Patterns of Preoperative Opioid Exposure
We classified preoperative opioid exposure into 5 distinct groups based on dose, recency, duration, and continuity. The attributes of groups 1–4 are summarized in Table 2. Group 1 patients (n = 50,495) had remote, low-dose use of opioids within 1 month before surgery. Median [interquartile range (IQR)] prescription amount was 250 (400) OME, received at a median of 8 (4) months before surgery. Group 2 patients (n = 70,024) were characterized by recent (within 2 months), moderate dose use of low duration. Patients in this group received a median equivalent of 540 (975) OME over a 2 months duration. Group 3 patients (n = 30,108) received a higher dose of 4050 (4640) OME over a higher duration of 7 months. They had more recent preoperative opioid exposure and some discontinuity of fills (median continuity 4 months). Group 4 patients (n=17,952) had the highest dose use (“high chronic”), receiving a median equivalent of 11,964 (15,460) OME over 11 months. Patients in this group had sustained use (median continuity 11 months), and had filled 1 month before surgery.
Table 2.
Patient Groups and Attributes of Preoperative Opioid Exposure within One Year of Surgery
| Total oral morphine equivalent (OME)* filled during preop | Duration in month | Continuity in month | Recency in month | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Group name | n | % | median | iqr† | median | iqr | median | iqr | median | iqr |
| 1 | Minimal | 50,495 | 29.95 | 250 | 400 | 1 | 0 | 1 | 0 | 8 | 4 |
| 2 | Low | 70,024 | 41.54 | 540 | 975 | 2 | 2 | 1 | 1 | 2 | 1 |
| 3 | Moderate | 30,108 | 17.86 | 4050 | 4640 | 7 | 2 | 4 | 2 | 2 | 1 |
| 4 | High Chronic | 17,952 | 10.65 | 11,964.4 | 15,460 | 11 | 1 | 11 | 2 | 1 | 1 |
5 OME = one 5mg hydrocodone tablet.
IQR = interquartile range
Overall readmission rates stratified by preoperative opioid exposure are summarized in Table 3. Among minimal preoperative opioid users, there were 58 (0.11%) opioid-related readmissions, 3259 (6.45%) pain-related readmissions, 1622 (3.21%) respiratory-related readmissions, and 6305 (12.49%) general readmissions. Among patients with low preoperative opioid exposure, there were 102 (0.15%) opioid-related readmissions, 5261 (7.51%) pain-related readmissions, 2526 (3.61%) respiratory-related readmissions, and 9602 (13.71%) general readmissions. Patients with moderate opioid exposure before surgery were at greater risk of readmission with 63 (0.21%) opioid-related readmissions, 2908 (9.66%) pain-related readmissions, 1474 (4.90%) respiratory-related readmission, and 4885 (16.22%) general readmissions. Patients with high chronic opioid exposures experienced the highest risk of readmission, with 82 (0.46%) opioid-related readmissions, 2072 (11.54%) pain-related readmissions, 1065 (5.93%) respiratory-related readmissions, and 3167 (17.64%) general readmissions.
Table 3.
Association between Preoperative Opioid Exposure and Readmissions
| Opioid-related Readmission | Pain-related Readmission | Respiratory-related Readmission | General Readmission | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Group Name | Total n | n | % | n | % | n | % | n | % |
| 0 | Opioid-naïve | 205,412 | 147 | 0.07 | 10,205 | 4.97 | 5,529 | 2.69 | 23,017 | 11.21 |
| 1 | Minimal | 50,495 | 58 | 0.11 | 3,259 | 6.45 | 1,622 | 3.21 | 6,305 | 12.49 |
| 2 | Low | 70,024 | 102 | 0.15 | 5,261 | 7.51 | 2,526 | 3.61 | 9,602 | 13.71 |
| 3 | Moderate | 30,108 | 63 | 0.21 | 2,908 | 9.66 | 1,474 | 4.9 | 4,885 | 16.22 |
| 4 | High Chronic | 17,952 | 82 | 0.46 | 2,072 | 11.54 | 1,065 | 5.93 | 3,167 | 17.64 |
Association of preoperative opioid exposure and postoperative readmissions
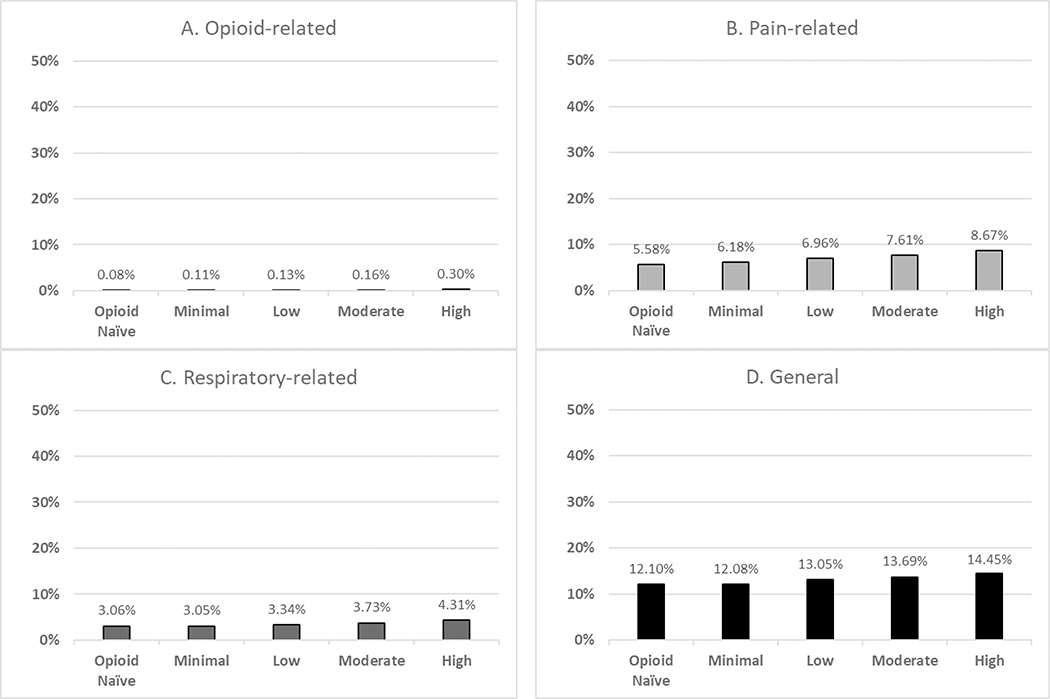
After multivariable risk adjustment, preoperative opioid use was significantly associated with an increased risk of readmission (Figure 1). Compared to the opioid-naïve group (0.08%), patients with minimal and low levels of opioid exposure had increased adjusted rate of opioid-related readmission (0.11% and 0.13%, respectively). Likelihood of opioid-related readmissions for moderate level users was double (0.16%) that of opioid-naïve patients, and the high chronic exposure group had the greatest risk of readmission (0.30%).
Figure 1.
Adjusted Rates of opioid-related, pain-related, and respiratory-related, and general Readmission (%) by Preoperative Use (opioid-naïve, minimal, low, moderate, and high chronic)
We observed similar associations between preoperative opioid exposure and pain-related readmissions. Risk of pain-related readmissions after discharge was higher (8.67%) in patients with high chronic opioid exposure, compared to their opioid-naïve counterparts (5.58%). Minimal, low, and moderate levels of exposure were also associated with increased risk of pain-related readmissions (6.18%, 6.96%, and 7.61%, respectively).
Compared to baseline (3.06%), high chronic exposure was predictive of increased respiratory-related readmissions (4.31%). Patients with low and moderate levels of opioid exposure also experienced greater risk of respiratory-related readmissions relative to the opioid-naïve group (3.34% and 3.73%, respectively).
We observe a similar risk of general readmissions in patients with minimal preoperative opioid exposures (12.08%) as baseline (12.10%). However, patients with low, moderate, and chronic high exposure to opioids within 12 months of surgery were at higher risk of general readmissions (13.05%, 13.69%, and 14.45%, respectively).
Opioid-related Readmissions
The results of our multivariate logistic regression for preoperative opioid exposures are summarized in Table 4. High chronic use was the most influential predictor of opioid-related readmission, with high chronic users 3.7-fold more likely to have opioid-related readmissions compared to opioid-naïve patients (high: OR 3.70, 95% CI: 2.71–5.04). Other variables significantly associated with opioid-related readmission included diagnoses of alcohol and substance use disorder (OR 2.44, 95% CI: 1.77–3.37) and concurrent fills of benzodiazepines during the perioperative period (OR 2.08, 95% CI: 1.55–2.78). Patients with low and moderate preoperative use were also at significantly higher risk of opioid-related readmission (low: OR 1.63, 95% CI: 1.26–2.12; moderate: OR 1.90, 95% CI: 1.38–2.61).
Table 4.
Association between Preoperative Opioid Exposure and Respiratory-related Complications, Opioid-related Complications, Pain-related Complications, and General Readmissions within 30 days after Discharge
| Opioid-related Readmissions | Pain-related Readmissions | Respiratory-related Readmissions | General Readmissions | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Preop Opioid Exposure Group (Ref: Opioid-naïve) | ||||||||
| Minimal | 1.36 (1.00 1.85) | 0.052 | 1.12 (1.07 1.16) | <0.001 | 1.00 (0.94 1.06) | 0.974 | 1.00 (0.97 1.03) | 0.931 |
| Low | 1.63 (1.26 2.12) | <0.001 | 1.27 (1.23 1.32) | <0.001 | 1.10 (1.05 1.16) | <0.001 | 1.09 (1.06 1.12) | <0.001 |
| Moderate | 1.90 (1.38 2.61) | <0.001 | 1.40 (1.34 1.47) | <0.001 | 1.24 (1.16 1.32) | <0.001 | 1.16 (1.12 1.20) | <0.001 |
| High | 3.70 (2.71 5.04) | <0.001 | 1.62 (1.53 1.71) | <0.001 | 1.44 (1.34 1.55) | <0.001 | 1.23 (1.18 1.29) | <0.001 |
| Age, y (Ref: 65–69) | ||||||||
| 70–74 | 0.84 (0.66 1.09) | 0.188 | 1.06 (1.02 1.10) | 0.002 | 1.11 (1.05 1.17) | <0.001 | 1.08 (1.06 1.11) | <0.001 |
| 75–79 | 1.08 (0.83 1.41) | 0.577 | 1.17 (1.12 1.22) | <0.001 | 1.37 (1.30 1.44) | <0.001 | 1.23 (1.20 1.27) | <0.001 |
| 80–84 | 1.16 (0.85 1.58) | 0.343 | 1.32 (1.26 1.38) | <0.001 | 1.51 (1.43 1.61) | <0.001 | 1.41 (1.36 1.46) | <0.001 |
| ≥85 | 1.40 (0.98 1.99) | 0.065 | 1.55 (1.47 1.63) | <0.001 | 1.92 (1.79 2.05) | <0.001 | 1.64 (1.58 1.71) | <0.001 |
| Female (Ref: Male) | 1.14 (0.93 1.41) | 0.204 | 1.00 (0.97 1.02) | 0.714 | 0.92 (0.88 0.96) | <0.001 | 0.82 (0.81 0.84) | <0.001 |
| Race (Ref: White) | ||||||||
| Black | 0.92 (0.60 1.40) | 0.696 | 1.27 (1.20 1.33) | <0.001 | 1.05 (0.97 1.12) | 0.229 | 1.28 (1.23 1.33) | <0.001 |
| Hispanic | 0.98 (0.61 1.55) | 0.919 | 0.92 (0.86 0.97) | 0.005 | 0.69 (0.63 0.75) | <0.001 | 0.96 (0.92 1.01) | 0.084 |
| Other | 1.24 (0.67 2.26) | 0.495 | 0.97 (0.89 1.05) | 0.421 | 0.74 (0.66 0.84) | <0.001 | 0.98 (0.92 1.04) | 0.439 |
| Missing | 2.33 (0.95 5.71) | 0.065 | 0.86 (0.69 1.07) | 0.177 | 0.68 (0.48 0.97) | 0.036 | 0.83 (0.70 0.97) | 0.021 |
| Medicaid eligibility (Ref: No) | 0.68 (0.51 0.91) | 0.009 | 1.29 (1.24 1.34) | <0.001 | 1.64 (1.56 1.71) | <0.001 | 1.33 (1.29 1.36) | <0.001 |
| Charlson Comorbidity Index (Ref: None (CCI 0)) | ||||||||
| Mild (CCI 1, 2) | 0.88 (0.68 1.15) | 0.342 | 1.19 (1.15 1.24) | <0.001 | 1.50 (1.41 1.60) | <0.001 | 1.20 (1.17 1.24) | <0.001 |
| Moderate (CCI 3, 4) | 0.96 (0.72 1.30) | 0.802 | 1.37 (1.31 1.43) | <0.001 | 1.98 (1.85 2.11) | <0.001 | 1.42 (1.38 1.47) | <0.001 |
| Severe (CCI ≥5) | 1.22 (0.90 1.66) | 0.205 | 1.71 (1.63 1.79) | <0.001 | 2.65 (2.48 2.84) | <0.001 | 1.84 (1.78 1.90) | <0.001 |
| History of tobacco use (Ref: Non-smoker) | 1.26 (1.00 1.60) | 0.052 | 1.13 (1.09 1.17) | <0.001 | 1.49 (1.43 1.56) | <0.001 | 1.12 (1.09 1.15) | <0.001 |
| Surgery type None (Ref: Minor) | ||||||||
| Major | 1.90 (1.53 2.36) | <0.001 | 1.21 (1.17 1.24) | <0.001 | 1.19 (1.15 1.24) | <0.001 | 1.20 (1.17 1.22) | <0.001 |
| Mental Health Disorders | ||||||||
| Adjustment (Ref: No) | 1.60 (1.03 2.50) | 0.037 | 1.01 (0.92 1.10) | 0.878 | 0.94 (0.83 1.06) | 0.327 | 1.02 (0.95 1.09) | 0.554 |
| Anxiety | 1.20 (0.94 1.54) | 0.147 | 1.16 (1.12 1.21) | <0.001 | 1.14 (1.08 1.20) | <0.001 | 1.13 (1.10 1.17) | <0.001 |
| Mood | 1.15 (0.90 1.46) | 0.267 | 1.19 (1.15 1.23) | <0.001 | 1.19 (1.13 1.25) | <0.001 | 1.17 (1.14 1.20) | <0.001 |
| Suicide or self-harm | 1.24 (0.43 3.55) | 0.687 | 1.43 (1.15 1.78) | 0.001 | 1.03 (0.76 1.39) | 0.838 | 1.38 (1.15 1.66) | 0.001 |
| Disruptive | 1.83 (0.84 3.98) | 0.128 | 1.00 (0.83 1.20) | 0.960 | 0.86 (0.67 1.12) | 0.264 | 1.05 (0.91 1.21) | 0.532 |
| Personality | 1.38 (0.48 3.94) | 0.551 | 1.12 (0.88 1.41) | 0.362 | 0.95 (0.69 1.30) | 0.745 | 1.21 (1.01 1.46) | 0.042 |
| Psychosis | 1.41 (0.90 2.22) | 0.132 | 1.16 (1.08 1.25) | <0.001 | 1.33 (1.21 1.45) | <0.001 | 1.19 (1.12 1.27) | <0.001 |
| Alcohol or other substance use disorders | 2.44 (1.77 3.37) | <0.001 | 1.20 (1.12 1.29) | <0.001 | 0.99 (0.90 1.09) | 0.860 | 1.19 (1.12 1.25) | <0.001 |
| Other Mental Disorders | 1.55 (1.06 2.27) | 0.023 | 1.18 (1.10 1.27) | <0.001 | 1.10 (1.00 1.21) | 0.057 | 1.12 (1.06 1.18) | <0.001 |
| Pain Disorders | ||||||||
| Arthritis (Ref: No) | 1.38 (0.96 1.97) | 0.083 | 1.16 (1.11 1.21) | <0.001 | 0.89 (0.84 0.94) | <0.001 | 0.89 (0.87 0.92) | <0.001 |
| Back | 1.04 (0.85 1.28) | 0.696 | 1.14 (1.11 1.18) | <0.001 | 1.01 (0.97 1.06) | 0.528 | 1.06 (1.04 1.08) | <0.001 |
| Neck | 1.11 (0.87 1.40) | 0.403 | 1.02 (0.98 1.06) | 0.299 | 0.96 (0.91 1.01) | 0.112 | 0.98 (0.95 1.00) | 0.087 |
| Other pain | 1.14 (0.93 1.39) | 0.203 | 1.22 (1.19 1.26) | <0.001 | 1.18 (1.13 1.22) | <0.001 | 1.15 (1.13 1.18) | <0.001 |
| Any hospitalization in previous year (Ref: No) | 1.12 (0.88 1.43) | 0.367 | 1.28 (1.24 1.32) | <0.001 | 1.46 (1.40 1.53) | <0.001 | 1.36 (1.33 1.40) | <0.001 |
| Skilled nursing facility stay in previous year (Ref: No) | 1.32 (0.91 1.91) | 0.151 | 0.99 (0.94 1.06) | 0.853 | 1.15 (1.06 1.23) | <0.001 | 1.02 (0.98 1.08) | 0.323 |
| Benzo and Opioid filled concurrently during periop period (Ref: No) | 2.08 (1.55 2.78) | <0.001 | 1.19 (1.12 1.26) | <0.001 | 1.01 (093 1.11) | 0.774 | 1.13 (1.08 1.19) | <0.001 |
Pain-related Readmissions
Higher preoperative opioid exposure was also associated with increased risk of pain-related readmissions. Increased likelihood of pain-related readmissions was found to be significant even for patients with minimal preoperative opioid exposure compared to opioid-naïve patients (minimal: OR 1.12, 95% CI: 1.07–1.16; low: OR 1.27, 95% CI: 1.23–1.32; moderate: OR 1.40, 95% CI: 1.34–1.47; high: OR 1.62, 95% CI: 1.53–1.71). Patients with a Charlson Comorbidity Index >=5 had the highest risk of pain-related readmissions (OR 1.71, 95% CI: 1.63–1.79). Mental health disorders, including suicidality (OR 1.43, 95% CI: 1.15–1.78) and alcohol or substance abuse disorders (OR 1.20, 95% CI: 1.12–1.29), were also predictive of pain-related readmissions.
Respiratory-related Readmissions
Preoperative opioid exposure was significantly associated with an increased risk of respiratory-related readmissions as compared to patients who were opioid-naïve (low: OR 1.10, 95% CI: 1.05–1.16); moderate: OR 1.24, 95% CI: 1.16–1.32; high: OR 1.44, 95% CI: 1.34–1.55). A high Charlson Comorbidity Index score (>=5) was the most significant predictor of respiratory-related readmissions (OR 2.65, 95% CI: 2.48–2.84). Other attributes correlated with higher risk of respiratory-related readmissions include history of tobacco use (OR 1.49, 95% CI: 1.43–1.56) and hospitalization in the previous year (OR 1.46, 95% CI: 1.40–1.53).
General Readmissions
While minimal opioid exposure prior to surgery was not significantly associated with higher general readmissions (OR 1.00, 95% CI: 1.40–1.53), low, moderate, and high chronic preoperative opioid exposures were predictive of general readmissions (low: OR 1.09, 95% CI: 1.06–1.12); moderate: OR 1.16, 95% CI: 1.12–1.20; high: OR 1.23, 95% CI: 1.18–1.29). A high Charlson Comorbidity Index score (>=5) was the most significant predictor of general readmissions (OR 1.84, 95% CI: 1.78–1.90), followed by age of 85 years or older (OR 1.64, 95% CI: 1.58–1.71).
DISCUSSION
In this national cohort of Medicare beneficiaries undergoing elective surgery, we observed that nearly 1 of every 2 patients (45%) presenting for elective surgery filled an opioid prescription in the previous 12 months, a relatively higher preoperative opioid use rate compared to younger cohorts described in previous studies.10, 18, 26 To capture intermittent use, this study’s definition of preoperative opioid exposure includes any fills in the year prior to surgery. While likelihood of readmissions rose with higher preoperative opioid exposure, we found that even remote, minimal use increased the risk of readmissions compared to opioid-naïve patients. For patients with recent, moderate dose use of low duration—which accounted for 41.5% of the preoperative opioid users—our results indicated a significantly higher risk of opioid-related, pain-related, and respiratory-related readmissions. Taken together, these findings highlight the importance of preoperative risk screening and optimization for patients already using opioids prior to undergoing elective surgery.
Our research aligns with prior studies examining the association between preoperative opioid exposure and increased postoperative healthcare utilization 9,27,28 and further describes the nuanced effect of varying degrees of opioid exposure. Among studies examining the association between preoperative opioid exposure and health outcomes, many have stratified groups based on the duration of preoperative opioid use alone.29,30,31,32 Incorporating the granular details of dosage, timing, and continuity allows for identification of the highest risk groups, specifically among patients with a high degree of preoperative opioid exposure. Increased pain-related complications in patients with preoperative opioid exposure have been well documented,33,34 and may relate to analgesic tolerance and opioid-induced hyperalgesia, along with other pathophysiologic effects of opioids.35 In this context, patients with preoperative opioid exposure could require additional opioid prescriptions after discharge or larger prescriptions,8 which may be challenging in light of a growing number of policies restricting opioid prescribing for acute pain. Notably, in this cohort, even patients with relatively minimal preoperative opioid exposure were more likely to experience pain-related readmissions.
Surprisingly, few studies have described the relationship between preoperative opioid exposure and respiratory-related readmissions after discharge. In one study, opioid abuse and dependence in patients undergoing elective orthopedic surgery was associated with postoperative morbidity and mortality, including respiratory failure.36 This may be due to the challenging nature of managing postoperative pain in patients with high opioid tolerance, whose higher opioid exposure may cause nocturnal hypoxemia and increase morbidity risk for patients with preexisting obstructive sleep apnea.37,38 Consistent with these reported outcomes, our analysis found that high chronic opioid exposure significantly increased the likelihood of respiratory-related readmissions even when controlling for other comorbidities. Even patients with relatively low and moderate levels of preoperative opioid exposures had greater risk of respiratory readmissions after discharge.
Opioid-related readmissions in patients with preoperative opioid exposure have previously been contextualized under discharge planning for patients in remission from opioid use disorder (OUD).39 In such patients, poorly controlled pain and access to prescription opioids can lead to both craving and relapse.40,41 Overdose prevention education and nasal naloxone prescription have been suggested as part of their relapse mitigation strategy. While there are distinct differences between high chronic use and OUD, our data shows significantly greater risk of opioid-related readmissions after surgery in patients with high chronic use. With high chronic use as the most influential predictor of opioid-related readmission, providing naloxone prescriptions at discharge may be warranted for some high-risk patients as part of their safe postoperative pain management plan.
Our study has several notable limitations. First, this is a retrospective analysis of Medicare claims data, and we could only account for opioid prescriptions that patients filled rather than the amount consumed. We also could not account for prescription opioids obtained outside of active insurance, medications that were filled prior to the restricted 12-month window, and opioids obtained from diverted prescriptions or other illicit opioid use (e.g. heroin use). Analysis of administrative claims data depends on coding methodology and accuracy, which may lead to an underestimation or overestimation of readmissions data. Additionally, although we did account for comorbid conditions, this may not fully capture patient frailty, which may affect risk of readmission after discharge. Finally, this study may not be generalizable to other age groups.
Despite these limitations, our findings have important implications for practitioners and policy makers. As standard practice, surgeons can set expectations by discussing postoperative pain and duration of opioid use with patients. For patients expected to need ongoing opioid prescriptions after surgery, surgeons may consider strategies like multimodal pain management therapy that have shown to significantly reduce follow-up pain scores and readmissions after discharge.42 One study of patients undergoing total joint arthroplasty also reported improved pain and functional outcomes after preoperative opioid reductions, providing further rationale for preoperative opioid weaning to minimize risk after surgery.43,44 Multidisciplinary programs that cater to individual pain management needs, which may include preoperative opioid weaning if appropriate, have the potential to reduce complications after surgery among patients with preoperative opioid exposure.45,46 These results complement our findings and highlight the importance of preoperative screening, which may facilitate disclosing risk to patients, coordinating care with their usual prescriber, and allocating resources effectively. Future clinical studies should assess postoperative outcomes of opioid-weaning protocols optimized for different surgical procedures, the results from which may better inform consideration for practical implementation.
As preoperative opioid exposure has shown to be predictive of readmissions, surgeons can benefit from routinely screening for preoperative opioid exposure as part of surgical risk assessment. This is particularly relevant to patients with relatively low and moderate levels of preoperative opioid exposure, whose remote or infrequent prescription filling may exclude them from being routinely queried. A prior study of patients undergoing major abdominal surgery found preoperative opioid use, which was quantified as a binary variable, to be predictive of increased costs and worse postoperative outcomes.10 By adding granularity to the levels of preoperative opioid exposure, our study validates thresholds of clinically meaningful risk by demonstrating that even minimal or low levels of opioid exposures can increase readmission rates, thereby contributing to higher healthcare costs. Future studies may consider incorporating details of dose, duration, recency, and continuity of use to better quantify cost burden associated with varying levels of preoperative opioid exposure.
In addition to optimizing preoperative counseling regarding pain expectations, our finding that 10% of our cohort met criteria for high chronic use underscores the importance of identifying risk factors and screening patients prior to surgery. However, all surgical patients receiving postoperative opioids can benefit from a more coordinated transitioning of care after discharge. In a cross-sectional survey of primary care physicians, most respondents reported deficiencies (poor communication, unclear postoperative plan, and unspecified provider roles in postsurgical care) in the transfer of care process for postsurgical patients and perceived these inadequate transitions to have contributed to adverse events.47 Developing guidelines for transitions of care for postoperative opioid prescribing and incentivizing multidisciplinary care coordination can promote a more patient-centered care, while minimizing suboptimal outcomes.48
Conclusion
Among Medicare beneficiaries 65 years and older, our study found that higher levels of preoperative opioid exposure were associated with increased respiratory-related, pain-related, and opioid-related readmissions after elective surgery. Even minimal preoperative opioid exposure was predictive of readmissions. Our findings emphasize the importance of screening patients prior to surgery and tailoring safe postoperative pain management plans for patients with varying levels of preoperative opioid exposure.
Supplementary Material
Acknowledgments
Sources of Support: Drs. Waljee, Englesbe and Brummett receive funding from the National Institute on Drug Abuse (RO1 DA042859), the Michigan Department of Health and Human Services (E20180672-00 Michigan DHHS - MA-2018 Master Agreement Program) as well as the Substance Abuse and Mental Health Administration (SAMHSA: E20180568-00 MA-2018 Master Agreement Program) and the Centers for Disease Control and Prevention (E20182818-00 MA-2018 Master Agreement Program). Dr. Englesbe receives salary support from Blue Cross Blue Shield of Michigan.
Footnotes
Disclosures: Dr. Brummett serves as a consultant for Heron Therapeutics.
REFERENCES
- 1.International Narcotics Control Board, Narcotic Drugs 2018: Estimated World Requirements for 2019, Statistics for 2017 (New York: United Nations, 2019), available at https://www.incb.org/incb/en/narcotic-drugs/Technical_Reports/narcotic_drugs_reports.html. [Google Scholar]
- 2.Han B, Compton WM, Blanco C, et al. Prescription opioid use, misuse, and use disorders in U.S. Adults: 2015 national survey on drug use and health. Ann Intern Med. 2017. DOI: 10.7326/M17-0865. [DOI] [PubMed] [Google Scholar]
- 3.Opioids in Medicare Part D: Concerns about Extreme Use and Questionable Prescribing. July 2019. Available at: https://oig.hhs.gov/oei/reports/oei-02-17-00250.pdf. Accessed July 31, 2019. [Google Scholar]
- 4.Gomes T, Tadrous M, Mamdani MM, et al. The Burden of Opioid-Related Mortality in the United States. JAMA Network Open. 2018. DOI: 10.1001/jamanetworkopen.2018.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montandon G, Slutsky AS. Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical End Point. Chest. 2019. DOI: 10.1016/j.chest.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 6.de Boer HD, Detriche O, Forget P. Opioid-related side effects: Postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Practice and Research: Clinical Anaesthesiology. 2017. DOI: 10.1016/j.bpa.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Roeckel LA, Le Coz GM, Gavériaux-Ruff C, et al. Opioid-induced hyperalgesia: Cellular and molecular mechanisms. Neuroscience. 2016. DOI: 10.1016/j.neuroscience.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 8.Hernandez-Boussard T, Graham LA, Desai K, et al. The fifth vital sign: post-operative pain predicts 30-day readmissions and subsequent emergency department visits. Ann Surg. 2017;266(3):516–524. DOI: 10.1097/SLA.0000000000002372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brix LD, Bjørnholdt KT, Thillemann TM, et al. Pain-related unscheduled contact with healthcare services after outpatient surgery. Anaesthesia. 2017. DOI: 10.1111/anae.13876. [DOI] [PubMed] [Google Scholar]
- 10.Cron DC, Englesbe MJ, Bolton CJ, et al. Preoperative opioid use is independently associated with increased costs and worse outcomes after major abdominal surgery. Ann Surg. 2017;265:695–701. [DOI] [PubMed] [Google Scholar]
- 11.Waljee JF, Cron DC, Steiger RM, et al. Effect of preoperative opioid exposure on healthcare utilization and expenditures following elective abdominal surgery. Ann Surg. 2017; 265:715–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hilliard PE, Waljee J, Moser S, et al. Prevalence of preoperative opioid use and characteristics associated with opioid use among patients presenting for surgery. JAMA Surg. 2018;153:929–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain N, Brock JL, Phillips FM, et al. Chronic preoperative opioid use is a risk factor for increased complications, resource use, and costs after cervical fusion. Spine J. 2018. DOI: 10.1016/j.spinee.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Petrick A, Brindle SA, Vogels E, et al. The readmission contradiction: toward clarifying common misconceptions about bariatric readmissions and quality improvement. Surg Obes Relat Dis. 2018. DOI: 10.1016/j.soard.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Hospital Readmissions Reduction Programs (HRRP). July 31, 2019. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed September 23, 2019.
- 16.Tsai TC, Joynt KE, Orav EJ, et al. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013. DOI: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jencks SF, Williams M V., Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009. DOI: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 18.Vu JV, Cron DC, Lee JS, et al. Classifying Preoperative Opioid Use for Surgical Care. Ann Surg. 2018. DOI: 10.1097/sla.0000000000003109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daoust R, Paquet J, Moore L, et al. Incidence and risk factors of long-term opioid use in elderly trauma patients. Ann Surg. 2018. DOI: 10.1097/SLA.0000000000002461. [DOI] [PubMed] [Google Scholar]
- 20.Makris UE, Abrams RC, Gurland B, et al. Management of persistent pain in the older patient: A clinical review. JAMA - Journal of the American Medical Association. 2014. DOI: 10.1001/jama.2014.9405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore BJ, Barrett ML. Case Study: Exploring How Opioid-Related Diagnosis Codes Translate From ICD-9-CM to ICD-10-CM [cup-us.ahrq.gov] April 24, 2017. Available at: https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp. Accessed July 22, 2019.
- 22.Mayhew M, DeBar LL, Deyo RA, et al. Development and Assessment of a Crosswalk Between ICD-9-CM and ICD-10-CM to Identify Patients with Common Pain Conditions. J Pain. 2019. DOI: 10.1016/j.jpain.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Centers for Disease Control and Prevention. Calculating total daily dose of opioids for safer dosage. Available at: https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed July 22, 2019.
- 24.Gan G, Ma C, Wu J. Data Clustering: Theory, Algorithms, and Applications. 2007. DOI: 10.1137/1.9780898718348. [DOI] [Google Scholar]
- 25.HCUP CCS. Healthcare Cost and Utilization Project (HCUP). March 2017. Agency for Healthcare Research and Quality, Rockville, MD. Available at: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed on July 1, 2019. [Google Scholar]
- 26.Ross ME, Wheeler LJ, Flink DM, et al. Preoperative opioid use in Gynecologic Oncology: A common comorbidity relevant to the perioperative period. Gynecol Oncol. 2019. DOI: 10.1016/j.ygyno.2019.03.156. [DOI] [PubMed] [Google Scholar]
- 27.Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee GC. Preoperative Opiate Use Independently Predicts Narcotic Consumption and Complications After Total Joint Arthroplasty. J Arthroplasty. 2017. DOI: 10.1016/j.arth.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 28.Kim Y, Cortez AR, Wima K, et al. Impact of Preoperative Opioid Use After Emergency General Surgery. J Gastrointest Surg. 2018. DOI: 10.1007/s11605-017-3665-x [DOI] [PubMed] [Google Scholar]
- 29.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Jt Surg - Ser A. 2011. DOI: 10.2106/JBJS.J.01473 [DOI] [PubMed] [Google Scholar]
- 30.Hills JM, Pennings JS, Archer KR, et al. Preoperative Opioids and 1-year Patient-reported Outcomes After Spine Surgery. Spine (Phila Pa 1976). 2019. DOI: 10.1097/BRS.0000000000002964. [DOI] [PubMed] [Google Scholar]
- 31.Weick J, Bawa H, Dirschl DR, Luu HH. Preoperative opioid use is associated with higher readmission and revision rates in total knee and total hip arthroplasty. J Bone Jt Surg - Am Vol. 2018. DOI: 10.2106/JBJS.17.01414. [DOI] [PubMed] [Google Scholar]
- 32.Jain N, Brock JL, Malik AT, Phillips FM, Khan SN. Prediction of Complications, Readmission, and Revision Surgery Based on Duration of Preoperative Opioid Use. J Bone Jt Surg. 2019. DOI: 10.2106/jbjs.18.00502. [DOI] [PubMed] [Google Scholar]
- 33.Dasinger EA, Graham LA, Wahl TS, et al. Preoperative opioid use and postoperative pain associated with surgical readmissions. American Journal of Surgery. 2019. DOI: 10.1016/j.amjsurg.2019.02.033 [DOI] [PubMed] [Google Scholar]
- 34.Jain N, Brock JL, Malik AT, et al. Prediction of Complications, Readmissions, and Revision Surgery Based on Duration of Preoperative Opioid Use. J Bone Jt Surg. 2019. DOI: 10.2106/jbjs.18.00502. [DOI] [PubMed] [Google Scholar]
- 35.Hayhurst CJ, Durieux ME. Differential Opioid Tolerance and Opioid-induced Hyperalgesia: A Clinical Reality. Anesthesiology. 2016. DOI: 10.1097/ALN.0000000000000963. [DOI] [PubMed] [Google Scholar]
- 36.Menendez ME, Ring D, Bateman BT. Preoperative Opioid Misuse is Associated With Increased Morbidity and Mortality After Elective Orthopaedic Surgery. Clin Orthop Relat Res. 2015. DOI: 10.1007/s11999-015-4173-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zutler M, C. Holty J-E. Opioids, Sleep, and Sleep-Disordered Breathing. Curr Pharm Des. 2011. DOI: 10.2174/138161211796197070. [DOI] [PubMed] [Google Scholar]
- 38.Wolfe RM, Pomerantz J, Miller DE, et al. Obstructive sleep apnea: Preoperative screening and postoperative care. Journal of the American Board of Family Medicine. 2016. DOI: 10.3122/jabfm.2016.02.150085. [DOI] [PubMed] [Google Scholar]
- 39.Ward EN, Quaye ANA, Wilens TE. Opioid use disorders: Perioperative management of a special population. Anesth Analg. 2018. DOI: 10.1213/ANE.0000000000003477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsui JI, Lira MC, Cheng DM, et al. Chronic pain, craving, and illicit opioid use among patients receiving opioid agonist therapy. Drug Alcohol Depend. 2016. DOI: 10.1016/j.drugalcdep.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Larson MJ, Paasche-Orlow M, Cheng DM, et al. Persistent pain is associated with substance use after detoxification: A prospective cohort analysis. Addiction. 2007. DOI: 10.1111/j.1360-0443.2007.01759.x. [DOI] [PubMed] [Google Scholar]
- 42.Desai K, Carroll I, Asch SM, et al. Utilization and effectiveness of multimodal discharge analgesia for postoperative pain management. J Surg Res. 2018;228:160–169. DOI: 10.1016/j.jss.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen LCL, Sing DC, Bozic KJ. Preoperative Reduction of Opioid Use Before Total Joint Arthroplasty. J Arthroplasty. 2016. DOI: 10.1016/j.arth.2016.01.068. [DOI] [PubMed] [Google Scholar]
- 44.McAnally H Rationale for and approach to preoperative opioid weaning: a preoperative optimization protocol. Perioper Med. 2017. DOI: 10.1186/s13741-017-0079-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hanna MN, Speed TJ, Shechter R, et al. An Innovative Perioperative Pain Program for Chronic Opioid Users: An Academic Medical Center’s Response to the Opioid Crisis. Am J Med Qual. 2019. DOI: 10.1177/1062860618777298 [DOI] [PubMed] [Google Scholar]
- 46.Vetter TR, Kain ZN. Role of the Perioperative Surgical Home in Optimizing the Perioperative Use of Opioids. Anesth Analg. 2017. DOI: 10.1213/ANE.0000000000002280 [DOI] [PubMed] [Google Scholar]
- 47.Uppal NK, Eisen D, Weissberger J, et al. Transfer of care of postsurgical patients from hospital to the community setting: Cross-sectional survey of primary care physicians. Am J Surg. 2015. DOI: 10.1016/j.amjsurg.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 48.Klueh MP, Sloss KR, Dossett LA, et al. Postoperative opioid prescribing is not my job: A qualitative analysis of care transitions. Surg (United States). 2019. DOI: 10.1016/j.surg.2019.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.