Abstract
We examined the trends in geographic variation in Medicare per capita spending and growth from 2007 to 2017 and found that the variation narrowed during this period. The difference in Medicare price- and risk-adjusted per capita spending between hospital referral regions (HRRs) in the top decile and those in the bottom decile decreased from $3,388 in 2007 to $2,916 in 2017—a reduction of $472, or 14 percent. The spending convergence occurred almost entirely between 2009 and 2014, during the early years of the Affordable Care Act (ACA). The highest-spending HRRs in 2007 had the lowest annual growth rates from 2007 to 2017, and the lowest-spending HRRs in 2007 had the highest annual growth rates. We also found that a greater supply of postacute care providers, especially hospice providers, significantly predicted lower spending growth across HRRs after the implementation of the ACA.
Medicare per capita spending varies widely across geographic regions in the US,1–3 even after geographic differences in health services prices and patient health are accounted for.4–7 Without evidence that Medicare beneficiaries in high-spending regions have better health outcomes than those in low-spending regions,8–10 the additional spending in those regions has been regarded as a reflection of wasteful utilization.1 Although much research has been done to understand the sources of this variation,4,5,11–13 less is known about the overall trends in this variation in the past decade, how growth in Medicare per capita spending differs between high- and low-spending regions over time, or specific regional factors associated with spending growth.
In the past decade a variety of delivery and provider payment reforms, such as accountable care organizations (ACOs) and bundled payment, have been implemented to contain health care spending and improve efficiency in care delivery, primarily through changing provider incentives and behaviors.14,15 These reforms have great potential to reduce geographic variation in Medicare spending if they can have a greater impact on provider efficiency in high-spending regions relative to low-spending regions and can eliminate unnecessary health care use. However, previous studies found that delivery and payment innovations have made less progress in traditionally high-spending regions compared with low-spending regions. For example, Medicare ACOs have lower penetration in hospital referral regions (HRRs) in the southern US, which tends to be a region with higher per capita spending.16 Hospitals in southern and rural areas also are less likely to participate in ACOs or other delivery and payment innovations.17 Therefore, it is unclear whether Medicare geographic variation narrowed after the wide implementation of care delivery and payment innovations.
Using HRR-level data for 2007–17, this study provides an up-to-date analysis of the trends in geographic variation in Medicare per capita spending, documents variation in growth patterns across HRRs, and examines HRR-level beneficiary and market characteristics associated with the annual growth rate in Medicare per capita spending over the course of a decade. Findings of this study will further inform debates regarding effective policies for reducing unnecessary utilization and improving the value of health care.
Study Data And Methods
Data And Study Population
Our primary analysis used the 2007–17 Medicare Geographic Variation Public Use File from the Centers for Medicare and Medicaid Services (CMS).18 This data source includes beneficiaries with both Part A and Part B coverage who enrolled in Medicare’s fee-for-service program. Beneficiaries who were enrolled at any point over the course of a year in a Medicare Advantage plan or in Part A only or Part B only were excluded from the sample.18 Consistent with previous studies of Medicare geographic variation, we used the Geographic Variation Public Use File at the HRR level. All 306 HRRs were included in this study. We combined these data with health resources supply data from the Area Health Resources File from the Health Resources and Services Administration and the Provider of Services file from CMS to examine supply factors associated with differences in rates of spending growth across HRRs.
Analyses
Our primary measure of spending was price- and risk-adjusted per capita total Medicare spending at the HRR level from the Geographic Variation Public Use File. This measure included spending on all Medicare Parts A and B services and accounted for geographic differences in prices (for example, labor costs) and beneficiaries’ health status, measured by CMS Hierarchical Condition Categories (CMS HCC) scores.19 Geographic variation in this spending measure therefore reflects geographic differences in factors other than price or beneficiaries’ health status, which could include supply of health care providers, provider treatment intensity, and patient preference.1,4,5,12
We examined trends in average Medicare per capita spending for both high-spending and low-spending HRRs and the ratio between them from 2007 to 2017. Consistent with previous literature, we defined high-spending regions as HRRs in the top 10 percent in terms of price- and risk-adjusted total Medicare per capita spending in a year, and low-spending regions as HRRs in the bottom 10 percent.1 The groups of high- and low-spending HRRs therefore may differ from year to year, reflecting changes in an HRR’s position in terms of Medicare per capita spending relative to other HRRs. We also examined geographic variation in Medicare per capita spending by care setting (for example, physician, outpatient, and inpatient) between high- and low-spending HRRs. All spending measures were inflation adjusted using the Consumer Price Index for Medical Care from the Bureau of Labor Statistics in 2017 dollars.
To understand the trends in geographic variation over time, we analyzed variation in growth rates of Medicare per capita spending across HRRs for the entire study period, 2007–17, as well as for subperiods. We calculated the compound annualized growth rates for the entire period and the subperiods by dividing spending in the end year (for example, 2017) by spending in the start year (for example, 2007), raising the ratio to the power of 1 divided by number of years in between (for example, 10) and subtracting 1 from the result.20 We identified the top ten and bottom ten HRRs in terms of the compound annualized growth rates and their spending deciles in 2007 and 2017.
Finally, we used linear regressions to examine the association between baseline HRR-level beneficiary and market characteristics and subsequent growth rates. Beneficiary characteristics from the Geographic Variation Public Use File included average age; shares of beneficiaries who were female, African American, Hispanic, or eligible for both Medicare and Medicaid; and average CMS HCC score. Market characteristics included Medicare Advantage penetration and the number of each of the following health care providers per 1,000 population: primary care physicians, hospital beds, skilled nursing facility beds, home health agencies, ambulatory surgery centers, and registered nurses employed by hospices. The latter is arguably a more granular measure of hospice capacity than number of hospices. Using an established method, we converted these county-level characteristics to the HRR level.21 All regressions used heteroscedasticity-robust standard errors and were weighted by the number of fee-for-service beneficiaries in each HRR. We used Stata, version 14, for all analyses.
Sensitivity Analysis
We performed a sensitivity analysis using Medicare per capita spending adjusted for price, age, sex, and race from the Dartmouth Atlas of Health Care.22–24 Many risk-adjustment methods, including CMS HCC score, rely on the claims data-based diagnosis codes of comorbidities. In addition to capturing patient health risk, these scores may reflect the variation in treatment or diagnosis intensity of providers across regions.25,26 Therefore, using the price- and risk-adjusted spending measure may under-estimate the extent of variation across HRRs and cause bias in analyses. To address this potential issue, we repeated our analysis using Medicare per capita spending that adjusted for price and basic patient demographics without accounting for patient health risk. These data were available from 2007 to 2016 from the Dartmouth Atlas of Health Care.22–24
Limitations
Our study had several limitations. First, the Geographic Variation Public Use File did not include Medicare Part D spending, which may lead to an underestimation of the geographic variation in Medicare spending. Second, the Geographic Variation Public Use File also did not include spending in Medicare Advantage plans, so the results represent only geographic variation among Medicare fee-for-service beneficiaries. Third, by focusing on HRRs as the geographic unit, we were unable to examine variation in spending across smaller geographic units, such as hospital service areas. Finally, our analysis does not provide causal interpretation regarding the factors that drive potentially differential spending growth across HRRs.
Study Results
Trends In Geographic Variation In Medicare Spending
The gap in price- and risk-adjusted Medicare per capita spending between high- and low-spending HRRs narrowed between 2007 and 2017 in terms of both the ratio of and the absolute differences in dollar amounts (exhibit 1). The dollar difference in mean spending between high- and low-spending HRRs was $3,388 in 2007 compared with $2,916 in 2017, representing a reduction of $472, or 14 percent. The ratio in mean spending between high- and low-spending HRRs declined from 1.42 in 2007 to 1.33 in 2017, or 9 percentage points. These reductions were uneven across the study period: The dollar-amount difference between high- and low-spending HRRs actually widened somewhat from 2007 to 2009, followed by a steady decline from 2009 to 2014, before stabilizing from 2014 to 2017. Overall, there was continuous decline in the ratio of spending between high- and low-spending HRRs from 2007 to 2017 (except from 2008 to 2009 and from 2016 to 2017).
Exhibit 1. Trends in geographic variation in Medicare per capita spending, by hospital referral region (HRR), 2007–17.
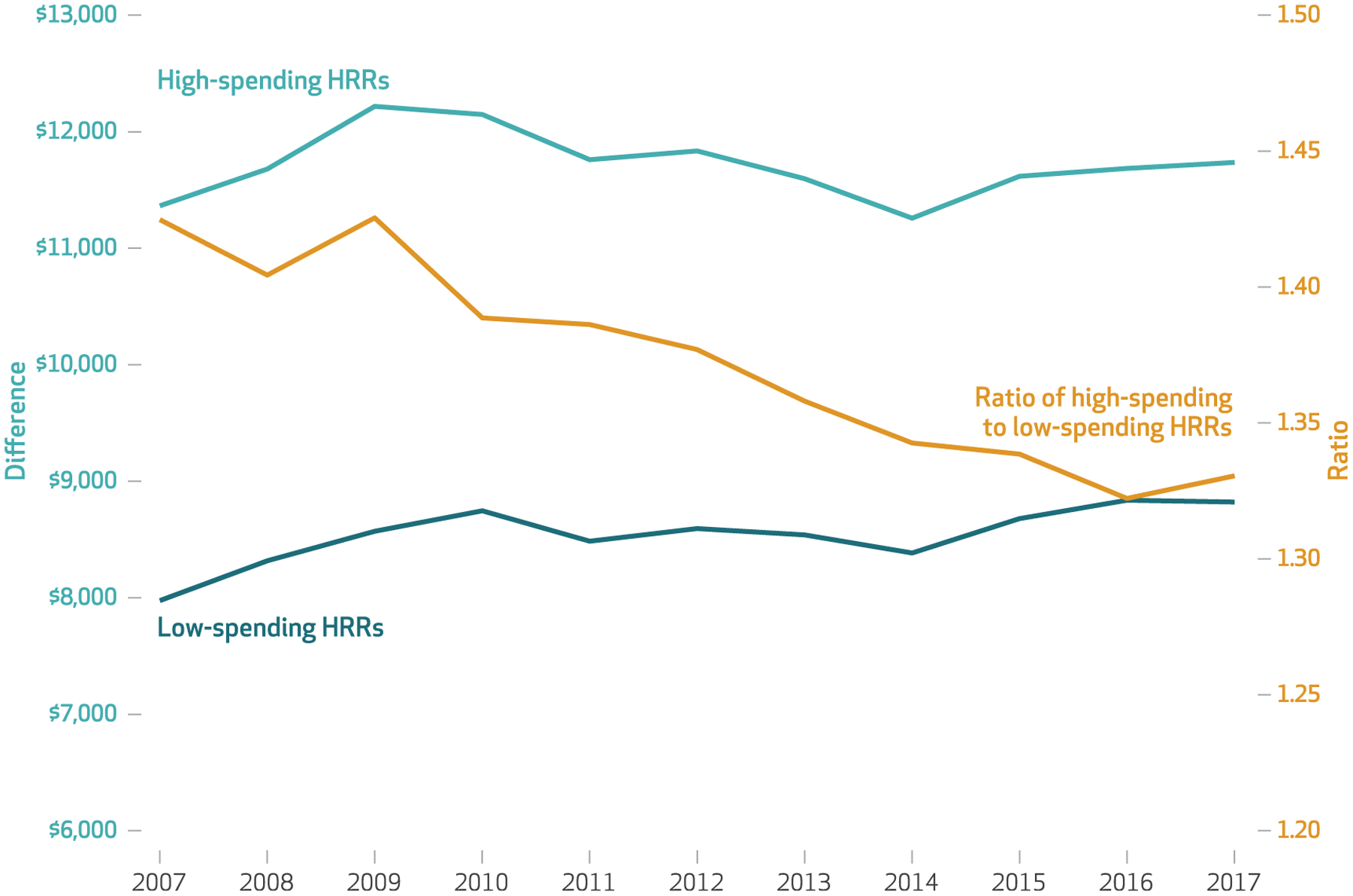
SOURCE Authors’ analysis of data for 2007–17 from the Medicare Geographic Variation Public Use File (Centers for Medicare and Medicaid Services). NOTES High-spending HRRs were in the top 10 percent of price- and risk-adjusted total Medicare per capita spending each year, and low-spending HRRs were in the bottom 10 percent.
The trends in geographic variation differed by care setting (see online appendix exhibit 1).27 The gap in per capita spending on physician ($178, or an 18 percent reduction), inpatient ($319, or a 52 percent reduction), and postacute ($224, or a 15 percent reduction) care narrowed between high- and low-spending HRRs from 2007 to 2017, whereas the gap in outpatient per capita spending was relatively stable. These findings were consistent when measured by ratios between high- and low-spending HRRs. The variation in spending on hospice care was stable in terms of differences in dollar amounts, but it narrowed in terms of ratios between high- and low-spending HRRs.
Variation In Spending Growth Rates Across Regions
The average ratio in 2017 to 2007 Medicare per capita spending across HRRs was 1.065, as illustrated in exhibit 2 by the slope of the fitted line in the scatterplot correlating HRR-level 2017 (y axis) and 2007 (x axis) spending. The HRRs above the fitted line experienced faster spending growth than the average level across all HRRs, and those below the line experienced slower growth. The highest-spending HRRs in 2007 (those with per capita spending above $11,000; for example, Miami, Florida, and McAllen and Harlingen, Texas) almost all experienced slower growth than the national average. In contrast, almost all of the lowest-spending HRRs in 2007 (those with spending lower than $8,500; for example, Honolulu, Hawaii, and San Jose and San Francisco, California) had faster growth than the national average. Despite this, the lowest-spending HRRs in 2007 remained the lowest in 2017, whereas some of the highest spending HRRs in 2007 moved down in their relative rankings in 2017, replaced by HRRs that had moderately high spending in 2007.
Exhibit 2. Relationship between 2007 and 2017 price- and risk-adjusted Medicare per capita spending, by hospital referral region (HRR).
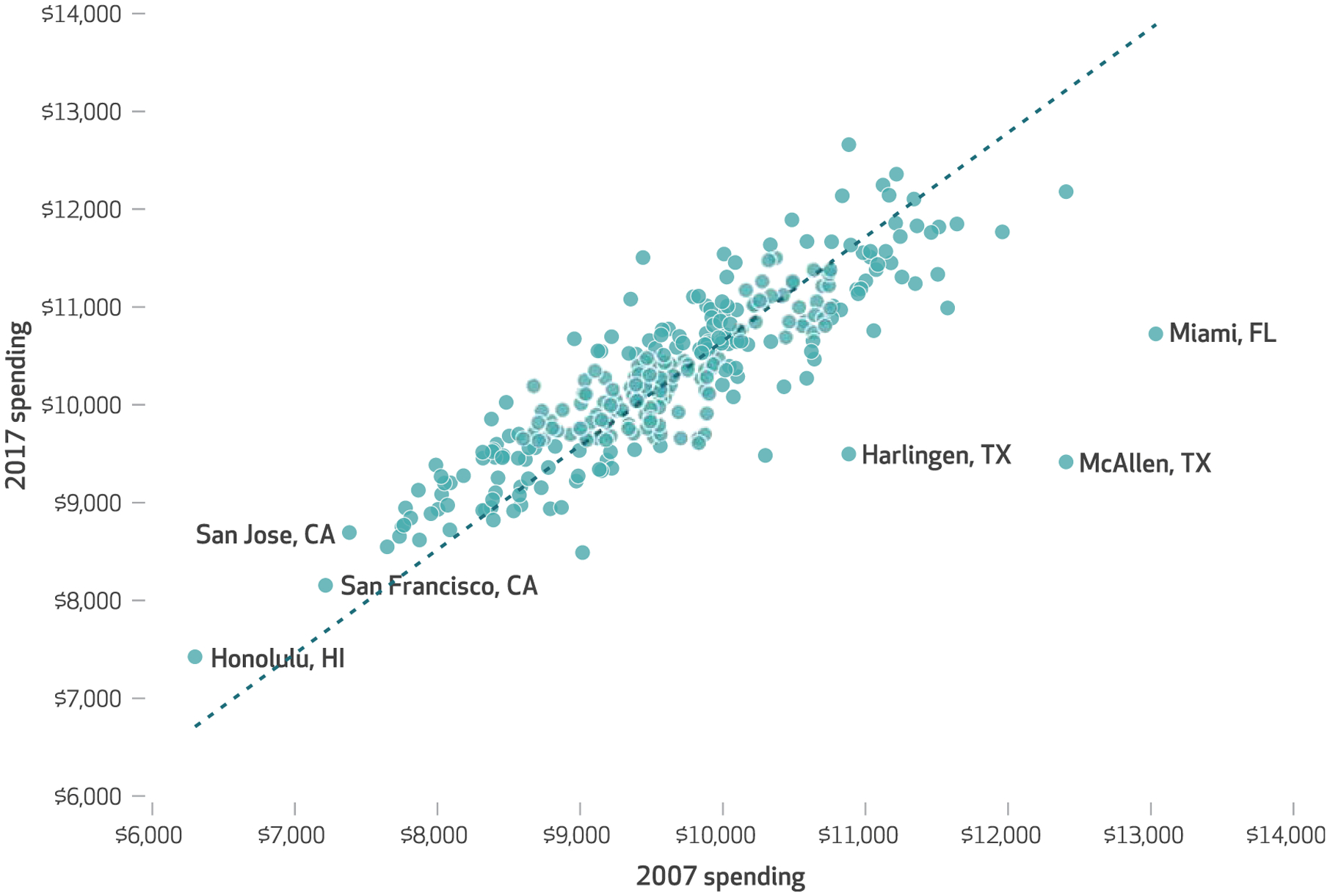
SOURCE Authors’ analysis of data for 2007–17 from the Medicare Geographic Variation Public Use File (Centers for Medicare and Medicaid Services). NOTE Each point in the scatterplot represents an HRR.
These patterns are further illustrated in exhibit 3, which examines compound annualized growth rates. Among the ten HRRs with the highest annual growth rates between 2007 and 2017, nine were in the bottom five deciles in 2007 and four were in the lowest decile in 2007. Two of these ten HRRs remained in the lowest decile from 2007 to 2017 (Honolulu, Hawaii, and San Jose, California), and two HRRs went to the top decile in 2017, including Idaho Falls, Idaho (fifth decile in 2007), and Wichita Falls, Texas (ninth decile in 2007).
Exhibit 3.
Hospital referral regions (HRRs) with the highest and lowest annual growth rate in price- and risk-adjusted Medicare per capita spending between 2007 and 2017
| HRRs by compound annualized growth rate | Deciles of Medicare per capita spending | Compound annualized growth rate (%) | |
|---|---|---|---|
| 2007 | 2017 | ||
| TOP 10 | |||
| Idaho Falls, ID | 5 | 10 | 2.0 |
| Ventura, CA | 3 | 7 | 1.8 |
| Fort Smith, AR | 4 | 9 | 1.7 |
| Roanoke, VA | 2 | 4 | 1.7 |
| Honolulu, HI | 1 | 1 | 1.7 |
| San Jose, CA | 1 | 1 | 1.6 |
| Charlottesville, VA | 1 | 4 | 1.6 |
| Newport News, VA | 2 | 5 | 1.6 |
| Santa Rosa, CA | 1 | 2 | 1.6 |
| Wichita Falls, TX | 9 | 10 | 1.5 |
| BOTTOM 10 | |||
| McAllen, TX | 10 | 2 | −2.7 |
| Miami, FL | 10 | 8 | −1.9 |
| Harlingen, TX | 9 | 2 | −1.4 |
| New Orleans, LA | 8 | 2 | −0.8 |
| Wausau, WI | 3 | 1 | −0.6 |
| Baton Rouge, LA | 10 | 8 | −0.5 |
| Baltimore, MD | 10 | 8 | −0.3 |
| Odessa, TX | 9 | 5 | −0.3 |
| Saginaw, MI | 8 | 5 | −0.2 |
| Traverse City, MI | 6 | 3 | −0.2 |
SOURCE Authors’ analysis of data from the Medicare Geographic Variation Public Use File (Centers for Medicare and Medicaid Services) and Area Health Resources File (Health Resources and Services Administration).
Among the ten HRRs with the slowest (and negative) annual spending growth between 2007 and 2017, nine were in the top five deciles in 2007, with four in the top decile in 2007. All four of these HRRs fell below the top decile in 2017; of those, McAllen, Texas, had the lowest spending growth (−2.7 percent) and the biggest drop in deciles, going from the tenth decile in 2007 to the second in 2017.
Characteristics Associated With Spending Growth
To further examine regional factors associated with variation in spending growth across HRRs, exhibit 4 shows multivariable regression results predicting HRR-level growth rates in per capita spending using HRR-level beneficiary and market characteristics. To account for the temporal changes in growth patterns reported in exhibit 1, we divided the eleven-year study period into three subperiods: 2007–09 (period 1), 2009–14 (period 2), and 2014–17 (period 3). We conducted separate analyses for each subperiod. For each subperiod, we used the HRR characteristics measured in the first, baseline year to predict the compound annualized spending growth rate during the subperiod. To accompany the regression results, appendix exhibit 2 shows summary statistics of the predictors for each subperiod by high- and low-spending HRRs.27
Exhibit 4.
Association between baseline hospital referral region (HRR) characteristics and annual growth rate in price- and risk-adjusted Medicare per capita spending, by subperiod, 2007–17
| Coefficient | |||
|---|---|---|---|
| 2007–09 | 2009–14 | 2014–17 | |
| BENEFICIARY CHARACTERISTICS | |||
| Mean age | 0.041 | 0.040 | 0.081 |
| Percent female | 0.010 | 0.039 | −0.027 |
| Percent African American | 0.005 | −0.009 | −0.011 |
| Percent Hispanic | −0.015 | −0.005 | 0.005 |
| Percent dual-eligible | 0.016 | −0.004 | 0.066**** |
| Mean CMS HCC score | 0.705 | −2.474*** | −4.343*** |
| MARKET CHARACTERISTICS | |||
| Percent average Medicare Advantage enrollment rate | 0.010* | −0.005 | −0.011 |
| Per 1,000 population: | |||
| Number of primary care physicians | −0.340 | −0.332 | 0.101 |
| Number of hospital beds | −0.080 | 0.001 | 0.138** |
| Number of skilled nursing facility beds | −0.151**** | 0.008 | 0.030 |
| Number of home health agencies | 1.099 | −9.753**** | −1.283 |
| Number of ambulatory surgery centers | 8.316 | −10.225* | −0.834 |
| Number of RNs employed by hospices | −0.578 | −0.887** | −0.016** |
SOURCE Authors’ analysis of data from the Medicare Geographic Variation Public Use File and Provider of Services File (Centers for Medicare and Medicaid Services) and the Area Health Resources File (Health Resources and Services Administration). NOTES N = 306 HRRs. This exhibit presents the results of multivariable regressions. Regressions are weighted by the number of fee-for-service beneficiaries in each HRR. See the text for more details. CMS HCC is Centers for Medicare and Medicaid Services Hierarchical Condition Categories. RN is registered nurse.
p < 0:10
p < 0:05
p < 0:01
p < 0:001
BENEFICIARIES: Few beneficiary characteristics were significantly associated with annual spending growth rates. The percentage of dual-eligible patients was associated with a significantly higher growth rate in period 3. A higher mean CMS HCC score was associated with lower growth rates in periods 2 and 3, reflecting the same general pattern documented earlier. Appendix exhibit 2 shows that areas with higher spending, which also had generally sicker beneficiaries, were better able to curb spending growth.27
MARKETS: Several market or supply characteristics, especially those related to postacute care, significantly predicted spending growth. In period 1, HRRs with more skilled nursing facility beds had significantly lower spending growth. The number of home health agencies and number of registered nurses employed by hospices per 1,000 population were significantly associated with lower spending growth in period 2. In period 3, HRRs with more hospital beds per 1,000 population had significantly higher spending growth, and those with more hospice-employed nurses per 1,000 population had significantly lower spending growth (exhibit 4). These relationships provide a plausible, although by no means conclusive, explanation for the slower spending growth in high-spending HRRs compared with low-spending HRRs post-2010, as the former had generally higher numbers of postacute care providers per capita than the latter (appendix exhibit 2).27
Sensitivity Analysis Results
Using the Dartmouth Atlas’s Medicare per capita spending data adjusted for price and basic demographics instead of CMS HCC scores, we obtained largely consistent results in terms of trends in geographic variation in Medicare spending over time, by subperiod, by care setting, and by key beneficiary and market characteristics associated with sub-period-specific spending growth across HRRs (appendix exhibits 3–8).27 One notable difference from the previous results was that the HRRs with the highest spending (those spending more than $12,000), despite experiencing some of the slowest growth rates from 2007 to 2016, remained in the top decile in 2016 in terms of per capita spending (appendix exhibit 4).27 These included Miami, Florida; McAllen and Harlington, Texas; and Monroe, Louisiana (appendix exhibit 7).27 This could suggest additional unnecessary spending, reflected in more aggressive diagnoses and potential upcoding in those regions. Another difference was that more HRRs with spending below the median in 2007 experienced a lower-than-average growth rate (1.055) from 2007 to 2016, as illustrated by the dots below the fitted line in appendix exhibit 4.27
Discussion
We found that variation in Medicare per capita spending across HRRs narrowed from 2007 to 2017. The difference in price- and risk-adjusted per capita spending between high- and low-spending HRRs decreased from $3,388 in 2007 to $2,916 in 2017, representing a reduction of $472, or 14 percent. This change was primarily driven by a faster rate of decrease from 2010 to 2014 and a slower rate of increase from 2014 to 2017 in mean Medicare per capita spending among high- relative to low-spending HRRs. These patterns are consistent with previous studies finding a substantial slowdown in overall health care spending growth between 2010 and 2014 and accelerated growth after 2014, both of which have been at least partially attributed to specific provisions of the ACA implemented before and after 2014.28,29
Accordingly, we found that high-spending HRRs in 2007 had the lowest growth rates during the study period, whereas low-spending HRRs in 2007 had the highest growth rates. Finally, we found that a greater supply of postacute care providers at baseline, such as home health agencies and hospice providers, was associated with lower growth in Medicare per capita spending in the subsequent period. Findings were largely consistent when we used Medicare per capita spending adjusted only for price and basic demographics.
Overall, the trend in geographic variation in Medicare spending between 2007 and 2017 is encouraging. The decline in mean Medicare per capita spending between 2010 and 2014 among both high- and low-spending HRRs, with a steeper decline among high-spending HRRs, may indicate improved efficiency in health care delivery and decreased unnecessary health care use that previously contributed to well-documented geographic variation in spending. These changes were driven mostly by reductions in geographic variation in spending among physician, inpatient, and postacute care settings. Early provisions of the ACA targeting acute and postacute care, including a reduction in the annual payment increase among providers, Medicare antifraud activities with stiffer penalties, and other delivery and payment reforms in acute care settings (for example, the Hospital Readmissions Reduction Program), are likely to have contributed to these results.28,30
The fact that the gap between high- and low-spending HRRs stabilized without an increase after 2014 may suggest that factors associated with earlier reduction in per capita spending variation across regions remained in effect. However, it also suggests that more recent policy has been less successful than some of the early ACA provisions in further reducing geographic variation in Medicare per capita spending. For instance, the strong negative association between home health resources and growth rate between 2009 and 2014 likely reflects the effect of several ACA provisions that specifically targeted postacute settings, including payment cuts and more stringent requirements for home health care.28 The fact that this association was no longer significant after 2014 could suggest that these policies may have approached their maximum impact in terms of slowing down the growth rate in postacute care settings. Although this study was not designed to draw any causal conclusions, the largely stagnant geographic variation in Medicare per capita spending after 2014 warrants further investigation.
The beneficiary and market characteristics associated with spending growth across HRRs provide further insight into the plausible driving forces behind geographic variation in spending and the changes therein. Medicaid expansion and the Medicaid primary care fee bump likely explain the positive association between share of dual-eligible patients and spending growth after 2014, given improved health care access and increased utilization in this population.31–33 This may be particularly relevant in low-spending areas, which had a higher average percentage of dual-eligible patients compared with high-spending areas. In addition, compared with areas with sicker beneficiaries at baseline (as measured by higher CMS HCC scores), areas with healthier beneficiaries had higher growth rates after 2009, which may at least partially be attributed to the fact that providers in those areas were financially rewarded for keeping patients healthy and spending low. However, further investigations are needed to examine the mechanisms behind the inverse relationship between CMS HCC scores and spending growth.
Our finding that hospital capacity was positively related to spending growth after 2014 may indicate that utilization was higher in regions with more hospital bed availability during this period. It is also possible that regions with more hospital beds have large, consolidated health systems created by the rapid increase in vertical and horizontal consolidation in health care markets that took place after the ACA was implemented. Such consolidations largely accelerated after 201134 and were associated with increased spending or even higher spending growth rates,35 although it is difficult to draw any definitive conclusion from one significant coefficient, given the large number of coefficients estimated. In comparison, the negative association between hospice capacity and spending growth rate was observed for both subperiods after 2009 and may suggest that the effective use of palliative care and hospice benefits could offer a lower-cost alternative for patients at end of life, who account for a large proportion of Medicare spending.36 Recent literature suggests that physicians’ beliefs explain much of the geographic variation in end-of-life care spending, whereas patients’ preferences explain little.12 Al-tering these beliefs by further reducing incentives for intensive care and encouraging the use of palliative care in hospice settings may be a key to further reducing geographic variation in Medicare spending and producing health care cost savings in the near future.
Geographic variation in Medicare per capita spending has been of interest to policy makers and researchers for decades, raising hopes of generating cost savings by lowering Medicare costs in high-spending regions without compromising quality and outcomes. To date, much attention has been focused on examining the magnitude and sources of the cross-sectional variation. Relatively little has been done to analyze the change in the variation, especially in more recent years. In this study we analyzed trends in the variation in Medicare per capita spending and the differential growth rates among high- and low-spending regions and provided tentative evidence of the potential drivers of the trends. More research is warranted to quantify the impact of specific reforms on narrowing of geographic variation in health care spending and to derive policy solutions to further reduce such variation.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health (Grant No. K99AG064030 to Yongkang Zhang; Grant No. K01AG066946 to Jing Li). Li was also supported by a Weill Cornell Medicine JumpStart Career Development Award. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Weill Cornell Medicine.
Contributor Information
Yongkang Zhang, Department of Population Health Sciences at Weill Cornell Medical College, in New York, New York..
Jing Li, Department of Population Health Sciences at Weill Cornell Medical College..
NOTES
- 1.Newhouse JP, Garber AM, Graham RP, McCoy MA, Mancher M, Kibria A, editors. Variation in health care spending: target decision making, not geography. Washington (DC): National Academies Press; 2013. [PubMed] [Google Scholar]
- 2.Newhouse JP, Garber AM. Geographic variation in health care spending in the United States: in-sights from an Institute of Medicine report. JAMA. 2013;310(12):1227–8. [DOI] [PubMed] [Google Scholar]
- 3.Newhouse JP, Garber AM. Geographic variation in Medicare services. N Engl J Med. 2013;368(16): 1465–8. [DOI] [PubMed] [Google Scholar]
- 4.Finkelstein A, Gentzkow M,Williams H. Sources of geographic variation in health care: evidence from patient migration. Q J Econ. 2016;131(4): 1681–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zuckerman S, Waidmann T, Berenson R, Hadley J. Clarifying sources of geographic differences in Medicare spending. N Engl J Med. 2010;363(1):54–62. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood). 2010;29(3): 537–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skinner J. Causes and consequences of regional variations in health care. In: Pauly MV, McGuire TG, Barros PP, editors. Handbook of health economics. Amsterdam: North-Holland/Elsevier; 2011. p. 45–93. [Google Scholar]
- 8.Fowler FJ Jr, Gallagher PM, Anthony DL, Larsen K, Skinner JS. Relationship between regional per capita Medicare expenditures and patient perceptions of quality of care. JAMA. 2008;299(20):2406–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4): 288–98. [DOI] [PubMed] [Google Scholar]
- 10.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff (Millwood). 2004;(Suppl Web Exclusives):W4–184–97. DOI: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- 11.Sirovich BE, Gottlieb DJ, Welch HG, Fisher ES. Regional variations in health care intensity and physician perceptions of quality of care. Ann Intern Med. 2006;144(9):641–9. [DOI] [PubMed] [Google Scholar]
- 12.Cutler D, Skinner JS, Stern AD, Wennberg D. Physician beliefs and patient preferences: a new look at regional variation in health care spending. Am Econ J Econ Policy. 2019;11(1):192–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baker LC, Bundorf MK, Kessler DP. Patients’ preferences explain a small but significant share of regional variation in Medicare spending. Health Aff (Millwood). 2014;33(6): 957–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berwick DM. Launching accountable care organizations—the proposed rule for the Medicare Shared Savings Program. N Engl J Med. 2011; 364(16):e32. [DOI] [PubMed] [Google Scholar]
- 15.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366(12):1075–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muhlestein D, Bleser WK, Saunders RS, Richards R, Singletary E, McClellan MB. Spread of ACOs and value-based payment models in 2019: gauging the impact of path-ways to success. Health Affairs Blog [blog on the Internet]. 2019. October 21 [cited 2020 Sep 9]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20191020.962600/full/ [Google Scholar]
- 17.Colla CH, Lewis VA, Tierney E, Muhlestein DB. Hospitals participating in ACOs tend to be large and urban, allowing access to capital and data. Health Aff (Millwood). 2016; 35(3):431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services. Medicare geographic variation [Internet]. Baltimore (MD): CMS; 2019. November 27 [cited 2020 Sep 9]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/index [Google Scholar]
- 19.Pope GC, Kautter J, Ellis RP, Ash AS, Ayanian JZ, Lezzoni LI, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004; 25(4):119–41. [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper Z, Craig S, Gray C, Gaynor M, Van Reenen J. Variation in health spending growth for the privately insured from 2007 to 2014. Health Aff (Millwood). 2019;38(2):230–6. [DOI] [PubMed] [Google Scholar]
- 21.Baicker K, Chandra A. Understanding agglomerations in health care. In: Glaeser E, editor. Agglomeration economics. Chicago (IL): University of Chicago Press; 2010. p. 211–36. [Google Scholar]
- 22.Dartmouth Atlas of Health Care. General atlas rates [Internet]. Lebanon (NH): Dartmouth Atlas; [cited 2020 Sep 29]. Available from: https://atlasdata.dartmouth.edu/downloads/general [Google Scholar]
- 23.Chernew ME, Sabik LM, Chandra A, Gibson TB, Newhouse JP. Geographic correlation between large-firm commercial spending and Medicare spending. Am J Manag Care. 2010;16(2):131–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Adesoye T, Kimsey LG, Lipsitz SR, Nguyen LL, Goodney P, Olaiya S, et al. Geographic variation in Medicare and the military healthcare system. Am J Manag Care. 2017; 23(8):e259–64. [PubMed] [Google Scholar]
- 25.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional variations in diagnostic practices. N Engl J Med. 2010; 363(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finkelstein A, Gentzkow M, Hull P, Williams H. Adjusting risk adjustment—accounting for variation in diagnostic intensity. N Engl J Med. 2017;376(7):608–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. To access the appendix, click on the Details tab of the article online.
- 28.White C, Cubanski J, Neuman T. How much of the Medicare spending slowdown can be explained? Insights and analysis from 2014 [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2014. December 17 [cited 2020 Sep 8]. Available from: https://www.kff.org/report-section/how-much-of-the-medicare-spending-slowdown-can-be-explained-issue-brief/ [Google Scholar]
- 29.Martin AB, Hartman M, Benson J, Catlin A, National Health Expenditure Accounts Team. National health spending in 2014: faster growth driven by coverage expansion and prescription drug spending. Health Aff (Millwood). 2016;35(1):150–60. [DOI] [PubMed] [Google Scholar]
- 30.Grabowski DC, Huckfeldt PJ, Sood N, Escarce JJ, Newhouse JP. Medicare postacute care payment reforms have potential to improve efficiency of care, but may need changes to cut costs. Health Aff (Millwood). 2012; 31(9):1941–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med. 2016;176(10):1501–9. [DOI] [PubMed] [Google Scholar]
- 32.Polsky D, Richards M, Basseyn S, Wissoker D, Kenney GM, Zuckerman S, et al. Appointment availability after increases in Medicaid payments for primary care. N Engl J Med. 2015;372(6):537–45. [DOI] [PubMed] [Google Scholar]
- 33.Li J, Pesko MF, Unruh MA, Jung H-Y. Effect of the Medicaid primary care rate increase on prenatal care utilization among Medicaid-insured women. Matern Child Health J. 2019;23(11):1564–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nikpay SS, Richards MR, Penson D. Hospital-physician consolidation accelerated in the past decade in cardiology, oncology. Health Aff (Millwood). 2018;37(7):1123–7. [DOI] [PubMed] [Google Scholar]
- 35.McWilliams JM, Chernew ME, Zaslavsky AM, Hamed P, Landon BE. Delivery system integration and health care spending and quality for Medicare beneficiaries. JAMA Intern Med. 2013;173(15):1447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duncan I, Ahmed T, Dove H, Max-well TL. Medicare cost at end of life. Am J Hosp Palliat Care. 2019;36(8): 705–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


