Abstract
Cumulative evidence supports the association between perceived childhood neglect and adulthood psychological and physical health. To date, pathways mediating this association remain largely unknown, though other evidence suggests that negative patterns of appraisal, including injustice perception related to pain, may be shaped by prior adverse social experiences. Consequently, the current study examined perceived injustice about chronic pain as a possible factor connecting childhood neglect and pain-related outcomes, given its relevance for both adaptation to chronic pain and to prior adverse life experiences. Patients (n = 742) visiting a tertiary pain clinic completed a survey administered via the Collaborative Health Outcomes Information Registry. Path modeling analyses were used to examine perceived injustice as a mediator of the relationships between childhood neglect and affective distress and physical function, after controlling for pain intensity and pain catastrophizing. Patients endorsing childhood neglect reported higher levels of perceived injustice and worse affective distress and physical function. Further, inclusion of perceived injustice as a mediator fully accounted for the relationship between neglect and current levels of physical function, and accounted for a significant proportion of the relationship between neglect and current levels of affective distress. These preliminary findings suggest that perceived injustice appears to be a more proximal factor by which prior experiences of neglect may adversely affect adaptation to chronic pain. Given the single-item assessment of childhood neglect and cross-sectional nature of the current findings, further research may focus on replicating these findings in longitudinal studies with validated measures and examining other adverse social experiences (e.g., abuse, social disparities) that may contribute to injustice perception and poor pain-related outcomes.
Keywords: Childhood neglect, Perceived injustice, Chronic pain, Pain catastrophizing, Affective distress, Physical function
Childhood maltreatment, defined as childhood abuse and neglect, is associated with chronic pain in adulthood (Davis, Luecken, & Zautra, 2005; Norman et al., 2012), and is reported by up to 69% of patients with various chronic pain conditions (Bohn, Bernardy, Wolfe, & Häuser, 2013; Khandker, Brady, Stewart, & Harlow, 2014; Tietjen et al., 2010b, c). Research has paid less attention to childhood neglect as a health risk factor compared to childhood sexual and physical abuse (Norman et al., 2012). Child neglect is defined as failure to meet a child’s basic needs, including food, health care, supervision, education, and safety (Norman et al., 2012). As expected, child neglect is linked to family environment factors such as poverty, large family size, parental separation, domestic violence, crimes, and parents’ substance use (Brown, Cohen, Johnson, & Salzinger, 1998; Dong et al., 2004). Similar to research findings on other forms of maltreatment (e.g., physical abuse, emotional abuse) (Davis et al., 2005; Norman et al., 2012), studies find that childhood neglect is associated with an increased risk of multiple adulthood health problems including chronic pain (Goodwin & Stein, 2004; Norman et al., 2012) and higher health care costs (Walker et al., 1999). In patients with chronic pain, childhood neglect is associated with worse health status as a flattened daytime cortisol pattern, higher daily pain ratings, and more symptoms of depression and anxiety have been observed in those who endorse childhood neglect (Yeung, Davis, & Ciaramitaro, 2015). Notably, among adult migraineurs, those who endorse childhood neglect are more likely to endorse chronic than episodic migraines, and greater emotional distress (Tietjen et al., 2010a, b, c). Hence, identifying modifiable factors linking childhood neglect with current indicators of health in adulthood remains a significant yet unanswered research question. Therefore, the current study purports to present preliminary results on the relationship between perceived childhood neglect and psychosocial and physical dysfunction among adult patients seeking treatment for chronic pain conditions, as well as to identify potential factors that may connect distal influences such as childhood neglect with more immediate indicators of adjustment to chronic pain.
One potential area of inquiry concerns cognitive appraisals, which have been shown to have significant implications for adjustment to chronic pain (Edwards, Cahalan, Mensing, Smith, & Haythornthwaite, 2011; McParland & Eccleston, 2013; Sturgeon & Zautra, 2012; Sullivan et al., 2008) and appear to be shaped by adverse life experiences including those from childhood. First, appraisal bias, defined as a disposition to interpret situations in a certain direction (Mehu & Scherer, 2015), has been observed in children living with parents with financial hardship, as they have appraisal bias toward more hostile interpretations and report more anger (Chen & Matthews, 2001). Also, when children perceive their parent’s job insecurity, they are more likely to believe in an unjust world, which predicts more negative mood (Barling & Mendelson, 1999). Furthermore, adult survivors of childhood neglect report more anxiety symptoms as well as paranoia and hostility (Gauthier, Stollak, Messé, & Aronoff, 1996). This evidence suggests that childhood neglect is associated with appraisal bias toward more hostile interpretations, unfairness, and social injustice. Although the negative view of the world and the self, following childhood maltreatment, is believed to generalize to health (Kendall-Tackett, 2002), it remains unknown whether childhood neglect would be associated with patterns of cognitive appraisal specific to chronic pain.
One such cognitive appraisal concerns ‘injustice beliefs,’ which have been recently proposed to be a relevant cognitive appraisal to pain and pain-related outcomes (Sullivan et al., 2008). Perceived injustice about pain comprises of two factors: (a) injury severity/irreparability of loss and (b) blame/unfairness. The first factor of injury severity and irreparability of loss refers to ‘nobody understands how severe or serious my pain condition is’ and ‘my life will never be the same.’ The second factor of blame and unfairness refers to ‘I am suffering because of someone else’s negligence,’ and ‘it all seems so unfair’ (Sullivan et al., 2008). These injustice appraisals predict pain intensity, disability, and unfavorable health outcomes (Miller et al., 2018; Sullivan et al., 2008; Sullivan, Scott, & Trost, 2012). Importantly, perceived injustice is found to best predict work-related disability, whereas a well-established maladaptive pain appraisal, pain catastrophizing, best predicts pain severity ratings (Sullivan et al., 2008).
The Perceived Unfairness Model (Jackson, Kubzansky, & Wright, 2006) presents a theoretical framework for the current study. In this model, perceived unfairness is explained as a stressor, which subsequently activates a cascade of psychological and physical processes. Repeated exposure to such stressor contributes to biological, social, and behavioral mechanisms that increase physiologic overload, which can lead to serious health consequences over time (Jackson et al., 2006). Children and adults growing up with unmet needs may be more vulnerable to detrimental health consequences because childhood is a critical developmental period and the impact of perceived unfairness is cumulative, starting from the early life (Jackson et al., 2006). Additionally, those who are being neglected may develop an injustice appraisal of the world (Barling & Mendelson, 1999; Chen & Matthews, 2001; Gauthier et al., 1996). Accordingly, perceived childhood neglect, which serves as an antecedent and leads to a cognitive bias toward social injustice, may increase the likelihood of developing injustice appraisals specific to chronic pain. Importantly, this injustice belief system not only provides a lens to interpret situations and initiates a cascade of negative psychological and physical consequences (Jackson et al., 2006), but also serves as a guideline for behaviors and predicts an unfavorable disease trajectory (Bissell, Ziadni, & Sturgeon, 2018).
Research on the association between childhood neglect and perceptions of injustice is sparse, particularly in the context of chronic pain. As a result, the current study examined perceived injustice as a possible cognitive factor linking the relationship between perceived childhood neglect and adulthood health in patients with chronic pain, above and beyond other relevant constructs such as pain intensity and pain catastrophizing. It was hypothesized that perceived childhood neglect would be associated with greater perceived injustice about chronic pain conditions and worse psychological and physical function, and the associations between perceived childhood neglect and psychological and physical function would be mediated by perceived injustice.
Methods
Study procedures, which involved exclusively retrospective review of clinical data, were approved by the University’s Institutional Review Board.
Participants
Data were collected from the initial visit of consecutive 742 patients at the Stanford Pain Management Center, a large tertiary care pain clinic, between July 2015 and September 2015. Baseline demographics are presented in Table 1. Perceived childhood neglect was endorsed by 12.1% of patients. Gender was assessed by a binary response option (0 = male, 1 = female). The patients in this study were mostly middle aged (M = 49.7, SD = 15.4), female (66.3%), and White/Caucasian (54.2%). The non-White/non-Caucasian patients were mostly Hispanic/Latino (10.1%), followed by Asian (8.9%), African American (2.7%), and multi-racial or other (24.1%). Endorsed marital status included married (53.7), never married (21.2%), divorced (13.7%), and other categories (11.7%). The median levels of education were an Associate’s Degree for patients with and without endorsed perceived childhood neglect. Two binary variables (“yes/no”) were used to describe work and disability status: 43.0% and 27.2% reported currently ‘not working’ and ‘being on disability,’ respectively. About 42.0% of patients endorsed current alcohol use and 10.2% endorsed current cigarette smoking. Aforementioned demographic variables did not differ by endorsement of perceived childhood neglect. In contrast, higher endorsement of drug use and drug treatment history were found among patient endorsing perceived childhood neglect. The respective prevalence rates of drug use and drug treatment history were 16.7% and 13.3% for patients endorsing perceived childhood neglect versus 8.1% and 4.3% for patients not endorsing it. Pain duration was also significantly different; patients endorsing perceived childhood neglect reported a longer duration of pain (M = 8.8 years, SD = 10.9) than patients not endorsing it (M = 6.0, SD = 9.1).
Table 1.
Demographics
| Whole sample (n = 742) | No responders to childhood neglect (n = 652) | Yes responders to childhood neglect (n = 90) | χ2 | p | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Gender | 6.03 | .017 | |||
| Female | 492 (66.3) | 422 (64.7) | 70 (77.8) | ||
| Male | 250 (33.7) | 230 (35.3) | 20 (22.2) | ||
| Race/Ethnicity | 0.92 | .368 | |||
| White/Caucasian | 402 (54.2) | 349 (53.5) | 53 (58.9) | ||
| The others | 340 (45.8) | 303 (46.5) | 37 (41.1) | ||
| (Hispanics/Latino) | 75 (10.1) | 68 (10.4) | 7 (7.8) | ||
| (Asian) | 66 (8.9) | 58 (8.9) | 8 (8.9) | ||
| (African American) | 20 (2.7) | 17 (2.6) | 3 (3.3) | ||
| (Multi-racial, etc.) | 179 (24.1) | 160 (24.5) | 19 (21.1) | ||
| Marital statusa | 0.24 | .651 | |||
| Married | 395 (53.7) | 345 (53.4) | 50 (56.2) | ||
| The others | 340 (46.3) | 301 (46.6) | 39 (43.8) | ||
| (Never married) | 156 (21.2) | 140 (21.7) | 16 (18.0) | ||
| (Divorced) | 101 (13.7) | 85 (13.2) | 16 (18.0) | ||
| (Separated) | 22 (3.0) | 21 (3.3) | 1 (1.1) | ||
| (Widowed) | 26 (3.5) | 22 (3.4) | 4 (4.5) | ||
| (Living together) | 35 (4.8) | 33 (5.1) | 2 (2.2) | ||
| Educationb | 4.08 | .054 | |||
| Less than Bachelor’s | 369 (50.5) | 309 (48.1) | 53 (59.6) | ||
| Bachelor’s or higher | 362 (49.5) | 333 (51.9) | 36 (40.4) | ||
| (< High School) | 172 (23.5) | 143 (22.3) | 29 (32.6) | ||
| (High School) | 85 (11.6) | 81 (12.6) | 4 (4.5) | ||
| (Associate’s Degree) | 106 (14.5) | 85 (13.2) | 20 (22.5) | ||
| (Bachelor’s Degree) | 193 (26.3) | 172 (26.8) | 20 (22.5) | ||
| (Master’s or higher) | 131 (17.9) | 119 (18.5) | 12 (13.5) | ||
| (Professional School or PhD) | 46 (6.3) | 42 (6.5) | 4 (4.5) | ||
| Current work statusa (not working) | 316 (43.0) | 283 (43.7) | 33 (37.5) | 1.23 | .302 |
| Current disability status (on disability) | 202 (27.2) | 173 (26.5) | 29 (32.2) | 1.29 | .258 |
| Currently drinking (Yes = 1) | 312 (42.0) | 277 (42.5) | 35 (38.9) | 0.42 | .570 |
| Currently smokingc (Yes = 1) | 75 (10.2) | 62 (9.6) | 13 (14.6) | 2.16 | .139 |
| History of drug use (Yes = 1) | 68 (9.2) | 53 (8.1) | 15 (16.7) | 6.93 | .017 |
| History of drug treatment (Yes = 1) | 40 (5.4) | 28 (4.3) | 12 (13.3) | 12.7 | .002 |
| M (SD) | M (SD) | M (SD) | t | p | |
| Age (years) | 49.7 (15.4) | 49.4 (15.7) | 51.3 (13.1) | 1.22 | .225 |
| Pain duration (year) | 6.3 (9.4) | 6.0 (9.1) | 8.8 (10.9) | 2.33 | .022 |
Missing n;
7,
11,
6
In terms of pain conditions, patients self-reported their pain complaints according to several broad categories (i.e., nerve, muscle, disk, bone, infection, and cancer related, unknown, and undiagnosed medical problem; multiple selections were permitted). In the current study, patients most commonly identified their pain as being related to nerve problems (49.2%, n = 365), followed by muscle (26.3%, n = 195), disk (22.0%, n = 163), bone (13.1%, n = 97), infections (4.2%, n = 31), and cancer (2.6%, n = 19). Patients endorsed one (37.9%), two (21.0%), or more than two (19.6%) underlying causes of their pain. About 21.6% did not endorse any of the provided pain categories. Notably, 23.5% (n = 174) of the current sample reported injury as being the cause of their chronic pain and 76.5% (n = 568) reported non-injury-related chronic pain. IEQ scores were higher in patients endorsing injury as a cause for chronic pain (M = 19.70, SD = 12.12) than their counterparts (M = 17.31, SD = 11.17), t (740) = 2.42, p = .016. Distribution of pain diagnoses for patients visiting our clinic can be found at https://links.lww.com/ALN/B433.
Procedures
Patients were asked to complete an initial set of questionnaires through the CHOIR system, which could be completed up to one week prior to their first clinic visit or using a tablet computer during their first medical appointment at the clinic. CHOIR assesses several domains of physical, psychological, and social functioning using legacy surveys as well as Patient-Reported Outcomes Measurement Information Systems (PROMIS)® item banks developed by the National Institutes of Health. PROMIS item banks are obtained from Northwestern University Assessment Center, including item content and item parameters (Gershon et al., 2010). Computerized adaptive testing (CAT) is administered by CHOIR-CAT (Gershon et al., 2010). Use of CHOIR-CAT reduces participant burden by administering a select subset of items from each item bank until the resulting measurement meets pre-set criteria for standard errors; this approach typically requires fewer items than traditional forms of assessment (Cella, Gershon, Lai, & Choi, 2007; Gershon et al., 2010). No missing values were observed in the PROMIS measures. Because missing values were minimally observed in smoking status (1.5%), marital and work status (0.9%), and education levels (0.8%), pairwise deletion was used.
Measures
Demographics
Participants completed questions related to gender, age, ethnicity, marital status, education levels, work status, disability status, and pain characteristics.
Perceived Childhood Neglect
Perceived childhood neglect was assessed using a binary (yes/no) variable as part of patients’ intake assessment. Patients were asked “do you feel you were neglected as a child?” This variable, albeit brief, serves as a screener for perceived childhood neglect.
Perceived Injustice
Perceived injustice was assessed using the Injustice Experience Questionnaire (IEQ) (Sullivan et al., 2008). The IEQ consists of 12 items, scored from 0 (“never”) to 4 (“all the time”); IEQ scores are computed as a sum score with a range from 0 to 48, with higher scores representing a greater degree of perceived injustice about pain conditions (α = 0.92) (Sullivan et al., 2008). Representative items from the IEQ include “I worry that my condition is not being taken seriously” and “Most people don’t understand how severe my condition is.” The IEQ has demonstrated adequate psychometric properties (Sullivan et al., 2008) and been validated for use in patients with acute injury (Sullivan et al., 2008; Trost et al., 2015) and chronic pain (Rodero et al., 2012; Scott, Trost, Milioto, & Sullivan, 2013). A cutoff score of 19 on the IEQ has been identified in previous studies as indicative of long-term disability (Scott et al., 2013).
The Pain Catastrophizing Scale (PCS) is the most widely used empirical and clinical measure of pain catastrophizing (13 items, α = 0.87) (Sullivan, Bishop, & Pivik, 1995). Each item is rated on a 5-point Likert scale, ranging from 0 (not at all) to 4 (all the time). The total scores range from 0 to 52 with higher scores indicating greater tendency for pain catastrophizing. This scale assesses domains of rumination, magnification of the negative consequences of chronic pain, and helplessness related to pain that have been negatively associated with pain intensity, physical and mental function, and response to treatment (Granot & Ferber, 2005; Severeijns, Vlaeyen, van den Hout, & Weber, 2001; Turner, Jensen, Warms, & Cardenas, 2002).
PROMIS Pain Intensity. Pain intensity was assessed on a numerical rating scale (NRS) using a modified PROMIS Pain Intensity scale (Farrar, Young Jr, LaMoreaux, Werth, & Poole, 2001). Respondents were asked to rate their average pain intensity over the previous 7 days on a scale of 0–10. Assessment of pain intensity using an NRS has been supported in prior studies (Cook et al., 2013).
PROMIS Instruments item banks for Depression, Anxiety, Anger, Physical Function, and Social Isolation (Cella et al., 2007) were administered. Although all descriptions of PROMIS item banks are available online (https://www.nihpromis.org), their general content will be summarized here. The PROMIS item banks were developed using Item Response Theory approach (Riley, Pilkonis, & Cella, 2011). Higher scores on depression, anxiety, anger, and social isolation signified greater severity of these symptoms, whereas lower scores on physical function signified worse physical function. All PROMIS assessments were converted to T-scores (M = 50, SD = 10). Questions were framed according the experience of symptoms or functioning over the past 7 days.
Analyses
Analyses were conducted using SPSS version 21 and the PROCESS macro (Hayes, 2016). First, descriptive statistics and independent t tests were conducted to compare current and past history of physical and psychological function between patients with and without endorsed perceived childhood neglect, and Pearson correlations were computed to examine the bivariate relationships among perceived childhood neglect, IEQ scores, PCS scores, ratings for average pain, and the PROMIS measures. The averages of PROMIS-Depression, Anxiety, and Anger T-scores (negative affect T-scores) were used as a measure of negative affect and the PROMIS-Physical Function T-scores were used as a measure for physical function. Mediation analyses were conducted in two steps: first, by examining the direct effect of the neglect variable on both physical function and negative affect, followed by estimating the indirect effect of neglect on physical function and negative affect through perceived injustice. Ratings for the average pain and PCS scores were entered as covariates to examine whether the mediated (indirect) effects would be significant above and beyond the effect of well-known covariates. All indirect effects were estimated using a 5000-draw bootstrap-estimated product of coefficient (ab) approach. This approach utilizes a product of the predictor-mediator path coefficient (the a path) and the mediator-outcome path coefficient (the b path). The product of coefficients estimation approach has been deemed preferable to estimation via computation of differences between the direct and indirect paths due to a decreased susceptibility to type I error and a greater ability to detect mediated effects (i.e., greater power) (MacKinnon, Lockwood, & Williams, 2004). All direct and indirect effects are represented using standardized path coefficients, which allows for comparison of the relative sizes of each path. All analyses were two-tailed and used an alpha value of 0.05 unless otherwise specified.
Results
Descriptive statistics of our patients are presented in Table 2. The means of IEQ and PCS total scores were 17.9 (SD = 11.4) and 23.8 (SD = 12.7), suggesting that our patients reported higher levels of perceived injustice about chronic pain to patients reporting sustained injury (reported mean = 19.6 with SD of 12.6, n = 266), t(1006) = 2.03, p = .043 (Sullivan, 2008), and higher levels of pain catastrophizing than patients injured at work (reported mean = 20.9 with SD of 12.5, n = 851), t(591) = 4.74, p = .0001 (Sullivan, 2009). Overall, our patients reported an average pain intensity of moderate severity (M = 5.7, SD = 2.3), and average social isolation (M = 47.9 T, SD = 9.5), but slightly elevated depressive (M = 54.6 T, SD = 10.1) and anxiety symptoms (55.8 T, SD = 10.0), and substantially reduced physical function (M = 37.7 T, SD = 9.4).
Table 2.
Comparison of perceived injustice, pain catastrophizing, pain ratings, and PROMIS measures between the patients with and without endorsing childhood neglect
| Whole sample (n = 742) | ‘No’ responders to childhood neglect (n = 652) | ‘Yes’ responders to childhood neglect (n = 90) | d | t | p | |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||||
| IEQ total scores | 17.9 (11.4) | 17.1 (11.2) | 23.8 (11.6) | 0.59 | 5.30 | < .001 |
| PCS total scores | 23.8 (12.7) | 23.1 (12.6) | 28.6 (12.6) | 0.44 | 3.91 | < .001 |
| Pain ratings for average pain | 5.7 (2.3) | 5.6 (2.3) | 6.4 (1.9) | 0.38 | 3.54 | .001 |
| PROMIS-depression | 54.6 (10.1) | 53.8 (10.1) | 60.4 (8.7) | 0.70 | 5.92 | < .001 |
| PROMIS-anxiety | 55.8 (10.0) | 55.1 (9.9) | 61.2 (9.5) | 0.63 | 4.83 | < .001 |
| PROMIS-anger | 50.3 (10.4) | 49.4 (10.0) | 56.7 (10.8) | 0.70 | 6.35 | < .001 |
| PROMIS-negative affect | 53.6 (9.3) | 52.8 (9.1) | 59.5 (8.7) | 0.75 | 6.57 | < .001 |
| PROMIS-physical function | 37.7 (9.4) | 38.1 (9.6) | 34.9 (7.3) | −0.38 | −3.78 | < .001 |
| PROMIS-social isolation | 47.9 (9.5) | 47.1 (9.3) | 54.1 (9.2) | 0.76 | 6.82 | < .001 |
PROMIS measures used T-scores
Second, independent t tests were conducted to compare the IEQ total scores, PCS total scores, pain ratings, and PROMIS measures between patients endorsing and not endorsing perceived childhood neglect (Table 2). To reduce Type I error for multiple comparisons, α of 0.006 was considered significant (0.05 divided by nine variables). The results showed that patients endorsing perceived childhood neglect reported lower scores on the PROMIS-Physical Function and higher scores on the IEQ, PCS, and the PROMIS-Depression, Anxiety, Anger, and Social Isolation measures than patients not endorsing it. Pain ratings were not significantly different between the two at p value of .006. Therefore, worse physical, psychological, and social functions as well as greater pain catastrophizing and injustice beliefs about chronic pain conditions were observed in patients endorsing perceived childhood neglect.
Thirdly, Pearson correlation coefficients were calculated (Table 3). All correlation coefficients were in the expected direction. Especially, endorsement of perceived childhood neglect and higher IEQ scores were associated with worse physical function and greater pain catastrophizing, negative affect, and pain ratings. It should also be noted that all correlations (|rs|= .110–.692) were less than 0.90 and VIF values (1.06–2.20) were less than 10, suggesting no significant multicollinearity issues (Weaving et al., 2019).
Table 3.
Pearson correlation coefficients
| (a) Childhood neglect | (a) | (b) | (c) | (d) | (e) |
| (b) IEQ scores | .191** | ||||
| (c) PCS total scores | .142** | .692** | |||
| (d) Ratings for average pain | .110* | .360** | .413** | ||
| (e) Negative affect T-scores | .235* | .652** | .631** | .306** | |
| (f) Physical function T-scores | −.112** | −.363** | −.314** | −.439** | −.356** |
n of 742 for all measures
Finally, SPSS PROCESS 3.1 (Model 4) was used to examine whether the association between perceived childhood neglect and negative affect would be mediated by perceived injustice about chronic pain in adjusting for pain ratings and pain catastrophizing (Fig. 1). First of all, the single predictor model was significant (Fig. 1 Upper), suggesting that perceived childhood neglect predicted greater negative affect (path c, R = 4.15, p < .001). Then, as hypothesized, endorsement of perceived childhood neglect was associated with higher IEQ scores (path a, R = 3.17, p = .0007), suggesting that patients endorsing perceived childhood neglect reported greater injustice beliefs about their pain condition. A significant direct effect of perceived childhood neglect on negative affect was also observed (path c, R = 3.14, p < .0001), suggesting that endorsement of perceived childhood neglect was associated with greater negative affect. Additionally, the indirect effect of perceived childhood neglect on negative affect through perceived injustice was significantly different from zero (path a × path b, R = 1.01, 95% bootstrap CI 0.39–1.72), suggesting perceived injustice as a significant mediator.
Fig. 1.
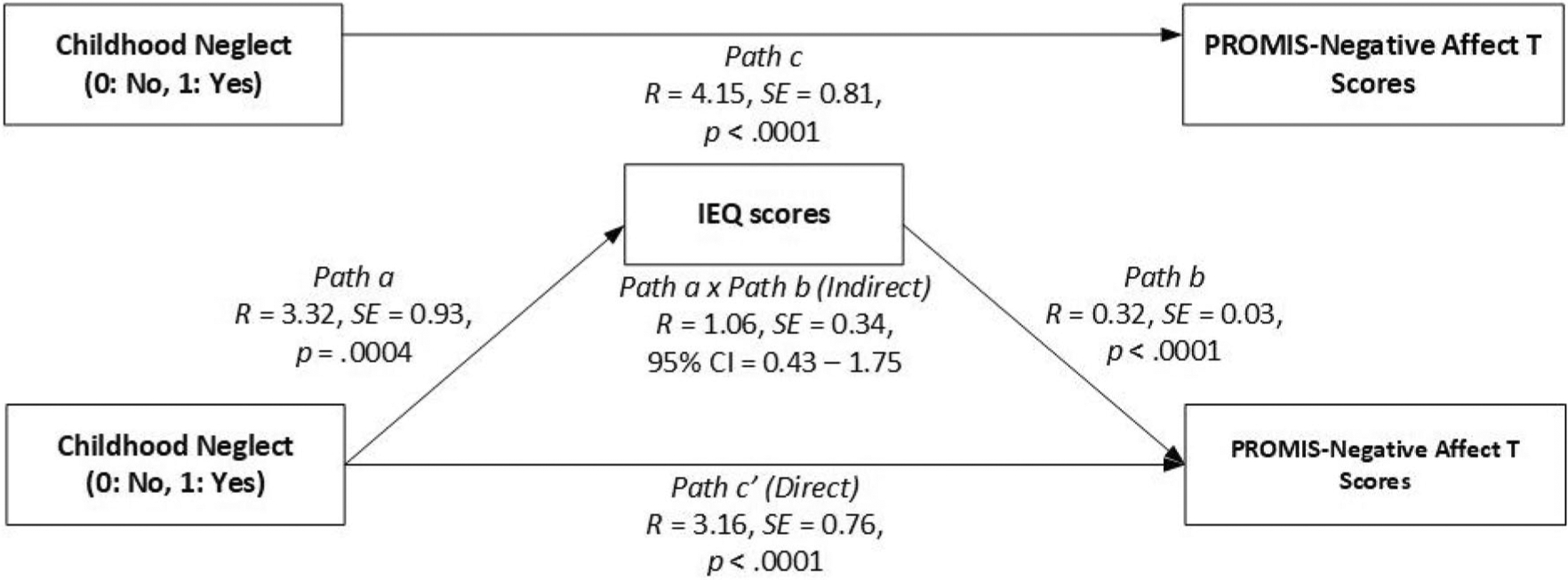
A diagram depicting the direct and indirect effect of childhood neglect on negative affect through perceived injustice and pain catastrophizing
Another mediation analysis was conducted to examine whether the association between perceived childhood neglect and physical function would be mediated by perceived injustice about chronic pain after adjusting for pain ratings and pain catastrophizing (Fig. 2). First, the single predictor model was not significant (Fig. 2), suggesting that perceived childhood neglect did not predict physical function (path c, p = .129) and the direct effect of perceived childhood neglect on physical function was also not significant (path c’, p = .3821). However, as hypothesized, the indirect effect of perceived childhood neglect on physical function through perceived injustice was significantly different from zero (path a × path b, R = − 0.59, 95% bootstrap CI − 1.08 to − 0.20), suggesting perceived injustice as a significant mediator.
Fig. 2.
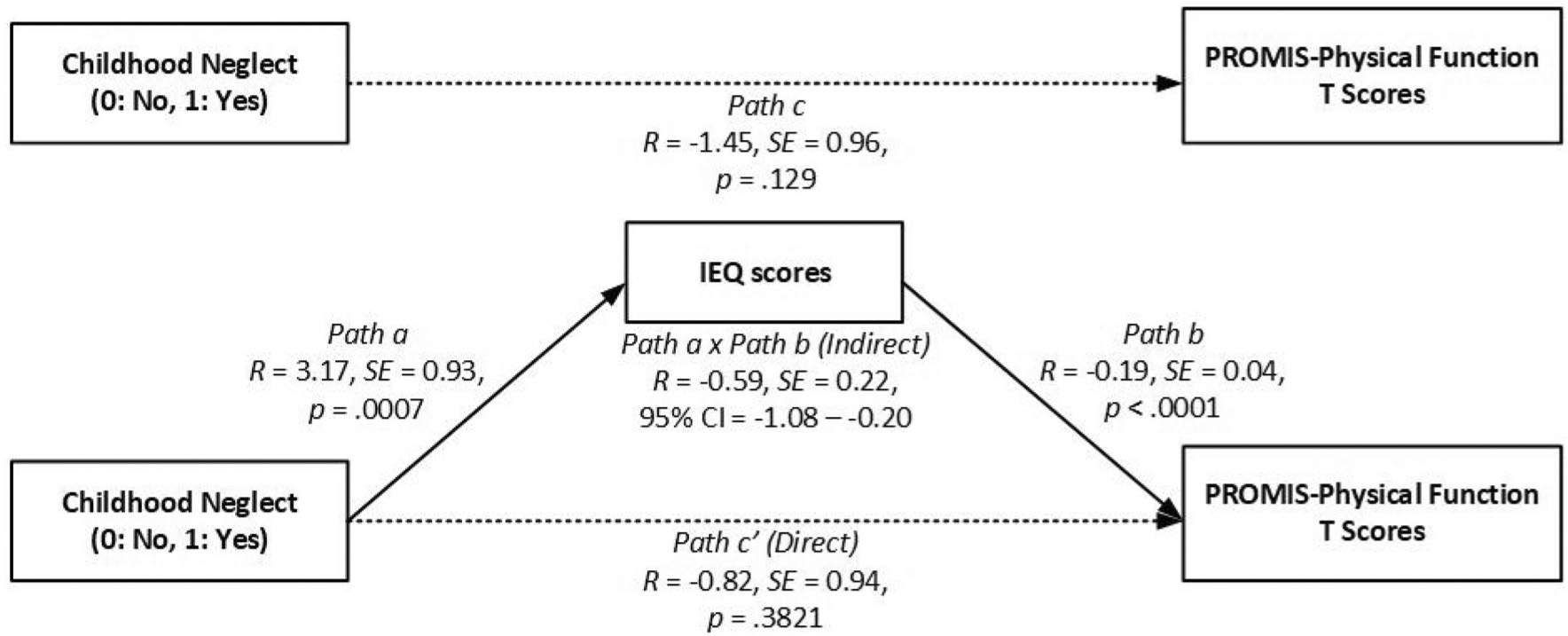
A diagram depicting the direct and indirect effect of childhood neglect on physical function through perceived injustice (IEQ) and pain catastrophizing (PCS). Solid lines: significant paths; a dotted line: non-significant path
Discussion
To our knowledge, the current study pilot is the first to examine whether perceived childhood neglect was associated with greater negative affect and poorer physical function, through perceived injustice, in adult patients with chronic pain seeking treatment at a tertiary pain clinic. As hypothesized, patients endorsing perceived childhood neglect reported poorer physical function, greater negative affect, and greater perceived injustice. Additionally, findings showed significant indirect effects of perceived childhood neglect on negative affect and physical function through perceived injustice, suggesting that perceived injustice was a significant mediator.
The current preliminary study findings are broadly consistent with Kendall’s theoretical pathways from childhood maltreatment to physical health (Kendall-Tackett, 2002) and the Perceived Unfairness Model (Jackson et al., 2006). Kendall proposed behavioral, social, emotional, and cognitive pathways linking childhood maltreatment and physical health. Specifically, adults who endorse childhood maltreatment engage in more health risk behaviors, experience more relationship dysfunction, experience emotional distress, and develop internal mental frames that are distorted toward a more negative, fearful, or mistrusting view of self and others, all of which contribute to worse physical health (Kendall-Tackett, 2002). Accordingly, patients in the current sample endorsing perceived childhood neglect reported more social isolation and negative affect. The cognitive pathway was of particular interest to the current study. In this cognitive pathway, adult survivors of childhood maltreatment have chronically negative, fearful, and mistrusting views of the world, life, themselves, and others (Kendall-Tackett, 2002). This negative self-perception can be generalized to negative appraisals of one’s own health (Kendall-Tackett, 2002). The current study findings also indicate that this appraisal pattern may be influenced by perceived childhood neglect, and may manifest more immediately in the context of injustice appraisals about irreversible health conditions such as chronic pain.
Perceived injustice, defined as feelings of blame and the irreparability of loss related to chronic pain condition, has significant implications for negative emotional and physical states in adult patients with chronic pain, particularly those endorsing perceived childhood neglect. Our preliminary findings demonstrate that injustice perceptions were associated with perceived childhood neglect as well as and more immediate indicators of worse emotional and physical functioning. Our results may indicate that perceived injustice may act as a more proximal indicator through which prior adverse experiences affect adaptation to a chronic health condition. From a conceptual standpoint, the Perceived Unfairness model (Jackson et al., 2006) lends support to the notion that unfair early life events/membership in a disadvantaged group (i.e., those who faced childhood neglect) might influence the development of injustice experiences, which subsequently influence health status. Further, it has been suggested that perceptions of injustice may arise from violations of just-world beliefs (Major, Kaiser, O’brien, & McCoy, 2007; Sullivan et al., 2008). In the case of childhood neglect, these stem from basic violations of a stable and predictable environment, whereby elevated just-world beliefs may predispose some individuals to perceive greater injustice (Major et al., 2007; Sullivan et al., 2008). The current results, albeit preliminary, are among the first to demonstrate empirical support for a coherent model connecting perceived childhood neglect and adjustment to chronic pain through injustice-specific cognitive appraisal.
To date, perceived injustice has been discussed primarily as a condition-specific variable, reflecting an appraisal of a justice violation in relation to experiences stemming from an injury or an illness. However, preliminary findings from this study suggest that perceived injustice also arises out of a more stable and global attribution pattern shaped by childhood maltreatment and similar adverse experiences. Once established, it may be that this attribution pattern manifests in response to subsequent life events, and may ultimately have implications for physical and mental health in later life (Cukor & McGinn, 2006; Gibb et al., 2001; Lumley & Harkness, 2007; Rekart, Mineka, Zinbarg, & Griffith, 2007; Sachs-Ericsson, Verona, Joiner, & Preacher, 2006). This interpretation is also consistent with research showing that perceived injustice, within a non-injury context, may reflect an enduring tendency to experience negative life events as unjust, and is associated with worse pain outcomes (Yakobov, Suso-Ribera, Vrinceanu, Adams, & Sullivan, 2019). Similar patterns have also been noted in response to prior experiences of racial discrimination, which appear to correlate with higher condition-specific injustice perception among individuals with chronic low back pain (Ziadni et al., 2019). More broadly, studies have found that several maladaptive schemas such as negative self-worth, danger schema or approaching threat (Gibb et al., 2001), hopeless view of future (Rekart et al., 2007), perceived uncontrollability (Sachs-Ericsson et al., 2006), self-criticism (Cukor & McGinn, 2006), and disconnectedness with others and rejection (Lumley & Harkness, 2007) mediate the association between childhood maltreatment and adulthood mental health. In addition, these constructs are intertwined in the “social aspects” of the pain experience (Sturgeon et al., 2016). Feelings of unfairness and blame can originate in childhood following neglect, and necessitate identification of a situation responsible for one’s experience of neglect. Similarly, feelings of unfairness may be salient among patients experiencing chronic pain, and can be directed toward external figures, including others who may be responsible for pain-related difficulties (as in the case of acute injuries due to the negligence of others), those responsible for treating pain (such as medical providers), and society as a whole, from which an individual with chronic pain may feel alienated or stigmatized (McParland & Eccleston, 2013).
Our preliminary findings are informative in several ways. First, perceived childhood neglect has received less attention as a health risk factor compared to childhood sexual and physical abuse. Among our patients, perceived childhood neglect was common, and was endorsed by 12.1% of patients, which indicates that neglect may itself be an overlooked factor contributing to different patterns of adjustment to chronic pain and suggests the potential value of routinely assessing perceptions of childhood adversity/maltreatment as part of assessment intakes for treatment-seeking patients with chronic pain. Second, we found that endorsement of childhood neglect was associated with worse psychological and physical function in patients with mixed etiology of chronic pain. Therefore, our results extend on previous findings of childhood neglect as being associated with greater pain and emotional distress in patients with fibromyalgia (Yeung et al., 2015) and migraines (Tietjen et al., 2010a, c), and highlight the clinical implication of perceived childhood neglect assessment at a pain clinic. Our results also showed that perceptions of injustice were significantly elevated among patients who had a memory of being neglected by caregivers in childhood, and therefore, these patients may be at risk for worse health outcomes. Lastly, the current study findings demonstrate the value in assessing injustice beliefs about pain, above and beyond the impact of pain intensity and catastrophizing, particularly among patients who endorse perceived childhood neglect, as it can serve as a possible treatment target. Cognitive-restructuring treatment approaches can be optimized to target cognitions and perceptions of injustice to reduce the impact of perceived childhood neglect on current health status above and beyond the effect of known covariates like pain severity and pain catastrophizing.
The current study includes limitations that warrant mention. First, the binary nature of the childhood neglect variable poses a threat to validity and reliability, and may account for the low rate of reported childhood neglect in our sample. Future studies should consider using validated measures of neglect such as the Adverse Childhood Experiences (Felitti et al., 2019), Early Childhood Trauma Inventory (Bremner, Vermetten, & Mazure, 2000), and Childhood Trauma Questionnaire (Bernstein et al., 2003), of which items range from 10 to 28 and, therefore, may be impractical at a busy outpatient pain clinic. The study participants were patients with mixed etiologies for chronic pain in a tertiary pain clinic, which is a unique patient population who might have been seeking treatment for many years, often with limited success. Indeed, the current patients demonstrated high rates of disability (27.2%), and an average pain duration of six years. In addition, the binary nature of the childhood neglect variable poses a threat to instrument validity. Second, the study participants were patients with mixed etiologies for chronic pain in a tertiary pain clinic, which is a unique patient population who might have been seeking treatment for many years, often with limited success. Indeed, the current patients demonstrated high rates of disability (27.2%), and an average pain duration of six years. However, we were not able to assess family history of chronic pain or control for the potential impact of the pathogenetic heterogeneity on study findings. Also, the study relied on patient self-report, which presents a potential for self-report bias and may not have the same degree of sensitivity and specificity as longer, clinically validated measures. Importantly, the history of childhood neglect, in addition to the longstanding nature of chronic pain, in the current study patients may suggest that perceptions of injustice may have developed and been maintained differently than in individuals facing acute trauma, where elements of loss and irreparability of loss may be more recent and, therefore, more salient. Additionally, causal inferences in terms of directionality of examined effects cannot be made due to the cross-sectional nature of the data, and our interpretation of mediation findings should be understood with this significant limitation in mind. Given the framing of neglect experiences as occurring during childhood, there is a reasonable argument that this variable may be assumed to carry at least some degree of temporal precedence compared to other variables in our model that explicitly assess current symptoms and cognitive appraisal patterns. However, we cannot attest to the stability of this measure across time, and our findings would be strengthened in any case by examination of these factors in longitudinal studies. Given relative paucity of research examining antecedents or correlates of perceived injustice in chronic pain populations, we propose that the statistical models in the current paper add incrementally to the current knowledge base, even if they are interpreted simply as a representation of the topography of relationships connecting more distal influences (i.e., childhood neglect) to more proximal indicators of chronic pain symptom severity and adjustment.
As noted previously, our findings warrant replication and extension in longitudinal studies. As appraisal processes may vary across time, whether due to general adaptation, changes in pain intensity or quality, or psychological intervention, examination of how these factors interrelate across time may yield additional information regarding causality and the temporal ordering of effects. Similarly, replication of these findings in clinical studies targeting perceived injustice may help to identify a treatment target in a vulnerable patient population. Importantly, this is the first study to identify perceived injustice as a potential modifiable mediator of the relationship between perceived childhood neglect and physical and psychological function even after adjusting for well-known covariates such as pain ratings and pain catastrophizing scores. Therefore, this model should be further examined with other possible mediators or moderators. For example, PTSD symptoms were found as a mediating variable between childhood maltreatment and more pain locations in young adults (Beal et al., 2020), or moderating variable between childhood trauma and adult pain (Raphael & Widom, 2011). Additionally, some found that PTSD symptoms co-exist, but are an independent predictor of worse pain in patients with wide spread pain (Coppens et al., 2017). Hence, future studies should examine the role of PTSD, in addition to the impact of the pathogenetic heterogeneity among patients with chronic pain. To date, we are not aware of studies examining perceived injustice as a key mediator of treatment responses; indeed, the degree to which perceived injustice beliefs vary across time or may be changed via clinical intervention is unclear. However, our findings suggest that this variable may be a treatment target to promote better emotional well-being and overall quality of life for patients with chronic pain who endorse perceived childhood neglect. Identifying modifiable moderators of this mediated effect would be useful to uncover additional treatment targets. For example, future studies should investigate effective coping strategies for mitigating the impact of unfairness at an individual level as well as possible preventative measures for these experiences at community and policy levels. The current findings also highlight the potential value of therapeutic approaches that may address the impact of prior neglect and maladaptive patterns of cognitive appraisal that may subsequently arise. In addition to the aforementioned concept of optimizing cognitive restructuring approaches to address injustice perception specifically, there may also be value in therapeutic approaches that facilitate processing of emotional distress that may arise and maintain from prior adverse life experiences, which have demonstrated promising results in chronic pain populations in recent years (Burger et al., 2016; Lumley et al., 2017).
The current study presents a cross-sectional mediation model representing the effects of perceptions of childhood neglect prior to the age of 17 on worse psychological and physical function through greater injustice beliefs. The relative salience of perceived injustice as a potential cognitive factor adversely impacting health status in individuals with chronic pain and perceived childhood neglect suggests that this factor warrants additional studies to determine injustice belief about pain as a potential key treatment target.
Funding
Funding was supported by National Institute on Drug Abuse (Grant No. K23DA047473).
Footnotes
Conflicts of interest All authors have contributed to the research, approved the manuscript, and agreed to authorship. Maisa S. Ziadni, Dokyoung S. You, John A. Sturgeon, Sean C. Mackey, Beth D. Darnall declare that they have no conflict of interest.
References
- Barling J, & Mendelson MB (1999). Parents’ job insecurity affects children’s grade performance through the indirect effects of beliefs in an unjust world and negative mood. Journal of Occupational Health Psychology, 4, 347–355. [DOI] [PubMed] [Google Scholar]
- Beal SJ, Kashikar-Zuck S, King C, Black W, Barnes J, & Noll JG (2020). Heightened risk of pain in young adult women with a history of childhood maltreatment: A prospective longitudinal study. Pain, 161, 156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Desmond D (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Bissell DA, Ziadni MS, & Sturgeon JA (2018). Perceived injustice in chronic pain: An examination through the lens of predictive processing. Pain Management, 8, 129–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn D, Bernardy K, Wolfe F, & Häuser W (2013). The association among childhood maltreatment, somatic symptom intensity, depression, and somatoform dissociative symptoms in patients with fibromyalgia syndrome: A single-center cohort study. Journal of Trauma & Dissociation, 14, 342–358. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Vermetten E, & Mazure CM (2000). Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: The Early Trauma Inventory. Depression and Anxiety, 12, 1–12. [DOI] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, & Salzinger S (1998). A longitudinal analysis of risk factors for child maltreatment: Findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse & Neglect, 22, 1065–1078. [DOI] [PubMed] [Google Scholar]
- Burger AJ, Lumley MA, Carty JN, Latsch DV, Thakur ER, Hyde-Nolan ME, … Schubiner H (2016). The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: A preliminary, uncontrolled trial. Journal of Psychosomatic Research, 81, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Gershon R, Lai JS, & Choi S (2007). The future of outcomes measurement: Item banking, tailored short-forms, and computerized adaptive assessment. Quality of Life Research, 16 Suppl 1, 133–141. [DOI] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B,… Rose M (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45, S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, & Matthews KA (2001). Cognitive appraisal biases: An approach to understanding the relation between socioeconomic status and cardiovascular reactivity in children. Annals of Behavioral Medicine, 23, 101–111. [DOI] [PubMed] [Google Scholar]
- Cook KF, Dunn W, Griffith JW, Morrison MT, Tanquary J, Sabata D, … Dudgeon BJ (2013). Pain assessment using the NIH Toolbox. Neurology, 80, S49–S53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppens E, Van Wambeke P, Morlion B, Weltens N, Giao Ly H, Tack J, … Van Oudenhove L (2017). Prevalence and impact of childhood adversities and post-traumatic stress disorder in women with fibromyalgia and chronic widespread pain. European Journal of Pain, 21, 1582–1590. [DOI] [PubMed] [Google Scholar]
- Cukor D, & McGinn LK (2006). History of child abuse and severity of adult depression: The mediating role of cognitive schema. Journal of Child Sexual Abuse, 15, 19–34. [DOI] [PubMed] [Google Scholar]
- Davis DA, Luecken LJ, & Zautra AJ (2005). Are reports of childhood abuse related to the experience of chronic pain in adulthood?: A meta-analytic review of the literature. Clinical Journal of Pain, 21, 398–405. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, … Giles WH (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28, 771–784. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Cahalan C, Mensing G, Smith M, & Haythornthwaite JA (2011). Pain, catastrophizing, and depression in the rheumatic diseases. Nature Reviews Rheumatology, 7, 216. [DOI] [PubMed] [Google Scholar]
- Farrar JT, Young JP Jr., LaMoreaux L, Werth JL, & Poole RM (2001). Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain, 94, 149–158. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (2019). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 56, 774–786. [DOI] [PubMed] [Google Scholar]
- Gauthier L, Stollak G, Messé L, & Aronoff J (1996). Recall of childhood neglect and physical abuse as differential predictors of current psychological functioning. Child Abuse & Neglect, 20, 549–559. [DOI] [PubMed] [Google Scholar]
- Gershon R, Rothrock NE, Hanrahan RT, Jansky LJ, Harniss M, & Riley W (2010). The development of a clinical outcomes survey research application: Assessment Center SM. Quality of Life Research, 19, 677–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Donovan P, … Tierney S (2001). History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognitive Therapy and Research, 25, 425–446. [Google Scholar]
- Goodwin RD, & Stein MB (2004). Association between childhood trauma and physical disorders among adults in the United States. Psychological Medicine, 34, 509–520. [DOI] [PubMed] [Google Scholar]
- Granot M, & Ferber SG (2005). The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: A prospective study. Clinical Journal of Pain, 21, 439–445. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2016). The PROCESS macro for SPSS and SAS. Retrieved from https://processmacro.org/index.html.
- Jackson B, Kubzansky LD, & Wright RJ (2006). Linking perceived unfairness to physical health: The perceived unfairness model. Review of General Psychology, 10, 21–40. [Google Scholar]
- Kendall-Tackett K (2002). The health effects of childhood abuse: Four pathways by which abuse can influence health. Child Abuse & Neglect, 26, 715–729. [DOI] [PubMed] [Google Scholar]
- Khandker M, Brady SS, Stewart EG, & Harlow BL (2014). Is chronic stress during childhood associated with adult-onset vulvodynia? Journal of Women’s Health, 23, 649–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MN, & Harkness KL (2007). Specificity in the relations among childhood adversity, early maladaptive schemas, and symptom profiles in adolescent depression. Cognitive Therapy and Research, 31, 639–657. [Google Scholar]
- Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte SE, Clauw DJ, et al. (2017). Emotional awareness and expression therapy, cognitive-behavioral therapy, and education for fibromyalgia: A cluster-randomized controlled trial. Pain, 158, 2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major B, Kaiser CR, O’brien LT, & McCoy SK (2007). Perceived discrimination as worldview threat or worldview confirmation: Implications for self-esteem. Journal of Personality and Social Psychology, 92, 1068–1086. [DOI] [PubMed] [Google Scholar]
- McParland JL, & Eccleston C (2013). “It’s Not Fair” social justice appraisals in the context of chronic pain. Current Directions in Psychological Science, 22, 484–489. [Google Scholar]
- Mehu M, & Scherer KR (2015). The appraisal bias model of cognitive vulnerability to depression. Emotion Review, 7, 272–279. [Google Scholar]
- Miller MM, Wuest D, Williams AE, Scott EL, Trost Z, & Hirsh AT (2018). Injustice perceptions about pain: Parent–child discordance is associated with worse functional outcomes. Pain, 159, 1083–1089. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9, e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael KG, & Widom CS (2011). Post-traumatic stress disorder moderates the relation between documented childhood victimization and pain 30 years later. PAIN®, 152, 163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rekart KN, Mineka S, Zinbarg RE, & Griffith JW (2007). Perceived family environment and symptoms of emotional disorders: The role of perceived control, attributional style, and attachment. Cognitive Therapy and Research, 31, 419–436. [Google Scholar]
- Riley WT, Pilkonis P, & Cella D (2011). Application of the National Institutes of Health patient-reported outcomes measurement information system (PROMIS®) to mental health research. Journal of Mental Health Policy and Economics, 14, 201–208. [PMC free article] [PubMed] [Google Scholar]
- Rodero B, Luciano JV, Montero-Marín J, Casanueva B, Palacin JC, Gili M, … Garcia-Campayo J (2012). Perceived injustice in fibromyalgia: Psychometric characteristics of the Injustice Experience Questionnaire and relationship with pain catastrophising and pain acceptance. Journal of Psychosomatic Research, 73, 86–91. [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Verona E, Joiner T, & Preacher KJ (2006). Parental verbal abuse and the mediating role of self-criticism in adult internalizing disorders. Journal of Affective Disorders, 93, 71–78. [DOI] [PubMed] [Google Scholar]
- Scott W, Trost Z, Milioto M, & Sullivan MJ (2013). Further validation of a measure of injury-related injustice perceptions to identify risk for occupational disability: A prospective study of individuals with whiplash injury. Journal of Occupational Rehabilitation, 23, 557–565. [DOI] [PubMed] [Google Scholar]
- Severeijns R, Vlaeyen JW, van den Hout MA, & Weber WE (2001). Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clinical Journal of Pain, 17, 165–172. [DOI] [PubMed] [Google Scholar]
- Sturgeon JA, Carriere JS, Kao M-CJ, Rico T, Darnall BD, & Mackey SC (2016). Social disruption mediates the relationship between perceived injustice and anger in chronic pain: A collaborative health outcomes information registry study. Annals of Behavioral Medicine, 50, 802–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturgeon JA, & Zautra AJ (2012). State and trait pain catastrophizing and emotional health in rheumatoid arthritis. Annals of Behavioral Medicine, 45, 69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJ (2008). User Manual for the Injustice Experience Questionnaire IEQ. https://sullivan-painresearch.mcgill.ca/pdf/ieq/IEQManual.pdf
- Sullivan MJ (2009). The pain catastrophizing scale: User manual (pp. 1–36). Montreal: McGill University. https://sullivan-painresearch.mcgill.ca/pdf/pcs/PCSManual_English.pdf [Google Scholar]
- Sullivan MJ, Adams H, Horan S, Maher D, Boland D, & Gross R (2008). The role of perceived injustice in the experience of chronic pain and disability: Scale development and validation. Journal of Occupational Rehabilitation, 18, 249–261. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Bishop SR, & Pivik J (1995). The pain catastrophizing scale: Development and validation. Psychological Assessment, 7, 524–532. [Google Scholar]
- Sullivan MJ, Scott W, & Trost Z (2012). Perceived injustice: A risk factor for problematic pain outcomes. Clinical Journal of Pain, 28, 484–488. [DOI] [PubMed] [Google Scholar]
- Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, … Aurora SK (2010a). Childhood maltreatment and migraine (part I). Prevalence and adult revictimization: A multicenter headache clinic survey. Headache: The Journal of Head and Face Pain, 50, 20–31. [DOI] [PubMed] [Google Scholar]
- Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, … Aurora SK (2010b). Childhood maltreatment and migraine (part II). Emotional abuse as a risk factor for headache chronification. Headache: The Journal of Head and Face Pain, 50, 32–41. [DOI] [PubMed] [Google Scholar]
- Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, … Aurora SK (2010c). Childhood maltreatment and migraine (part III). Association with comorbid pain conditions. Headache: The Journal of Head and Face Pain, 50, 42–51. [DOI] [PubMed] [Google Scholar]
- Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, … Warren AM (2015). Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabilitation Psychology, 60, 213–221. [DOI] [PubMed] [Google Scholar]
- Turner JA, Jensen MP, Warms CA, & Cardenas DD (2002). Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain, 98, 127–134. [DOI] [PubMed] [Google Scholar]
- Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, … Katon W (1999). Costs of health care use by women HMO members with a history of childhood abuse and neglect. Archives of General Psychiatry, 56, 609–613. [DOI] [PubMed] [Google Scholar]
- Weaving D, Jones B, Ireton M, Whitehead S, Till K, & Beggs CB (2019). Overcoming the problem of multicollinearity in sports performance data: A novel application of partial least squares correlation analysis. PLoS ONE, 14, e0211776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakobov E, Suso-Ribera C, Vrinceanu T, Adams H, & Sullivan MJ (2019). Trait perceived injustice is associated with pain intensity and pain behavior in participants undergoing an experimental pain induction procedure. Journal of Pain, 20, 592–599. [DOI] [PubMed] [Google Scholar]
- Yeung EW, Davis MC, & Ciaramitaro MC (2015). Cortisol profile mediates the relation between childhood neglect and pain and emotional symptoms among patients with fibromyalgia. Annals of Behavioral Medicine, 50, 87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziadni MS, Sturgeon JA, Bissell D, Guck A, Martin KJ, Scott W, et al. (2019). Injustice appraisal, but not pain catastrophizing, mediates the relationship between perceived ethnic discrimination and depression and disability in low back pain. The Journal of Pain. 10.1016/j.jpain.2019.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


