Abstract
Retroperitoneal lymphangioma is an uncommon and benign mesodermal tumour that arises from the retroperitoneal lymphatics. Notably, it is a rare occurrence in adults, where <200 adult retroperitoneal lymphangioma cases have been published in the literature. Additionally, retroperitoneal lymphangioma is often difficult to diagnose preoperatively and formal diagnosis is frequently determined following surgical exploration. Here, we describe a rare case of retroperitoneal lymphangioma in a 74-year-old man who presented with a 6-month history of intermittent fresh per rectal bleeding with an incidental non-tender left iliac fossa firm mass on examination. Computed tomography scan established a retroperitoneal cystic lesion abutting the aorta and left common iliac vessels. Surgical exploration revealed a large cystic mass and a clean plane of dissection was performed, where the mass was completely excised with all the key structures preserved. Histology was consistent with a retroperitoneal lymphangioma.
INTRODUCTION
Retroperitoneal lymphangiomas often present without symptoms and are identified either during imaging investigations for other conditions or surgery [1]. However, when the tumour is large and compresses on adjacent structures, the patient may experience symptoms including weight loss, pain and abdominal distension. Surgical removal is recommended for symptomatic, large or enlarging cystic lesions in view of their potential to invade adjacent structures with resultant complications, such as bleeding or renal obstruction [2]. Localized lymphangioma presents a good prognosis following surgery with a low reported rate of recurrence [3]. Herein, we describe a 74-year-old male with retroperitoneal lymphangioma who underwent successful surgical resection.
CASE REPORT
Our patient is a 74-year-old Chinese man with previous history of hypertension and hyperlipidaemia. He was referred from the community clinic for evaluation of 6-month history of intermittent fresh per rectal bleeding associated with hard stools. On examination, the abdomen was soft, non-tender and not distended. An incidental non-tender and firm left iliac fossa mass measuring 10 cm × 8 cm was palpated.
Computed tomography (CT) of the abdomen and pelvis indicated a well-circumscribed hypodense structure in the left side of the retroperitoneum adjacent to the aorta, the left common iliac artery and left common iliac vein measuring 13 cm × 9.7 cm × 15.8 cm where retroperitoneal lymphangioma was a consideration (Fig. 1). There was no significant thickened septation or mural nodularity. The low-density well-circumscribed left retroperitoneal lesion appeared to be cystic in nature displacing the left common iliac artery anteriorly. The left ureter was also displaced anteriorly resulting in mild left hydroureteronephrosis. The case was presented and discussed at a multidisciplinary tumour board where imaging was reviewed and there were no aggressive features seen. Differentials included a retroperitoneal cystic lymphangioma, mesenteric cyst or peritoneal inclusion cyst. Surgical resection was recommended. The patient elected to proceed with resection of the retroperitoneal tumour.
Figure 1.
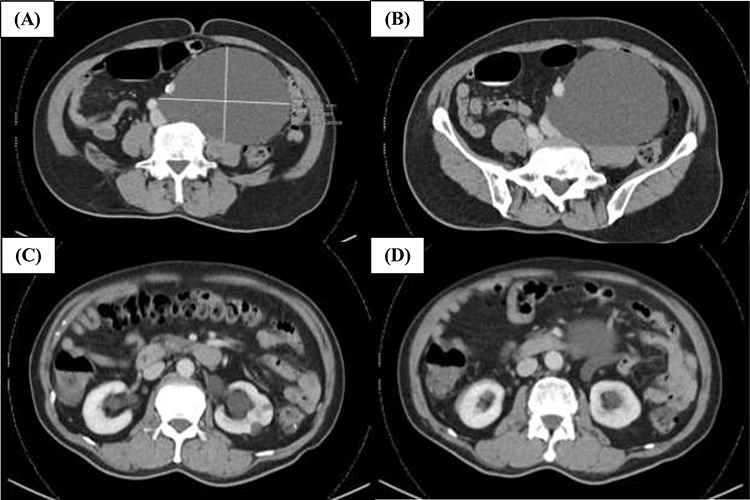
Representative CT images of the retroperitoneal lymphangioma. (A) Well-circumscribed hypodense structure in the left side of the retroperitoneum adjacent to the aorta, left common iliac artery and left common iliac vein measuring ~13 cm × 9.7 cm × 15.8 cm. There is no significant thickened septation or mural nodularity. (B) The left common iliac artery is displaced anteriorly. (C and D) There is mild mass effect resulting in mild dilatation of the left renal pelvicaliceal system and upper ureter. Both kidneys show symmetrical enhancement and renal cortex is of satisfactory thickness.
The patient underwent left ureteral double-J (DJ) stenting and resection of left retroperitoneal mass. The left ureter was displaced anteriorly by the retroperitoneal mass causing proximal hydroureter and hydronephrosis. Following left ureteral DJ stenting by the urology team, a midline laparotomy was made and sigmoid mesentery taken off the retroperitoneal mass. Intraoperatively, the left cystic retroperitoneal tumour was observed to be adherent to the left ureter, left iliac vessels, vertebrae, psoas and sigmoid mesentery (Fig. 2). The left ureter was dissected and slung. Subsequently, the tumour was carefully dissected off the aorta and left iliac vessels. Notably, the thin wall and cystic nature of the retroperitoneal tumour rendered it at risk of rupture and required careful handling. The lymphatic vessels were clipped and tied. The left gonadal vessels were also taken between ties as it entered the cystic mass. The retroperitoneal cystic tumour was excised intact and sent for histopathological examination. The left common iliac artery and left ureter were clearly visualized and preserved (Fig. 2). Full milk feeds were given intraoperatively to test for leak and no leak was visualized following 30 minutes.
Figure 2.
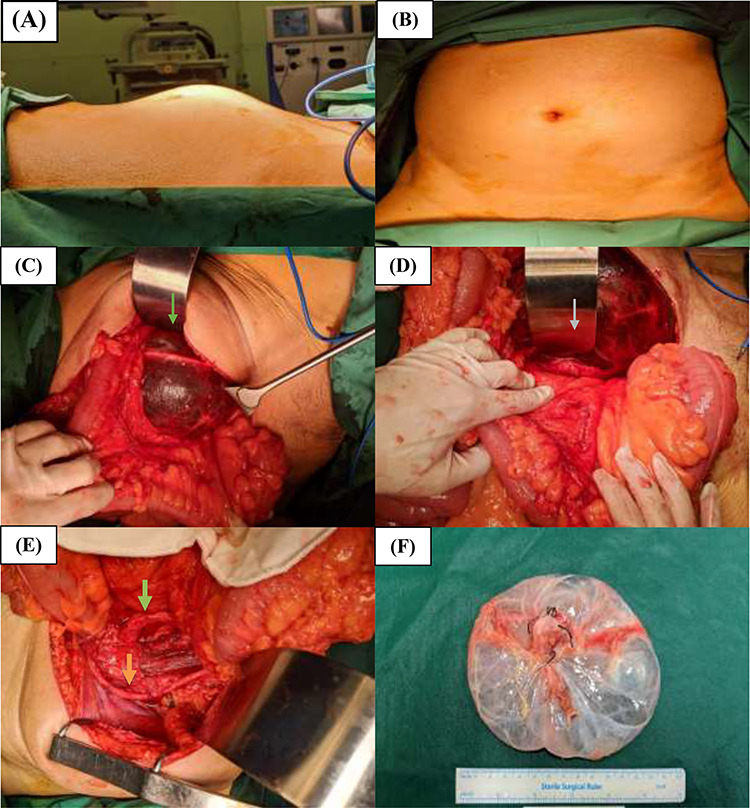
Preoperative and intraoperative photographs of the retroperitoneal cystic tumour. (A) Right lateral and (B) top-down preoperative views of the abdomen demonstrating the palpable left iliac fossa mass. (C and D) Intraoperative views of the retroperitoneal cystic mass with the left common iliac artery identified (grey arrow) and left ureter (green arrow) overlying the mass. (E) The left common iliac artery (grey arrow) and left ureter (green arrow) can be clearly seen and are preserved intact following resection of the retroperitoneal cystic mass. (F) Photograph of the retroperitoneal cystic mass specimen.
HISTOLOGY
Gross examination of the specimen showed a cyst measuring 9 cm × 8 cm × 1.5 cm. The cyst appeared unilocular and contained clear fluid. The external surface was smooth and the inner lining was smooth with no solid component or papillary excrescences. Histologically, the mass was made up of a cystic lesion with a fibrotic and degenerate cyst wall that was mostly denuded of lining cells. Within this wall, there were numerous vascular spaces lined mostly by normal-appearing endothelial cells with small nuclei and inconspicuous nucleoli. In some areas, there were clusters of cells with similar cytomorphology set in a myxoid background, and these areas likely represented myxoid degeneration. Alcian blue-periodic acid-Schiff (AB-PAS) stain highlighted these myxoid areas. The endothelial cells were positively stained for CD31, ERG and D2-40 immunostains. Immunohistochemical stains for Calretinin, HHV8 and Cam5.2 were negative. No evidence of high-grade sarcoma was seen. The final histology result was consistent with a retroperitoneal lymphangioma.
FOLLOW-UP
The patient tolerated the operation well and had an uneventful postoperative recovery. Diet was gradually escalated. He was discharged on post-operative Day 11.
DISCUSSION
Lymphangiomas are rare and benign neoplasms of the lymphatic system and occur in locations in which lymphatics are normally found [4]. The aetiology of these benign tumours is unclear where inflammatory and fibrotic processes on a background of genetic predisposition have been proposed [4]. A lymphangioma is a congenital neoplasm that is assumed to develop as a result of the failure of the lymphatic vessels to integrate with normal draining lymphatics at ~14–20 weeks of intrauterine life [5, 6]. Due to the aberrant connections between the lymphatic sacs with the venous system, lymphatic fluid stasis occurs in the lymphatic sacs leading to the formation of cystic tumours filled with serous or chylous fluid, which are encased in a layer of endothelial cells [2, 5]. Other lymphangioma origin explanations include the obstruction of lymph channels secondary to fibrosis, failure of endothelial secretory function, trauma or inflammation [3].
The use of various imaging modalities can complement each other in the preoperative evaluation of cystic lymphangioma [6]. Ultrasound imaging is useful as it reveals the cystic nature and internal structure of the lesion, particularly septations with clear fluid. CT imaging has the ability to distinguish lymphangiomas from adjacent bowel loops and differentiate para-pelvic renal lymphangiomatosis from hydronephrosis [7]. Preliminary CT imaging in the current case clearly showed a well-circumscribed cystic tumour close to the aorta and left iliac vessels. Magnetic resonance imaging renders images in various planes without losing resolution, which enables the precise identification of mass location from surrounding vascular and soft tissues for more accurate assessment [8]. Guided biopsy of the lesion is oftentimes challenging and seldom undertaken because of the tumour location and concerns of malignancy dissemination possibilities [9]. When fine-needle biopsy is carried out, copious amounts of lymphocytes may be observed [9]. Preoperative diagnosis of cystic lymphangiomas remains challenging, despite the availability of sensitive imaging modalities as they are almost indistinguishable from other cystic neoplasms on imaging [9]. Therefore, retroperitoneal lymphangioma diagnosis is frequently established following laparotomy or laparoscopy and confirmed on histopathological examination in conjunction with immunohistochemical staining.
Complete surgical removal of the neoplasm is the optimum treatment in view of the potential to increase in size and compress adjacent structures [3]. Furthermore, there is a risk of the cystic lesion rupture, leading to bleeding that can be potentially life-threatening [5]. The surgeon may partially resect involved organs should the lymphangioma invades or adheres to adjacent organs. Incomplete resection often results in recurrence and redo surgery presents a challenge. Complete surgical excision may also be challenging in cases where there is local invasion and encasement of important structures, such as major vessels and ureter. The excision and exposure may be more challenging in patients with retroperitoneal lymphangiomas than other intra-abdominal locations. In our case, although preoperative imaging was suggestive of the tumour displacing the aorta and left iliac vessels, the lymphangioma could be excised from these vessels and complete surgical resection was attained. In the last decade, 43 reports of surgical resection on retroperitoneal lymphangiomas have been published [10]. The recurrence rates ranged between 0% and 13.6%. Most recurrences occurred in patients who underwent a partial excision or had retroperitoneal cysts. Alternatives to surgery include argon coagulator, radiotherapy and sclerosing treatments such as alcoholic solutions, OK-432, doxycycline and bleomycin, with varying results reported [10]. These methods may be used for patients who are not fit for surgical resection; however, they have been associated with a higher recurrencerate.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
OCAJ is funded by the National Medical Research Council Transition Award (NMRC/TA/0061/2017).
Contributor Information
Hui Jun Lim, Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), Division of Surgery and Surgical Oncology, National Cancer Centre Singapore, Singapore.
Joey Wee-Shan Tan, Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), Division of Surgery and Surgical Oncology, National Cancer Centre Singapore, Singapore; Laboratory of Applied Human Genetics, Division of Medical Sciences, National Cancer Centre Singapore, Singapore.
Claramae Shulyn Chia, Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), Division of Surgery and Surgical Oncology, National Cancer Centre Singapore, Singapore; SingHealth Duke-NUS Oncology Academic Clinical Program, Duke-NUS Medical School, Singapore, Singapore.
Chin-Ann Johnny Ong, Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), Division of Surgery and Surgical Oncology, National Cancer Centre Singapore, Singapore; Laboratory of Applied Human Genetics, Division of Medical Sciences, National Cancer Centre Singapore, Singapore; SingHealth Duke-NUS Oncology Academic Clinical Program, Duke-NUS Medical School, Singapore, Singapore; Institute of Molecular and Cell Biology, A*STAR Research Entities, Singapore, Singapore.
REFERENCES
- 1. de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg 1998;85:395–7. [DOI] [PubMed] [Google Scholar]
- 2. Ozdemir H, Kocakoc E, Bozgeyik Z, Cobanoglu B. Recurrent retroperitoneal cystic lymphangioma. Yonsei Med J 2005;46:715–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fanaei S, Ziaee S. Retroperitoneal cystic lymphangioma: case report. Surg Sci 2011;2:209–11. [Google Scholar]
- 4. Cutillo DP, Swayne LC, Cucco J, Dougan H. CT and MR imaging in cystic abdominal lymphangiomatosis. J Comput Assist Tomogr 1989;13:534–6. [DOI] [PubMed] [Google Scholar]
- 5. Cherk M, Nikfarjam M, Christophi C. Retroperitoneal lymphangioma. Asian J Surg 2006;29:51–4. [DOI] [PubMed] [Google Scholar]
- 6. Sarno RC, Carter BL, Bankoff MS. Cystic lymphangiomas: CT diagnosis and thin needle aspiration. Br J Radiol 1984;57:424–6. [DOI] [PubMed] [Google Scholar]
- 7. Hauser H, Mischinger HJ, Beham A, Berger A, Cerwenka H, Razmara J, et al. Cystic retroperitoneal lymphangiomas in adults. Eur J Surg Oncol 1997;23:322–6. [DOI] [PubMed] [Google Scholar]
- 8. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg 1985;120:1266–9. [DOI] [PubMed] [Google Scholar]
- 9. Hayami S, Adachi Y, Ishigooka M, Suzuki H, Sasagawa I, Kubota Y, et al. Retroperitoneal cystic lymphangioma diagnosed by computerized tomography, magnetic resonance imaging and thin needle aspiration. Int Urol Nephrol 1996;28:21–6. [DOI] [PubMed] [Google Scholar]
- 10. Makni A, Chebbi F, Fetirich F, Ksantini R, Bedioui H, Jouini M, et al. Surgical management of intra-abdominal cystic lymphangioma. Report of 20 cases. World J Surg 2012;36:1037–43. [DOI] [PubMed] [Google Scholar]


