Abstract
Non-pharmacological interventions and tracing-testing strategy proved insufficient to reduce SARS-CoV-2 spreading worldwide. Several vaccines with different mechanisms of action are currently under development. This review describes the potential target antigens evaluated for SARS-CoV-2 vaccine in the context of both conventional and next-generation platforms.
We reported experimental data from phase-3 trials with a focus on different definitions of efficacy as well as factors affecting real-life effectiveness of SARS-CoV-2 vaccination, including logistical issues associated to vaccine availability, delivery, and immunization strategies. On this background, new variants of SARS-CoV-2 are discussed.
We also provided a critical view on vaccination in special populations at higher risk of infection or severe disease as elderly people, pregnant women and immunocompromised patients. A final paragraph addresses safety on the light of the unprecedented reduction of length of the vaccine development process and faster authorization.
Keywords: SARS-CoV-2, COVID-19, Vaccination, Primary prevention
1. Introduction
After the first outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on December 2019 in the region of Hubei, China, >2.1 millions people died and 98.2 millions have been infected despite the unprecedented implementation of infection control measures worldwide [1]. Non-pharmacological interventions (e.g. social distancing, face masking, hand washing, and ventilation) and tracing-testing strategy cannot eliminate the viral transmission [2]. An effective vaccination strategy based on efficacious vaccines could reduce SARS-CoV-2-related morbidity, mortality, and infectiousness [3]. Numerous SARS-CoV-2 vaccines based on different mechanisms of action are currently under development. The aim of the present review is to describe the results of experimental studies on SARS-CoV-2 vaccines, as well as the public health strategies to be implemented in national and regional scenarios.
2. Potential target antigens for SARS-CoV-2 vaccines
SARS-CoV-2 is an enveloped, single-stranded RNA virus belonging to the Coronaviridae family [4]. Its genome encodes for four structural proteins: spike (S), envelope (E), membrane (M), and nucleocapsid (N) [5]. The S proteins appear as spikes on the viral surface and its trimeric form contains two subunits: S1 responsible for receptor binding (a fragment called receptor-binding domain (RBD) binds ACE-2 receptor on cellular surfaces) and S2 responsible for membrane fusion and cell entry [[6], [7], [8]]. The S protein can trigger a cellular and humoral (neutralizing antibodies, NAbs) immune response [9,10]. NAbs titer is correlated with the levels of anti-RBD IgG [9,11]. N and M proteins can induce specific cytotoxic T lymphocytes, even if translational experiments demonstrated that immunity induced by M protein did not protect against the occurrence of SARS- CoV-2 infection [[12], [13], [14], [15]]. On the contrary, vaccines expressing the N protein caused pneumonia following the activation of eosinophils and TH2 cells [16]. E protein is poorly immunogenic owing to its small ectodomains for immune recognition [14].
3. SARS-CoV-2 vaccine platforms
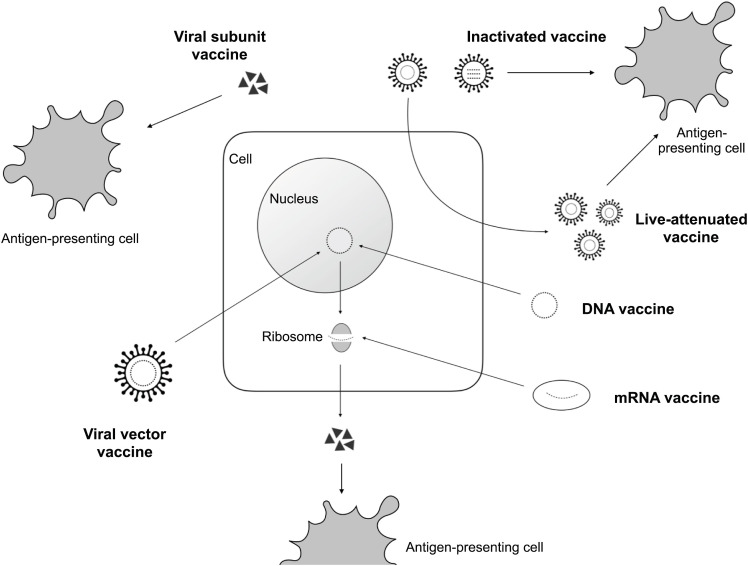
Vaccine platforms can be conventional and next generation (Table 1 ) [17,18]. Conventional vaccine platforms are virus- or protein-based. Virus-based vaccines can consist of inactivated or live-attenuated virus. Since whole-inactivated viruses do not replicate, adjuvants are required to stimulate the immune system [18]. Live-attenuated virus vaccines are generated by passaging in cell culture until the virus loses its pathogenic properties. Protein-based vaccines consist of a protein purified from the virus or virus-infected cells, recombinant protein, or virus-like particles. Virus-like particles lacks the genome. Whole-inactivated virus and protein-based vaccines require multiple vaccinations to induce protective immunity [18]. The majority of COVID-19 vaccine clinical trials are based on a next-generation platform, speeding up the vaccine development process [17,19]. Next-generation platform encompasses viral vector vaccines, nucleic acid-based vaccines, and antigen-presenting cells vaccines. Viral vectors vaccines consist of non-replicating or replicating virus vectors with a gene encoding SARS-CoV-2 antigen [17]. The antigen is produced by transduced host cells. Nucleic acid-based vaccines are based on DNA o mRNA fragments transduced or translated in the human cells [20]. Once injected into the muscle or skin, DNA plasmids enter human cells by electroporation. Subsequently, the plasmid DNA induces the host cell to produce temporarily the target protein via a sequential transcription-to- translation process [21]. Similarly, the mRNA vaccine temporarily induces the cell to produce the antigen protein coded by the mRNA [22]. Unlike DNA, RNA must be transported in various ways to enter the human cell. In the COVID-19 vaccines under development the mRNA is carried by lipid microvesicles [23,24]. Artificial antigen-presenting cells, previously explored for cancer vaccines, are used to stimulate T cell responses [25]. They are produced with lentiviruses to effectively mimic antigen-presenting cells [26]. However, this latter approach seems unaffordable for mass vaccination strategies owing to specific and complicated cold-chain requirements and onerous infusion procedures [19]. Fig. 1 summarize the mechanism of action of the vaccine platforms.
Table 1.
The main mechanisms of action and characteristics of the major types of vaccines [[17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]].
| Type | Mechanism of action | Advantages | Disadvantages |
|---|---|---|---|
| Classical platforms | |||
| Whole live-attenuated vaccine | Virus is attenuated by in vitro or in vivo passage or reverse- genetic mutagenesis. |
|
|
|
|
||
|
|
||
|
|
||
| Whole inactivated vaccine | Viruses is physically or chemically inactivated but preserve the integrity of the virus particle. |
|
|
|
|
||
|
|
||
|
|
||
| Viral subunit | Recombinant viral proteins induce immune response that elicit neutralizing antibodies without a cell-mediated response. |
|
|
|
|
||
|
|
||
| |||
| RNA Vaccines | Fragments of mRNA (isolated or genetically engineered) producing viral antigen(s) in the cytoplasm through direct protein translation in vivo. |
|
|
|
|
||
|
|
||
|
|
||
| DNA Vaccines | Viral antigen(s) encoded by a recombinant DNA plasmid are produced in host cells via a sequential transcription- to- translation process. |
|
|
|
|
||
|
|
||
| Viral vector | A replicating or non-replicating virus vector transports virus gene. |
|
|
|
|
||
|
|
||
| Antigen-presenting cells | Vector systems are used to express viral proteins and immune modulatory genes in order to modify aAPC stimulating T cell responses. |
|
|
| |||
| |||
Legend: BSL3: biosafety level 3.GMO: Genetically modified organism. aAPC: artificial antigen presenting cells.
Fig. 1.
Mechanism of action of each vaccine platforms.
4. Phase-3 trials on SARS-CoV-2 vaccines
Currently, phase-3 trials are published for 4 vaccines [23,24,28,29] (Table 2 ).
Table 2.
A summary of available phase-3 trials on SARS-CoV-2 vaccines on date February 5th, 2021.
| Vaccine | Type of vaccine | Phase | Patients enrolled | Country | Median follow-up time | Primary outcome | Results | Safety | Efficacy on severe cases |
|---|---|---|---|---|---|---|---|---|---|
| ChAdOx1 nCoV-19 [29] | Viral vector | 2/3 | 23848 | United Kingdom, Brazil, and South Africa | 3.4 months | Occurrence of virologically-confirmed, symptomatic COVID-19. | 30 (0.5%) cases among 5807 participants in the vaccine arm and 101 (1.7%) cases among 5829 participants in the control group resulting in vaccine efficacy of 70.4%. | Serious adverse events and adverse events of special interest balanced across the study arms. | No cases of severe COVID-19 in the ChAdOx1 vaccine group. In the control group there were 10 cases hospitalized for COVID-19; 2 were classified as severe COVID-19, including one death. |
| A case of transverse myelitis was reported 14 days after ChAdOx1 nCoV-19 booster vaccination as being possibly related to vaccination, with the independent neurological committee considering the most likely diagnosis to be of an idiopathic, short segment, spinal cord demyelination. | |||||||||
| mRNA- BNT162b2 [23] | RNA | 2/3 | 43548 | 152 sites worldwide (mostly United States) | 2 months | Occurrence of COVID-19 starting 7 days after the second injection of the vaccine | 8 cases (0.04%) of Covid-19 among participants assigned to receive BNT162b2 and 162 (0.86%) cases among those assigned to placebo resulting in vaccine efficacy of 95%. | More BNT162b2 recipients than placebo recipients reported any adverse event (27% and 12%, respectively) or a related adverse event (21% and 5%). | 1 case of severe COVID-19 in the BNT162b2 vaccine group. In the control group there were 9 cases of severe COVID-19. |
| BNT162b2 recipients reported more local reactions than placebo recipients (mild-to-moderate pain at the injection site was the most commonly reported local reaction, with less than 1% of participants reporting severe pain). | |||||||||
| Four related serious adverse events were reported among BNT162b2 recipients (shoulder injury related to vaccine administration, right axillary lymphadenopathy, paroxysmal ventricular arrhythmia, and right leg paresthesia). | |||||||||
| mRNA-1273 [24] | RNA | 3 | 30420 | United States | 64 days | Occurrence of COVID-19 starting 14 days after the second injection of the vaccine | 11 cases in the vaccine group (3.3 per 1000 person-years) and 185 cases in the placebo group (56.5 per 1000 person-years), indicating 94.1% efficacy of the mRNA-1273 vaccine. | The frequency of medically attended adverse events (9.7% vs. 9.0%) and serious adverse events (0.6% in both groups) were similar. | No cases of severe COVID-19 in the vaccine group. In the control group there were 30 cases of severe COVID-19, including one death. |
| Adverse events at the injection site occurred more frequently in the mRNA-1273 group than in the placebo group after both the first dose (84.2%, vs. 19.8%) and the second dose (88.6%, vs. 18.8%). However, these events were of low severity. | |||||||||
| Gam-COVID-Vac [28] | Viral vector | 3 | 21977 | Russia | 48 days | Occurrence of PCR-confirmed COVID-19 starting 21 days after the first dose. | 16 (0.1%) cases among 14.964 participants in the vaccine arm and 62 (1.3%) cases among 4902 participants in the control group resulting in vaccine efficacy of 91.6%. | The most common adverse events were flu-like illness, injection site reactions, headache, and asthenia. 30 adverse events were grade 3 (0.38%). None of the serious adverse events were considered associated with vaccination. | No cases of moderate or severe COVID-19 in the Gam-COVID-Vac vaccine group. In the control group there were 20 cases of moderate or severe COVID-19. |
4.1. ChAdOx nCoV-19 vaccine [29]
The first report provides an interim pooled analysis of four ongoing randomized trials carried out in three countries which enrolled 11,636 participants aged ≥18 years randomized 1:1 to receive the ChAdOx1 nCoV-19 vaccine or a control intervention (meningococcal vaccine or saline). The ChAdOx1 nCoV-19 vaccine was developed at Oxford University and consists of a replication-deficient chimpanzee adenoviral vector ChAdOx1, containing the SARS-CoV-2 structural surface spike protein gene. Two doses of the vaccine were administered at least 4 weeks apart. However, timing of priming and booster vaccine administration significantly varied. Furthermore, some of the participants received a low dose which contained half of standard dose, followed by a standard dose (LD/SD). The primary outcome was virologically confirmed COVID-19 disease, defined as a SARS-CoV-2–positive swab combined with at least one qualifying symptom (fever ≥37.8 °C, cough, shortness of breath, or anosmia or ageusia). The majority of the study sample (86.7%) were aged 18–55 years. 30/5807 (0.5%) and 101/5829 (1.7%) developed COVID-19 disease in the vaccine and in the control arm, respectively, resulting in a vaccine efficacy of 70.4%. Vaccine efficacy was 62.1% in participants who received two SD vaccines in comparison with 90% of the LD/SD group. Serious adverse events were equally described in both study arms. A case of vaccine-related transverse myelitis was reported 14 days after ChAdOx1 nCoV-19 booster vaccination.
4.2. BNT162b2 vaccine [23]
BNT162b2 is a lipid nanoparticle-formulated, mRNA vaccine administered intramuscularly. Adults recruited in the trial were ≥16 years of age, healthy or with stable chronic medical conditions (e.g., HIV, hepatitis B, hepatitis C). Key criteria for exclusion from the trial included a previous diagnosis of COVID-19, immunosuppression, pregnancy and breastfeeding women status. A total of 43,548 participants were randomized to receive either the vaccine or a saline placebo. Median age at vaccination was 52 years (16–91) and 21% had at least one concomitant medical condition. The primary endpoint was efficacy against COVID-19 disease with onset ≥7 days after the second dose. A total of 8 COVID-19 cases was recorded among participants assigned to receive BNT162b2 and 162 cases among those assigned to placebo; BNT162b2 was 95% (95% credible interval, 90.3 to 97.6) effective. Protective effect was observed by 12 days after the first dose when the cumulative COVID-19 incidence among placebo and vaccine recipients began to diverge. Similar vaccine efficacy was observed in stratified analyses by age, sex, race, ethnicity, baseline body-mass index, and comorbidities. Ten cases of severe Covid-19 with onset after the first dose occurred in placebo (9 cases) and BNT162b2 (1 case) recipients. Severe systemic events were reported in <2% of vaccine recipients after any dose, whereas fatigue (3.8%) and headache (2.0%) were more frequent after the administration of the second dose. No deaths were recorded. Systemic events were more often reported in younger (16–55 years) vaccine recipients and more often after dose 2.
4.3. MRNA-1273 vaccine [24]
mRNA-1273 vaccine was developed by Moderna and Vaccine Research Center at the National Institute of Allergy and Infectious Diseases (NIAID), within the National Institutes of Health (NIH). The main study enrolled 30,420 participants aged ≥18 years with no documented history of SARS-CoV-2 infection. The first dose was followed by a second injection 28 days later. Saline placebo was given to the control group. The primary outcome was the occurrence of symptomatic COVID-19 disease starting 14 days after the second injection. 11 cases of COVID-19 occurred in the vaccine group (3.3 per 1000 person-years) and 185 cases in the placebo group (56.5 per 1000 person-years), indicating an efficacy of 94.1%. Vaccine efficacy was similar across pre-determined groups of interest, including those who already had antibodies against SARS-CoV-2 at the time of enrollment and among those who were 65 years of age or older. Severe Covid-19 occurred in 30 participants, with one death, exposed to the placebo group. Moderate-to-severe systemic adverse events (fatigue, myalgia, arthralgia, and headache) were described in ~50% of participants in the mRNA-1273 group after the second dose. Adverse events occurred ~15 h after vaccination and resolved by day 2, with no sequelae. The incidence of serious adverse events was similar in mRNA-1273 and placebo arms. Adverse events at the injection site occurred more frequently in the mRNA-1273 group after the first (84.2% VS. 19.8%) and the second dose (88.6% VS. 18.8%). In the mRNA-1273 group, local events were mainly grade 1 or 2 in severity and lasted a mean of 2.6 and 3.2 days after the first and second dose, respectively. The most common injection-site event was pain (86.0%).
4.4. Gam-COVID-Vac vaccine [28]
Gam-COVID-Vac is a heterologous recombinant adenovirus (rAd)-based vaccine. The randomized, double-blind, placebo-controlled, phase 3 trial is ongoing at 25 hospitals in Moscow, Russia. Participants were randomly assigned (3:1) to receive vaccine or placebo, with stratification by age group. However, the interim efficacy analysis was published on 2 February 2021 based on almost half of the planned patients. The first dose was followed by a second injection 21 days later. Key inclusion criteria were: age 18 years or older; negative anti-SARS-CoV-2 IgM and IgG antibody and SARS-CoV-2 PCR tests; no contact with anyone with COVID-19 in the preceding 14; negative urine pregnancy test (for women of child-bearing potential); no history of vaccine-induced reactions; and no acute infectious or respiratory disease in the 14 days before enrolment. The primary outcome was the occurrence of PCR-confirmed COVID-19 starting 21 days after the first dose. 16 (0.1%) COVID cases among 14.964 participants occurred in the vaccine arm and 62 (1.3%) COVID cases occurred among 4902 participants in the control group resulting in vaccine efficacy of 91.6%. Notably, vaccine efficacy was 91.8% (67.1–98.3) in participants older than 60 years. No cases of moderate or severe COVID-19 occurred in the Gam-COVID-Vac vaccine group whereas 20 cases of moderate or severe COVID-19 occurred in the control group there were 20 cases. Most of the reported adverse events (94%) were mild. The most common adverse events were flu-like illness, injection site reactions, headache, and asthenia. None of the serious adverse events were considered associated with vaccination.
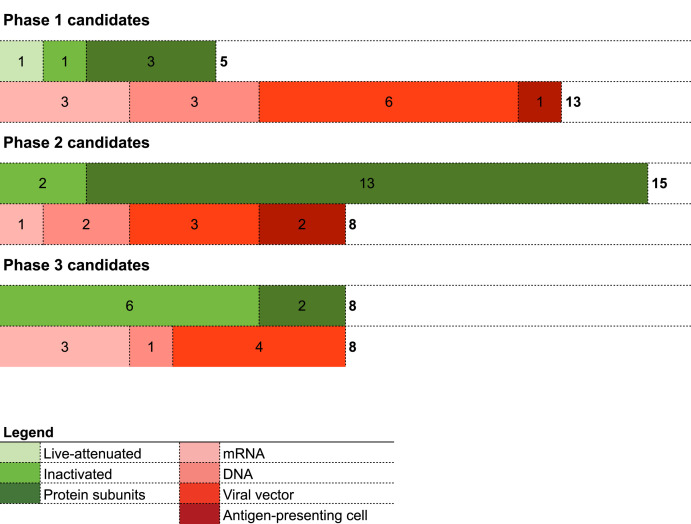
Other vaccines are currently under study, of which candidates with ongoing phase-1-2-3 trials are shown in Fig. 2 .
Fig. 2.
Phase-1-2-3 trials on COVID-19 vaccines (last update 29 January 2021).
5. Efficacy of SARS-CoV-2 vaccines in experimental studies
The definition of vaccine efficacy is challenging. From a clinical perspective the endpoints are heterogenous. Phase 3 trials demonstrated efficacy against COVID-19 disease (effective immunity), although data concerning the reduction of viral circulation among vaccinated people are not yet known (sterilizing immunity) [23,24,28,29]. The WHO document on the preferred and minimally acceptable profiles of human vaccines against SARS-CoV-2 recommended an ideal 50% cut-off against several outcomes, including disease, severe disease, and/or viral transmission [31]. The primary outcome adopted by the clinical trials performed until now is the occurrence of COVID-19 disease [[23], [24], [28], [29], [30]]. Whether first-generation vaccines will be effective on viral transmission or can prevent severe clinical manifestations is still a matter of debate. An effective vaccine which prevents severe disease might reduce mortality in high-risk groups and relieve pressure on health-care systems [3]. Severe COVID-19 cases were significantly lower in the experimental vaccinated groups, although clinical trials were not designed to assess the impact on severe disease [23,24,28,29]. However, clinically effective vaccines could not prevent SARS-CoV-2 transmission. Preliminary studies show that nasal shedding of SARS-CoV-2 was not different when vaccinated animals are compared with a control group, even if viral load in lower airways of vaccinated decreased [32,33]. Furthermore, the route of administration of COVID-19 vaccines currently under development is intramuscular, which predominantly produces a systemic IgG response and a poor mucosal response [34]. Data on humans are lacking and future studies should prove if a vaccine which elicits the mucosal immunity can reduce upper airway viral shedding and, then, viral transmission. The assumption that mass vaccination will result in successful control of SARS-CoV-2 infection with acceptable social costs is currently not supported by any scientific evidence. Recently, a set of clinical endpoints has been proposed to standardize evaluation and comparison of efficacy among vaccine candidates, overall and across relevant subgroups [35]. The proposed clinical endpoints are: SARS-CoV2 infection; COVID-19 symptomatic infection; asymptomatic infection; severe COVID-19; non-severe COVID-19; and burden of disease (BOD). SARS-CoV2 infection is defined by positive RNA PCR result or SARS-CoV2 seroconversion. COVID-19 symptomatic infection is defined by a protocol-specified list of COVID-19 symptoms with virologic confirmation of SARS-CoV-2 infection. Asymptomatic infection is defined by SARS-CoV-2 seroconversion without prior diagnosis of the COVID-19 disease. Severe COVID-19 is defined by virologic confirmation of SARS-CoV-2 infection and at least one of the following criteria: respiratory failure; evidence of shock; clinically significant acute renal, hepatic, or neurologic dysfunction; admission to an intensive care unit; and death. Non-severe COVID-19 is defined by virologic confirmation of SARS-CoV-2 infection, absence of criteria for severe COVID-19 and the presence of at least one of the following criteria: fever or chills; cough; shortness of breath or difficulty breathing; fatigue; muscle or body aches; headache; new loss of taste or smell; sore throat; congestion or runny nose; nausea or vomiting; and diarrhea. Finally, BOD is an endpoint based on a score that weights the disease severity. The score is 0 for no COVID-19, 1 for non-severe COVID-19, and 2 for severe COVID-19.
6. Factors affecting vaccine effectiveness in a real-world scenario
Vaccine efficacy estimated during the clinical trials might not account for real-life conditions. Several factors might affect the effectiveness of a mass vaccination and the herd immunity. It is assumed that immunity is short-lived. Antibody titer can wane within weeks after infection and the magnitude of the antibody neutralization in asymptomatics decreases faster than in symptomatics [36]. Data from the phase-1 trial of mRNA-1273 vaccine suggested that antibody titers persisted for about 4 months in immunized individuals [37]. As a consequence, SARS-CoV-2 infection can become endemic worldwide [38]. However, in case of long-lasting immunity, a mass vaccination campaign must face logistical challenges related to large-scale production and distribution. The reduction of COVID-19 mortality strictly depends on the high vaccine coverage of high risk groups (i.e., elderly individuals and/or patients with concomitant diseases). Definition of the priority groups is the cornerstone for a key change of the main epidemiological indicators, fitting principles of social justice to mitigate disparities and health inequities across ethnic minorities and geography.
The storage and transport, based on reliable cold-chains, require adequate infrastructures: this organizational issue could result in heterogeneity of national immunization coverage [39].
Moreover, public acceptance plays a crucial role for a successful vaccination campaign. A recent survey in 19 countries reported that the acceptance rate of a SARS-CoV-2 vaccine is far from being universal [40]. Vaccine hesitancy has recently increased ignoring overwhelming scientific evidence on safety and effectiveness of vaccines. Clear and transparent communication of both personal and public health advantages, as well as on the risk of adverse events, must be promptly undertaken by national and regional authorities and stakeholders.
New variants of SARS-CoV-2 might affect vaccine effectiveness. SARS-CoV-2 belongs to the RNA viruses, that have a high mutation rate. Genetic instability has long been considered to represent a challenge to develop effective vaccines against RNA viruses. The spike N501Y substitution located within the RBD could become a global threat: it is associated to a higher viral load and increased transmissibility (50–70%) [41,42]. Variants detected in the United Kingdom and South Africa share this mutation. The E484K mutation in the RBD can help viral escape from a highly neutralizing convalescent plasma [43,44]. This variant has been recently described across several Brazilian regions (e.g., Manaus city where the population natural immunity was higher than 50% [44,45]. However, immunity depends on antibodies and cellular responses, which could surrogate or replace the poor antibody neutralization.
6.1. Special populations
Clinical trials carried out until now demonstrated efficacy and safety of vaccines in a homogeneous immunocompetent population [23,24,28,29]. However, scientific concerns have been raised for the vaccination of elderly people, pregnant women, people aged less than 16 years, and immunocompromised patients. Those populations are at higher risk of infection or severe disease [[46], [47], [48]]. Immunosenescence, immunodeficiency, or pregnancy-related immune impairment could make the individuals more vulnerable to the viral infection and impair the immune response following vaccination [46].
Efficacy of the mRNA-1273 SARS-CoV-2 vaccine was lower in individuals >65 years (86.4%) when compared with that of individuals aged 18–65 years (95.6%) [23]. It is well known that aging is associated with loss of immunological memory, reduced repertoire of immunological responses, and increased inflammatory tone [49,50]. A recent phase-1 open label trial of mRNA-1273 recruited persons aged 56–70 years and those ≥71 years [51]. Notably, a slight reduction of the antibody neutralization tests was detected in subjects older than 71 years [51]. However, the data from the Gam-COVID-Vac vaccine are promising since they evidenced a vaccine efficacy of 91.8% (67.1–98.3) in participants older than 60 years that is similar to the 91.6% of the entire population analyzed [28].
Pregnant women have been systematically excluded from clinical trials on Covid-19 interventions, although several therapies are considered safe during pregnancy (e.g., systemic steroids and hydroxychloroquine). A review on international clinical trial registries found 155 COVID-19 trials, with 80% excluding pregnant women [52]. This imbalance should be immediately interrupted to decrease in equal access to health resources. Recently, the SOLIDARITY trialists extended inclusion also to pregnant women, paving a new way in the Covid-19 research [53].
The majority of the vaccine trials excluded children and adolescents [23,24,28,29]. It is currently unknown if they develop the same effective immunity of the adult population, whether a reduced dose can be beneficial, or age-related safety issues could occur. Furthermore, epidemiologists and public health specialists have suggested that COVID-19 cannot be defeated without a global childhood and adolescent vaccination [54]. Clinical trials on children aged 12 years or older are currently ongoing [55,56].
6.2. Safety issues
To address the clinical and public health threat of the COVID-19 pandemic, the vaccine development process has been reduced from the conventional 10–15 years to 1–2 years [19]. This unprecedented achievement depended on a faster authorization process and on new manufacturing platforms. Safety is a prerequisite for a vaccine to be administered. Indeed, a vaccine is not a drug for critically ill people, but rather a treatment that is given to those who are well to prevent the risk of a severe disease. Safety is determined by the vaccine platform, the adjuvant, the mode and route of vaccine administration, the age of vaccinees and the pre-existing vaccine immunity [57].
One of the main potential barrier to the development of safe and efficacious COVID-19 vaccines is the risk that insufficient titres of neutralizing antibodies might trigger antibody-dependent enhancement (ADE) of disease [32,58]. ADE depends on an increased Fc-mediated cellular entry of the virus or excessive immune complex formation with subsequent inflammation [59]. In individuals challenged by homotypic or heterotypic serotype viruses, the antibodies will recognize viral antigens and mediate antibody-dependent disease exacerbation in two ways [60]. First, virus–antibody complexes might enter Fc receptor (FcR)-bearing cells, such as dendritic cells and monocytes, by FcR-mediated internalization, which is termed ‘antibody-dependent enhancement’ (ADE) resulting in increased viral replication [[61], [62], [63]]. After entering in the host, the virus may activate a harmful immune response, resulting in the release of proinflammatory cytokines. The activated TH2 cells contribute to the activation of antibody production. However, they release interleukin-4 (IL-4), IL-13 and IL-5, as well as eosinophil chemoattractant, thus resulting in eosinophil infiltration and proinflammatory cytokine production in the lung [62,63]. Safety concerns were initially based on experimental data showing that immunization against SARS-CoV-2 may result in enhanced viral replication in vitro and diffuse alveolar damage in vivo in a population of non-human primates [63,64]. However, this effect is supposed to be limited to inactivated or viral vector vaccine formulations. Clinical data on humans are currently lacking and vaccine trials did not report any severe events related to ADE [23,24,28,29]. However, clinical trials might be unpowered to detect rare severe adverse events: safety profile of SARS-CoV-2 vaccines should be carefully adjusted following the information retrieved from post-marketing drug monitoring programs.
7. Conclusions
The announcement of new vaccines readily available for the immunization of individuals at risk and general population is only an intermediate step in the battle against SARS-CoV-2. The limitations we described may potentially affect vaccine efficacy and effectiveness, as well as its ability to generate herd immunity. The logistical issues associated to vaccine availability, delivery, and immunization strategies, and the occurrence of new variants fully or partially resistant to vaccine-induced antibodies represent the main concern in low-, middle-, and high-income countries. However, the marketing of new vaccines, achieved after an unprecedented rapid development process based on new technologies and platforms, could represent the key momentum for the control of the Covid-19 pandemic.
Author contributions
Conceptualization: AG, FA, GS, SA, FB. Data curation and formal analysis: AG, FA, GS, LS. Methodology: GS, LS. Writing - original draft: AG, FA. Writing - review and editing: AG, FA, AV, LS, SA. All authors read and approved the final manuscript.
Funding
Not applicable.
Institutional review board statement
Not applicable.
Declaration of competing interest
The authors declared no conflict of interest.
Acknowledgments
Not applicable.
References
- 1.https://www.who.int/publications/m/item/weekly-epidemiological-update---27-january-2021
- 2.Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the Achilles' Heel of current strategies to control Covid-19. N. Engl. J. Med. 2020;382(22):2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodgson S.H., Mansatta K., Mallett G., Harris V., Emary K.R.W., Pollard A.J. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect. Dis. 2021;21(2):e26–e35. doi: 10.1016/S1473-3099(20)30773-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundstrom K. Coronavirus pandemic-therapy and vaccines. Biomedicines. 2020;8:109. doi: 10.3390/biomedicines8050109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lan J., Ge J., Yu J., Shan S., Zhou H., Fan S., et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 7.Letko M., Marzi A., Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai Y., et al. Distinct conformational states of SARS-CoV-2 spike protein. Science. 2020;369:1586–1592. doi: 10.1126/science.abd4251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suthar M.S., et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep. Med. 2020;1:100040. doi: 10.1016/j.xcrm.2020.100040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao Q., et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369:77–81. doi: 10.1126/science.abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ni L., et al. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity. 2020;53:971–977. doi: 10.1016/j.immuni.2020.04.023. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grifoni A., et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181:1489–1501. doi: 10.1016/j.cell.2020.05.015. e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gao W., et al. Effects of a SARS-associated coronavirus vaccine in monkeys. Lancet. 2003;362:1895–1896. doi: 10.1016/S0140-6736(03)14962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du L., He Y., Jiang S., Zheng B.J. Development of subunit vaccines against severe acute respiratory syndrome. Drugs Today. 2008;44:63–73. doi: 10.1358/dot.2008.44.1.1131830. [DOI] [PubMed] [Google Scholar]
- 15.Sun J., et al. Generation of a broadly useful model for COVID-19 pathogenesis, vaccination, and treatment. Cell. 2020;182:734–743. doi: 10.1016/j.cell.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yasui F., et al. Prior immunization with severe acute respiratory syndrome (SARS)-associated coronavirus (SARS- CoV) nucleocapsid protein causes severe pneumonia in mice infected with SARS- CoV. J. Immunol. 2008;181:6337–6348. doi: 10.4049/jimmunol.181.9.6337. [DOI] [PubMed] [Google Scholar]
- 17.van Riel D, de Wit E. Next-generation vaccine platforms for COVID-19. Nat. Mater.. 2020 Aug;19(8):810-812. doi:10.1038/s41563-020-0746-0.PMID.32704139. [DOI] [PubMed]
- 18.Mathew S, Faheem M, Hassain NA, Benslimane FM, Thani AAA, Zaraket H, Yassine HM. Platforms exploited for SARS-CoV-2 vaccine development. Vaccines (Basel). 2020 Dec 25;9(1):11. doi: 10.3390/vaccines9010011.PMID.33375677.PMCID.PMC7824029. [DOI] [PMC free article] [PubMed]
- 19.Lurie N., Saville M., Hatchett R., Halton J. Developing Covid-19 vaccines at pandemic speed. N. Engl. J. Med. 2020;382(21):1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- 20.Zhang C., Maruggi G., Shan H., Li J. Advances in mRNA vaccines for infectious diseases. Front. Immunol. 2019;10:594. doi: 10.3389/fimmu.2019.00594. Published 2019 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pardi N., Hogan M.J., Porter F.W., Weissman D. mRNA vaccines - a new era in vaccinology. Nat. Rev. Drug Discov. 2018;17:261–279. doi: 10.1038/nrd.2017.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corbett K.S., et al. SARS- CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature. 2020;586(7830):567–571. doi: 10.1038/s41586-020-2622-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polack F.P., Thomas S.J., Kitchin N., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baden L.R., El Sahly H.M., Essink B., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine [published online ahead of print, 2020 Dec 30] N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2035389. 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Su Q., Igyártó B.Z. One-step artificial antigen presenting cell-based vaccines induce potent effector CD8 T cell responses. Sci. Rep. 2019;9(1):18949. doi: 10.1038/s41598-019-55286-5. Published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uhlig K.M., Schülke S., Scheuplein V.A., et al. Lentiviral protein transfer vectors are an efficient vaccine platform and induce a strong antigen-specific cytotoxic T cell response. J. Virol. 2015;89(17):9044–9060. doi: 10.1128/JVI.00844-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaur S.P., Gupta V. COVID-19 Vaccine: a comprehensive status report. Virus Res. 2020;288:198114. doi: 10.1016/j.virusres.2020.198114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Logunov D.Y., Dolzhikova I.V., Shcheblyakov D.V., et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia [published online ahead of print, 2021 Feb 2] Lancet. 2021 doi: 10.1016/S0140-6736(21)00234-8. S0140–6736(21)00234-00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Voysey M., Clemens S.A.C., Madhi S.A., et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK [published correction appears in Lancet. 2021 Jan 9;397(10269):98] Lancet. 2021;397(10269):99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 31.https://www.who.int/publications/m/item/who-target-product-profiles-for-covid-19-vaccines
- 32.Yu J., et al. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science. 2020 Aug 14;369(6505):806–811. doi: 10.1126/science.abc6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Doremalen N., Purushotham J., Schulz J., et al. 2021. Intranasal ChAdOx1 nCoV-19/AZD1222 Vaccination Reduces Shedding of SARS-CoV-2 D614G in Rhesus Macaques; p. 2021. Preprint. bioRxiv. 01.09.426058. Published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586(7830):516–527. doi: 10.1038/s41586-020-2798-3. [DOI] [PubMed] [Google Scholar]
- 35.Mehrotra D.V., Janes H.E., Fleming T.R., et al. Clinical endpoints for evaluating efficacy in COVID-19 vaccine trials. Ann. Intern. Med. 2021;174(2):221–228. doi: 10.7326/M20-6169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seow J., et al. Longitudinal evaluation and decline of antibody responses in SARS-CoV-2 infection. Nat. Microbiol. 2020 Dec;5(12):1598–1607. doi: 10.1038/s41564-020-00813-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jackson L.A., Anderson E.J., Rouphael N.G., et al. An mRNA vaccine against SARS-CoV-2 - preliminary report. N. Engl. J. Med. 2020;383(20):1920–1931. doi: 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368(6493):860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burki T. Equitable distribution of COVID-19 vaccines. Lancet Infect. Dis. 2021;21(1):33–34. doi: 10.1016/S1473-3099(20)30949-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lazarus J.V., Ratzan S.C., Palayew A., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020:1–4. doi: 10.1038/s41591-020-1124-9. [published online ahead of print, 2020 Oct 20] [published correction appears in Nat Med. 2021 Jan 11;:] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tegally, H. et al Preprint at medRxiv 10.1101/2020.12.21.20248640 (2020). [DOI]
- 42.Davies, N. G. et al Preprint at medRxiv 10.1101/2020.12.24.20248822 (2020).. [DOI]
- 43.Andreano E., Piccini G., Licastro D., et al. 2020. SARS-CoV-2 Escape in Vitro from a Highly Neutralizing COVID-19 Convalescent Plasma; p. 2020. Preprint. bioRxiv. 12.28.424451. Published 2020 Dec 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vasques Nonaka, C.K.; Miranda Franco, M.; Gräf, T.; Almeida Mendes, A.V.; Santana de Aguiar, R.; Giovanetti, M.; Solano de Freitas Souza, B. Genomic Evidence of a Sars-Cov-2 Reinfection Case with E484K Spike Mutation in Brazil. Preprints 2021, 2021010132 (doi: 10.20944/preprints202101.0132.v1).
- 45.Sabino E.C., Buss L.F., Carvalho M.P.S., et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence [published online ahead of print, 2021 Jan 27] Lancet. 2021 doi: 10.1016/S0140-6736(21)00183-5. S0140–6736(21)00183-00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shields A.M., Burns S.O., Savic S., Richter A.G., UK PIN COVID-19 Consortium COVID-19 in patients with primary and secondary immunodeficiency: the United Kingdom experience [published online ahead of print, 2020 Dec 15] J. Allergy Clin. Immunol. 2020 doi: 10.1016/j.jaci.2020.12.620. S0091–6749(20)32406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038 [published correction appears in Lancet. 2020 Mar 28;395(10229):1038] Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Capobianco G., Saderi L., Aliberti S., et al. COVID-19 in pregnant women: a systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;252:543–558. doi: 10.1016/j.ejogrb.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bottazzi B., Riboli E., Mantovani A. Aging, inflammation and cancer. Semin. Immunol. 2018;40:74–82. doi: 10.1016/j.smim.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 50.Haq K., McElhaney J.E. Immunosenescence: influenza vaccination and the elderly. Curr. Opin. Immunol. 2014;29:38–42. doi: 10.1016/j.coi.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 51.Anderson E.J., Rouphael N.G., Widge A.T., et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N. Engl. J. Med. 2020;383(25):2427–2438. doi: 10.1056/NEJMoa2028436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taylor M.M., Kobeissi L., Kim C., et al. Inclusion of pregnant women in COVID-19 treatment trials: a review and global call to action [published online ahead of print, 2020 Dec 16] Lancet Glob Health. 2020 doi: 10.1016/S2214-109X(20)30484-8. S2214–109X(20)30484-30488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Public health emergency SOLIDARITY trial of treatments for COVID-19 infection in hospitalized patients. http://www.isrctn.com/ISRCTN83971151 (Accessed on January 20, 2021). no abstract available.
- 54.Zimet G.D., Silverman R.D., Fortenberry J.D. Coronavirus disease 2019 and vaccination of children and adolescents: prospects and challenges [published online ahead of print, 2020 Nov 5] J. Pediatr. 2020 doi: 10.1016/j.jpeds.2020.11.002. S0022–3476(20)31379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.ClinicalTrials.gov Identifier: NCT04649151.
- 56.ClinicalTrials.gov Identifier: NCT04368728.
- 57.Duclos P. A global perspective on vaccine safety. Vaccine. 2004;22(15–16):2059–2063. doi: 10.1016/j.vaccine.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 58.Kliks S.C., Nimmanitya S., Nisalak A., Burke D.S. Evidence that maternal dengue antibodies are important in the development of dengue hemorrhagic fever in infants. Am. J. Trop. Med. Hyg. 1988;38:411–419. doi: 10.4269/ajtmh.1988.38.411. [DOI] [PubMed] [Google Scholar]
- 59.Polack F.P., Hoffman S.J., Crujeiras G., Griffin D.E. A role for nonprotective complement-fixing antibodies with low avidity for measles virus in atypical measles. Nat. Med. 2003;9(9):1209–1213. doi: 10.1038/nm918. [DOI] [PubMed] [Google Scholar]
- 60.Sariol A., Perlman S. Lessons for COVID-19 immunity from other coronavirus infections. Immunity. 2020;53:248–263. doi: 10.1016/j.immuni.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Robinson W.E., Jr., Montefiori D.C., Mitchell W.M. Antibody-dependent enhancement of human immunodeficiency virus type 1 infection. Lancet. 1988;1:790–794. doi: 10.1016/s0140-6736(88)91657-1. [DOI] [PubMed] [Google Scholar]
- 62.Lee W.S., Wheatley A.K., Kent S.J., DeKosky B.J. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat. Microbiol. 2020 Oct;5(10):1185–1191. doi: 10.1038/s41564-020-00789-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu L., et al. Anti-spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight. 2019 Feb 21;4(4) doi: 10.1172/jci.insight.123158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Q., Zhang L., Kuwahara K., et al. Immunodominant SARS coronavirus epitopes in humans elicited both enhancing and neutralizing effects on infection in non-human primates [published correction appears in ACS Infect Dis. 2020 may 8;6(5):1284-1285] ACS Infect. Dis. 2016;2(5):361–376. doi: 10.1021/acsinfecdis.6b00006. [DOI] [PMC free article] [PubMed] [Google Scholar]