Abstract
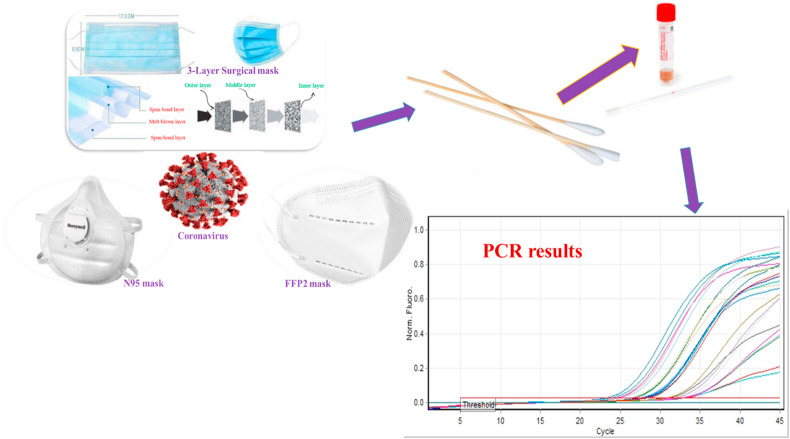
One of the simplest and most effective individual measures is to wear a mask to prevent the spread of respiratory droplets from carriers to healthy people and patients admitted to corona wards and their staff. This research aimed to investigate the contamination of internal and external surfaces of various masks used by patients and staff with SARS coronavirus, as well as the possibility of airborne transmission in Imam Khomeini Hospital, Ardabil. For this purpose, twenty-five staff members and ten patients participated voluntarily in this cross-sectional study. Sampling was performed using swaps on both sides (inside and outside) of various surgical masks, N-95, and filtering face piece FFP2 through standard methods in compliance with the relevant conditions and from a surface of at least 5 cm2. Next, the collected samples were immediately transferred to a laboratory and analyzed by real-time PCR method to detect the presence of SARS-CoV-2 virus after viral genome extraction. Based on the obtained results, from a total of 30 collected samples (25 of personnel masks plus 5 samples of hospitalized patients’ masks). A total of 60 masks were sampled. For every collected sample, the researchers studied both inside and outside of the mask. Upon analyzing the data, it was showed that 6 mask samples were positive for the presence of coronavirus. Nonetheless, all samples taken from both inside and outside of the personnel masks (N-95 and FFP2 types of masks) were negative. Among the 6 positive samples, four cases were related to the internal part, one case to the outer part of the three-layer surgical masks, and one to the outer part of the N-95 masks in hospitalized patients. As masks reduce the concentration of virus particles, they can play an important role in creating immunity.
Keywords: COVID-19, Face masks, Control, Prevention
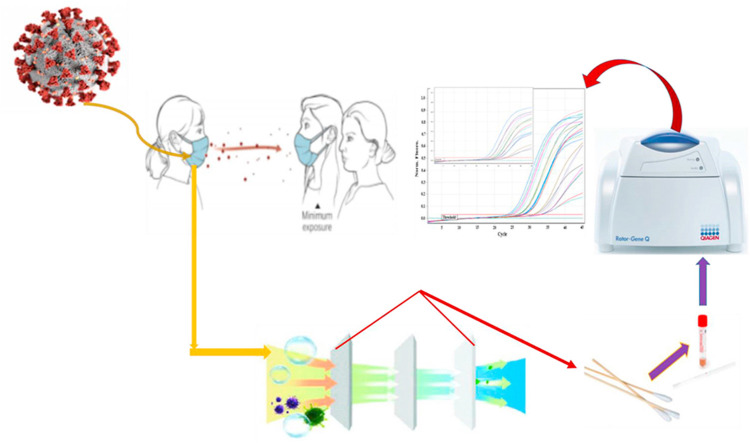
Graphical abstract
1. Introduction
Since 2019, the whole world has been astonished by a new virus called COVID-19 that can cause the severe respiratory syndrome. Studies show that this member of coronaviruses has a close relationship with animals such as bats (Chan et al., 2020; Cheng et al., 2020a). Actually, 72 days after the announcement of the first patient in Wuhan (China), on March 11, 2020, the World Health Organization (WHO) declared COVID-19 as a pandemic (https://www.who.int/dg/sp, 2020). The COVID-19 disease is mainly characterized by symptoms such as fever, dry cough, and shortness of breath. Some symptoms like nausea, vomiting, abdominal discomfort, and diarrhea are listed, but they are not very typical in this disease (Bai et al., 2020; Kotfis and Skonieczna-Żydecka, 2020). Airborne transmission is one of the three commonly accepted modes of viral transmission (Morawska et al., 2020). But there is no certain study that approves the airborne transmission of coronavirus (Lewis, 2020; Morawska and Cao, 2020). The basic reproduction number of the new coronavirus is estimated to be in the range between 1.4 and 3.9, and the infectivity of the virus is higher than seasonal influenza (0.9e2.1) and Middle East Respiratory Syndrome (MERS) (0.29e1.44), and is close to Severe Acute Respiratory Syndrome (SARS) (~3) (Feng et al., 2020). According to the WHO, there is no decisive medication for the novel coronavirus, so people are obliged to follow preventive measures (Luo et al., 2020). As a non-pharmaceutical intervention (NPI) measure, masks can be effective to reduce the risk of infections, lots of studies like (Jefferson et al.) have shown that wearing a mask can be one of the important barriers to transmission of respiratory viruses (Jefferson et al., 2011). There are some studies that show the use of masks significantly reduces the risk of diseases like SARS and influenza (MacIntyre et al., 2009; Zhang et al., 2013). We know that the size of SARS-CoV-2 is approximately 120 nm, so it is 10–50 times smaller than Staphylococcus auras. In fact, the size of the virus does not play a critical role because the pathogen test for the effectiveness of surgical masks shows that the virus is on droplets (Sommerstein et al., 2020a). There are different types of masks used in this pandemic, including medical masks such as N-95 respirators, cloth (homemade) masks, surgical face masks, FFP2 masks, FFP2 with expiratory valve (Luo et al., 2020; Sommerstein et al., 2020a; Jiang et al., 2020). To prevent coivd-19 infection, cloth masks are not recommended because the infection-test rate is very high on both parts of masks in comparison with the medical and surgical masks (Luo et al., 2020; MacIntyre et al., 2015). Overall, wearing a mask is very effective, and it is strongly recommended that the public wear the mask during this pandemic, even homemade masks with low efficiency (Eikenberry et al., 2020). As the respiratory system function is like an air pump and masks act as a filter, the COVID-19 outbreak rate can be reduced by wearing masks. Accordingly, this research aimed to explore whether different types of masks can prevent the spread of COVID-19 or not.
2. Materials and methods
2.1. Approval statement
This project was approved to by ethic code IR. ARUMS.REC.1399.249 in accordance to the ethical principles and the national norm and standards for conducting medical research in Iran.
2.2. Specimen collection, storage, and transfer
This study was performed in the corona ward of Imam Khomeini hospital in Ardabil city. Ardabil is one of the cities affected by the Corona outbreak and has been frequently under red alert. Ardabil city is the capital of Ardabil province, located in the northwest of Iran. Its population is about 625,000 people.
This research investigated the presence of coronavirus on the surface of the masks studying the corona ward staff and patients in the hospital. The inclusion criteria were only patients with severe form of COVID 19 who were hospitalized in the intensive care unit and the staff working in this department in the morning and evening shifts. Other patients with other conditions and other respiratory infections were excluded from the study. All of these patients were men over 65 years old. Overall, 25 staff members and 5 patients of the corona ward participated in this study voluntarily. Samples taken for each person included the inside and outside of the masks, so a total of 60 mask samples were collected and analyzed. At first, the staff was justified not to touch their mask surface at all while working. The staff, who touched their masks, were excluded from the study. The staff who wore face shield were excluded from this study. As the maximum shift time per person lasts for 8 h and health protection protocols do not recommend wearing a mask for more than 8 h, sampling was done after at least 8 h of face covering. Initially, the masks were completely sterile, and while wearing a new mask, great care was taken not to touch it. Some participants could be corona positive and have the virus in their mask, so samples were taken from both sides of the mask at the end of the shift. Participants with a positive result in their masks were tested for their corona infection.
For this study, 60 samples were taken from 30 masks (inner and outer side). Twenty-five samples from staff and 10 from patients’ masks. The samples were taken from different kinds of used masks in hospitals. Three kinds of masks were examined (three-layer surgery mask, N-95 mask, and FFTP mask). In the first step, we took the swap out of the package and moistened it with the virus transmission medium. We rotated the wet swab with sufficient pressure in at least two different directions and prevented the swap from drying out. A minimum surface of 5 cm2 (central part of the mask) was selected for swapping. After sampling, each swab was placed in Eppendorf tubes containing 300 μL of the sterile viral transport medium (containing 200 mL of double distilled sterile water mixed with protein stabilizer, antibiotic, and buffer solution). The swap samples were placed in a clean bag and sealed. The outer surface of the bag was disinfected with 80–60% ethanol, 80% isopropyl alcohol, or 5% sodium hypochlorite solution and then placed in another package. The prepared samples were maintained at 4 °C until delivery to the virology laboratory. We also collected control samples along with the experimental samples.
2.3. Positive and negative control
The first set of control sample collection was performed in the same way including opening the package and removing the swab from the tube, but no sampling was done from any mask. The second set of control samples involved closed swap packages which were stored and tested with mask samples, simultaneously. The samples were centrifuged in the laboratory for 4 min at 12,000 rpm and then the supernatant was discarded and the remaining microtubule was extracted using the high pure viral nucleic acid kit. By means of the cDNA synthesis kit, we made cDNA and used appropriate primers designed for N and ORF1ab genes to perform PCR and Real-time.
2.4. Viral genome extraction
Virus genome extraction was performed using a nucleic acid extraction kit (Gene favor) and the extracted genomes were placed in the freezer at - 70 °C for the next step.
2.5. Running real-time PCR and data analyses
The extracted genome was placed in the reaction micro-tube along with other reaction components to detect the SARS-CoV-2 virus. Then the real-time PCR results were interpreted based on the kit protocol and then the positive and negative results were determined. The following steps were performed for virus identification: at the first stage, the appropriate concentrations of reagents, temperature cycle, and a sufficient number of replication cycles were performed for the initial screening stage. The specific primer and probe real-time reverse transcriptase-polymerase chain reaction (RTPCR) targeting ORF1ab and N genes (Nucleoprotein gene) Applied Biosystems™ Real-Time PCR System 7500 with software v2.0.5 was used to run RTPCR. Appropriate concentrations of the synthesis reaction for real-time PCR MasterMix: Per reaction H2O (RNAse free) 0.6 μl 2x Reaction mix 12.5 μl MgSO4 (50 mM) 0.4 μl BSA (1 mg/mL) 1 μl Primer ORF1a/b _SARSr-F (10 μM stock solution) 1.5 μl GTGARATGGTCATGTGTGGCGG Primer ORF1a/b _SARSr-R (10 μM stock solution) 2 μl CARATGTTAAASACACTATTAGCATA Probe RdRP_SARSr-P1 (10 μM stock solution) 0.5 μl FAM- CCAGGTGGWACRTCATCMGGTGATGC- BBQ Probe RdRP_ SARSr-P2 (10 μM stock solution) 0.5 μl FACAGGTGGAACCTCATCAGGAGATGC-BBQ, Probe nCOV_2019, N gene F primerAAATTTTGGGGACCAGGAAC, 2019n-COV,N gene R primer TGGCAGCTGTGTAGGTCAAC, Taq EnzymeMix 1 μl, Template RNA, add 5 μl, Total reaction mix 20 μl. Thermal Cycler: 55 °C 10′ 94 °C 3′ 94 °C 15″ 58 °C 30″ 45x (Table 1 ). It is worth mentioning that all tests were operated in accordance with national safety protocols. Schematic presentation of sampling from masks of patients and staff in corona wards are presented in Fig. 1 .
Table 1.
Primers and probes used in this study.
| Organisms | Target gene | Sequence (5′–3′) | Cycling parameters |
|---|---|---|---|
| SARS-CoV-2 | Probe & Primer ORF1a/b |
FACAGGTGGAACCTCATCAGGAGATGC-BBQ F-GTGARATGGTCATGTGTGGCGG R-CARATGTTAAASACACTATTAGCATA |
55 °C 10′ 94 °C 3′ 94 °C 15″ 58 °C 30″ 45x. |
| Primer &Probe N gene |
F-AAATTTTGGGGACCAGGAAC R-TGGCAGCTGTGTAGGTCAA PFAM-ATGTCGCGCATTGGCATGGA-BHQ |
55 °C 10′ 94 °C 3′ 94 °C 15″ 58 °C 30″ 45x. |
Fig. 1.
Schematic presentation of sampling from masks of patients and staff in corona wards.
3. Results
In the present study, 50 samples of face masks (25 samples from the inside part and 25 samples from the outside part of the mask) were sampled to detect the COVID-19 virus (Table 2 ). The results showed that all samples of the studied masks (three-layer surgical, N-95 and FFP2 masks) were negative in terms of the virus presence (Table 2). In this study, sampling was performed every 8 h (in morning and evening shifts). It should be noted that the type of hospital ventilation system at the time of sampling was also mechanical/natural. Moreover, 5 mask samples (five samples from the inside part and five samples from the outside part of the masks) were sampled to check the COVID-19 presence in the masks of infected patients at the hospital. The results showed that the inside parts of all samples were positive for the presence of SARS-CoV-2. However, only one sample of the outlet part of the masks (three-layer surgical mask sample) was positive for the presence of SARS-CoV-2 (Table 3 ). The information about environment status at the time of sampling from the inside and outside of different types of masks examined to identify SARS-CoV-2 is presented in Table 4 . According to Table 4, the temperature and relative humidity at the time of sampling in different wards of the hospital were between 19.5 and 28 °C and 33–41%, respectively. The results of the other study related to masks used the prevention of the spread of COVID-19 are summarized in Table 5 .
Table 2.
SARS-CoV-2 in the masks samples of hospital medical staff.
| Mask types | Sampling section | Occupation of medical staff | Number of samples | Results |
|---|---|---|---|---|
| 3-Layer Surgical | Inside | Nurse | S1 | Negative |
| Nurse | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Sampler | S4 | Negative | ||
| Corona ward nurse | S5 | Negative | ||
| Service staff | S6 | Negative | ||
| Nurse | S7 | Negative | ||
| Corona Emergency Nurse | S8 | Negative | ||
| Corona Emergency Nurse | S9 | Negative | ||
| Nurse | S10 | Negative | ||
| Nurse | S11 | Negative | ||
| Outside | Nurse | S1 | Negative | |
| Nurse | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Sampler | S4 | Negative | ||
| Corona ward nurse | S5 | Negative | ||
| Service staff | S6 | Negative | ||
| Nurse | S7 | Negative | ||
| Corona Emergency Nurse | S8 | Negative | ||
| Corona Emergency Nurse | S9 | Negative | ||
| Nurse | S10 | Negative | ||
| Nurse | S11 | Negative | ||
| N-95 | Inside | Nurse | S1 | Negative |
| Corona ward physician | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Nurse | S4 | Negative | ||
| Nurse | S5 | Negative | ||
| Nurse | S6 | Negative | ||
| Corona ward nurse | S7 | Negative | ||
| Corona Emergency Nurse | S8 | Negative | ||
| Service staff | S9 | Negative | ||
| Physician | S10 | Negative | ||
| Outside | Nurse | S1 | Negative | |
| Corona ward physician | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Nurse | S4 | Negative | ||
| Nurse | S5 | Negative | ||
| Nurse | S6 | Negative | ||
| Corona ward nurse | S7 | Negative | ||
| Corona Emergency Nurse | S8 | Negative | ||
| Service staff | S9 | Negative | ||
| Physician | S10 | Negative | ||
| FFP2 | Inside | Nurse | S1 | Negative |
| Service staff | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Nurse | S4 | Negative | ||
| Outside | Nurse | S1 | Negative | |
| Service staff | S2 | Negative | ||
| Nurse | S3 | Negative | ||
| Nurse | S4 | Negative |
Table 3.
SARS-CoV-2 in the mask samples of people infected with coronavirus.
| Mask types | Sampling section | Number of samples | Ct- ORF1ab gene | Ct- N gene | Results |
|---|---|---|---|---|---|
| 3-Layer Surgical | Inside | S1 | 36.83 | 35.58 | Positive |
| S2 | 34.99 | 33.5 | Positive | ||
| S3 | 34.35 | 33.23 | Positive | ||
| S4 | 33.62 | 32.42 | Positive | ||
| Outside | S1 | 34.39 | 33.92 | Positive | |
| S2 | – | – | Negative | ||
| S3 | – | – | Negative | ||
| S4 | – | – | Negative | ||
| N95 | Inside | S1 | 31.42 | 28.61 | Positive |
| Outside | S1 | – | – | Negative |
Table 4.
Environmental status information at the time of sampling from the inside and outside of different types of masks examined for identify SARS-CoV-2.
| Mask types | Occupation of medical staff | Number of samples | Status of windows | Ventilation system | Temperature (°C) | Relative humidity (%) | Results |
|---|---|---|---|---|---|---|---|
| 3-Layer Surgical | Nurse | 12 | Close | Mechanical/Natural | 21.5–27.8 | 35.0–40.0 | Negative |
| Sampler | 2 | Close | Mechanical/Natural | 27.1 | 36.0 | Negative | |
| Corona ward nurse | 2 | Close | Mechanical/Natural | 25.4 | 34.0 | Negative | |
| Service staff | 2 | Close | Mechanical/Natural | 26.9 | 39.0 | Negative | |
| Corona Emergency Nurse | 4 | Close | Mechanical/Natural | 25.5–28.0 | 38.0–40.0 | Negative | |
| N-95 | Nurse | 10 | Close | Mechanical/Natural | 24.6–27.3 | 35.0–41.0 | Negative |
| Corona ward physician | 2 | Close | Mechanical/Natural | 26.8 | 36.0 | Negative | |
| Corona ward nurse | 2 | Close | Mechanical/Natural | 25.5 | 35.0 | Negative | |
| Corona Emergency Nurse | 2 | Close | Mechanical/Natural | 28.0 | 41.0 | Negative | |
| Physician | 2 | Close | Mechanical/Natural | 24.9 | 36.0 | Negative | |
| Service staff | 2 | Close | Mechanical/Natural | 27.3 | 40.0 | Negative | |
| FFP2 | Nurse | 6 | Close | Mechanical/Natural | 25.5–27.8 | 34.0–37.0 | Negative |
| Service staff | 2 | Close | Mechanical/Natural | 27.0 | 36.0–41.0 | Negative | |
| 3-Layer Surgical | People infected with Covid-19 | 8 | Close | Mechanical/Natural | 19.5–25.8 | 33.0–36.0 | 5S. Positive |
| N95 | People infected with Covid-19 | 2 | Close | Mechanical/Natural | 20.3–24.5 | 34.0–35.0 | 1S. Positive |
Table 5.
Summary results of the other study related to masks used for prevention of spread of COVID-19.
| Raw | Study area | Finding | Ref |
|---|---|---|---|
| 1 | Canada | N95 respirators had clearly more effective than medical masks. | 23 |
| 2 | USA | The results of this study showed that wearing a face mask can be effectively decrease the slope of spreading. | 33 |
| 3 | China | High quality standard surgical masks appear to be as effective as FFP2 masks in preventing health care workers from SARS. | 27 |
| 4 | China | Study results indicate that surgical face masks could prevent transmission of human coronaviruses and influenza viruses from symptomatic individuals. | 34 |
| 5 | China | A meta-analysis of randomized controlled trials showed that surgical masks and N95 respirators were similarly effective in preventing influenza-like illness and laboratory-confirmed influenza among healthcare workers | 18 |
| 6 | USA | Mask effectiveness for respiratory infection prevention is stronger in health care than community. N95 masks might reduce SARS-CoV-1 risk vs. surgical masks in health care settings; however, applicability to SARS-CoV-2 is uncertain. | 35 |
| 7 | USA | Community-wide mask wearing may contribute to the control of COVID-19 by reducing the amount of emission of respiratory droplets from persons with subclinical or mild COVID-19. | 2 |
| 8 | Iran | All samples taken from both inside and outside of the personnel masks were negative (N-95 and FFP2 types of masks). Four positive samples were found on the internal part, one case was related to the outer part of the three-layer surgical masks and the last case were related to the outer part of the N-95 masks in hospitalized patients. | This study |
4. Discussion
During the SARS-CoV-2 pandemic, great numbers of facemasks may be essential to be used for long times to prevent people from infections (Long et al., 2020). In this study, we have investigated the presence of coronavirus on the surface of the masks using the corona ward staff and patients in the hospital. The results showed that not only the inside part of all patients’ samples was positive for the presence of SARS-CoV-2 but also two samples of the outside part of the masks (one N-95 sample and one three-layer surgical mask sample) were positive for the presence of SARS-CoV-2.
The use of N-95 facemask possibly results in uneasiness, headaches, nausea, and vomiting. A former study (Chen et al., 2017) reported that there was a reverse connection between the level of compliance with wearing an N-95 facemask and the risk of clinical respiratory illness. It is challenging to ensure high agreement due to this discomposure of N-95 facemask in all studies. Among the available literature, some have indicated that airborne transmission of the COVID-19 virus can potentially occur (Cheng et al., 2020b; Ong et al., 2020). However, a possible hypothesis is that since the diameter of the ritual pores of the mask is larger than the diameter of the virus, there is a possibility of virus particles leaking into the outer layer of the mask. The pore size in N-95 masks is generally 100–300 nm, while the diameter of SARS-CoV-2 viral particles is 120 nm and the virus may be present from an infected person no longer in the space but still in the air you are breathing (Infectious disease physic, 2020). Although the benefit of population-level public facial masking to protect others during the COVID-19 pandemic has received a great deal of attention, low certainty evidence suggests that medical masks and N-95 respirators offer similar protection against viral respiratory infection including coronavirus in healthcare workers during non–aerosol-generating care (Bartoszko et al., 2020). Airborne model testing indicated that surgical masks, cotton masks, and N-95 masks provide some safety from the transmission of infective COVID-19 however; medical masks (surgical masks and even N-95 masks) could not entirely block the transmission of virus aerosols/droplets even when closed (Ueki et al., 2020). Yu Wang et al. investigated transmission of COVID-19 within relatives and close contacts responsible for the widespread growth of the epidemic and found that use of face mask by the primary case and family contacts before the primary case developed symptoms was 79% effective in reducing transmission (Wang et al., 2020). Similar studies have shown face mask use could result in a large reduction in risk of infection with robust connotations with N95 or similar masks compared with reusable surgical masks or similar (Chu et al., 2020). Masks differ principally in their maximum internal leak proportion limit. Masks such as filtering facepiece (FFP) masks were designed to protect healthcare-workers, while three layer surgical masks were originally proposed to protect patients. So far, no direct trial with these masks has been published for SARS-CoV-2. Both of them can protect the individual from large sprays and droplets neither these type mask completely inhibits transmission, which may be due to unsuitable usage and different transmission pathways (Sommerstein et al., 2020b; Smereka et al., 2020). Due to the fact that masks reduce the concentration of virus particles, they may play an important role in creating immunity. The current project aimed to evaluate the effectiveness of types of respirators and the possibility of air-born transmission of SARS-CoV-2. Concerning the temperature and relative humidity at the time of sampling in different wards of the hospital, they were maintained between 19.5 and 28 °C and 33–41%, respectively (Table 4 ). The results of a paper from University of Nicosia, disclose that a major decline of virus viability happens when both high temperature and low relative humidity co-occur (Dbouk and Drikakis, 2020). The respiratory droplets can travel over distance and their concentration persists significant at any temperature if the relative humidity is high. This finding is in contradiction with what was previously supposed by many epidemiologists (Dbouk and Drikakis, 2020). Casanova et al. used the transmissible gastroenteritis virus (TGEV) and mouse hepatitis virus (MHV) to determine effects of air temperature and relative humidity on the persistence of coronaviruses over the environment (Casanova et al., 2010). At 4 °C, the infectious virus persisted for as long as 28 days, and the lowest level of inactivation occurred at 20% relative humidity. Inactivation was more rapid at 20 °C than 4 °C for all humidity levels. Viruses persisted for 5–28 days and the slowest inactivation occurred at low relative humidity (Casanova et al., 2010; Dargahi et al., 2021). In the study by Mecenas et al. excessive similarity was observed in the findings concerning the effect of temperature and humidity on the seasonal transmissibility and viability of COVID-19. This research along with other similar studies consistently agree that cold and dry environments increase the power of virus spread while warm and wet climates appear to decrease the spread of COVID-19 (Mecenas et al., 2020).
Table 5 summarizes of results obtained by other studies related to masks used to prevent COVID-19 spread. Accordingly, most of these studies report that wearing a face mask can efficiently reduce the slope of SARS-CoV-2 virus spread. These studies also indicate that wearing surgical face masks and N95 respirators can prevent the transmission of human coronaviruses and influenza viruses as effectively as FFP2 masks (Li et al., 2020; Leung et al., 2020; Chou et al., 2020).
There are several limitations in this study; first, the number of sampling concentrating on the community was small. Second, sensitivity data displayed unbalanced results for preparation so more research on mask structures is necessary to propose ways of overcoming the weaknesses of current masks and design optimal and useful masks.
5. Conclusion
Wearing masks is a part of physical preventive measures that may help decrease the spread of corona virus from respiratory excretions. Although wearing a facemask alone is not adequate to offer safety or source control, and other individual and community level measures should also be observed to cease SARS-CoV-2 transmission. However, a possible hypothesis is that since the diameter of the ritual pores of the mask is larger than the diameter of the virus, there is a possibility of virus particles leaking into the outer layer of the mask.
Credit author statement
Chiman karami, Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Supervision, Funding acquisition. Farhad Jeddi, Methodology. Abdollah Dargahi & Mehdi Vosoughi, Methodology, Validation, Formal analysis, Writing – original draft. Mehdi Sarailo, Validation, Formal analysis, Supervision. Aidin hadisi, Methodology. S.Ahamad Mokhtari, Writing - initial drafting. Morteza Alighadri, Formal analysis, Investigation. Somayeh Biparva Haghighi, Formal analysis, writing and text revision.
Funding
This study was financially supported by Ardabil University of Medical Sciences.
Declaration of competing interest
The authors declared no conflict of interest.
Acknowledgement
This study was financially supported by Ardabil University of Medical Sciences. The authors would like to acknowledge all health-care workers who collaborated in the diagnosis and treatment of patients in corona wards in Iran.
References
- Bai Y., Yao L., Wei T., Tian F., Jin D.-Y., Chen L., et al. Presumed asymptomatic carrier transmission of COVID-19. 2020;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartoszko J.J., Farooqi M.A.M., Alhazzani W., Loeb M. Medical masks vs N95 respirators for preventing COVID‐19 in healthcare workers: a systematic review and meta‐analysis of randomized trials. J Influenza other respiratory viruses. 2020;14(4):365–373. doi: 10.1111/irv.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010 May 1;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.-W., Kok K.-H., Zhu Z., Chu H., To K.K.-W., Yuan S., et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Chughtai A.A., MacIntyre C.R. Herd protection effect of N95 respirators in healthcare workers. J Journal of International Medical Research. 2017;45(6):1760–1767. doi: 10.1177/0300060516665491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.-C., Chuang V.W., So S.Y., Chen J.H., Sridhar S., et al. 2020. The Role of Community-wide Wearing of Face Mask for Control of Coronavirus Disease 2019 (COVID-19) Epidemic Due to SARS-CoV-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.-C., Chen J.H., Yip C.C., Chuang V.W., Tsang O.T., et al. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. J Infection Control Hospital Epidemiology. 2020;41(5):493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R., Dana T., Jungbauer R., Weeks C., McDonagh M.S. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings: a living rapid review. Ann. Intern. Med. 2020 Oct 6;173(7):542–555. doi: 10.7326/M20-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. J. Lancet. 2020 doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dargahi A., Jeddi F., Vosoughi M., Karami C., Hadisi A., Mokhtarie S.A., Alighadri M., Haghighi S.B., Sadeghi H. Investigation of SARS CoV-2 virus in environmental surface. Environ. Res. 2021 Jan 23:110765. doi: 10.1016/j.envres.2021.110765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dbouk T., Drikakis D. Weather impact on airborne coronavirus survival. Phys. Fluids. 2020 Sep 1;32(9) doi: 10.1063/5.0024272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., et al. 2020. To Mask or Not to Mask: Modeling the Potential for Face Mask Use by the General Public to Curtail the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S., Shen C., Xia N., Song W., Fan M. Cowling BJJTLRM. Rational use of face masks in the COVID-19 pandemic. 2020;8(5):434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2020. https://www.who.int/dg/speeches/detail/WD-GsoratmboC-M 2020 w-d-g-s-o-r-a-t-m-b-o-c--m-AA.
- Infectious disease physician breaks down coronavirus mask myths. https://news.llu.edu/health-wellness/infectious-disease-physician-breaks-down-coronavirus-mask-myths. 2020
- Jefferson T., Del Mar C.B., Dooley L., Ferroni E., Al‐Ansary L.A., Bawazeer G.A., et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. 2011;7 doi: 10.1002/14651858.CD006207.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang F.-C., Jiang X.-L., Wang Z.-G., Meng Z.-H., Shao S.-F., Anderson B.D., et al. Detection of severe acute respiratory syndrome coronavirus 2 RNA on surfaces in quarantine rooms. J Emerging Infectious Diseases. 2020;26(9):2162. doi: 10.3201/eid2609.201435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotfis K., Skonieczna-Żydecka KJAit. COVID-19: gastrointestinal symptoms and potential sources of SARS-CoV-2 transmission. 2020;52(2):171. doi: 10.5114/ait.2020.93867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H., Chu D.K., Shiu E.Y., Chan K.H., McDevitt J.J., Hau B.J., Yen H.L., Li Y., Ip D.K., Peiris J.M., Seto W.H. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020 May;26(5):676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis D.J.N. Is the coronavirus airborne? Experts can’t agree. 2020;580(7802):175. doi: 10.1038/d41586-020-00974-w. [DOI] [PubMed] [Google Scholar]
- Li T., Liu Y., Li M., Qian X., Dai S.Y. Mask or no mask for COVID-19: a public health and market study. PloS One. 2020 Aug 14;15(8) doi: 10.1371/journal.pone.0237691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Y., Hu T., Liu L., Chen R., Guo Q., Yang L., et al. Effectiveness of N95 respirators versus surgical masks against influenza: a systematic review and meta‐analysis. J. Evid. Base Med. 2020;13(2):93–101. doi: 10.1111/jebm.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo H., Tang Q-l, Shang Y-x, Liang S-b, Yang M., Robinson N., et al. Can Chinese medicine be used for prevention of corona virus disease 2019 (COVID-19)? A review of historical classics, research evidence and current prevention programs. 2020:1–8. doi: 10.1007/s11655-020-3192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Cauchemez S., Dwyer D.E., Seale H., Cheung P., Browne G., et al. Face mask use and control of respiratory virus transmission in households. 2009;15(2):233. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Seale H., Dung T.C., Hien N.T., Nga P.T., Chughtai A.A., et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. 2015;5(4) doi: 10.1136/bmjopen-2014-006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mecenas P., Bastos R.T., Vallinoto A.C., Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PloS One. 2020 Sep 18;15(9) doi: 10.1371/journal.pone.0238339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J.J.E.I. 2020. Airborne Transmission of SARS-CoV-2: the World Should Face the Reality; p. 105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Tang J.W., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., et al. How can airborne transmission of COVID-19 indoors be minimised? 2020;142:105832. doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y., et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. J Jama. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smereka J., Ruetzler K., Szarpak L., Filipiak K.J., Jaguszewski M., Analgesia Role of mask/respirator protection against SARS-CoV-2. J. Anesth. 2020 doi: 10.1213/ANE.0000000000004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerstein R., Fux C.A., Vuichard-Gysin D., Abbas M., Marschall J., Balmelli C., et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. 2020;9(1):1–8. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerstein R., Fux C.A., Vuichard-Gysin D., Abbas M., Marschall J., Balmelli C., et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. J Antimicrobial Resistance. 2020;9(1):1–8. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueki H., Furusawa Y., Iwatsuki-Horimoto K., Imai M., Kabata H., Nishimura H., et al. Effectiveness of face masks in preventing airborne transmission of SARS-CoV-2. J MSphere. 2020;5(5) doi: 10.1128/mSphere.00637-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Tian H., Zhang L., Zhang M., Guo D., Wu W., et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. J BMJ Global Health. 2020;5(5) doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Peng Z., Ou J., Zeng G., Fontaine R.E., Liu M., et al. Protection by face masks against influenza A (H1N1) pdm09 virus on trans-Pacific passenger aircraft, 2009. 2013;19(9):1403. doi: 10.3201/eid1909.121765. [DOI] [PMC free article] [PubMed] [Google Scholar]