Abstract
Environmental noise has been growing in recent years, causing numerous health problems. Highly sensitive environments such as hospitals deserve special attention, since noise can aggravate patients’ health issues and impair the performance of healthcare professionals. This work consists of a systematic review of scientific articles describing environmental noise measurements taken in hospitals between the years 2015 and 2020. The researchers started with a consultation of three databases, namely, Scopus, Web of Science, and ScienceDirect. The results indicate that for the most part, these studies are published in journals in the fields of medicine, engineering, environmental sciences, acoustics, and nursing and that most of their authors work in the fields of architecture, engineering, medicine, and nursing. These studies, which are concentrated in Europe, the Americas, and Asia, use as reference values sound levels recommended by the World Health Organization. Leq measured in hospital environments showed daytime values ranging from 37 to 88.6 dB (A) and nighttime values of 38.7 to 68.8 dB (A). Leq values for outdoor noise were 74.3 and 56.6 dB (A) for daytime and nighttime, respectively. The measurements were taken mainly inside hospitals, prioritizing more sensitive departments such as intensive care units. There is a potential for growth in work carried out in this area, but research should also include discussions about guidelines for improvement measures aimed at reducing noise in hospitals.
Graphical abstract
Keywords: Noise pollution, Acoustics, Hospital environment, Public health, Environmental noise, Sound pressure level
Introduction
Over the last few decades, noise pollution has grown mainly due to urban expansion and the increasing size of vehicle fleets, which is considered an aggravating factor for public health (Hanninen et al. 2014). Several problems related to human health and cognitive activities are attributed to noise, such as sleep disturbance (Muzet 2007; Basner and McGuire 2018), annoyance (Miedema and Oudshoorn 2001; Licitra et al. 2016; Guski et al. 2017; Paiva et al. 2019), cardiovascular diseases (Babisch et al. 2005; Dratva et al. 2012; Sorensen et al. 2017; Héritier et al. 2018; van Kempen et al. 2018; Lin et al. 2020), perception, and learning (Erickson and Newman 2017; Minichilli et al. 2018).
There is even a greater concern in areas considered sensitive to noise, such as hospitals, where noise affects the well-being of patients, slowing their recovery, reducing the productivity of professionals, and increasing the occurrence of medical errors (Hsu et al. 2012; Loupa et al. 2019; Montes-González et al. 2019; Loupa 2020). Moreover, noise can also have a negative effect on visitors and the hospital as a whole (Zannin et al. 2019) and can increase the incidence of rehospitalization (Hagerman et al. 2005). The main factors involved in noise audible inside hospitals may originate outdoors, e.g., vehicle traffic, or indoors, e.g., conversations among employees and/or patients (Ravindra et al. 2016).
Several studies on environmental noise measurements in hospitals that have been carried out around the world (Busch-Vishniac et al. 2005; Fortes-Garrido et al. 2014; Zannin and Ferraz 2016; Montes-González et al. 2019) have revealed noise levels exceeding those recommended for a healthy environment. The World Health Organization (WHO) suggests that sound levels should not exceed Leq 35 dB (A) in the daytime and Leq 30 dB (A) to Lmax 40 dB (A) at night in hospital environments (Berglund et al. 1999). The United States Environmental Protection Agency (USEPA) recommends daytime and nighttime sound levels of less than Leq 45 and 35 dB (A), respectively (USEPA 1974).
In practice, even with technological advances in hospital equipment and construction processes, noise levels inside hospitals have gradually increased from the 1960s to the present day (Busch-Vishniac et al. 2005; Busch-Vishniac and Ryherd 2019). Sound level assessments in hospitals are performed in various ways, given the complexity of hospital environments (Wallis et al. 2019).
The purpose of this systematic review was to survey research conducted between the years 2015 and 2020 pertaining noise measurement in hospitals around the world by examining top ranking scientific and academic journals.
Methods
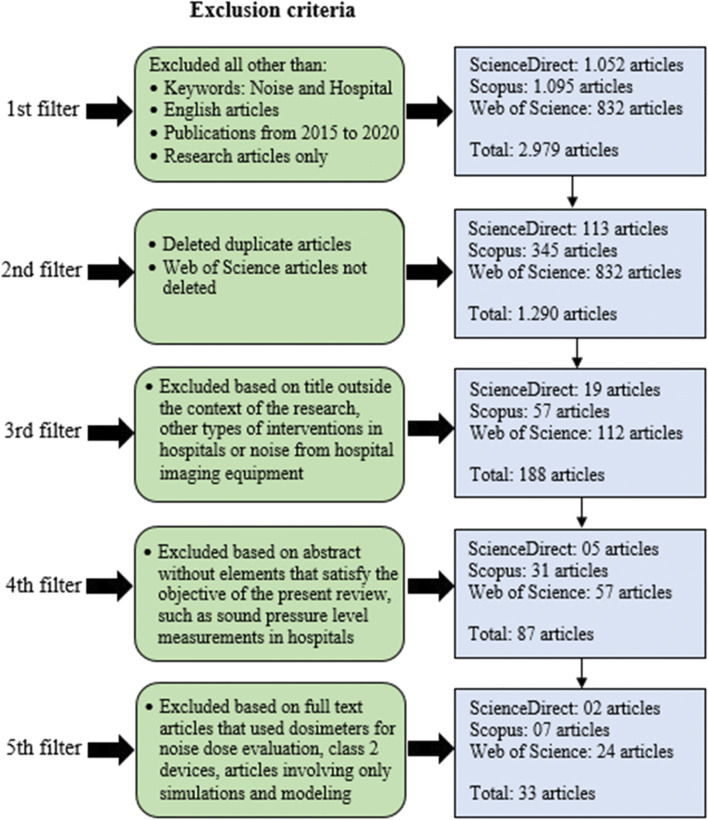
The systematic review of the literature in electronic format involved three databases, Scopus, Web of Science, and ScienceDirect. The first filter employed in the search selected articles published in the last 6 years (from 2015 to 2020), only articles in English, research articles (excluding technical and review notes), and keywords “Noise” and “Hospital.” The second filter excluded duplicate articles, while articles found in the Web of Science database were kept as reference (without excluding them). The third filter removed articles containing titles outside the context of the research, such as other types of interventions in hospitals or noise from hospital imaging equipment (e.g., X-ray machines). The fourth filter excluded articles whose abstract did not contain elements that met the objective of this review, such as those that did not measure sound pressure levels outside or inside hospitals. Lastly, in the fifth filter, after the articles were read in full, those stating that their authors had taken measurements using noise dosimeters (that evaluated only the noise dose) were excluded, since this is a special device for measuring individual exposure to sound pressure levels. Research that used class 2 equipment was excluded in order to equalize the work in terms of quality and quantity of resources of class 1 equipment. Also excluded were articles involving only simulations and modeling, but not measurements.
The articles selected after applying the five filters revealed the following information: (a) the databases containing the largest number of published articles; (b) the areas of knowledge of the journals in which the articles are published; (c) the countries whose hospitals have been studied and the laws/standards used as reference; (d) the authors’ profession/area of expertise and the main focus of their studies (areas outside or inside hospitals); (e) measurement methods and parameters that were used; (f) works that adopted/proposed noise mitigation measures; and (g) future perspectives for the area. Figure 1 summarizes the literature review filtering scheme, while Appendix 1 Table 6 provides information about all the final articles selected.
Fig. 1.
Literature review filtering scheme
Table 6.
Information about all the final articles selected
| Authors of the studies | Area of knowledge of the scientific journal | City and country of study | Laws/standards of reference | Authors’ field of expertise | Focus of study | Equipment used | Proposed and/or adopted measures |
|---|---|---|---|---|---|---|---|
| Carvalhais et al. 2015 | Environmental science | Porto, Portugal | WHO | Health and environment | Inside 1 hospital (neonatal ICU) | 01-DB Solo-Premium | Proposed and adopted measures |
| Chen 2015 | Acoustics + ultrasound | Several cities in Taiwan | WHO | Architecture | Inside 16 hospitals (several waiting rooms) | Brüel & Kjær Pulse | Proposed one measure |
| Fiedler and Zannin 2015 | Environmental science | Curitiba, Brazil | Curitiba Municipal Law No. 10625/2002 | Environmental acoustics | Outside 2 hospitals | Brüel & Kjær 2250 and 2238 | Proposed measures in simulations |
| Filus et al. 2015 | Medicine | Curitiba, Brazil | NBR 10152/87 | Communication disorders | Inside 1 hospital (emergency room) | Brüel & Kjær 2230 | Proposed measures |
| Lahav 2015 | Medicine | Boston, USA | American Academy of Pediatrics (AAP) | Medicine | Inside 1 hospital (neonatal ICU) | Brüel & Kjær 2250-L | No |
| Monazzam et al. 2015 | Medicine | Teheran, Iran | National Iranian Department of Environment | Occupational, public and environmental health | Outside 3 hospitals | Brüel & Kjær 2230 | Proposed measures |
| Oliveira et al. 2015 | Medicine | Portugal | WHO | Pediatrics | Inside 1 hospital (5 pediatric wards and corridors) | 01 dB Symphonie | No |
| Garrido Galindo et al. 2016 | Medicine | Santa Marta, Colombia | Cited only a national law and several international laws | Environmental systems modeling | Inside 1 hospital (3 ICUs) | Casella CEL-633-C1K1 | No |
| Luetz et al. 2016 | Genetic engineering | Germany | WHO | Medicine | Inside 1 hospital (2 ICU rooms) | XL2 | Adopted measures |
| Pirsaheb et al. 2016 | Engineering | Kermanshah, Iran | NIOSH (98)/EPA (74)/Iranian standards | Engineering (environmental health) | Inside 1 hospital (several points) | TES 1358 | Proposed measures and external studies |
| Shield et al. 2016 | Acoustics + ultrasound | London, England | WHO | Architecture and built environment | Inside 2 hospitals (5 wards) | Norsonic 140 | Proposed measures |
| Shoemark et al. 2016 | Pediatrics | Melbourne, Australia | National standard/American Academy of Pediatrics Committee on Environmental Health/Consensus Committee on Newborn ICU Design | Pediatrics | Inside 2 hospitals (neonatal/pediatric ICU and nursery) | Quest Sound Pro DL | No |
| de Araújo Vieira et al. 2016 | Engineering | João Pessoa, Brazil | NBR 10152/87 | Engineering | Inside, but do not mention number of hospitals (9 adult ICUs) | Brüel & Kjær 2250-L | No |
| Ai et al. 2017 | Civil engineering | Hong Kong, China | Not cited | Engineering | Inside 1 hospital (pediatric dental clinic and lab for dental implants and prosthetics) | Brüel & Kjær 2270 | No |
| Disher et al. 2017 | Ward nursing | Nova Scotia, Canada | Not cited | Nursing | Inside 1 hospital (3 neonatal ICUs and 1 pediatric ICU) | 3 M SoundPro | Proposed measures |
| D’Souza et al. 2017 | Medicine | Udupi, India | EPA/WHO/American Academy of Pediatrics Committees | Nursing | Inside 1 hospital (neonatal ICU) | Brüel & Kjær 2250 | No |
| Galindo et al. 2017 | General medicine | Santa Marta, Colombia | Did not use any, but quoted other authors | Environmental systems modeling | Inside 1 hospital (neonatal ICU) | Casella CEL-633-C1K1 | No |
| Santos et al. 2017 | Environmental science | Northern Portugal | WHO/EPA/American Academy of Pediatrics -AAP | Environmental health | Inside 3 hospitals (neonatal ICU) | 01 dB Solo-Premium | Proposed measures |
| Bevan et al. 2018 | Medicine: pediatrics | Southampton, England | WHO | Clinical and experimental medical sciences | Inside 1 hospital (private rooms) | Brüel & Kjær 2236 | No |
| Predrag et al. 2018 | Engineering | Banja Luka, Bosnia and Herzegovina | National standard | Protection and ecology | Outside 2 hospitals | Brüel & Kjær 2260 | No |
| Bliefnick et al. 2019 | Acoustics + ultrasound | Central USA | WHO | Architectural engineering and construction | Inside 1 hospital (15 patient rooms and 5 nursing stations) | Larson Davis 831 | Proposed and adopted measures |
| Cho et al. 2019 | Medicine | Seoul, South Korea | WHO | Physical metrology | Inside 1 hospital (several points) | Brüel & Kjær 2270 | No |
| Loupa et al. 2019 | Environmental science | Kavala, Greece | Not cited | Air pollution | Inside and outside 1 hospital (several locations) | Casella CEL-490 | No |
| Montes-González et al. 2019 | Environmental science | Badajoz, Spain | WHO/EPA/Spanish legislation | Applied physics | Inside 1 hospital (16 points) | 01 dB OPER@/Brüel & Kjær 2250 L and 2238 | Proposed measures |
| Terzi et al. 2019 | Nursing | Istanbul, Turkey | WHO | Health sciences | Inside 1 hospital (10 ICUs) | Brüel & Kjær 2250-L | No |
| Tezel et al. 2019 | Environmental science | Trabzon, Turkey | Turkish legislation | Environmental engineering | Outside 48 hospitals | SVAN 958 | No |
| Wu et al. 2019 | Engineering | Harbin, Wuchang, Qitaihe, Chifeng, Changchun, Meihekou, China | Not cited | Environmental science and technology | Inside 18 hospitals (wards) | BSWA-801 | No |
| Yildirim and Mayda 2019 | Medicine | Düzce, Turkey | WHO/EPA/Turkish legislation | Public health | Inside 1 hospital (11 waiting areas of the outpatient clinics) | SVAN 957 | No |
| Zijlstra et al. 2019 | Multidisciplinary | Groningen, Netherlands | WHO | Applied sciences | Inside 1 hospital (infusion center) | Brüel & Kjær 2250 | Proposed and adopted measures |
| Astin et al. 2020 | Nursing | Northern England | WHO | Health sciences | Inside 1 hospital (2 rooms) | Casella, CEL-632C | Proposed measures |
| García-Rivero et al. 2020 | Acoustics + ultrasound | Lima, Peru | WHO/Peruvian regulations | Environmental sustainability | Outside 4 hospitals | BSWA-308 | Proposed measures |
| Hasegawa and Ryherd 2020 | Acoustics + ultrasound | Midwestern USA | Not cited | Architecture | Inside 1 hospital (PICU and pediatric medical-surgical) | Larson Davis 831 | Proposed measures |
| Tang et al. 2020 | Engineering | Shenzhen, China | Chinese GB/T 51153-2015 standard | Architecture | Inside 1 hospital (hospital street, outpatient waiting areas) | Casella CEL-6X0 | No |
Results and discussion
Databases and areas of knowledge of journals
After applying the filters, the database found to contain the largest number of articles was Web of Science, with 73%, followed by Scopus with 21% and ScienceDirect with 6%. Figure 2 shows the areas of knowledge of the journals (SCImago 2020) in which the articles were published.
Fig. 2.
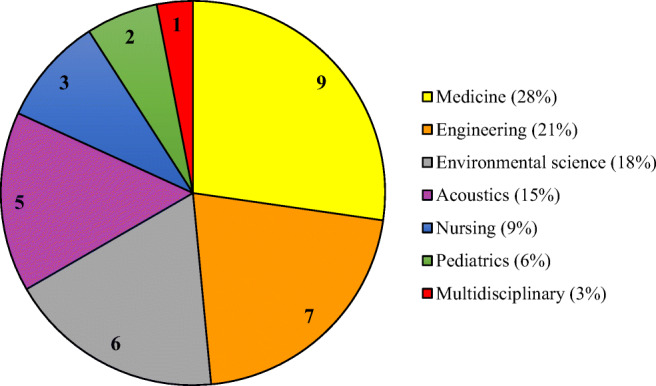
Areas of knowledge of scientific journals. Areas of knowledge of scientific journals extracted from the site: https://www.scimagojr.com
Figure 2 shows that 28% of the articles were published in medical journals, followed by 21% in engineering, 18% in environmental sciences, 15% in acoustics, 9% in nursing, 6% in pediatrics, and 3% in multidisciplinary journals, indicating the interdisciplinarity of the subject and its importance in several fields of science.
Countries where the studies were conducted
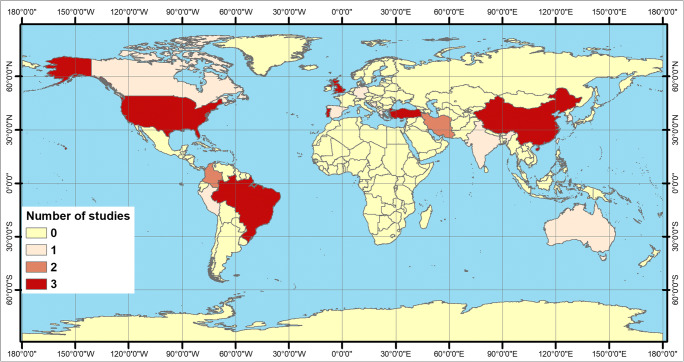
Among the 33 studies selected in this review, the countries with the highest participation rates were the USA (n = 3), Brazil (n = 3), China (n = 3), England (n = 3), Portugal (n = 3), and Turkey (n = 3) (9% each), followed by Colombia (n = 2) and Iran (n = 2) (6% each one), Germany, Australia, Bosnia and Herzegovina, Canada, South Korea, Spain, Greece, the Netherlands, India, Peru, and Taiwan (each with 1 study, corresponding to approximately 3% each) (see Fig. 3).
Fig. 3.
Global map showing the distribution of countries where studies were performed
Approximately 42% of studies are located in Europe (although Turkey is geographically situated between two continents, for the purpose of this review it was considered in Europe), 18% in South America, 12% in North America, 24% in Asia, and 4% in Oceania. Research on the African continent does not exist for the period and the criteria adopted in this review. One of the hypotheses for the paucity of studies on noise in hospitals in the African continent is that there are other more urgent needs, such as access to drinking water and treatment of some diseases, such as HIV and Ebola. Several researchers cite the lack of noise-related research in Africa (Okokon et al. 2018; Sieber et al. 2018). In a review study on noise pollution, Khan et al. (2018) found that most research on the subject has been conducted in Europe, demonstrating a potential gap for studies in this area in Africa, Oceania and South America. In a review study on noise in hospitals, Wallis et al. (2020) found that 33% of research was performed in Europe (in twelve countries), 38% in North America (in two countries), 5% in South America (two countries), 17% in Asia (four countries), 5% in Oceania (one country), and 2% in Africa (one country). In addition to the global geographic gap, if one considers, for example, that the USA has 6090 hospitals (AHA 2021), there is also a regional/local gap, since hospitals have different configurations, activities, layouts, etc.
Standards/laws used as references in studies
Although several countries have noise pollution laws and/or standards, many studies use other references as a parameter to assess whether or not measured noise levels pose risks to human health. Table 1 describes the main characteristics of laws and standards used as references in the studies.
Table 1.
Laws and standards used as references
| Evaluated parameters | W | E | AA | IR | BR | N | CL | A | CC | RD | GB | PR | NC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of citations | 15 | 5 | 4 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Outdoors, daytime (dB) | - | 55 | - | 55 | - | 50 | 55 | - | - | 60 | - | 50 | - |
| Indoors, daytime (dB) | 35 | 45 | 45 | 45 | 35-45 | 40 | - | 45 | 65 | 40-45 | 55 | - | - |
| Outdoors, nighttime (dB) | - | 55 | - | 45 | - | 55 | 45 | - | - | 50 | - | - | - |
| Indoors, nighttime (dB) | 30 | 35 | 45 | 35 | - | 35 | - | 45 | 65 | 30-35 | - | - | - |
W World Health Organization, E United States Environmental Protection Agency 1974, AA American Academy of Pediatrics, IR Iranian Standards, BR Brazilian Standards (NBR 10152/1987), N National Institute for Occupational Safety and Health – Occupational Noise Exposure 199 8, CL Curitiba Municipal Law no. 10625/2002, A Australian Standards, CC Consensus Committee for Neonatal Intensive Care Unit Design, RD Real Decreto 1367/2007, GB Chinese GB/T 51153-2015 standard, PR Peruvian National Environmental Standards for Noise, NC not cited
It was found that 45% of the studies cited the WHO as a reference for noise values, followed by the United States Environmental Protection Agency (EPA) with 15% and the American Academy of Pediatrics (AAP) with 12%. The WHO has more restrictive noise values than the other laws/standards cited in other studies, since it considers overall well-being. Taken together, WHO and EPA are the pioneer institutions in creating standard values for hospital noise (Baqar et al. 2017). Other studies have shown that the values recommended by the WHO are widely used as a reference for noise levels in hospitals (Wallis et al. 2019), although these levels are often exceeded and unlikely to be achieved (Loupa 2020).
Other countries and/or cities had their own particularities when they created their reference laws and considered not only the general health and well-being of the population. Most of these laws/standards are quite old, dating back to the 1970s, 1980s, or 1990s, when cities were less crowded and vehicle fleets smaller. Jahan et al. (2016) state that noise pollution was not a major concern for the population of Bangladesh in the 1970s and early 1980s, but that the risk of noise pollution increased and exceeded the level of tolerance in response to the growing number of motor vehicles in the country. Urban and demographic growth is not always planned, and it is difficult to adjust external environmental noise emission standards to acceptable levels.
To assess the effect of noise exposure of people in different countries, other factors must be considered as well, such as psychological, economic, social, cultural, climatic, and others not yet identified (Sieber et al. 2018).
Table 2 shows the range of equivalent sound pressure levels (Leq) for indoor and outdoor environments observed in the studies.
Table 2.
Equivalent internal and external noise levels from studies
| Author | Indoor noise dB (A) Leq | Outdoor noise dB (A) Leq | ||
|---|---|---|---|---|
| Daytime | Nighttime | Daytime | Nighttime | |
| Carvalhais et al. 2015 | 48.7–71.7 (24 h) | |||
| Chen 2015 | 51–73 | |||
| Fiedler and Zannin 2015 | > 65 | |||
| Filus et al. 2015 | 56.6–64.7 | 59.0–68.8 | ||
| Lahav 2015 | 58.7–60.0 | |||
| Monazzam et al. 2015 | 59.9–70.1 | |||
| Oliveira et al. 2015 | 54.8–65.2 | 43.4–54.9 | ||
| Garrido Galindo et al. 2016 | 58.9–65.7 | 57.0–64.2 | ||
| Luetz et al. 2016 | 50.9–56.2 (24 h) | |||
| Pirsaheb et al. 2016 | 52.0–88.6 | |||
| Shield et al. 2016 | 50.0–60.6 | 41.4–52.9 | ||
| Shoemark et al. 2016 | 55–65 (24 h) | |||
| de Araújo Vieira et al. 2016 | 58.2–65.6 | |||
| Ai et al. 2017 | 62.6–67.7 | |||
| Disher et al. 2017 | 43–70 (24 h) | |||
| D’Souza et al. 2017 | 59.4–62.1 | |||
| Galindo et al. 2017 | 59.5–65.3 (24 h) | |||
| Santos et al. 2017 | 46.6–71.7 (24 h) | |||
| Bevan et al. 2018 | 38.7–62.0 | |||
| Predrag et al. 2018 | 64.6–69.9 | 58.3–65.4 | ||
| Bliefnick et al. 2019 | 52–61 (24 h) | |||
| Cho et al. 2019 | 37–67 | |||
| Loupa et al. 2019 | 57–76 | |||
| Montes-González et al. 2019 | 55.7–60.2 | 51.4–55.5 | ||
| Terzi et al. 2019 | 61–71 (24 h) | |||
| Tezel et al. 2019 | 62.7–84.7 (24 h) | |||
| Wu et al. 2019 | 57.3–63.8 | |||
| Yildirim and Mayda 2019 | 48.5–70.8 | |||
| Zijlstra et al. 2019 | 39.7–54.6 (24 h) | |||
| Astin et al. 2020 | 49.2–51.6 | |||
| García-Rivero et al. 2020 | 83.3–88.6 | |||
| Hasegawa and Ryherd 2020 | 51.8–59.8 (24 h) | |||
| Tang et al. 2020 | 45–70.5 | |||
The indoor daytime Leq values in hospitals ranged from 37 dB (A) (Cho et al. 2019) to 88.6 dB (A) (Pirsaheb et al. 2016), while the nighttime levels varied from 38.7 dB (A) (Bevan et al. 2018) to 68.8 dB (A) (Filus et al. 2015). The outdoor noise level (Leq) was 74.3 in the daytime and 56.6 dB (A) at night. For measurements lasting 24 hours or longer, the values ranged from 39.7 (Zijlstra et al. 2019) to 71.7 dB (A) (Carvalhais et al. 2015; Santos et al. 2017). As for studies of outdoor noise levels, these varied from 83.3 to 88.6 dB (A) in the daytime (García-Rivero et al. 2020), from 58.3 to 65.4 dB (A) at night (Predrag et al. 2018), and from 62.7 to 84.7 dB (A) in a 24 h period (Tezel et al. 2019).
Even in countries that have technical guidelines for measuring indoor sound levels, such as Brazil through the NBR 10152 standard, it was found that the levels exceeded recommended ones (Filus et al. 2015; de Araújo Vieira et al. 2016).
Authors’ field of expertise
Like the journals that publish articles on noise in hospitals, the main authors of the publications also have different areas of expertise. In Table 3, note that the total of 33 selected articles were divided into 21 distinct areas. Areas such as architecture and engineering, which represent 27% of the authors’ specialties, contribute to the quality and interpretation of noise assessments in hospitals. Among the authors’ areas of expertise, 36% are in medicine, nursing and other related areas such as pediatrics, communication disorders, public health, health sciences, health and environment, and experimental clinical sciences. One of the explanations for these numbers is that most of the authors have some connection with hospitals (medical, nursing, pediatrics, and other departments, as well as medical laboratories). This facilitates not only the development of the study, in terms of bureaucracy, but also the methodology (choice of noise measurement points, authorization from specific departments, and analysis in different layouts, among others). The areas of expertise of the remaining 37% of authors are in environment, physics, and acoustics. This indicates that the subject has attracted increasing attention from different areas (Loupa 2020), since noise is often underestimated.
Table 3.
Areas of expertise of the main authors of scientific papers
| Area of expertise | Number |
|---|---|
| Architecture | 5 |
| Engineering | 4 |
| Health and environment | 2 |
| Medicine | 2 |
| Modeling of environmental systems | 2 |
| Nursing | 2 |
| Pediatrics | 2 |
| Air pollution | 1 |
| Applied physics | 1 |
| Applied sciences | 1 |
| Communication disorders | 1 |
| Environmental acoustics | 1 |
| Environmental health | 1 |
| Environmental science and technology | 1 |
| Environmental sustainability | 1 |
| Experimental clinical sciences | 1 |
| Health sciences | 1 |
| Occupational and environmental health | 1 |
| Physical metrology | 1 |
| Public health | 1 |
| Protection and ecology | 1 |
The authors’ areas of expertise were extracted from the information contained in their articles, sometimes in the headings, sometimes at the end
Focus of the studies (areas outside and/or inside hospitals)
Table 4 describes the focus of the studies in terms of location, which may be outside or inside the hospital building, as well as the number of studies.
Table 4.
Focus of studies and number of studies conducted outdoors and indoors
| Focus of study | Hospitals studied indoors | Hospitals studied outdoors | Hospitals studied outdoors and indoors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Out. and In. | Out. | In. | One | Two | ≥ Three | N.c. | One | Two | ≥ Three | N.c. | One | Two | ≥ Three |
| 1 | 5 | 27 | 21 | 2 | 3 | 1 | - | 2 | 3 | - | 1 | - | - |
Out. outdoors, In. indoors, N.c. not cited
Eighty-two percent of studies measured noise levels inside hospitals, while 15% measured noise outside hospital buildings and 3% took measurements both outdoors and indoors. Indoor measurements are important to evaluate the level of acoustic comfort of patients and medical staff, since a quiet environment is beneficial for both, lowers the physical and mental stress of hospital staff, and contributes to hasten patient recovery (Mousavi and Sohrabi 2018). Outdoor measurements are normally taken to draw up acoustic maps, which are useful tools for diagnosing and evaluating urban noise and indicating the noise levels that reach the hospital facade (Fiedler and Zannin 2015; Zannin and Ferraz 2016). Studies combining outdoor and indoor noise measurements are more laborious, but they can better describe the stressors that may originate outside buildings, such as vehicle traffic, or inside, such as medical equipment and loud conversations (Zannin and Ferraz 2016). Hospitals are environments where patients need to rest and recover and should therefore be quiet indoors and outdoors (Ramadhan and Talal 2015).
Measurements taken outside hospitals usually evaluate traffic noise generated by light vehicles, e.g., motorcycles and cars, and by heavy vehicles, e.g., buses, trucks, and trains. The studies conducted inside hospital environments in specific locations or in various departments are listed in Fig. 4.
Fig. 4.
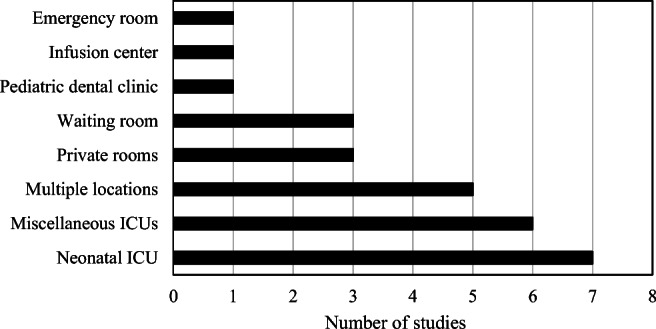
Hospital environments and number of studies conducted
Most of the studies available in the literature that involved measuring noise inside hospitals prioritized departments where patients are most vulnerable. Of the total of studies carried out indoors, 26% were conducted in neonatal ICUs, 22% in various different ICUs, and 19% in multiple locations inside hospitals. In addition, 22% were carried out in private and waiting rooms and 11% in emergency rooms, infusion center, and dental clinic. In another review of the literature on noise in hospitals, the authors found that 70% of the studies involved measurements taken in ICUs, and the remainder in different hospital departments (Wallis et al. 2019).
Measurement methods and parameters used
Table 5 describes the criteria adopted in the studies for installing the microphone of the sound level meter, such as height and distance from reflective surfaces, measurement time, and evaluated parameters. Most of the studies examined in this review used Leq dB (A) as a parameter. Other parameters such as Lmax are present in 39% of the studies, followed by Lmin with 27%. Some studies consider the statistical indices most commonly employed, such as L5, L10, L50, L90, and L95 (employed in approximately 73% of the studies), and others less common ones, such as L1, L70, L30, and L33 (used in 12% of the studies). It is noteworthy that 27% of the studies also performed frequency analysis (Carvalhais et al. 2015; Chen 2015; Lahav 2015; Ai et al. 2017; Galindo et al. 2017; Santos et al. 2017; Bliefnick et al. 2019; Loupa et al. 2019; Hasegawa and Ryherd 2020). In addition, 30% performed subjective analysis with questionnaires (Chen 2015; Oliveira et al. 2015; de Araújo Vieira et al. 2016; Ai et al. 2017; Santos et al. 2017; Cho et al. 2019; Wu et al. 2019; Zijlstra et al. 2019; Astin et al. 2020; Tang et al. 2020), or used reverberation time measures such as RT30, RT20 (Chen 2015; Cho et al. 2019), or the Speech Intelligibility Index (SII) (Bliefnick et al. 2019).
Table 5.
Microphone installation height, distance from reflective surfaces, measurement time, and evaluated parameters
| Source | Microphone | Time | Parameters | |
|---|---|---|---|---|
| Height (m) | Distance (m) | |||
| Carvalhais et al. 2015 | 1–1.65 | 1 | 24 h | LAeq, LAFmax |
| Chen 2015 | 1.2 | 1 | 15 min | LAeq, Lmin, Lmax, L5, L95, L10, L90, L70, L30 |
| Fiedler and Zannin 2015 | 1.3 | 2 | 10 min | LAeq |
| Filus et al. 2015 | - | - | 2.5 min | LAeq, Lmin, Lmax |
| Lahav 2015 | - | - | 5 days | LAeq |
| Monazzam et al. 2015 | 1.3 | 3 | 10, 15, 30 min | LAeq |
| Oliveira et al. 2015 | Corner of the ceiling | Beside the bed | 3 days | LAeq |
| Garrido Galindo et al. 2016 | 0.55 of the ceiling | 1.23–5.4 | 24 h | LAeq, Lmax, L90 |
| Luetz et al. 2016 | - | 0.40 next to the patient's head, door and window | 24 h | LAeq, LAFmax |
| Pirsaheb et al. 2016 | 1.5 | - | - | LAeq |
| Shield et al. 2016 | 3 of the ceiling | - | 5–14 days | LAeq, Lmax |
| Shoemark et al. 2016 | Near the head of the beds | - | 24 h | LAeq, Lmin, Lmax |
| de Araújo Vieira et al. 2016 | Ear height of professionals | 1 | 8 h | LAeq |
| Ai et al. 2017 | 1.1–1.2 | - | 10 min | LAeq |
| Disher et al. 2017 | - | - | 24 h | LAeq, Lmax, L10 |
| D’Souza et al. 2017 | - | 0.15 of hospital equipment | 1 week | LAeq, Lmin, Lmax, L10 |
| Galindo et al. 2017 | 0.60 of the ceiling | 2.15 | 20 days | LAeq, Lmin, Lmax, L10, L50, L90 |
| Santos et al. 2017 | 1–1.65 | 1 | 7 days | LAeq, LCpeak |
| Bevan et al. 2018 | - | - | 2 nights | LAeq |
| Predrag et al. 2018 | 1.7 | 3 | 15 min | LAeq, L1, L10 |
| Bliefnick et al. 2019 | 1 m behind the patient | - | 1 week | LAeq, Lmin, Lmax, LCpeak, L5, L95, L10, L90, L50 |
| Cho et al. 2019 | Near the ceiling, shelves, bed | - | 10 min–22 h | LAeq |
| Loupa et al. 2019 | 0.9–1.8 | 2 | 8 h | LAeq, Lmin, Lmax, L10, L95 |
| Montes-González et al. 2019 | 1.5 | - | 15 min, 14 days | LAeq |
| Terzi et al. 2019 | - | - | 24 h | LAeq |
| Tezel et al. 2019 | 4 | - | 24 h | LAeq |
| Wu et al. 2019 | 1.2–1.5 | 1 | 5 min | LAeq |
| Yildirim and Mayda 2019 | 1.5 | 1 | 8 h | LAeq |
| Zijlstra et al. 2019 | On the ceiling | - | 4 days | LAeq, Lmin, Lmax |
| Astin et al. 2020 | On the ceiling | - | 52 days | LAeq, Lmax |
| García-Rivero et al. 2020 | 1.5 | 3 | 5 min | LAeq, Lmin, Lmax, LApeak |
| Hasegawa and Ryherd 2020 | 0.76 above the patient’s head | - | 48 h | LAeq, Lmin, Lmax, LCpeak, L5, L95, L10, L90, L50, L33 |
| Tang et al. 2020 | 0.75 | - | 3 min | LAeq |
Distance of measurements from ground height ranged from 0.75 to 4 m, with some studies installing microphones on the ceiling or objects in order to protect the equipment, not disturb the hospital routine, or avoid the Hawthorne effect, enabling them to take long-term noise measurements (D’Souza et al. 2017; Cho et al. 2019; Zijlstra et al. 2019; Astin et al. 2020). As for the distance from reflective surfaces, 18% of the studies adopted 1 m.
Measurement times varied widely, ranging from 2.5 min to 52 days of uninterrupted measurement (Filus et al. 2015; Astin et al. 2020), although 21% of the studies took 24-h sound level measurements.
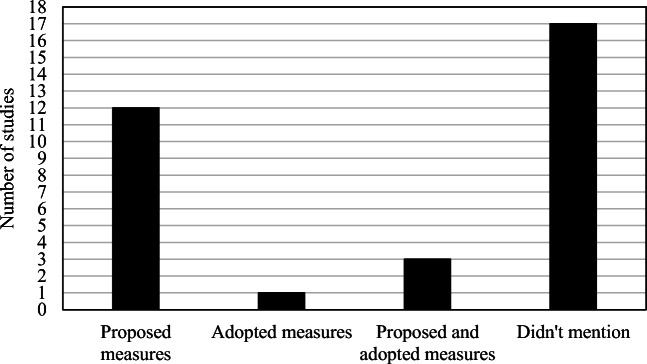
Studies that adopted/proposed noise mitigation measures
Some studies proposed or adopted measures to mitigate noise in hospitals, as indicated in Fig. 5. Studies that proposed measures for possible noise mitigation in hospitals represent 36% of the total number of studies analyzed in this review, while 52% of studies did not adopt or propose measures and only took measurements. Studies that adopted measures in order to make “before and after” comparisons represent 3% of the total, while 9% proposed and adopted noise mitigation measures.
Fig. 5.
Studies that proposed or adopted noise mitigation measures
Luetz et al. (2016) adopted ICU room modification measures, achieving noise reductions in the order of 2.8 dB (A). The main measures proposed by the studies for noise reduction in hospitals involve preventive and educational actions (Filus et al. 2015; Disher et al. 2017; Santos et al. 2017; Astin et al. 2020); use of sound absorbing materials (Chen 2015); adoption of barriers and architectural designs (Monazzam et al. 2015); simulations (Fiedler and Zannin 2015; Montes-González et al. 2019); changes in equipment; physical installations, and procedures (Pirsaheb et al. 2016; Shield et al. 2016); and more studies in different locations and hospitals (Hasegawa and Ryherd 2020; García-Rivero et al. 2020).
Studies that proposed and adopted noise control measures involved a training program (Carvalhais et al. 2015) in which the noise levels showed no variation after implementation of the program, a non-talking rule (Zijlstra et al. 2019) whose implementation led to a noise reduction of 1.1 dB (A), and a quiet hospital environment (Bliefnick et al. 2019).
Vehicle traffic noise is what most affects the modern human lifestyle (Ruiz-Padillo et al. 2016). Changes in driver behavior can contribute to reduce noise levels that reach hospital facades. However, some studies have indicated that despite the significant reduction in the number of vehicles circulating during the COVID-19 pandemic, reductions in noise levels were lower than expected, a fact that is attributed the high driving speed of the remaining vehicles (Asensio et al. 2020). Other factors that contribute to traffic noise levels and that deserve attention are the types of tires (Licitra et al. 2017) and of paving (Praticò and Anfosso-Lédée 2012; Praticò 2014; Licitra et al. 2015; Licitra et al. 2019; Del Pizzo et al. 2020).
Future perspectives in this field
Noise measurements are extremely important for assessing the level of exposure to which people are subjected, given the risks associated with this type of pollution. In hospitals, these measurements are even more important, given the physical and emotional vulnerability of patients and the stress to which hospital staff are subjected daily. Hence, working in extreme situations while subjected to noise levels exceeding those established by laws, standards, or agencies such as the WHO can delay the recovery of patients and impair the performance of healthcare professionals (Zannin and Ferraz 2016; Zannin et al. 2019; Busch-Vishniac and Ryherd 2019; Loupa 2020).
An average of 5.5 articles per year were published in the period studied in this review, as illustrated in Fig. 6.
Fig. 6.
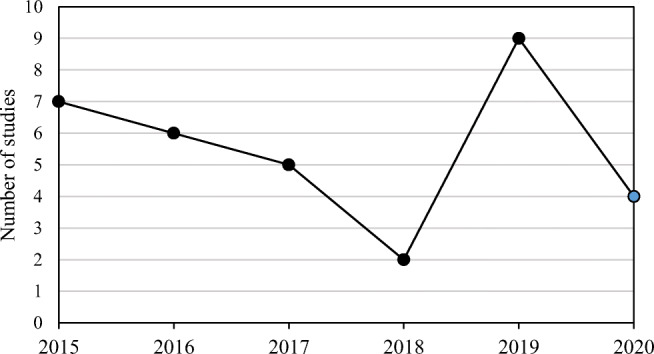
Number of studies conducted in the last 6 years
In order to improve noise assessments in hospitals, research must contain as much information as possible, e.g., locations where equipment was installed, measurement height from ground level, distance from reflective surfaces, measurement time, noise sources, and measurement period (Wallis et al. 2019). As can be seen in Table 5, the information provided by some studies is insufficient for a careful reproduction or analysis, even those that took measurements for 24 h or more. Studies published in journals in the area of acoustics (e.g., Bliefnick et al. 2019; Hasegawa and Ryherd 2020) offer more complete information, extracting the maximum quality and diversity of resources provided by the equipment used, thus enabling the analysis of a series of interventions and improvements in the quality of the environment. Given the diversity of ways in which the studies are conducted, perhaps a more comprehensive standardization strategy is needed in order to balance noise measurement procedures in indoor hospital environments, considering that the forms of noise measurements in outdoor environments with validation on maps ensure more reliable results.
Conclusions
Several scientific journals have published studies on environmental noise assessment in hospitals, mainly in the areas of medicine, engineering, environmental sciences, acoustics, and nursing. The areas of expertise of the authors of these studies correspond to those of the journals, since most of them are doctors, nurses, and engineers. The studies are concentrated mainly in Europe, the Americas, and Asia.
Most of the studies use the noise levels recommended by WHO as a reference to determine whether the measured noise levels may be harmful to human health in the hospital environment. However, it should be noted that the levels recommended by WHO are the most restrictive possible and that the noise levels measured in practically all the studies selected for this review were much higher. The Leq levels measured in indoor hospital environments varied from 37 to 88.6 dB (A) in the daytime and from 38.7 to 68.8 dB (A) at night, while the outdoor noise levels were 74.3 in the daytime and 56.6 dB (A) at night.
The main focus of the studies was the internal part of the hospitals, and most of them took measurements in only one hospital. Departments treating more sensitive and vulnerable patients that require greater attention from health care professionals, such as ICUs, were preferred environments for environmental noise measurements.
A considerable number of the studies only indicate if the measured noise levels are in conformity with some reference standard or law, but do not adopt or propose measures to reduce the levels.
This is a field of research with a potential for growth. However, there is a need for a more critical assessment of the quality of studies, aiming at scientific advances and reliable dissemination of information to the community in general.
Acknowledgements
The authors would like to thank the reviewers for their valuable contributions to improve this work.
Appendix 1
Authors’ contributions
All the authors whose names appear on the submission made substantial contributions to the conception or design of the work. Idea for the article: [ELA], [DCCS]. Authors who performed the literature search and data analysis: [ELA], [EAL]. Authors who drafted and critically revised the work: [ELA], [EAL], [DCCS], [RAO], [PHTZ]; [ACGM].
Data Availability
All data generated or analyzed in this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ai ZT, Mak CM, Wong HM. Noise level and its influences on dental professionals in a dental hospital in Hong Kong. Build Serv Eng Res Technol. 2017;38:522–535. doi: 10.1177/0143624417705529. [DOI] [Google Scholar]
- American Hospital Association (AHA) – AHA Hospital Statistics. (2021) Acess. in 27 Jan 2021, from https://www.aha.org/statistics/fast-facts-us-hospitals
- Asensio C, Pavón I, de Arcas G. Changes in noise levels in the city of Madrid during COVID-19 lockdown in 2020. J Acoust Soc Am. 2020;148:1748–1755. doi: 10.1121/10.0002008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astin F, Stephenson J, Wakefield J, Evans B, Rob P, Joanna G, Harris E. Night-time noise levels and patients’ sleep experiences in a medical assessment unit in Northern England. Open Nurs J. 2020;14:80–91. doi: 10.2174/1874434602014010080. [DOI] [Google Scholar]
- Babisch W, Beule B, Schust M, Kersten N, Ising H. Traffic noise and risk of myocardial infarction. Epidemiology. 2005;16:33–40. doi: 10.1097/01.ede.0000147104.84424.24. [DOI] [PubMed] [Google Scholar]
- Baqar M, Arslan M, Abbasi SA, Ashraf U, Khalid A, Zahid H. Noise pollution in the hospital environment of a developing country: a case study of Lahore (Pakistan) Arch Environ Occup Health. 2017;73:367–374. doi: 10.1080/19338244.2017.1371106. [DOI] [PubMed] [Google Scholar]
- Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15(3):519. doi: 10.3390/ijerph15030519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. Geneva: World Health Organization; 1999. [Google Scholar]
- Bevan R, Grantham-Hill S, Bowen R, Clayton E, Grice H, Venditti HC, Stickland A, Hill CM. Sleep quality and noise: comparisons between hospital and home settings. Arch Dis Child. 2018;104:147–151. doi: 10.1136/archdischild-2018-315168. [DOI] [PubMed] [Google Scholar]
- Bliefnick JM, Ryherd EE, Jackson R. Evaluating hospital soundscapes to improve patient experience. J Acoust Soc Am. 2019;145:1117–1128. doi: 10.1121/1.5090493. [DOI] [PubMed] [Google Scholar]
- Busch-Vishniac I, Ryherd E. Hospital soundscapes: characterization, impacts, and interventions. Acoust Today. 2019;15:11. doi: 10.1121/at.2019.15.3.11. [DOI] [Google Scholar]
- Busch-Vishniac IJ, West JE, Barnhill C, Hunter T, Orellana D, Chivukula R. Noise levels in Johns Hopkins Hospital. J Acoust Soc Am. 2005;118:3629–3645. doi: 10.1121/1.2118327. [DOI] [PubMed] [Google Scholar]
- Carvalhais C, Santos J, Da Silva MV, Xavier A. Is there sufficient training of health care staff on noise reduction in neonatal intensive care units? A pilot study from neonoise project. J Toxicol Environ Heal - Part A Curr Issues. 2015;78:897–903. doi: 10.1080/15287394.2015.1051204. [DOI] [PubMed] [Google Scholar]
- Chen CY. Characterizing subjective noisiness in hospital lobbies. Arch Acoust. 2015;40:235–246. doi: 10.1515/aoa-2015-0026. [DOI] [Google Scholar]
- Cho WH, Jeong CH, Chang JH, Lee SH, Park MK, Suh MW, Han JJ. Noise and room acoustic conditions in a tertiary referral hospital, Seoul National University Hospital. J Audiol Otol. 2019;23:76–82. doi: 10.7874/jao.2018.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Souza SRB, Lewis LE, Kumar V, Ramesh Bhat Y, Purkayastha J, Prakash H. Ambient noise levels in acute neonatal intensive care unit of a tertiary referral hospital. J Krishna Inst Med Sci Univ. 2017;6:50–58. [Google Scholar]
- de Araújo Vieira EM, da Silva LB, de Souza EL. The influence of the workplace indoor environmental quality on the incidence of psychological and physical symptoms in intensive care units. Build Environ. 2016;109:12–24. doi: 10.1016/j.buildenv.2016.09.007. [DOI] [Google Scholar]
- Del Pizzo A, Teti L, Moro A, et al. Influence of texture on tyre road noise spectra in rubberized pavements. Appl Acoust. 2020;159:107080. doi: 10.1016/j.apacoust.2019.107080. [DOI] [Google Scholar]
- Disher TC, Benoit B, Inglis D, Burgess SA, Ellsmere B, Hewitt BE, Bishop TM, Sheppard CL, Jangaard KA, Morrison GC, Campbell-Yeo ML. Striving for optimum noise-decreasing strategies in critical care: initial measurements and observations. J Perinat Neonatal Nurs. 2017;31:58–66. doi: 10.1097/JPN.0000000000000229. [DOI] [PubMed] [Google Scholar]
- Dratva J, Phuleria HC, Foraster M, Gaspoz JM, Keidel D, Künzli N, Liu LJS, Pons M, Zemp E, Gerbase MW, Schindler C. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect. 2012;120:50–55. doi: 10.1289/ehp.1103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson LC, Newman RS. Influences of background noise on infants and children. Curr Dir Psychol Sci. 2017;26:451–457. doi: 10.1177/0963721417709087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiedler PEK, Zannin PHT. Evaluation of noise pollution in urban traffic hubs-Noise maps and measurements. Environ Impact Assess Rev. 2015;51:1–9. doi: 10.1016/j.eiar.2014.09.014. [DOI] [Google Scholar]
- Filus W, De Lacerda ABM, Albizu E. Ambient noise in emergency rooms and its health hazards. Int Arch Otorhinolaryngol. 2015;19:205–209. doi: 10.1055/s-0034-1387165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortes-Garrido JC, Velez-Pereira AM, Gázquez M, Hidalgo-Hidalgo M, Bolívar JP. The characterization of noise levels in a neonatal intensive care unit and the implications for noise management. J Environ Health Sci Eng. 2014;12:1–8. doi: 10.1186/2052-336X-12-104. [DOI] [Google Scholar]
- Galindo APG, Caicedo YC, Vélez-Pereira AM. Noise level in a neonatal intensive care unit in Santa Marta - Colombia. Colombia Médica. 2017;48:119–124. doi: 10.25100/cm.v48i3.2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Rivero AE, Yuli-Posadas RÁ, Romero WR, Sánchez-Ccoyllo O, Bulege-Gutierrez W, Tasayco HGG, Fernández-Gusmán V. Daytime perimeter environmental noise in the vicinity of four hospitals in the city of Lima, Peru. Noise Mapp. 2020;7:239–247. doi: 10.1515/noise-2020-0020. [DOI] [Google Scholar]
- Garrido Galindo AP, Camargo Caicedo Y, Vélez-Pereira AM. Noise level in intensive care units of a public university hospital in Santa Marta (Colombia) Med Intensiva (English Ed) 2016;40:403–410. doi: 10.1016/j.medine.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Guski R, Schreckenberg D, Schuemer R. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and annoyance. Int J Environ Res Public Health. 2017;14:1–39. doi: 10.3390/ijerph14121539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman I, Rasmanis G, Blomkvist V, Ulrich R, Eriksen C, Theorell T. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. Int J Cardiol. 2005;98:267–270. doi: 10.1016/j.ijcard.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Hänninen O, Knol AB, Jantunen M, Lim TA, Conrad A, Rappolder M, Carrer P, Fanetti AC, Kim R, Buekers J, Torfs R, Iavarone I, Classen T, Hornberg C, Mekel OC, EBoDE Working Group Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environ Health Perspect. 2014;122:439–446. doi: 10.1289/ehp.1206154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasegawa Y, Ryherd E. Clustering acoustical measurement data in pediatric hospital units. J Acoust Soc Am. 2020;148:265–277. doi: 10.1121/10.0001584. [DOI] [PubMed] [Google Scholar]
- Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, De Hoogh K, Thiesse L, Rudzik F, Habermacher M, Köpfli M, Pieren R, Brink M, Cajochen C, Wunderli JM, Probst-Hensch N, Roösli M. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J. 2018;40:598–603. doi: 10.1093/eurheartj/ehy650. [DOI] [PubMed] [Google Scholar]
- Hsu T, Ryherd E, Waye KP, Ackerman J. Noise pollution in hospitals: impacts on patients. J Clin Out Mgmt. 2012;19:301–309. [Google Scholar]
- Jahan S, Munni S, Ghosh GC. Noise pollution at major schools, colleges and hospitals in small urban area: Focusing on Jessore municipality, Bangladesh. Nat Environ Pollut Technol. 2016;15:1089–1094. [Google Scholar]
- Khan J, Ketzel M, Kakosimos K, Sørensen M, Jensen SS. Road traffic air and noise pollution exposure assessment – a review of tools and techniques. Sci Total Environ. 2018;634:661–676. doi: 10.1016/j.scitotenv.2018.03.374. [DOI] [PubMed] [Google Scholar]
- Lahav A. Questionable sound exposure outside of the womb: frequency analysis of environmental noise in the neonatal intensive care unit. Acta Paediatr Int J Paediatr. 2015;104:e14–e19. doi: 10.1111/apa.12816. [DOI] [PubMed] [Google Scholar]
- Licitra G, Cerchiai M, Teti L, Ascari E, Bianco F, Chetoni M. Performance assessment of low-noise road surfaces in the leopoldo project: comparison and validation of different measurement methods. Coatings. 2015;5:3–25. doi: 10.3390/coatings5010003. [DOI] [Google Scholar]
- Licitra G, Fredianelli L, Petri D, Vigotti MA. Annoyance evaluation due to overall railway noise and vibration in Pisa urban areas. Sci Total Environ. 2016;568:1315–1325. doi: 10.1016/j.scitotenv.2015.11.071. [DOI] [PubMed] [Google Scholar]
- Licitra G, Teti L, Cerchiai M, Bianco F. The influence of tyres on the use of the CPX method for evaluating the effectiveness of a noise mitigation action based on low-noise road surfaces. Transp Res Part D Transp Environ. 2017;55:217–226. doi: 10.1016/j.trd.2017.07.002. [DOI] [Google Scholar]
- Licitra G, Moro A, Teti L, del Pizzo A, Bianco F. Modelling of acoustic ageing of rubberized pavements. Appl Acoust. 2019;146:237–245. doi: 10.1016/j.apacoust.2018.11.009. [DOI] [Google Scholar]
- Lin YT, Chen TW, Chang YC, Chen ML, Hwang BF. Relationship between time-varying exposure to occupational noise and incident hypertension: a prospective cohort study. Int J Hyg Environ Health. 2020;226:113487. doi: 10.1016/j.ijheh.2020.113487. [DOI] [PubMed] [Google Scholar]
- Loupa G (2020) Influence of noise on patient recovery. Curr Pollut Rep. 10.1007/s40726-019-00134-3
- Loupa G, Katikaridis A, Karali D, Rapsomanikis S. Mapping the noise in a Greek general hospital. Sci Total Environ. 2019;646:923–929. doi: 10.1016/j.scitotenv.2018.07.315. [DOI] [PubMed] [Google Scholar]
- Luetz A, Weiss B, Penzel T, Fietze I, Glos M, Wernecke KD, Bluemke B, Dehn AM, Willemeit T, Finke A, Spies C. Feasibility of noise reduction by a modification in ICU environment. Physiol Meas. 2016;37:1041–1055. doi: 10.1088/0967-3334/37/7/1041. [DOI] [PubMed] [Google Scholar]
- Miedema HME, Oudshoorn CGM. Annoyance from transportation noise: relationships with exposure metrics DNL and DENL and their confidence intervals. Environ Health Perspect. 2001;109:409–416. doi: 10.1289/ehp.01109409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minichilli F, Gorini F, Ascari E, Bianchi F, Coi A, Fredianelli L, Licitra G, Manzoli F, Mezzasalma L, Cori L. Annoyance judgment and measurements of environmental noise: a focus on Italian secondary schools. Int J Environ Res Public Health. 2018;15:1–17. doi: 10.3390/ijerph15020208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monazzam MR, Karimi E, Abbaspour M, Nassiri P, Taghavi L. Spatial traffic noise pollution assessment - a case study. Int J Occup Med Environ Health. 2015;28:625–634. doi: 10.13075/ijomeh.1896.00103. [DOI] [PubMed] [Google Scholar]
- Montes-González D, Barrigón-Morillas JM, Escobar VG, Vílchez-Gómez R, Rey-Gozalo G, Atanasio-Moraga P, Méndez-Sierra JA (2019) Environmental noise around hospital areas: a case study. Environ - MDPI 6:41. 10.3390/environments6040041
- Mousavi SA, Sohrabi P. A comprehensive evaluation of the level of noise pollution in hospitals of Kermanshah university of medical sciences. Glob Nest J. 2018;20:363–367. doi: 10.30955/gnj.002416. [DOI] [Google Scholar]
- Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11:135–142. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Okokon EO, Taimisto P, Turunen AW, Amoda OA, Fasasi AE, Adeyemi LG, Juutilainen J, Lanki T. Particulate air pollution and noise: assessing commuter exposure in Africa’s most populous city. J Transp Health. 2018;9:150–160. doi: 10.1016/j.jth.2018.04.003. [DOI] [Google Scholar]
- Oliveira L, Gomes C, Bacelar Nicolau L, Ferreira L, Ferreira R. Environment in pediatric wards: Light, sound, and temperature. Sleep Med. 2015;16:1041–1048. doi: 10.1016/j.sleep.2015.03.015. [DOI] [PubMed] [Google Scholar]
- Paiva KM, Cardoso MRA, Zannin PHT. Exposure to road traffic noise: Annoyance, perception and associated factors among Brazil’s adult population. Sci Total Environ. 2019;650:978–986. doi: 10.1016/j.scitotenv.2018.09.041. [DOI] [PubMed] [Google Scholar]
- Pirsaheb M, Yarmohammadi H, Dabirian M, Abdollahzadeh D, Sohrabi Y. A study of public and local noise level in wards of a state hospital in Kermanshah. J Eng Appl Sci. 2016;11:1069–1073. doi: 10.3923/jeasci.2016.1069.1073. [DOI] [Google Scholar]
- Praticò FG. On the dependence of acoustic performance on pavement characteristics. Transp Res Part D Transp Environ. 2014;29:79–87. doi: 10.1016/j.trd.2014.04.004. [DOI] [Google Scholar]
- Praticò FG, Anfosso-Lédée F. Trends and issues in mitigating traffic noise through quiet pavements. Procedia Soc Behav Sci. 2012;53:203–212. doi: 10.1016/j.sbspro.2012.09.873. [DOI] [Google Scholar]
- Predrag I, Dragana NM, Ljiljana SB. Measuring and mapping noise pollution in the city of Banja Luka. Arch Tech Sci. 2018;1:89–96. doi: 10.7251/afts.2018.1018.089i. [DOI] [Google Scholar]
- Ramadhan SH, Talal SK. Noise pollution in wards and other areas in general hospital at Zakho city-Kurdistan region/Iraq. Int J Adv Appl Sci. 2015;2:16–20. [Google Scholar]
- Ravindra K, Singh T, Tripathy JP, Mor S, Munjal S, Patro B, Panda N. Assessment of noise pollution in and around a sensitive zone in North India and its non-auditory impacts. Sci Total Environ. 2016;566-567:981–987. doi: 10.1016/j.scitotenv.2016.05.070. [DOI] [PubMed] [Google Scholar]
- Ruiz-Padillo A, Ruiz DP, Torija AJ, Ramos-Ridao Á. Selection of suitable alternatives to reduce the environmental impact of road traffic noise using a fuzzy multi-criteria decision model. Environ Impact Assess Rev. 2016;61:8–18. doi: 10.1016/j.eiar.2016.06.003. [DOI] [Google Scholar]
- Santos J, Carvalhais C, Xavier A, Silva MV. Assessment and characterization of sound pressure levels in Portuguese neonatal intensive care units. Arch Environ Occup Health. 2017;73:121–127. doi: 10.1080/19338244.2017.1304883. [DOI] [PubMed] [Google Scholar]
- SCImago (2020) SJR — SCImago Journal & Country Rank [Portal]. http://www.scimagojr.com. Acessesed 27 Dec 2020
- Shield B, Shiers N, Glanville R. The acoustic environment of inpatient hospital wards in the United Kingdom. J Acoust Soc Am. 2016;140:2213–2224. doi: 10.1121/1.4962276. [DOI] [PubMed] [Google Scholar]
- Shoemark H, Harcourt E, Arnup SJ, Hunt RW. Characterising the ambient sound environment for infants in intensive care wards. J Paediatr Child Health. 2016;52:436–440. doi: 10.1111/jpc.13084. [DOI] [PubMed] [Google Scholar]
- Sieber C, Ragettli MS, Brink M, Olaniyan T, Baatjies R, Saucy A, Vienneau D, Probst-Hensch N, Dalvie MA, Röösli M. Comparison of sensitivity and annoyance to road traffic and community noise between a South African and a Swiss population sample. Environ Pollut. 2018;241:1056–1062. doi: 10.1016/j.envpol.2018.06.007. [DOI] [PubMed] [Google Scholar]
- Sorensen M, Nielsen OW, Sajadieh A, Ketzel M, Tjonneland A, Overvad K, Raaschou-Nielsen O. Long-term exposure to road traffic noise and nitrogen dioxide and risk of heart failure: a cohort study. Environ Health Perspect. 2017;125:097021. doi: 10.1289/EHP1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang H, Ding J, Lin Z. On-site measurement of indoor environment quality in a Chinese healthcare facility with a semi-closed hospital street. Build Environ. 2020;173:106637. doi: 10.1016/j.buildenv.2019.106637. [DOI] [Google Scholar]
- Terzi B, Azizoğlu F, Polat Ş, Kaya N, İşsever H. The effects of noise levels on nurses in intensive care units. Nurs Crit Care. 2019;24:299–305. doi: 10.1111/nicc.12414. [DOI] [PubMed] [Google Scholar]
- Tezel MN, Sari D, Ozkurt N, Keskin SS. Combined NOx and noise pollution from road traffic in Trabzon, Turkey. Sci Total Environ. 2019;696:134044. doi: 10.1016/j.scitotenv.2019.134044. [DOI] [Google Scholar]
- U.S. EPA (U.S. Environmental Protection Agency). 1974. Information on levels of environmental noise requisite to protect public health and welfare with an adequate margin of safety. Acess. in 27 Jan 2021, from http://www.nonoise.org/library/levels74/levels74.htm
- van Kempen E, Casas M, Pershagen G, Foraster M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15:1–59. doi: 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallis R, Harris E, Lee H, Davies W, Astin F. Environmental noise levels in hospital settings: a rapid review of measurement techniques and implementation in hospital settings. Noise Heal. 2019;21:200–216. doi: 10.4103/nah.NAH_19_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Meng Q, Li L, Mu J (2019) Interaction between sound and thermal influences on patient comfort in the hospitals of China’s northern heating region. Appl Sci 9. 10.3390/app9245551
- Yildirim H, Mayda AS (2019) Determination of noise levels in the outpatient clinics of medical faculty hospital at Duzce University. Konuralp Tıp Derg 11:235–241. 10.18521/ktd.434486
- Zannin PHT, Ferraz F. Assessment of indoor and outdoor noise pollution at a university hospital based on acoustic measurements and noise mapping. Open J Acoust. 2016;06:71–85. doi: 10.4236/oja.2016.64006. [DOI] [Google Scholar]
- Zannin PHT, Milanês ML, De Oliveira Filho MVM. Evaluation of noise in the vicinity of a hospital and a gated community. Curr Urban Stud. 2019;07:59–75. doi: 10.4236/cus.2019.71004. [DOI] [Google Scholar]
- Zijlstra E, Hagedoorn M, Krijnen WP, van der Schans CP, Mobach MP. The effect of a non-talking rule on the sound level and perception of patients in an outpatient infusion center. PLoS One. 2019;14:1–15. doi: 10.1371/journal.pone.0212804. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed in this study are included in this published article [and its supplementary information files].