Significance
Many countries closed schools during the pandemic to contain the spread of SARS-CoV-2. Sweden closed upper-secondary schools, while lower-secondary schools remained open, allowing for an evaluation of school closures. This study analyzes the impact of school closures on the spread of SARS-CoV-2 by comparing groups exposed and not exposed to open schools. We find that exposure to open schools resulted in a small increase in infections among parents. Among teachers, the infection rate doubled, and infections spilled over to their partners. This suggests that keeping lower-secondary schools open had a minor impact on the overall spread of SARS-CoV-2 in society. However, teachers are affected, and measures to protect them could be considered.
Keywords: COVID-19, SARS-CoV-2, school closures, social distancing
Abstract
To reduce the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), most countries closed schools, despite uncertainty if school closures are an effective containment measure. At the onset of the pandemic, Swedish upper-secondary schools moved to online instruction, while lower-secondary schools remained open. This allows for a comparison of parents and teachers differently exposed to open and closed schools, but otherwise facing similar conditions. Leveraging rich Swedish register data, we connect all students and teachers in Sweden to their families and study the impact of moving to online instruction on the incidence of SARS-CoV-2 and COVID-19. We find that, among parents, exposure to open rather than closed schools resulted in a small increase in PCR-confirmed infections (odds ratio [OR] 1.17; 95% CI [CI95] 1.03 to 1.32). Among lower-secondary teachers, the infection rate doubled relative to upper-secondary teachers (OR 2.01; CI95 1.52 to 2.67). This spilled over to the partners of lower-secondary teachers, who had a higher infection rate than their upper-secondary counterparts (OR 1.29; CI95 1.00 to 1.67). When analyzing COVID-19 diagnoses from healthcare visits and the incidence of severe health outcomes, results are similar for teachers, but weaker for parents and teachers’ partners. The results for parents indicate that keeping lower-secondary schools open had minor consequences for the overall transmission of SARS-CoV-2 in society. The results for teachers suggest that measures to protect teachers could be considered.
In the effort to contain the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), most countries closed schools. An estimated 1.3 billion students in 195 countries were affected by school closures in mid-April 2020 (1). These closures are likely to have a negative impact on student learning and well-being, especially for students from disadvantaged backgrounds (2, 3). School closures also affect labor supply, not least among healthcare workers, hence reducing healthcare capacity (4). While the costs associated with school closures are high, modeling studies question their effectiveness in reducing the transmission of SARS-CoV-2, and direct evidence is largely missing (5). The absence of direct evidence is because school closures were usually implemented early, universally, and in close proximity to a raft of nonpharmaceutical interventions (NPIs) that have been documented and modeled to bring about large reductions in the basic reproduction number (6–11). This renders it difficult, if not impossible, to disentangle the effects of each specific intervention.
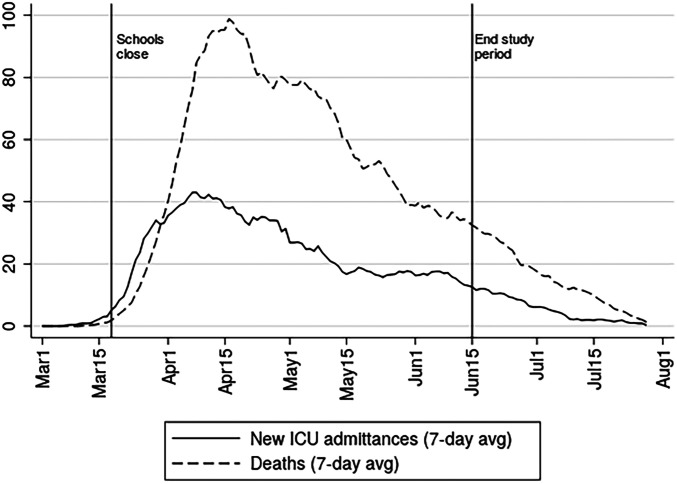
Sweden was an exception to the norm of universal school closures. On March 18, 2020, 1 week after the first reported death from COVID-19, upper-secondary schools moved to online instruction, while schools for younger students remained open until the end of the school year in mid-June. While other NPIs were also implemented (SI Appendix), this partial school closure allows for a comparison of individuals and households who were differently exposed to open and closed schools, but otherwise faced similar conditions throughout the period of widespread contagion illustrated in Fig. 1. In this study, we link detailed register data from Statistics Sweden on the entire Swedish population to all PCR-identified cases of SARS-CoV-2 reported to the Public Health Agency of Sweden and COVID-19 cases requiring medical treatment reported to the National Board of Health and Welfare between the time of school closure to the end of the school year. To study the general impact of school closure on the transmission of the virus, we estimate differences in infection rates between parents exposed to lower- and upper-secondary students. We further analyze differences in infection rates between lower- and upper-secondary teachers, as well as their partners.
Fig. 1.
COVID-19 deaths and intensive care unit (ICU) admissions. The 7-day averages (avg) of deaths and ICU admissions. Solid vertical lines mark the start of school closure and the end of the period of analysis. Data are from the Public Health Agency of Sweden (18).
For school closures to affect virus transmission, they must affect behavior and contact patterns. The impact of school closures on the transmission of SARS-CoV-2 further depends on how the virus spreads between students, from students to adults, and among adults in school and at home. Current reviews of the evidence suggest that while children and adolescents do get infected, they usually develop mild or no symptoms (12, 13). The susceptibility to infection appears to be lower among the young, but there is some uncertainty regarding this, as a large number of cases probably go undetected. Children and adolescents with mild or no symptoms may still carry and spread the infection, but the evidence available indicates that infectiousness, just as the severity of symptoms, is increasing in age. Outbreaks have been reported in connection to school openings and overnight summer camps (14, 15), but transmission within schools prior to their closure at the onset of the pandemic appears to have been limited (16, 17). A general caveat concerning the available evidence is that most studies on the susceptibility and infectiousness of children and adolescents have been conducted when schools were closed and other NPIs were in place.
Differences between groups can be attributed to school closures if the groups are behaviorally and biologically similar in all other respects that affect the probability to get infected and tested. Lower-secondary school (school years 7–9, typical age 14–16) is compulsory. Attendance to upper-secondary school (school years 10–12, typical age 17–19) is close to universal, but grade repetition is more common at the upper-secondary level, in particular among students with non-European Union (non-EU) background (19). We therefore restrict the main sample to parents without such a background, but also present results for all parents. The main selection concern regards the age of parents and students. Parental characteristics (age, sex, income, occupation, and region of origin and of residence) are controlled for, but the susceptibility and infectiousness are likely to increase in student age, and general behavior may differ between younger and older students. We therefore focus our attention on parents exposed to students in the final year of lower-secondary and first year of upper-secondary school. The main concern regarding differences between upper- and lower-secondary teachers and their partners refers to partner characteristics that are adjusted for. Given these restrictions and adjustments, the estimated differences can plausibly be attributed to the exposure to open and closed schools. The study thus offers credible, direct evidence on the impact of school closures on the SARS-CoV-2 pandemic.
Models based on influenza predict that school closures can be effective if they actually reduce the number of contacts, the basic reproduction number (R0) is below two, and the attack rate is higher in children than in adults (20). The basic reproduction number for SARS-CoV-2 is above two (21), and the attack rate in students is likely to be low relative to adults (12). The theoretical prior is therefore that the impact of school closures on the transmission of SARS-CoV-2 among parents is low (5). For teachers and their partners, a more substantive impact can be expected. Teachers at open schools were not only exposed to students, but also to other adults, both at work and during their commute. Upper-secondary teachers partly worked from school, but a substantive fraction did their teaching from home (SI Appendix).
Results
We estimate differences in infections among parents, teachers, and teachers’ partners who were differently exposed to lower (open) and upper (online) secondary schools using linear probability models (ordinary least squares [OLS]) and logistic regressions (Logit). Descriptive statistics are shown in Tables 3 and 4. The preferred outcome is PCR-confirmed SARS-CoV-2, which has the highest incidence (7.37 cases per 1,000 among lower- and upper-secondary parents and 4.69 per 1,000 among teachers). If we exclude healthcare workers, who were targeted for testing, the incidence drops to 4.33 per 1,000 among parents. One potential drawback of this outcome is that unbiased results rely on compared groups having equal propensity to get tested. In particular, it could be that those directly or indirectly exposed to open schools were more prone to get tested, which would exaggerate the impact of school closures. The risk of such bias is alleviated by the limited testing capacity that forced testing to be targeted toward those with severe symptoms and care workers throughout most of the relevant period (SI Appendix). However, we also analyze COVID-19 diagnoses from healthcare visits, which are less likely to suffer from bias due to behavioral differences. Healthcare coverage in Sweden is universal, and fees for doctor or hospital visits are low, assuring that individuals in need will seek care. This is particularly true for hospitalizations, since admittance to hospital is determined strictly on medical grounds. As receiving a COVID-19 diagnosis is a less frequent event (3.11/1,000 among parents; 2.60/1,000 among teachers), these estimations have lower statistical power. Low incidence is an even larger problem for severe cases (hospitalizations or deaths), which have an incidence of 1.43/1,000 among parents and 1.59/1,000 among teachers. Results for severe cases are reported in SI Appendix, Table S1.
Table 3.
Descriptive statistics: Parents
| Parents school years 7–12 | Parents school years 9–10 | |||||
| Full sample | Lower sec. | Upper sec. | Full sample | Lower sec. | Upper sec. | |
| Cases/1,000 | 7.37 | 7.20 | 7.56 | 7.57 | 8.00 | 7.15 |
| …ex health | 4.33 | 4.23 | 4.43 | 4.51 | 4.70 | 4.32 |
| …pre cutoff | 0.64 | 0.56 | 0.74 | 0.73 | 0.67 | 0.79 |
| Healthcare/1,000 | 3.11 | 2.91 | 3.34 | 3.22 | 3.06 | 3.37 |
| Severe cases/1,000 | 1.43 | 1.27 | 1.61 | 1.48 | 1.37 | 1.59 |
| # Deaths | 25 | 9 | 16 | 6 | 3 | 3 |
| Age | 50.27 (5.89) | 48.89 (5.76) | 51.81 (5.65) | 50.46 (5.69) | 49.98 (5.66) | 50.92 (5.69) |
| Obs. | 480,291 | 253,538 | 226,753 | 166,630 | 81,598 | 85,032 |
Table 4.
Descriptive statistics: Teachers and teachers’ partners
| Teachers | Teachers’ partners | |||||
| Full sample | Lower sec. | Upper sec. | Full sample | Lower sec. | Upper sec. | |
| Cases/1,000 | 4.69 | 5.91 | 3.25 | 6.16 | 6.60 | 5.64 |
| …ex health | 4.21 | 4.99 | 3.26 | |||
| …pre cutoff | 0.27 | 0.25 | 0.30 | 0.59 | 0.63 | 0.55 |
| Healthcare/1,000 | 2.60 | 3.29 | 1.79 | 2.65 | 2.77 | 2.51 |
| Severe cases/1,000 | 1.59 | 2.00 | 1.10 | 1.25 | 1.33 | 1.16 |
| # Deaths | 1 | 1 | 0 | 1 | 1 | 0 |
| Age | 47.84 (10.61) | 47.37 (10.58) | 48.39 (10.62) | 49.17 (10.14) | 49.01 (10.18) | 49.36 (10.08) |
| Obs. | 72,946 | 39,446 | 33,500 | 47,383 | 25,587 | 21,796 |
Note: The table shows descriptive statistics teachers and teachers’ partners. “Cases/1,000” denotes positive PCR tests per 1,000 until June 15, 2020. “…ex. health” means that healthcare and care workers are dropped (occupational codes 15, 22, 32, and 53). “…pre cutoff” refers to cases before the specified cutoff dates referring to school closures. Cutoff dates are March 25 for teachers and April 1 for teachers’ partners. “Healthcare/1,000” shows open care, inpatient care, and deaths related to COVID-19 per 1,000, reported until June 30. “Severe cases/1,000” shows only inpatient care and deaths related to COVID-19 per 1,000, reported until June 30. The number of deaths shows reported deaths before July 26 among those tested positive until June 15. SD for age is shown in parentheses. “Obs.” refers to the number of observations in the sample. Individuals with a positive PCR test with an invalid date are excluded. “sec.” refers to secondary school.
The data cover the entire relevant Swedish population and contain all reported cases, as well as detailed information on covariates (see Materials and Methods and SI Appendix for details). Upper-secondary schools moved online on March 18. Allowing for an incubation period from infection to symptoms of about a week (22), the cutoff date is set to March 25 for teachers and April 1 for parents and teachers’ partners. The school year ends during the second week of June, and the end date is therefore set to June 15 for PCR tests and June 30 for diagnoses through healthcare contacts.
Parents.
Parental school exposure is defined by the school year that the youngest child in the household attends. In order to attribute estimated differences to school closures, households must be similar in all aspects that affect the likelihood of getting infected or tested, except for their exposure to open and closed schools. By narrowing the comparison to parents with the youngest child in the final year of lower-secondary school (year 9) and the first year of upper-secondary school (year 10), we reduce the risk of introducing biases due to confounding factors. A potential threat to identification is that students with non-EU migrant backgrounds are more likely to repeat grades in upper-secondary schools, in particular, through preparatory programs (19). Although upper-secondary grade repetition occurs also for other groups, the concern is not as severe among families from Sweden, the EU, and the Nordic countries. To avoid selection into grade 10 in upper-secondary school, we restrict the population to parents born in Sweden, EU, and the Nordics (dropping 16% of the parental population). In SI Appendix, we substantiate these claims by showing balance on covariates predicting the incidence of SARS-CoV-2 for the main sample (SI Appendix, Fig. S2), while balancing tests perform worse when including non-EU migrants (SI Appendix, Fig. S3).
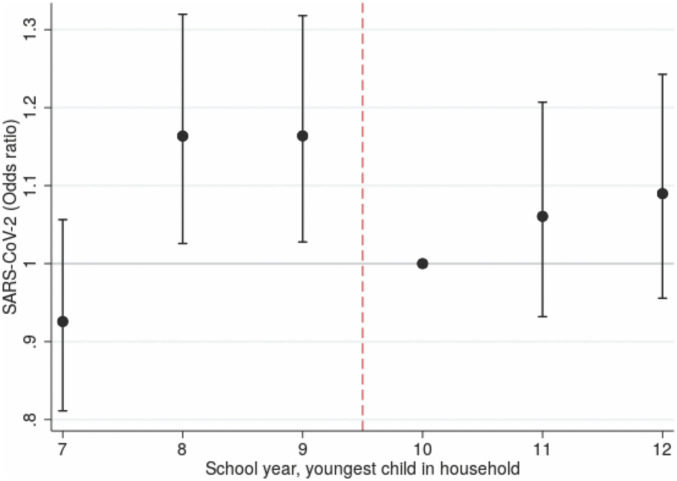
Fig. 2 shows the estimated odds ratios (ORs) for PCR-confirmed SARS-CoV-2 parents from logistic regressions, where we adjust for age, sex, occupation, educational attainment, income, and regions of residence and of origin. Results for parents by school years 7–12 show that there is a tendency of a positive age gradient, potentially indicating a higher parental risk of infection when exposed to older children. The most relevant comparison is therefore between school years 9 and 10 (reference category), for which we in Table 1 estimate an OR of 1.17 [95% CI (CI95) 1.03 to 1.32].
Fig. 2.
SARS-CoV-2 ORs for parents by school year of the youngest child in the household. ORs are estimated using logistic regression. The reference category is school year 10, and CI95 values are indicated.
Table 1.
Effect of exposure to open schools on PCR tests and COVID-19 diagnoses: Logit
| Logit (OR) | ||||||
| l)2-7 | Parents | Teachers | Partners | |||
| lr0.5em)2-3l0.5em)4-5l0.5em)6-7 | PCR | Diag. | PCR | Diag. | PCR | Diag. |
| Open | 1.17** [1.03, 1.32] | 0.94 [0.77, 1.14] | 2.01*** [1.52, 2.67] | 2.01*** [1.45, 2.79] | 1.29* [1.00, 1.67] | 1.04 [0.70, 1.52] |
| Obs. | 163,195 | 163,155 | 70,151 | 64,080 | 44,025 | 41,775 |
Results are estimated by using Logit. CI95 values are shown in brackets. “Open” indicates exposure to (open) lower-secondary schools. The outcome “PCR” refers to positive PCR tests, and “Diag.” refers to COVID-19 diagnoses. “Obs.” refers to number of observations in the regression. *P < 0.1; **P < 0.5; ***P < 0.01.
Corresponding results using OLS are shown in Table 2, which also includes results for COVID-19 diagnoses from healthcare contacts. The estimates indicate that parental exposure to open schools results in 1.05 (SE 0.43) additional SARS-CoV-2 cases per 1,000 individuals and (SE 0.26) additional COVID-19 diagnoses per 1,000. The OR for COVID-19 diagnoses is 0.94 [CI95 0.77 to 1.14]. The estimates for COVID-19 diagnoses are thus negative, albeit imprecise and statistically indistinguishable from zero. This indicates that the increase in PCR-confirmed cases does not necessarily translate into similar size effects on the probability to get a COVID-19 diagnosis when visiting a doctor or being admitted to hospital. The same applies to the estimates for severe cases shown in SI Appendix, Table S1 [OR 0.84; CI95 0.64 to 1.11].
Table 2.
Effect of exposure to open schools on PCR tests and COVID-19 diagnoses: OLS
| OLS (cases/1,000) | ||||||
| l0.5em)2-7 | Parents | Teachers | Partners | |||
| lr0.5em)2-3lr0.5em)4-5l)6-7 | PCR | Diag. | PCR | Diag. | PCR | Diag. |
| Open | 1.05** | 0.17 | 2.81*** | 1.47*** | 1.47** | 0.14 |
| (0.43) | (0.26) | (0.59) | (0.36) | (0.71) | (0.46) | |
| M. dep. | 6.37 | 2.74 | 2.96 | 1.61 | 5.10 | 2.29 |
| Obs. | 166,630 | 166,719 | 72,946 | 72,976 | 47,383 | 47,413 |
Results are estimated by using linear probability models (OLS). SEs in parentheses are clustered at the school level for teachers and their partners and at the household level for parents. “Open” indicates exposure to (open) lower-secondary schools. “M. dep.” refers to mean dependent variable for the reference category exposed to (online) upper-secondary schools. The outcome “PCR” refers to positive PCR tests, and “Diag.” refers to COVID-19 diagnoses. “Obs.” refers to number of observations in the regression. **P < 0.5; ***P < 0.01.
Teachers.
We analyze differences between lower- and upper-secondary teachers and their partners. Upper-secondary teachers constitute a relevant counterfactual to the work situation that lower-secondary teachers had been in if their schools had moved to online instruction. The groups are also similar with respect to educational attainment and geographic dispersion. As there may still be differences in the household composition between the groups, we—in addition to the controls used for parents—adjust for the occupation and educational attainment of teachers’ partners, the number of children in separate age groups linked to the household, and whether or not the teacher is single. Table 1 shows that the likelihood of a positive PCR test was twice as high for lower-secondary than for upper-secondary teachers [OR 2.01; CI95 1.52 to 2.67]. Table 2 shows a corresponding OLS estimate of 2.81 additional cases per 1,000 (SE 0.59). The estimate for COVID-19 diagnoses [OR 2.01; CI95 1.45 to 2.79], indicates that the PCR results are not due to biased testing. SI Appendix, Table S1 shows an estimate for severe cases of similar magnitude [OR 2.15; CI95 1.41 to 3.29].
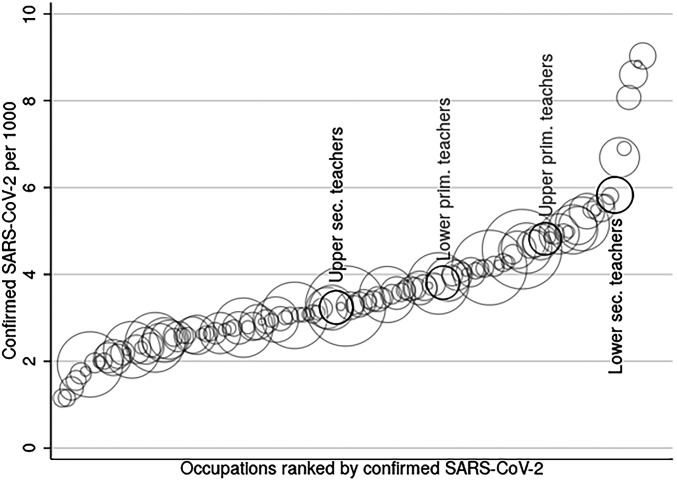
In order to gauge the magnitude of the estimated effects for teachers, Fig. 3 compares the incidence of detected SARS-CoV-2 among teachers with occupations at the three-digit level with at least 1,000 employees in ages 25–65 (healthcare workers excluded). Among the 124 compared occupations, upper-secondary teachers (3.25/1,000) are at the median, while lower-secondary teachers (5.91/1,000) constitute the seventh-most-affected occupation. Drivers (which includes taxi drivers) are the at the top of the distribution, while driving instructors have the same level of infections as lower-secondary teachers.
Fig. 3.
SARS-CoV-2 across occupations. Circle size corresponds to the number of employees in each occupation. Incidence (cases per 1,000) of detected SARS-CoV-2 by three-digit occupational codes (SSYK 2012) until June 15, 2020, is shown. Ages are 25–65, and only occupations with at least 1,000 employees are reported. Values for the upper- and lower-secondary teachers (as well as lower- and upper-primary teachers in gray) from the Teacher Register in our sample are indicated in black.
A list of all occupations is available in SI Appendix, Table S11. As another comparison, Tables 3 and 4 show that the incidence of SARS-CoV-2 is higher among lower-secondary teachers (5.91/1,000) than that of the parents to the students they teach (4.23/1,000, excluding healthcare workers). This is also the case for COVID-19 diagnoses and more severe health outcomes. Note that parents with non-EU backgrounds are excluded from these comparisons. The rate of infections is higher than average in this group, and, when included, the rate among lower-secondary parents increases to 5.33 cases per 1,000 (excluding healthcare).
Fig. 3 also indicates the incidence of detected SARS-CoV-2 among lower primary (school years 1–3; 3.81 cases per 1,000) and upper primary (years 4–6; 4.82 cases per 1,000) teachers. These teachers are less specialized and therefore not only meet younger, but also fewer, students than teachers at the lower-secondary level. They may also interact differently with their colleagues. The incidence among these teachers is below lower-secondary teachers, but above upper-secondary teachers, also when controlling for covariates (SI Appendix, Table S2). These results are consistent with a positive risk gradient in student age, but could reflect other differences in the work environment.
Teachers’ Partners.
The higher incidence of infections among lower-secondary teachers spilled over to their partners, who have a higher incidence of positive PCR tests than their upper-secondary counterparts [OR 1.29; CI95 1.00 to 1.67] (Table 1). This is evidence of within-household transmission from teachers to their partners. The estimates for teachers and their partners implies a secondary attack rate (SAR) between spouses of 0.52 [CI95 0.05 to 1.18].* This is well within the bounds of the between-spouse SAR of 0.43 [CI95 0.27 to 0.6] suggested from contact studies (23). However, the estimates for COVID-19 diagnoses for teachers’ partners are not statistically distinguishable from zero [OR 1.04; CI95 0.70 to 1.52], and the same applies for severe cases [OR 1.09; CI95 0.62 to 1.92] (SI Appendix, Table S1). The relatively imprecise estimates for these outcomes also renders them statistically indistinguishable from the estimates for PCR-confirmed SARS-CoV-2.
Robustness.
In SI Appendix, we provide several robustness tests of the main results. 1) Students in lower- and upper-secondary school are not fully comparable, as grade repetition is more common among the latter. Excluding covariates (except age and sex) in SI Appendix, Table S3 leads to a reduction in the estimates for parents [OLS 1.01, SE 0.43]. This is consistent with socioeconomic factors correlating both with upper-secondary grade repetition and the incidence of SARS-CoV-2. Dropping covariates (except age and sex) leads to a small increase in the estimated impact for teachers [2.94, SE 0.58] and their partners [1.58, SE 0.71]. Both results are consistent with lower-secondary partners being employed in more exposed occupations. Tests have already shown poor balance when including parents of non-EU background. However, widening the sample to include these parents does not substantially alter the results. The OLS estimates with controls [1.09, SE 0.42] and when only controlling for age and sex [1.02, SE 0.42] are similar to those for the main sample. ORs for both samples of parents are similar when only controlling for age and when excluding all controls (SI Appendix, Fig. S4). SI Appendix, Fig. S5 shows the ORs including all controls for the main sample (SI Appendix, Fig. S5A) as well as when non-EU migrants are included (SI Appendix, Fig. S5B). 2) Media searches reveal that some lower-secondary schools closed spontaneously and preemptively, albeit for brief periods of time (SI Appendix). As privately run independent schools were overrepresented in this group, we exclude individuals connected to such lower-secondary schools. This results in somewhat larger estimates for parents [1.33, SE 0.46] (SI Appendix, Table S4), consistent with balancing tests reflecting high socioeconomic status and, hence, less predicted exposure among these parents (SI Appendix, Fig. S6). Dropping independent lower-secondary schools only slightly affects the estimates for teachers [2.63, SE 0.63] and their partners [1.64, SE 0.77] (SI Appendix, Table S5). 3) It may have been more common among vocational programs to let small groups of students return to school to complete practical assignments. We therefore exclude parents connected to vocational upper-secondary programs. These tend to be of lower socioeconomic status, which is reflected in a poorly performing balancing test (SI Appendix, Fig. S6). Consistent with this test, the point estimate is reduced [0.64, SE 0.53] (SI Appendix, Table S4). 4) Rather than controlling for employment in the healthcare sectors, we drop teacher households where the partner is a healthcare employee. As expected, the results remain unchanged (SI Appendix, Table S5). 5) We derive a slightly different measure of parental exposure to lower-secondary schools that allows for a broader sample of parents, and the results are similar [0.98, SE 0.34] (SI Appendix, Table S4). 6) We broaden the comparison between lower- and upper-secondary parents by pooling those exposed to school years 8–11 and 7–12. This risks conflating the impact of exposure to open schools with student age. The estimate is lower for the 8–11 comparison [0.79, SE 0.31] and even lower, and insignificant, for years 7–12 [0.20, SE 0.26] (SI Appendix, Table S4). 7) Household size might affect the risk of infection, and it is decreasing by school year. Controlling for household size, however, does not affect the point estimates (SI Appendix, Table S6). 8) To ensure that the results are not sensitive to the choice of cutoff dates, we use March 25 and April 16 for all groups. Since fewer cases are detected from the latter date, the OLS estimates are slightly reduced, but the ORs are close to identical (SI Appendix, Table S7).
Heterogeneity.
How school closures affect the transmission of the virus depend on how they reduce contact between those potentially infected. This may differ depending on contextual factors, and we analyze two types of heterogeneity. First, we allow the estimates for exposure to lower-secondary schools to differ by population density in the district of residence. Second, since the timing of NPIs may affect their effectiveness (24), we let estimates vary by the regional rate of infections prior to school closure. The results in SI Appendix, Table S8 reveal interaction terms with large SEs, not allowing a clear interpretation.
Distribution of Cases across Schools.
Past coronavirus outbreaks (severe acute respiratory syndrome and Middle East respiratory syndrome) have shown large individual variation in infectiousness, implying that some individuals infected large numbers of secondary cases, leading to “superspreading events” (25). Estimates of the dispersion factor k—indicating heterogeneity in infectiousness—for SARS-CoV-2 vary, but suggest that this virus as well might spread in clusters (26, 27). If the spread is highly clustered and the virus spread at the schools, we would expect most of the cases to be concentrated to a few schools.
The data at hand are not ideal to study such transmission patterns, as the paucity of testing means that a large number of cases goes undetected. With this caveat in mind, SI Appendix, Fig. S7 shows how the cases are distributed across schools with different numbers of cases, and SI Appendix, Fig. S8 shows how cases are clustered in time within schools, separately for teachers and parents. There is some indication that cases among lower-secondary school teachers were relatively concentrated, but, among parents, the cases are more evenly distributed across schools and over time.
Students.
We do not study the impact of school closures on students, but for descriptive purposes, SI Appendix, Table S9 shows estimates of infection rates for students under age 18 in school years 7–10. The incidence for students in year 10 is 0.53 PCR-confirmed cases per 1,000, and estimated differences between school years are not statistically significant. Because of age-related differences in access to testing (SI Appendix), the severity of symptoms, risk behavior, and patterns of socialization, results for students are likely to be biased and difficult to interpret. It can be mentioned that there were zero COVID-19 deaths recorded in age groups 2–19 in Sweden until late July 2020. The rate of severe cases was also low; 94 hospitalizations were recorded among the 1.23 million students in compulsory school age 7–16 and 84 among the 339,000 youths ages 17–19 (SI Appendix, Table S10). There might be other health implications for children and adolescents, but analyzing this is beyond the scope of this study.
Discussion
On March 18, 2020, upper-secondary schools in Sweden moved to online instruction, while lower-secondary schools continued instruction as normal. This partial school closure provides a rare opportunity to study the impact on the transmission of SARS-CoV-2 during a period of widespread contagion. The impact of school closures on the transmission of the virus in society is best captured by the results for parents. We find that parental exposure to open, rather than closed, schools is associated with a somewhat higher rate of PCR-confirmed SARS-CoV-2 infections [OR 1.17; CI95 1.03 to 1.32]. The association is weaker for COVID-19 diagnoses from healthcare visits [OR 0.94; CI95 0.77 to 1.14] and severe cases that include hospitalizations and deaths [OR 0.84; CI95 0.64 to 1.11].
The positive association for PCR-confirmed cases could partly reflect other behavioral or biological differences between households with slightly younger and older children, but if treated as a causal, the estimates indicate that a hypothetical closure of lower-secondary schools in Sweden would have resulted in 266 fewer detected cases among the 253,538 parents in our sample. Limited testing capacity means that this only reflects a fraction of the actual number of cases, but it corresponds to a 15% reduction of the 1,825 detected cases among lower-secondary parents until mid-June (1,072 cases when excluding healthcare workers). Since sample restrictions are made, the actual number of parents exposed to lower-secondary schools is around 450,000 parents. The results thus indicate that closing lower-secondary schools would have resulted in a 17% decrease in infections among 4.5% of the Swedish population. It is important to note that this captures both primary and secondary infections among household adults, and the full implications for virus transmission have to be derived by using modeling. Although not conclusive in this regard, results are consistent with parental risk of infection increasing in student age. We might therefore somewhat underestimate the actual impact of keeping lower-secondary schools open. More importantly, this means that the implications of keeping upper- and lower-secondary schools open may not be symmetric.
Teachers were more severely affected by the decision to keep lower-secondary schools open. We estimate a PCR-confirmed infection rate twice as high among lower-secondary teachers relative to teachers at the upper-secondary level [OR 2.01; CI95 1.52 to 2.67]. This is fully consistent with the results for COVID-19 diagnoses from healthcare visits [OR 2.01; CI95 1.45 to 2.79] and severe cases [OR 2.15; CI95 1.41 to 3.29]. When excluding healthcare workers, a comparison of SARS-CoV-2 infection rates across 124 occupations shows that upper-secondary teachers are at the median, while lower-secondary teachers constitute the seventh-most-affected group. Other occupations with high infection rates (e.g., taxi drivers, driving instructors, social assistants, and police officers) tend to have close interactions at work. This suggests that infections occur at school, and there are some indications of clusters of cases among teachers. However, we cannot determine to what extent this is due to infections from students to teachers or if they reflect interactions between teachers. Primary-school teachers had lower rates of infection than teachers at the lower-secondary level, and the patterns are consistent with teacher risk increasing with student age. Alternative explanations, such as different modes of interactions between the teaching staff, are possible, and this highlights that the impact of keeping schools open may not be symmetric across educational settings.
Increased infections among lower-secondary teachers spill over to their partners, who have a higher PCR-confirmed infection rate than their upper-secondary counterparts [OR 1.29; CI95 1.00 to 1.67]. As for parents, the estimates are lower for COVID-19 diagnoses [OR 1.04; CI95 0.70 to 1.52] and severe cases [OR 1.09; CI95 0.62 to 1.92] among teachers’ partners.
Combining the estimates, 148 fewer cases of SARS-CoV-2 would have been detected among lower-secondary teachers (110) and their partners (38) if lower-secondary schools had closed. To this, we can add an estimate of 472 fewer cases among 450,000 adults exposed to lower-secondary students in their households. Most transmission is within households, so even if 620 fewer detected cases is a lower bound, this can be seen as relatively low compared to the country total of 53,482 detected cases until mid-June (35,556, excluding healthcare workers). Based on an age-specific case fatality rate of 1.1% (SI Appendix, Table S10), this corresponds to 6.5 fewer deaths, 5 among parents and 1.5 among teachers and their partners. This counterfactual inference regarding mortality is highly uncertain, however. In our sample, we count a total of 11 COVID-19–related deaths at the lower-secondary level (9 parents, 1 teacher, and 1 partner). The corresponding number at the upper-secondary level is 16 (all parents). For severe health outcomes, we find 79 cases among 39,446 lower-secondary teachers. According to the estimates, this number would have been down to 46 if lower-secondary schools had closed.
Closing the schools is a costly measure with potential long-run detrimental effects for students. The results presented are in line with theoretical work indicating that school closure is not an effective way to contain SARS-CoV-2 (5), at least not when facing as high a level of contagion as Sweden did during the spring of 2020. It is not clear how the results generalize to other settings, and studies have found both positive and negative associations between closed schools and the rate of transmission of SARS-CoV-2 (6, 11, 28, 29). The mixed evidence could reflect methodological differences and difficulties isolating the impact of schools. However, they could also reflect differences in how schools are organized and local conditions at the time of intervention. Unfortunately, our results do not allow any firm conclusions regarding interactions between school closures and local conditions. Another potentially important difference between settings is the level of the precautionary measures undertaken within schools. According to an international comparison (30), the measures recommended in Sweden (31) are best described as mild. In particular, there are no quarantine of those exposed unless they show symptoms of infection, there are no imposed class-size reductions, and face masks are rarely used (32).
While the overall impact on overall virus transmission was limited according to this study, keeping lower-secondary schools open had a quite substantial impact on teachers, and the results suggest that the risk to teachers can be increasing in student age. This should be taken into account, and precautionary measures could be considered.
Materials and Methods
We construct estimation samples for parents, teachers, and their partners using registers held by Statistics Sweden. Through the Multi-Generation register per December 31, 2019, and Longitudinal Integrated Database for Health-Insurance and Labour-Market Studies (LISA) per December 31, 2018, we identify all parents with children in relevant ages in their households. Children are assigned to school year, schools, and upper-secondary programs by using the Student Register as per October 15, 2019. We sample all parents in Sweden and their partners living in households with the youngest child in lower-or upper-secondary school. We also include parents with a biological or adopted child who does not live in the same household, but in the same region. The main analysis excludes parents born outside Sweden, the Nordic countries, and the EU. Information on detailed place of residence as of December 31, 2019, is available for all individuals in Sweden in the Register of the Total Population. The sample of teachers includes all teachers working at the lower- or upper-secondary levels in the Teacher Register and refers to the status of the teacher in the fall of 2019. Their partners are identified by using the household identifier in LISA. See SI Appendix for further details on the estimation samples. Information on the covariates—disposable income, educational attainment, and occupation—are available in LISA. Occupations are reported according to the Swedish Standard Classification of Occupations (SSYK 2012), which is based on the International Standard Classification of Occupations (ISCO-08). There are 46 occupation categories on the two-digit level.
Information on positive PCR tests of SARS-CoV-2 is from the Swedish Public Health Agency. Up until late July, there were 75,933 reported cases of SARS-CoV-2, out of which test dates are missing for 2,506 cases. As the majority of the cases without test dates are reported outside the main period of analysis, they are discarded. Personal identifiers are available for all cases, making it possible to link the test results to register data. Information on COVID-19 diagnoses until June 30 from the Inpatient-and Outpatient register is available from the National Board of Health and Welfare and on deaths from the Cause of Death register held by Statistic Sweden. By June 30, 2020, a total of 33,596 individuals had been diagnosed with COVID-19 (International Classification of Diseases 10 codes U07.1 or U07.2), either in the Patient Registers or the Cause of Death Register.
Tables 3 and 4 report descriptive statistics for parents, teachers, and teachers’ partners, starting with the incidence of positive PCR tests of SARS-CoV-2 as of June 15. Since healthcare workers were prioritized for testing, we also present the incidence excluding those working in healthcare. Healthcare workers are excluded by dropping those with occupational codes 15, 22, 32, and 53 (SSYK 2012). The tables further show the incidence of positive PCR test prior to the cutoff date chosen to reflect the infection rate prior to the move to online instruction at the upper-secondary level (March 25 for teachers and April 1 for parents and partners). The tables next display the incidence of COVID-19 diagnoses from healthcare visits and the incidence of severe cases as of June 30. Finally, they display the number of COVID-19–related deaths in each sample as of July 25 and the number of individuals in each group.
We use OLS and Logit to empirically analyze if SARS-CoV-2 infection can be attributed to being exposed to open or closed schools. We estimate the following OLS regression model for the three populations: parents, teachers, and teachers’ partners:
.The outcome is an indicator variable for a positive SARS-CoV-2 PCR test or being diagnosed with COVID-19 by a doctor in outpatient care or at a hospital. There is just one positive test per individual, and is an indicator for SARS-Cov-2/COVID-19 before the cutoff date. Including is a way of excluding preperiod cases without dropping such observations. is an indicator variable taking the value one if individual is exposed to (open) lower-secondary schools. Parents with the youngest child in lower-secondary school are defined as exposed, and parents with the youngest child in upper-secondary school are defined as unexposed. Lower-secondary teachers and their partners are defined as exposed and their upper-secondary counterparts as unexposed. X is a vector of individual and household characteristics. When estimating the model for teachers, the vector includes: 20 indicators for age categories (30 and below, 31–35, 36–40, biannual until age 66, 67–69, 70–74, 75–79, and 80+); sex; 7 indicators for categories of educational attainment; 46 indicators of categories of partners’ occupation; 12 region indicators of country of origin for those not born in Sweden; log of household income; indicator of having a teaching position; percent of full-time position; 290 indicators of municipality of residence; and household exposure to the number of children in age groups 2–6, 7–16, 17–19, and 20+, who reside in the same region as the teacher. The municipality fixed effects are exchanged for 21 region fixed effects when estimating the logistic model. The equivalent vector of variables is used for teachers’ partners, with the exception of own occupation instead of partner occupation. The vector of controls for parents include a similar set of variables as for teachers: age group categories, sex, municipality of residence, educational attainment, occupational categories (own and partners’), region of origin for those not born in Sweden (three indicators in the main sample), the log of disposable family income, and indicators for missing data on any of these variables. Migrants from non-EU/Nordic countries are excluded from the main sample of parents. SEs are clustered at the school level when estimating the model for teachers and teachers’ partners and at the household level when studying parents.
This project was approved by the Swedish Ethical Approval Board (Etikprövingsnämnden) on May 19, 2020 (decision number 2020-02323).
Supplementary Material
Acknowledgments
This work was supported by Handelsbankens Forskningssiftelser. We thank Jonas Björk, Lena Edlund, Jens Engleson, Tove Fall, Erik Grönqvist, Emily Oster, Oskar Nordström Skans, and David Strömberg for comments.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2020834118/-/DCSupplemental.
Data Availability.
Data are available from Statistics Sweden, the Public Health Agency, and the National Board of Health and Welfare following an ethical review. See SI Appendix for details on the respective databases. For further information on data availability and data access see ref. 33. Computer code is available at Open Science Framework (DOI: 10.17605/OSF.IO/4ZEGU).
References
- 1.UNESCO , 1.3 billion learners are still affected by school or university closures, as educational institutions start reopening around the world, says UNESCO (2020). https://en.unesco.org/news/13-billion-learners-are-still-affected-school-university-closures-educational-institutions. Accessed 14 August 2020.
- 2.Dorn E., Hancock B., Sarakatsannis J., Viruleg E.. COVID-19 and student learning in the United States: The hurt could last a lifetime (2020). https://www.mckinsey.com/industries/public-and-social-sector/our-insights/covid-19-and-student-learning-in-the-united-states-the-hurt-could-last-a-lifetime. Accessed 1 December 2020.
- 3.Guessoum S. B., et al. , Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 291, 113264 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bayham J., Fenichel E. P., Impact of school closures for COVID-19 on the US health-care workforce and net mortality: A modelling study. Lancet Public Health 5, e271–e278 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viner R. M., et al. , School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolescent Health 4, 397–404 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsiang S., et al. , The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 584, 262–267 (2020). [DOI] [PubMed] [Google Scholar]
- 7.Kraemer M. U. G., et al. , The effect of human mobility and control measures on the COVID-19 epidemic in China. Science, 368, 493–497 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan A., et al. , Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. J. Am. Med. Assoc. 323, 1915–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tian H., et al. , An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science 368, 638–642 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maier B. F., Brockmann D., Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China. Science 368, 742–746 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Auger K. A., et al. , Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA 324, 859–870 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ECDC . COVID-19 in children and the role of school settings in COVID-19 transmission, 6 August 2020 (2020). https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf Accessed 16 August 2020.
- 13.Goldstein E., Lipsitch M., Cevik M., On the effect of age on the transmission of SARS-CoV-2 in households, schools and the community. J. Infect. Dis., 10.1093/infdis/jiaa691 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stein-Zamir C., et al. , A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 25, 2001352 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szablewski C. M., SARS-CoV-2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. MMWR. Morb. Mortal. Wkly. Rep. 69, 1023–1025 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heavey L., Casey G., Kelly C., Kelly D., McDarby G., No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Euro Surveill. 25, 2000903 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macartney K., et al. , Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health 4, 807–816 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Public Health Agency of Sweden , Confirmed cases—daily updates (2020). https://www.arcgis.com/sharing/rest/content/items/b5e7488e117749c19881cce45db13f7e/data. Accessed 1 August 2020.
- 19.Swedish National Agency for Education . Elever i gymnasieskolan läsåret 2019/20 (dnr 2019:00860) (2020). https://www.skolverket.se/publikationer?id=6425. Accessed 30 October 2020.
- 20.Jackson C., et al. , The effects of school closures on influenza outbreaks and pandemics: Systematic review of simulation studies. PloS One 9, e97297 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R., Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 55, 105924 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lauer S. A., et al. , The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann. Intern. Med. 172, 577–582 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madewell Z. J., Yang Y., Longini I. M., Halloran M. E., Dean N. E., Household transmission of SARS-CoV-2: A systematic review and meta-analysis of secondary attack rate. JAMA Netw Open 3, e2031756 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caselli F. G., Grigoli F., Lian W., Sandri D., Protecting lives and livelihoods with early and tight lockdowns (2020). https://www.imf.org/-/media/Files/Publications/WP/2020/English/wpiea2020234-print-pdf.ashx. Accessed 1 December 2020.
- 25.Lloyd-Smith J. O., Schreiber S. J., Kopp P. E., Getz W. M., Superspreading and the effect of individual variation on disease emergence. Nature 438, 355–359 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Endo A., Abbott S., Kucharski A. J., Funk S., Estimating the overdispersion in COVID-19 transmission using outbreak sizes outside China. Wellcome Open Res. 5, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riou J., Althaus C. L., Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill. 25, 2000058 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haug N., et al. , Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. (2020). [DOI] [PubMed] [Google Scholar]
- 29.Isphording I. E., et al. , School re-openings after summer breaks in Germany did not increase SARS-CoV-2 cases. http://ftp.iza.org/dp13790. Accessed 1 December 2020.
- 30.Guthrie B. L., et al. , Summary of school re-opening models and implementation approaches during the COVID 19 pandemic (2020). https://globalhealth.washington.edu/file/6393/download. Accessed 1 December 2020.
- 31.Public Health Agency of Sweden . Suggestions for precautionary measures in preschool and compulsory school (2020). https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/verksamheter/information-till-skola-och-forskola-om-den-nya-sjukdomen-covid-19/forebyggande-atgarder-i-for–och-grundskola/. Accessed 28 January 2021.
- 32.YouGov . Personal measures taken to avoid COVID-19 (2020). https://today.yougov.com/topics/international/articles-reports/2020/03/17/personal-measures-taken-avoid-covid-19. Accessed 31 July 2020.
- 33.Statistics Sweden , Microdata at Statistic Sweden for research purposes. http://share.scb.se/OV9997/data/OV9999_2013A01_BR_X104BR1301.pdf. Accessed 5 February 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available from Statistics Sweden, the Public Health Agency, and the National Board of Health and Welfare following an ethical review. See SI Appendix for details on the respective databases. For further information on data availability and data access see ref. 33. Computer code is available at Open Science Framework (DOI: 10.17605/OSF.IO/4ZEGU).