Abstract
Background
This study aimed to evaluate the associations among oral health-related knowledge, attitudes, practice (KAP), self-rated oral health and oral health-related quality of life (OHRQoL) among Chinese college students.
Methods
Of the 2000 participants, 1751 (87.55%) students answered an online questionnaire between October 2019 and January 2020. The questionnaire included demographic characteristics, knowledge, attitudes, and practice related to oral health, self-rated oral health, and OHRQoL. Structural equation modelling was applied to assess the associations among study variables.
Results
Among the total students, oral health-related knowledge and attitudes were satisfactory, while the oral health practice was not optimistic. The final model showed satisfactory fitness to the data. Oral health knowledge was associated with attitudes directly and positively. Attitudes toward oral health had a direct and positive effect on practice. Oral health knowledge had an indirect effect on practice through attitudes. Oral health practice was directly associated with self-rated oral health. Oral health knowledge, practice, and self-rated oral health all affected OHRQoL directly and positively, while attitudes had a direct negative impact on OHRQoL.
Conclusions
OHRQoL was influenced by oral health knowledge, attitudes, practice, and self-rated oral health. Our findings support the KAP theory. Limitations of the KAP model were also found.
Keywords: Knowledge-attitudes-practice, Self-rated oral health, Oral health-related quality of life, Structural equation modeling, Chinese college students
Background
Good oral health is an essential component to maintain and improve general health and quality of life. Oral health-related quality of life (OHRQoL) can be used to measure the impact of oral health on an individual’s quality of life [1–3]. OHRQoL represents the subjective perception of oral conditions and subjective evaluation of physical function, psychological function, and social activity aspects of oral health [4–6]. OHRQoL can also assess the relationship between oral status and general health from subjective perspectives and experiences [7–9].
It is important to have a good OHRQoL for college students, who play a significant role in the future development of a country, eventually becoming the future promoters of social progress [10, 11]. Compared with middle-aged people, young college students are in a dynamic growth period, and their health, social psychology, lifestyles, and behaviours are more likely to change [11, 12]. Poor OHRQoL can negatively affect college students' oral health condition and general well-being in the future [13, 14]. Therefore, it is particularly important to identify factors associated with the OHRQoL of college students, in which it is conducive to determine oral health promotion intervention strategies [15].
Assessment of self-rated oral health is considered a valid and useful measurement indicator of oral health conditions in epidemiology, which can easily and simply evaluate the individual general oral health status [16–18]. Information on self-rated oral health can help dental clinicians determine routine diagnostic procedures [19] and assess the demand for treatment [20]. In addition, the evaluation of self-rated oral health can help individuals recognise the importance of regular dental check-ups [21].
Self-rated oral health is related to subjective perception factors and clinical oral factors [19–21]. Subjective perception factors include reported general oral health status and the presence of abnormal oral symptoms [20]. They are thought to affect self-rated oral health, which can further influence participants' quality of life [11, 19]. In addition, a study done by Yamane, et al. in Japan identified that self-related oral health was associated with OHRQoL in Japanese young adults [18]. However, few studies have been conducted to demonstrate the relationship between OHRQoL and self-rated oral health among college students in China.
Knowledge, attitudes, and practices (KAP) theory is one of the theoretical models used to change human health-related behaviours [22]. The KAP theory holds that healthy knowledge is the basis for establishing positive attitudes and healthy behaviours, and attitudes are the driving force of behavioural change, and promoting healthy behaviours is the goal [22]. Previous studies assessed the status of oral health-related knowledge, attitudes, and practices targeting different groups of people [23–26]. However, few studies have been conducted on the strength of the relationships between knowledge, attitudes, and practice related to oral health [18].
According to KAP theory, there is a causal relationship between knowledge, attitudes, and practice [27]. However, knowledge, attitudes, and practice are all potential variables that are difficult to measure directly. The traditional multivariate statistical method can only identify the factors that affect knowledge, attitudes, and practice, but cannot elucidate the complex causal relationships involved in the process. In comparison, structural equation modelling (SEM) is a far superior statistical technique, which can compensate for the defects of traditional statistical methods. This multivariate statistical analysis technique can deal with potential variables, observation indexes, and measurement errors simultaneously [28–30]. Furthermore, it can explore the causal relationships among potential variables and quantitatively evaluate the direct and indirect effects of variables [28–30]. To date, the SEM approach has been widely used in psychology, behavioural and social science, biomedicine, management, and other fields [31, 32].
This study aimed to evaluate the associations among oral health-related knowledge, attitudes, practice, self-rated oral health, and OHRQoL in a group of Chinese college students based on the KAP theory using an SEM approach.
Methods
Subjects and design
We used the convenience sampling technique to conduct this cross-sectional survey.
The sample size was calculated using the population proportion statistical formula [33]. N = Z2P (1 − P) d2 (Z = 1.96, P = 60.1%, d = 0.05), where Z = critical value corresponding to 95% confidence level = 1.96; P = Proportion with parameter (the awareness rate of oral health knowledge = 60.1%, which was from a previous study [34]). Therefore, the calculated sample size was 368 and, after considering a 20% non-response rate, the minimum required sample size was 441. However, a total sample size of 1751 was used for this study. Our sample size exceeded the minimum requirement. A sufficient sample size ensures the credibility of the research results.
College students were invited to participate in this study from a total of 22 universities throughout the northern (8 universities), southern (7 universities), and central (7 universities) regions of the Anhui Province located in the east of China. Participating universities were those that had responded positively to invitations to help collect data. Data were collected from 1 October 2019 through 26 January 2020.
We conducted a web-based questionnaire. The link to the online questionnaire was sent to administrators from the invited universities for distribution to registered college students. The link to the survey was also sent to students’ social media groups or forums. Furthermore, we encouraged the students who had received an online questionnaire to forward the link to their classmates. After providing informed consent, participants completed the anonymous online questionnaire independently. On average, questionnaires were completed within approximately 10–15 min.
The inclusion criteria were as follows: (1) no reading and comprehension disability; and (2) voluntary participation in the study and providing oral informed consent. The exclusion criteria were as follows: (1) incomplete data; (2) mental illnesses; and (3) reluctance to participate after the study was explained.
In total, 2000 college students were recruited for this study. A total of 1817 students completed the online questionnaire, with a response rate of 90.85%. However, 66 questionnaires were excluded because of too many missing values (> 10%). Ultimately, a total of 1751 complete and valid questionnaires were collected with an effective response rate of 87.55%.
Survey instruments
The original questionnaire was developed referring to the relevant literature review and the 4th National Oral Health Survey in the Mainland of China [34]. The items in the questionnaire were validated by several experts. The questionnaire was pre-tested on randomly sampled college students before the formal survey. The questionnaire was improved according to the results of the preliminary investigation and opinions of experts.
The questionnaires addressed socio-demographic characteristics, oral health-related knowledge, attitudes, practice, self-rated oral health, and OHRQoL.
The question ‘In general, how would you evaluate your oral health?’ was used to assess self-rated oral health. It was measured using a Likert scale with five options, whereby 1 was ‘very good’, and 5 was ‘very poor’ [11, 18]. Low scores reflected a good self-assessment of oral condition.
Oral health-rated knowledge consists of 9 items, for example ‘Plaque can cause tooth decay and periodontal disease, including gingivitis and periodontitis’ (K1); ‘Fluoride toothpaste can prevent caries’ (K2); ‘See your dentist or hygienist for regular dental exams that can help detect oral problems early and maintain your dental health’ (K3); ‘A regular dental deep cleaning using the ultrasonic dental scaler can maintain good oral hygiene’ (K4); ‘In the early stages of gingivitis, the gums bleed when brushing or biting hard objects’ (K5); ‘Acute pulpitis can produce intense spontaneous pain, nocturnal pain’ (K6); ‘Caries are often characterized by irritation, biting discomfort or pain’ (K7); ‘Halitosis is mainly caused by oral diseases’ (K8) and ‘Pit and fissure sealants can protect the teeth and prevent dental caries’ (K9). Response options were ‘True’ or ‘False’. The correct answer was scored 1, and incorrect answers were scored 0. The final scores of oral health-rated knowledge ranged from 0 to 9. Higher scores indicated better oral health knowledge. The total awareness rate of oral health knowledge was equal to the total number of knowledge questions answered correctly/(the number of knowledge items in each questionnaire × the number of effective response participants) × 100%. The awareness rate of each oral health knowledge question was equal to the number of participants answered correctly/the number of effective response participants × 100%.
Attitudes toward oral health care were measured using 4 items. They included ‘Do you think that oral diseases can harm the general health?’ (A1); ‘Do you think eating sweets (such as cakes, biscuits and juices) and carbonated drinks will not cause tooth decay?’ (A2); ‘Do you think regular cleaning is good for oral health?’ (A3) and ‘Do you think oral diseases can be prevented?’ (A4). The possible response was three options, whereby 0 was ‘Disagree’, 1 was ‘Uncertain’, and 2 was ‘Agree’. The final scores of attitudes toward oral health ranged from 0 to 8. Higher scores represented more positive attitudes toward oral health. The total holding rate of positive attitudes toward oral health was equal to the total number of positive attitudes questions/(the number of attitudes items in each questionnaire × the number of effective response participants × 100%. The holding rate of each positive attitudes questions was equal to the number of participants who opted ‘Agree’/the number of effective response participants × 100%.
Oral health practice was assessed using 8 items, which included ‘Do you brush your teeth more than twice a day?’ (P1); ‘Is your brushing time ≥ 3 min each time?’ (P2); ‘Do you often use fluoride toothpaste?’ (P3); ‘Do you think regular oral check-ups are good for oral health?’ (P4); ‘Do you change a toothbrush every three months?’ (P5); ‘Do you often use dental floss (or an interdental brush) to help clean your teeth?’ (P6); ‘Is your brushing method recommended by the Chinese association of stomatology as “horizontal vibrating brush method”?’ (P7) and ‘Do you often gargle after meals?’ (P8). Dichotomic answers: ‘Yes’ or ‘No’. Each of the items was scored 1 if conducted by the participant. The final scores of oral health practice ranged from 0 to 8.
Higher scores indicated better oral hygiene practices. The total execution rate of right oral health practice was equal to the total number of practice questions opted ‘Yes’/(the number of practice items in each questionnaire × the number of effective response participants) × 100%. The execution rate of each right oral health practice was equal to the number of participants opted ‘Yes’/the number of effective response participants × 100%.
Confirmatory factor analysis (CFA) and Cronbach's alpha were used to confirm the validity and reliability of the questionnaire. Cronbach's α for the KAP was α = 0.737.
The OHRQoL was assessed using the Chinese version of the OHIP-14 in our study [35] (Table S2). It can capture functional and psychosocial impairment aggravated by an oral health condition [36]. OHIP was first designed by Slade in 1994 [37], which contains 49 entries, namely OHIP-49. Three years later, Slade developed a short version of OHIP-14 based on OHIP-49 [1], which had good reliability, validity, and accuracy [38]. The OHIP-14 includes 14 items that explore the following 7 conceptual dimensions: functional limitation, physical pain, psychological discomfort, physical disability, social disability, and perceived handicap to measure the self-reported frequency of discomfort symptoms [39]. The responses included ‘very often = 4’, ‘often = 3’, ‘sometimes = 2’, ‘rarely = 1’ or ‘never = 0’ according to a five-point Likert scale. The higher the score on the OHIP-14, the worse the oral health status [40–42]. In this study, Cronbach’s α for the OHIP-14 CHN was α = 0.97.
Statistical analysis
IBM® SPSS® Statistics 25.0 and IBM® SPSS® Amos™ 24.0 were used for data analysis.
Mean ± standard deviation or frequency and percentage were used to describe the demographic information and oral health status of the participants.
We used the skewness–kurtosis test to check the normality of the study variables. The sample data showed a normal distribution, where the absolute value of skewness was < 3 and the absolute value of kurtosis was < 8 [43].
Spearman’s correlation was used to evaluate correlations between latent variables. All differences were assessed using two-tailed tests, and the significance level was set at p < 0.05.
A structural equation model was constructed to determine the relationship between oral health knowledge, attitudes, practice, self-rated oral health, and OHRQoL.
The bootstrap method [44] was used to test the significance of the mediating effect of related variables in the ideal model. In addition, a bias-corrected bootstrap 95% confidence interval (CI) was used to examine the significance of direct and indirect effects [45, 46].
The maximum likelihood estimate (MLE) was used for parameter estimation, and the test level was set to α = 0.05. We used the root mean square error of approximation (RMSEA), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), comparative fit index (CFI), incremental fit index (IFI), normed fit index (NFI), chi-square/degrees of freedom (χ2/df), and other indicators to evaluate the fitting effect of the model [47, 48].
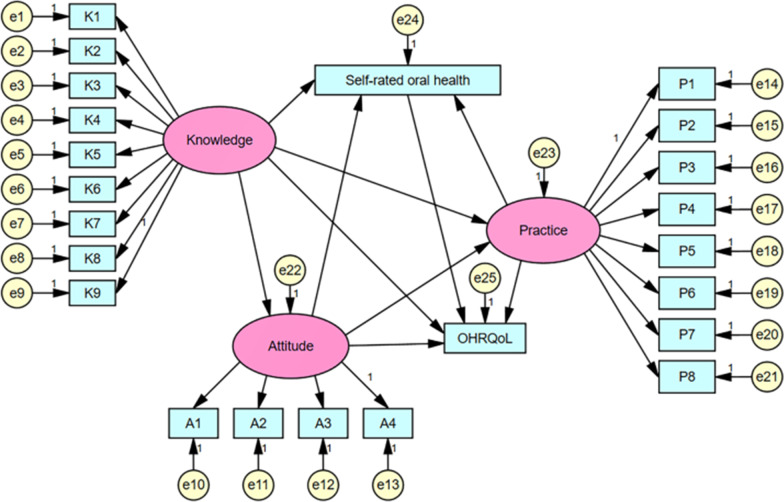
According to our hypothesis, Fig. 1 shows the ideal SEM of association among oral health-rated knowledge, attitudes, practice, self-rated oral health, and OHRQoL in a sample of college students in China.
Fig. 1.
The ideal SEM. Rectangles show observed variables, ellipses indicate potential variables, and circles represent residual terms
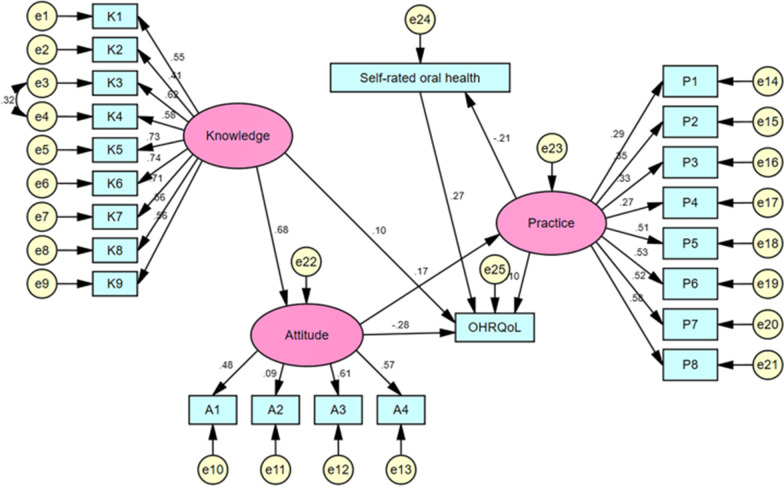
We removed the corresponding paths, because the path coefficients of ‘knowledge’ on ‘self-rated oral health’, ‘knowledge’ on ‘practice,’ and ‘attitudes’ on ‘self-rated oral health’ were not statistically significant in the ideal SEM fitting results (All p > 0.05).
In addition, the covariant relationships between e3 and e4 were established. Through repeated modification and fitting of the model, the fit indices of SEM finally reached the adaptation standards: χ2/df = 3.459, RMSEA = 0.037, GFI = 0.961, AGFI = 0.951, NFI = 0.900, IFI = 0.927, CFI = 0.926, PGFI = 0.780, PNFI = 0.797, and PCFI = 0.820.
The Cronbach's α value of the final SEM was 0.703 and the KMO value was 0.879, showing good reliability and validity [49, 50].
Results
Sample characteristics
As a result, we analysed data from 1751 college students (757 males, 994 females) aged 22.01 ± 4.83 years in this study. Overall, 17.76% of the participants had a healthier self-rated oral status, of which 4.97% were very good, and 12.79% were good. The mean total OHIP-14 score of the participants was 13.29 ± 12.15. Table 1 shows the specific demographic data, self-rated oral health, and mean total OHIP-14 score.
Table 1.
Demographic characteristics, self-rated oral health and OHIP-14 score of participants (n = 1751)
| Variable | Number | Constituent ratio/% |
|---|---|---|
| Gender | ||
| Male | 757 | 43.23 |
| Female | 994 | 56.77 |
| Major | ||
| Stomatology major | 277 | 15.82 |
| Medical non-oral specialty | 651 | 37.18 |
| Non-medical major | 823 | 47.00 |
| Annual household economic income | ||
| < ¥50,000 | 755 | 43.12 |
| ¥50,000–120,000 | 717 | 40.95 |
| > ¥120,000 | 279 | 15.93 |
| Family origin | ||
| Rural areas | 996 | 56.88 |
| Urban areas | 755 | 43.12 |
| Educational level | ||
| Freshman | 464 | 26.50 |
| Sophomore | 251 | 14.33 |
| Junior | 482 | 27.53 |
| Senior | 201 | 11.48 |
| Graduate | 172 | 9.82 |
| First-year graduate | 78 | 4.45 |
| Second-year graduate | 41 | 2.34 |
| Third-year graduate | 62 | 3.54 |
| Only-child or not | ||
| Yes | 532 | 30.38 |
| Two | 1027 | 58.65 |
| Three | 136 | 7.77 |
| Four or more | 56 | 3.20 |
| Self-rated oral health | ||
| Very good | 87 | 4.97 |
| Good | 224 | 12.79 |
| Fair | 1160 | 66.25 |
| Poor | 243 | 13.88 |
| Very poor | 37 | 2.11 |
| Oral Health Impact Profile-14 | ||
| Total | 13.29 ± 12.15a | |
| Age | 22.01 ± 4.83 | |
aMean ± SD
Descriptive analysis for oral health-related knowledge, attitudes, practice
The total awareness rate of oral health knowledge among college students was 86.26%. The total holding rate of positive attitudes toward oral health was 78.36%, which was slightly lower than that of knowledge, but most participants had favourable attitudes. The total execution rate of right practice toward oral health was 45.43%. The specific values are shown in Table 2.
Table 2.
Descriptive statistics for oral health-related knowledge, attitudes, practice
| M ± SD (range) | N (%) | M ± SD (range) | N (%) | M ± SD (range) | N (%) | |||
|---|---|---|---|---|---|---|---|---|
| K1 | 0.90 ± 0.30 (0–1) | 1574 (89.89) | A1 | 1.71 ± 0.58 (0–2) | 1362 (77.78) | P1 | 0.74 ± 0.44 (0–1) | 1292 (73.79) |
| K2 | 0.79 ± 0.41 (0–1) | 1381 (78.87) | A2 | 1.43 ± 0.85 (0–2) | 1162 (66.36) | P2 | 0.57 ± 0.50 (0–1) | 993 (56.71) |
| K3 | 0.88 ± 0.32 (0–1) | 1543 (88.12) | A3 | 1.78 ± 0.56 (0–2) | 1496 (85.44) | P3 | 0.42 ± 0.49 (0–1) | 744 (42.49) |
| K4 | 0.85 ± 0.36 (0–1) | 1489 (85.04) | A4 | 1.76 ± 0.59 (0–2) | 1468 (83.84) | P4 | 0.78 ± 0.41 (0–1) | 1367 (78.07) |
| K5 | 0.89 ± 0.31 (0–1) | 1565 (89.38) | P5 | 0.20 ± 0.40 (0–1) | 351 (20.05) | |||
| K6 | 0.90 ± 0.30 (0–1) | 1573 (89.83) | P6 | 0.37 ± 0.48 (0–1) | 652 (37.24) | |||
| K7 | 0.90 ± 0.31 (0–1) | 1568 (89.55) | P7 | 0.39 ± 0.49 (0–1) | 681 (38.89) | |||
| K8 | 0.83 ± 0.38 (0–1) | 1452 (82.92) | P8 | 0.16 ± 0.37 (0–1) | 284 (16.22) | |||
| K9 | 0.83 ± 0.38 (0–1) | 1448 (82.70) | ||||||
| K | 7.76 ± 2.02 (0–9) | 86.26% | A | 6.68 ± 1.56 (0–8) | 78.36% | P | 3.63 ± 1.91 (0–8) | 45.43% |
M, Mean; SD, Standard Deviation; K, Total awareness rate of oral health knowledge; A, Total holding rate of positive attitudes toward oral health; P, Total execution rate of right practice toward oral health
Correlation analysis among latent variables
There were positive correlations between oral health-related knowledge, attitudes, and practice (r = 0.437, 0.162, 0.095, all p < 0.01). The results are shown in Table 3.
Table 3.
Correlation analysis among latent variables
| Knowledge | Attitudes | Practice | |
|---|---|---|---|
| Knowledge | – | ||
| Attitudes | 0.437** | – | |
| Practice | 0.162** | 0.095** | - |
**p < 0.01 (two-tailed)
Structural equation model
Figure 2 shows the final SEM model. As shown in Fig. 2 and Table 4: (1) Knowledge had a direct effect on attitudes, with a direct effect value of 0.68. The direct effect of attitudes on practice was 0.17; the indirect effect of knowledge on practice through attitudes was 0.12, 95% CI: 0.06–0.17. Therefore, attitudes play a complete mediating role between knowledge and practice. (2) Practice had a direct and negative effect on self-rated oral health with an effect value of − 0.21. (3) Students' knowledge, attitudes, practice, and self-rated oral health all had direct influences on OHRQoL (all p < 0.05), and the direct effect values were 0.10, − 0.28, 0.10, and 0.27, respectively.
Fig. 2.
The final SEM. Rectangles show observed variables, ellipses indicate potential variables, and circles represent residual terms. The values of single-headed arrows represent the standardized coefficients. All pathways were significant (p < 0.05). OHRQoL was associated with oral health-related knowledge, attitudes, practice and self-rated oral health status
Table 4.
Bootstrap analysis of mediating effect significance test for the final mode
| Model paths | Standardized direct effects | 95% CI | Standardized indirect effects | 95% CI | ||
|---|---|---|---|---|---|---|
| LLCI | ULCI | LLCI | ULCI | |||
| Knowledge → Attitudes | 0.68*** | 0.60 | 0.75 | – | – | – |
| Attitudes → Practice | 0.17*** | 0.09 | 0.25 | – | – | – |
| Practice → Self-rated oral health | − 0.21*** | − 0.27 | − 0.15 | – | – | – |
| Self-rated oral health → OHRQoL | 0.27*** | 0.22 | 0.32 | – | – | – |
| Knowledge → Practice | – | – | – | 0.12*** | 0.06 | 0.17 |
| Knowledge → Self-rated oral health | – | – | – | − 0.03*** | − 0.04 | − 0.01 |
| Attitudes → Self-rated oral health | – | – | – | − 0.04*** | − 0.06 | − 0.02 |
| Knowledge → OHRQoL | 0.10* | 0.00 | 0.22 | − 0.18*** | − 16.63 | − 6.16 |
| Attitudes → OHRQoL | − 0.28*** | − 0.40 | − 0.17 | 0.01 | − 0.10 | 0.85 |
| Practice → OHRQoL | 0.10 ** | 0.03 | 0.17 | − 0.06*** | − 8.13 | − 3.40 |
All of the direct effects were significant (p < 0.05); *p < 0.05; **p < 0.01; ***p < 0.001
Among them, self-rated oral health had the greatest impact on OHRQoL (β = 0.27), followed by knowledge (β = 0.10), and practice (β = 0.10), and attitudes had a negative effect (β = − 0.28).
Discussion
This study aimed to explore the relationships between oral health-related knowledge, attitudes, practice, self-rated oral health, and OHRQoL among Chinese college students. The results showed that oral health-related knowledge and attitudes were satisfactory, and still need to be further improved, while oral health-related practice was at a slightly lower level. Oral health knowledge directly and positively affected attitudes. Attitudes toward oral health were directly and positively associated with oral health practice. Oral health knowledge had an indirect effect on practice through attitudes. Oral health practice was directly associated with self-rated oral health. Besides, oral health knowledge, practice, and self-rated oral health were found to be directly and positively associated with OHRQoL, while attitudes were negatively associated with OHRQoL among Chinese college students. To our knowledge, this study was one of the few studies that analysed the interaction mechanism of oral health-related KAP using SEM in a group of Chinese college students. Meanwhile, the current study was the first to explore the association between oral health-related KAP, self-rated oral health, and OHRQoL in this population in China.
Current status of oral health related KAP
To date, only a few investigations on ‘Knowledge-Attitudes-Practice’ have been conducted targeting Chinese college students' oral health based on the KAP theory. Similar studies in other countries used the Hiroshima University-Dental Behavioural Inventory (HU-DBI) questionnaire to survey dental health attitudes, perception, and behaviour [51, 52].
Our results showed that the awareness rate of oral health knowledge in Chinese college students was satisfactory. This was much higher than the results of the studies conducted by Liu et al. (37.6%) [53] and Chen, et al. (53.85%) [54] for Chinese comprehensive university students, and even higher than the findings (60.1%) from the fourth national oral health survey in the mainland of China targeting national residents [34]. This study also found that it was ideal for the holding rate of positive attitudes toward oral health, but this was lower than the findings (84.9%) of mainland residents revealed in the fourth national oral health survey of China [34]. However, our study showed that the execution rate of oral health behaviour of the participants was not optimistic, which needs improvement and deserves social attention. This result was slightly lower than the results of the study conducted by Abu-Gharbieh et al. targeting adult residents in the United Arab Emirates [55]. They reported that 53% of the participants performed better oral health behaviours. The different results of the mentioned studies may be due to the respective study design and survey instrument.
Notably, we found that the levels of oral health knowledge and attitudes were not coordinated with oral health behaviour. This might be explained by the fact that participants' acquisition of oral health knowledge did not lead to oral hygiene behavioural changes, which is a disconnect between knowledge and practice.
Spearman’s correlation analysis showed that there were positive correlations between oral health knowledge, attitudes, and practice among college students in China. This result supports the KAP theory about the causal chain of knowledge, attitudes, and practice [22]. Oral health education may be an effective strategy to improve college students’ knowledge, attitudes, and practice related to oral health [56].
The SEM model was constructed based on the KAP theory in our study. The KAP theory was developed as a human health promotion model [57]. It asserted that the change in human behaviour could be divided into three continuous processes: knowledge acquisition, belief generation, and practice/behaviour formation [57]. Knowledge, attitudes, and practice should have a positive relationship according to KAP theory [57]. In this study, the final model showed that there was a significant positive relationship between oral health knowledge and attitudes, and attitudes had a positive and direct effect on oral hygiene practice. However, oral health knowledge did not exhibit a direct relationship with practice.
Another noteworthy finding of our study was that oral health knowledge can indirectly and significantly affect oral hygiene practices through attitudes, that is, attitudes toward oral health played a mediating role in the KAP model for oral health. This finding was supported by scholars in other fields, and they also confirmed that knowledge can indirectly affect practice through attitudes [58, 59]. This indicates that obtaining oral health knowledge would motivate positive attitudes to get information about oral health and to perform oral health practice. Therefore, oral health knowledge is considered a prerequisite for oral health practice.
It is worth noting that our study demonstrated that the path coefficient for the direct effect of attitudes on practice was estimated to be β = 0.17, while the indirect effect of knowledge on practice was 0.12. These findings indicate that the influence of knowledge and attitudes on practice is limited. The possible reasons are explained by a limitation of the model in this study. Moreover, this may also reflect the limitation of the KAP theory in health behaviour interventions. In addition, a previous study showed that practice, apart from being correlated to both knowledge and attitudes, was also related to other factors, such as psychological factors [60, 61], level of education [62], family factors [56], and social environmental factors [63, 64].
Oral health related KAP, self-rated oral health and OHRQoL
Our study found that oral health knowledge and practice had significant, direct, and positive effects on OHRQoL among college students, which indicated that these two variables can be effective in changing oral health-related quality of life. The results of the study conducted by Alsumait et al. [65] were similar to our research findings. They reported that oral health knowledge and practice of primary school teachers were significantly associated with their OHRQoL. Furthermore, other studies confirmed a possible association between oral hygiene practice and OHRQoL [66–68].
This study also observed that attitudes toward oral health had a negative influence on OHRQoL. This finding was inconsistent with previous research [65]. The probable reason is that turning positive attitudes into positive practice might need to take time, so the improvement in oral health-related quality of life is not obvious.
A direct negative association was found between oral health practice and self-rated oral health in this study. This demonstrates that the higher scores of oral health practice, the lower the scores of self-assessments of oral health, according to the scoring method in our questionnaire design. In other words, better oral hygiene practice can improve self-assessment of oral condition. This result is consistent with those of previous studies targeting Japanese university students [16, 69].
This study also observed that self-rated oral health status had the greatest positive effect on OHRQoL, compared with other parameters (knowledge, attitudes, and practice). This finding implies that self-rated oral health status may play a superior role in determining OHRQoL. In other words, better self-related oral health resulted in better OHRQoL. This finding was supported by a similar study conducted by Yamane et al. in Japan [16], which reported that self-rated oral health was related to OHRQoL in a young Japanese population. In addition, this association was also observed in older Australians [69].
Analyses of deleted paths
The model and path analysis showed that the path from knowledge and attitudes to self-rated oral health did not fit the final model in this study. Furthermore, the direct path from oral health knowledge to practice was also removed. However, previous studies have shown a possible correlation between oral health knowledge, attitudes, and self-rated oral health [62, 70]. KAP theory also suggested that knowledge had a direct impact on practice [57]. The reason for the different results may be because of the respective survey design and the different demographic characteristics of participants (college students aged 22.01 ± 4.83 years from Anhui, China vs. Middle school students aged 15 to 16 years from Luma, Finland, or Lebanese pharmacists aged 39.3 ± 10.68 years) [62, 70].
Limitations
Our study has several limitations. First, the main challenge with the use of SEM is the inability to establish inferential causality in this cross-sectional study. Second, there may be a few self-reported questionnaire design flaws in this study, which might cause potential bias and lead respondents to provide socially acceptable responses. In addition, only college students in Anhui Province (China) were included as participants in our study, which may limit the generalizability of the results. Third, in the SEM analysis, the oral health-related knowledge, attitudes, practice, self-rated oral health, and OHRQoL were included. However, other relevant variables may exist, such as individual characteristics (gender, grade, and major) and environmental characteristics (family economic annual income and parents' education level) that Wilson and Cleary had put forward [71]. The results should be interpreted with caution. Further, more large-scale in-depth studies are needed in the future.
Conclusions
The results of this study showed that oral health knowledge and attitudes were satisfactory among Chinese college students, while their oral health practices were not optimistic. In addition, a direct positive relationship existed between oral health knowledge and attitudes. A direct positive association was found between oral health attitudes and oral health practices, and attitudes played a complete mediating role between knowledge and practice. OHRQoL was associated with oral health-related knowledge, attitudes, practice, and self-related oral health in this group of college students in China. Our findings support the KAP theory regarding the causal chain of knowledge, attitudes, and practice. Limitations of the KAP model were also found.
Acknowledgments
The authors would like to thank all participants for taking part in this study and all the people who kindly helped us in conducting this research.
Abbreviations
- SEM
Structural equation modelling
- KAP
Knowledge, attitudes, and practices
- CFI
Comparative fit index
- GFI
Goodness of fit index
- AGFI
Adjusted goodness of fit index
- NFI
Normed fit index
- RFI
Relative fit index
- IFI
Incremental fit index
- PNFI
Parsimonious normed fit index
- PCFI
Parsimony comparative of fit index
- PGFI
Parsimony goodness of fit index
- TLI
Tucker-Lewis index
- RMR
Root mean square residual
- RMSEA
Root mean square error of approximation
- MLE
Maximum likelihood estimate
- SD
Standard deviation
- OHRQoL
Oral health-related quality of life
- CI
Confidence interval
Authors’ contributions
SHZ and SKL gave substantial contributions to conception and design of this study. SHZ made critical revisions of the manuscript and supervised the whole process. SGZ performed the statistical analysis and drafted the initial manuscript. SGZ, SHZ, NTJ, TTH, LLZ, SHZ and SKL all helped to acquire the data. All authors have read and approved the final manuscript.
Funding
This study was funded by the National Innovation and Entrepreneurship Training Program for college students of China (No. 201910367045), Key Projects of Natural Science Research in Colleges in Anhui Province, China (No. KJ2018A1005), Innovation and Entrepreneurship Training Program for college Students in Anhui Province, China (No. S202010367051).
Availability of data and materials
The datasets used and/or analysed during the current study were available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The protocol of this study was approved by the Medical Ethics Committee of Bengbu Medical College (project code 2019-062). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Before data collection, all participants read the consent information, and provided verbal informed consents by clicking "Continue" to take this online survey. The informed consent protocol was approved by the ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shunhua Zhang, Email: 0800076@bbmc.edu.cn.
Shengkai Liao, Email: lsk3166@163.com.
References
- 1.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 2.Bendo CB, Paiva SM, Varni JW, Vale MP. Oral health-related quality of life and traumatic dental injuries in Brazilian adolescents. Community Dent Oral Epidemiol. 2014;42(3):216–223. doi: 10.1111/cdoe.12078. [DOI] [PubMed] [Google Scholar]
- 3.Llanos AH, Silva CGB, Ichimura KT, Rebeis ES, Giudicissi M, Romano MM, Saraiva L. Impact of aggressive periodontitis and chronic periodontitis on oral health-related quality of life. Braz Oral Res. 2018;32:e006. doi: 10.1590/1807-3107bor-2018.vol32.0006. [DOI] [PubMed] [Google Scholar]
- 4.Jaeken K, Cadenas de Llano Perula M, Lemiere J, Verdonck A, Fieuws S, Willems G. Reported changes in oral health-related quality of life in children and adolescents before, during, and after orthodontic treatment: a longitudinal study. Eur J Orthod. 2019;41(2):125–132. doi: 10.1093/ejo/cjy035. [DOI] [PubMed] [Google Scholar]
- 5.Mohamed S, Vettore MV. Oral clinical status and oral health-related quality of life: is socioeconomic position a mediator or a moderator? Int Dent J. 2019;69(2):119–129. doi: 10.1111/idj.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. 2011;90(11):1264–1270. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.da Fonseca RCL, Antunes JLF, Cascaes AM, Bomfim RA. Analysis of the combined risk of oral problems in the oral health-related quality of life of Brazilian adolescents: multilevel approach. Clin Oral Investig. 2020;24(2):857–866. doi: 10.1007/s00784-019-02976-z. [DOI] [PubMed] [Google Scholar]
- 8.Krisdapong S, Sheiham A, Tsakos G. Impacts of recurrent aphthous stomatitis on quality of life of 12- and 15-year-old Thai children. Qual Life Res. 2012;21(1):71–76. doi: 10.1007/s11136-011-9925-4. [DOI] [PubMed] [Google Scholar]
- 9.Rebelo MA, Cardoso EM, Robinson PG, Vettore MV. Demographics, social position, dental status and oral health-related quality of life in community-dwelling older adults. Qual Life Res. 2016;25(7):1735–1742. doi: 10.1007/s11136-015-1209-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wei CN, Harada K, Ueda K, Fukumoto K, Minamoto K, Ueda A. Assessment of health-promoting lifestyle profile in Japanese university students. Environ Health Prev Med. 2012;17(3):222–227. doi: 10.1007/s12199-011-0244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kojima A, Ekuni D, Mizutani S, Furuta M, Irie K, Azuma T, Tomofuji T, Iwasaki Y, Morita M. Relationships between self-rated oral health, subjective symptoms, oral health behavior and clinical conditions in Japanese university students: a cross-sectional survey at Okayama University. BMC Oral Health. 2013;13:62. doi: 10.1186/1472-6831-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vazquez Fde L, Cortellazzi KL, Kaieda AK, Guerra LM, Ambrosano GM, Tagliaferro EP, Mialhe FL, Meneghim Mde C, Pereira AC. Quality of life and socio-dental impact among underprivileged Brazilian adolescents. Qual Life Res. 2015;24(3):661–669. doi: 10.1007/s11136-014-0795-4. [DOI] [PubMed] [Google Scholar]
- 13.Krisdapong S, Prasertsom P, Rattanarangsima K, Sheiham A. Sociodemographic differences in oral health-related quality of life related to dental caries in thai school children. Community Dent Health. 2013;30(2):112–118. [PubMed] [Google Scholar]
- 14.Broadbent JM, Zeng J, Foster Page LA, Baker SR, Ramrakha S, Thomson WM. Oral health-related beliefs, behaviors, and outcomes through the life course. J Dent Res. 2016;95(7):808–813. doi: 10.1177/0022034516634663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pulache J, Abanto J, Oliveira LB, Bonecker M, Porras JC. Exploring the association between oral health problems and oral health-related quality of life in Peruvian 11- to 14-year-old children. Int J Paediatr Dent. 2016;26(2):81–90. doi: 10.1111/ipd.12160. [DOI] [PubMed] [Google Scholar]
- 16.Yamane-Takeuchi M, Ekuni D, Mizutani S, Kataoka K, Taniguchi-Tabata A, Azuma T, Furuta M, Tomofuji T, Iwasaki Y, Morita M. Associations among oral health-related quality of life, subjective symptoms, clinical status, and self-rated oral health in Japanese university students: a cross-sectional study. BMC Oral Health. 2016;16(1):127. doi: 10.1186/s12903-016-0322-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chew T, Brennan D, Rossi-Fedele G: Comparative Longitudinal Study on the Impact Root Canal Treatment and Other Dental Services Have on Oral Health-related Quality of Life Using Self-reported Health Measures (Oral Health Impact Profile-14 and Global Health Measures). J Endod 2019, 45(8):985–993 e981. [DOI] [PubMed]
- 18.Eriksson I, Unden AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30(2):326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- 19.Pattussi MP, Olinto MT, Hardy R, Sheiham A. Clinical, social and psychosocial factors associated with self-rated oral health in Brazilian adolescents. Community Dent Oral Epidemiol. 2007;35(5):377–386. doi: 10.1111/j.1600-0528.2006.00339.x. [DOI] [PubMed] [Google Scholar]
- 20.Astrom AN, Mashoto K. Determinants of self-rated oral health status among school children in northern Tanzania. Int J Paediatr Dent. 2002;12(2):90–100. doi: 10.1046/j.1365-263X.2002.00341.x. [DOI] [PubMed] [Google Scholar]
- 21.Ueno M, Zaitsu T, Ohara S, Wright C, Kawaguchi Y. Factors influencing perceived oral health of Japanese middle-aged adults. Asia Pac J Public Health. 2015;27(2):NP2296–NP2304. doi: 10.1177/1010539511428352. [DOI] [PubMed] [Google Scholar]
- 22.Bettinghaus EP. Health promotion and the knowledge-attitude-behavior continuum. Prev Med. 1986;15(5):475–491. doi: 10.1016/0091-7435(86)90025-3. [DOI] [PubMed] [Google Scholar]
- 23.Zhao Q, Wang SB, Xu G, Song Y, Han X, Liu Z, Zhou X, Zhang T, Huang K, Yang T, et al. Periodontal health: A national cross-sectional study of knowledge, attitudes and practices for the public oral health strategy in China. J Clin Periodontol. 2019;46(4):406–419. doi: 10.1111/jcpe.13082. [DOI] [PubMed] [Google Scholar]
- 24.Blaggana A, Grover V, Anjali, Kapoor A, Blaggana V, Tanwar R, Kaur H, Haneet RK. Oral health knowledge, attitudes and practice behaviour among secondary school children in Chandigarh. J Clin Diagn Res. 2016;10(10):1101–1106. doi: 10.7860/JCDR/2016/23640.8633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shubayr MA, Alexander LR, Tabatabai MA, Alagili DE. Knowledge, Attitude and practice of oral health promotion among oral health providers in Kingdom of Saudi Arabia. J Contemp Dent Pract. 2019;20(2):231–238. doi: 10.5005/jp-journals-10024-2503. [DOI] [PubMed] [Google Scholar]
- 26.Smyth E, Caamano F, Fernandez-Riveiro P. Oral health knowledge, attitudes and practice in 12-year-old schoolchildren. Med Oral Patol Oral Cir Bucal. 2007;12(8):E614–620. [PubMed] [Google Scholar]
- 27.Yang TZ, Ruan HJ, Li FZ. The application of structural equation modeling approach in epidemiological research. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26(4):297–300. [PubMed] [Google Scholar]
- 28.Abid A, Jie S, Aslam W, Batool S, Lili Y. Application of structural equation modeling to develop a conceptual model for smallholder's credit access: the mediation of agility and innovativeness in organic food value chain finance. PLoS ONE. 2020;15(8):e0235921. doi: 10.1371/journal.pone.0235921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheung MW. Some reflections on combining meta-analysis and structural equation modeling. Res Synth Methods. 2019;10(1):15–22. doi: 10.1002/jrsm.1321. [DOI] [PubMed] [Google Scholar]
- 30.Tarka P. An overview of structural equation modeling: its beginnings, historical development, usefulness and controversies in the social sciences. Qual Quant. 2018;52(1):313–354. doi: 10.1007/s11135-017-0469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tomarken AJ, Waller NG. Structural equation modeling: strengths, limitations, and misconceptions. Annu Rev Clin Psychol. 2005;1:31–65. doi: 10.1146/annurev.clinpsy.1.102803.144239. [DOI] [PubMed] [Google Scholar]
- 32.Kwok OM, Cheung MWL, Jak S, Ryu E, Wu JY. Editorial: recent advancements in structural equation modeling (SEM): from both methodological and application perspectives. Front Psychol. 1936;2018:9. doi: 10.3389/fpsyg.2018.01936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. Geneva: World Health Organization (WHO); 1991. [Google Scholar]
- 34.Record of the Press Conference on the results obtained from the 4th national oral health epidemiology survey. National Health Commission of the People’s Republic of China. 2017. http://www.gov.cn/xinwen/2017-09/20/content_5226224.htm. Accessed 20 Sept 2017.
- 35.Xin WN, Ling JQ. Validation of a Chinese version of the oral health impact profile-14. Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41(4):242–245. [PubMed] [Google Scholar]
- 36.Sanders AE, Slade GD, Lim S, Reisine ST. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol. 2009;37(2):171–181. doi: 10.1111/j.1600-0528.2008.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11(1):3–11. [PubMed] [Google Scholar]
- 38.Locker D, Allen PF. Developing short-form measures of oral health-related quality of life. J Public Health Dent. 2002;62(1):13–20. doi: 10.1111/j.1752-7325.2002.tb03415.x. [DOI] [PubMed] [Google Scholar]
- 39.Locker D. Measuring oral health: a conceptual framework. Community Dent Health. 1988;5(1):3–18. [PubMed] [Google Scholar]
- 40.Brennan DS, Teusner DN. Oral health impacts on self-rated general and oral health in a cross-sectional study of working age adults. Community Dent Oral Epidemiol. 2015;43(3):282–288. doi: 10.1111/cdoe.12152. [DOI] [PubMed] [Google Scholar]
- 41.Brennan DS, Anikeeva O, Teusner D. Dental visiting by insurance and oral health impact. Aust Dent J. 2013;58(3):344–349. doi: 10.1111/adj.12082. [DOI] [PubMed] [Google Scholar]
- 42.Brennan DS, Singh KA. General health and oral health self-ratings, and impact of oral problems among older adults. Eur J Oral Sci. 2011;119(6):469–473. doi: 10.1111/j.1600-0722.2011.00873.x. [DOI] [PubMed] [Google Scholar]
- 43.Ho AD, Yu CC. Descriptive statistics for modern test score distributions: skewness, kurtosis, discreteness, and ceiling effects. Educ Psychol Meas. 2015;75(3):365–388. doi: 10.1177/0013164414548576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7(4):422–445. doi: 10.1037/1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- 45.Wen ZLYB. Mediating effect analysis: method and model development. J Adv Psychol Sci. 2014;22:731–745. doi: 10.3724/SP.J.1042.2014.00731. [DOI] [Google Scholar]
- 46.Vansteelandt S, Daniel RM. Interventional effects for mediation analysis with multiple mediators. Epidemiology. 2017;28(2):258–265. doi: 10.1097/EDE.0000000000000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim SJ, Kim HY, Park YA, Kim SH, Yoo SY, Lee JE, Moon SY. Factors influencing fatigue among mothers with hospitalized children: a structural equation model. J Spec Pediatr Nurs. 2017;22(1):e12171. doi: 10.1111/jspn.12171. [DOI] [PubMed] [Google Scholar]
- 48.Elyasi M, Lai H, Major PW, Baker SR, Amin M. Modeling the Theory of Planned Behaviour to predict adherence to preventive dental visits in preschool children. PLoS ONE. 2020;15(1):e0227233. doi: 10.1371/journal.pone.0227233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Charter RA. Sample size requirements for precise estimates of reliability, generalizability, and validity coefficients. J Clin Exp Neuropsychol. 1999;21(4):559–566. doi: 10.1076/jcen.21.4.559.889. [DOI] [PubMed] [Google Scholar]
- 50.Yuan L, Wang DF, Lew B, Osman A, Jia CX. The future disposition Inventory-24: reliability and validity estimates in a large sample of Chinese University students. BMC Psychiatry. 2018;18(1):299. doi: 10.1186/s12888-018-1875-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Al-Wesabi AA, Abdelgawad F, Sasahara H, El Motayam K. Oral health knowledge, attitude and behaviour of dental students in a private university. BDJ Open. 2019;5:16. doi: 10.1038/s41405-019-0024-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Badovinac A, Bozic D, Vucinac I, Vesligaj J, Vrazic D, Plancak D. Oral health attitudes and behavior of dental students at the University of Zagreb, Croatia. J Dent Educ. 2013;77(9):1171–1178. doi: 10.1002/j.0022-0337.2013.77.9.tb05589.x. [DOI] [PubMed] [Google Scholar]
- 53.Liu WYHJ, Chen QY, et al. Analysis on the current situation and influencing factors of oral hygiene behavior of college students in Baotou. J Chin J Sch Health. 2017;38:1715–1717. [Google Scholar]
- 54.Chen FHB, Liu MY, et al. Investigation and analysis on oral health status and practice for college students in Fuzhou. J Chin J Sch Health. 2015;36:31–33. [Google Scholar]
- 55.Abu-Gharbieh E, Saddik B, El-Faramawi M, Hamidi S, Basheti M, Basheti M. Oral health knowledge and behavior among adults in the United Arab Emirates. Biomed Res Int. 2019;2019:7568679. doi: 10.1155/2019/7568679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oge OA, Douglas GVA, Seymour D, Adams C, Csikar J. Knowledge, attitude and practice among Health Visitors in the United Kingdom toward children's oral health. Public Health Nurs. 2018;35(1):70–77. doi: 10.1111/phn.12381. [DOI] [PubMed] [Google Scholar]
- 57.Cleary A, Dowling M. Knowledge and attitudes of mental health professionals in Ireland to the concept of recovery in mental health: a questionnaire survey. J Psychiatr Ment Health Nurs. 2009;16(6):539–545. doi: 10.1111/j.1365-2850.2009.01411.x. [DOI] [PubMed] [Google Scholar]
- 58.Peng Z, Yang F, Sun ZQ, Li MZ. Status on knowledge, attitudes, behavior regarding nutrition and food safety among 4–6 grade students from Chinas' two poverty-stricken counties. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34(7):673–676. [PubMed] [Google Scholar]
- 59.Li HW, Huang CH, Chou C, Wang TF. Knowledge, attitudes, practice and related factors of oral cancer prevention among public health nurses in Taiwan. Eur J Cancer Care (Engl) 2020;29(5):e13262. doi: 10.1111/ecc.13262. [DOI] [PubMed] [Google Scholar]
- 60.Caglar E, Bilgili N, Karaca A, Ayaz S, Asci FH. The psychological characteristics and health related behavior of adolescents: the possible of social physique anxiety and gender. Span J Psychol. 2010;13(2):741–750. doi: 10.1017/S1138741600002407. [DOI] [PubMed] [Google Scholar]
- 61.Lajunen T, Rasanen M. Can social psychological models be used to promote bicycle helmet use among teenagers? A comparison of the Health Belief Model, Theory of Planned Behavior and the Locus of Control. J Safety Res. 2004;35(1):115–123. doi: 10.1016/j.jsr.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 62.Hajj A, Hallit S, Azzo C, Abdou F, Akel M, Sacre H, Salameh P, Rabbaa Khabbaz L. Assessment of knowledge, attitude and practice among community pharmacists towards dental care: A national cross sectional survey. Saudi Pharm J. 2019;27(4):475–483. doi: 10.1016/j.jsps.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Faden AA, Alsalhani AB, Idrees MM, Alshehri MA, Nassani MZ, Kujan OB. Knowledge, attitudes, and practice behavior of dental hygienists regarding the impact of systemic diseases on oral health. Saudi Med J. 2018;39(11):1139–1147. doi: 10.15537/smj.2018.11.23267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Priyadarshini SR, Sahoo PK, Jena D, Panigrahi R, Patnaik S, Mohapatra A. Knowledge, attitude and practice of dental professionals towards substance use. J Int Soc Prev Community Dent. 2019;9(1):65–71. doi: 10.4103/jispcd.JISPCD_246_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alsumait A, ElSalhy M, Almunezaa E, Ariga J, Al-Mutawa S, Amin M. Relationship between oral health knowledge, attitude and practices of primary school teachers and their oral health-related quality of life: a cross-sectional study. Oral Health Prev Dent. 2016;14(6):519–528. doi: 10.3290/j.ohpd.a37137. [DOI] [PubMed] [Google Scholar]
- 66.Yoon HS, Kim HY, Patton LL, Chun JH, Bae KH, Lee MO. Happiness, subjective and objective oral health status, and oral health behaviors among Korean elders. Community Dent Oral Epidemiol. 2013;41(5):459–465. doi: 10.1111/cdoe.12041. [DOI] [PubMed] [Google Scholar]
- 67.Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rosing CK. Association between gingival bleeding and gingival enlargement and oral health-related quality of life (OHRQoL) of subjects under fixed orthodontic treatment: a cross-sectional study. BMC Oral Health. 2012;12:53. doi: 10.1186/1472-6831-12-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Montero J, Albaladejo A, Zalba JI. Influence of the usual motivation for dental attendance on dental status and oral health-related quality of life. Med Oral Patol Oral Cir Bucal. 2014;19(3):e225–231. doi: 10.4317/medoral.19366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Saho H, Ekuni D, Kataoka K, Taniguchi-Tabata A, Toyama N, Sugiura Y, Islam MM, Iwasaki Y, Morita M. Structural equation modeling to detect predictors of oral health-related quality of life among Japanese university students: a prospective cohort study. Qual Life Res. 2019;28(12):3213–3224. doi: 10.1007/s11136-019-02251-4. [DOI] [PubMed] [Google Scholar]
- 70.Tolvanen M, Lahti S, Miettunen J, Hausen H. Relationship between oral health-related knowledge, attitudes and behavior among 15–16-year-old adolescents: a structural equation modeling approach. Acta Odontol Scand. 2012;70(2):169–176. doi: 10.3109/00016357.2011.600722. [DOI] [PubMed] [Google Scholar]
- 71.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65. doi: 10.1001/jama.1995.03520250075037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study were available from the corresponding author on reasonable request.