Abstract
Prior research on health information exchange (HIE) typically measured provider usage through surveys or they summarized the availability of HIE services in a healthcare organization. Few studies utilized user log files. Using HIE access log files, we measured HIE use in real-world clinical settings over a 7-year period (2011-2017). Use of HIE increased in inpatient, outpatient, and emergency department (ED) settings. Further, while extant literature has generally viewed the ED as the most relevant setting for HIE, the greatest change in HIE use was observed in the inpatient setting, followed by the ED setting and then the outpatient setting. Our findings suggest that in addition to federal incentives, the implementation of features that address barriers to access (eg, Single Sign On), as well as value-added services (eg, interoperability with external data sources), may be related to the growth in user-initiated HIE.
Keywords: Health information exchange, interoperability, log-file analysis, HIE usage
INTRODUCTION
In 2009, the Health Information Technology for Economic and Clinical Health Act passed with the goal of facilitating the adoption of health information technology (HIT) across the United States. A specific application of HIT, health information exchange (HIE), involves the electronic sharing of clinical or administrative health data across the boundaries of healthcare facilities, health data repositories, and states.1 Widespread HIE has the potential to improve healthcare outcomes, boost efficiencies, and reduce costs of care.2 More recently, HIE has been touted as critical for the success of several healthcare reform strategies such as value-based and accountable care, patient-centered medical homes,3,4 as well as the Hospital Readmission Reduction Program.5 The federal government has thus far invested in excess of $500 million6 to develop infrastructure for data exchange with specific states,7 making additional investments of public and private funds to develop HIE capacity. Consequently, there has been a growth in HIE efforts across the United States, with about 96% of nonfederal acute care hospitals having the ability to engage in electronic exchange of clinical information by 2016.8
Current understanding of the growth in HIE comes primarily from analyses of self-reported data which measure the ability of hospitals to engage in HIE rather than actual use of HIE during clinical encounters. Most studies examine organizational adoption of HIE services, such as the ability to send an electronic summary of a clinical encounter to the next care provider—a specific criterion called for in the meaningful use incentive program.9 Data on the adoption rates of HIE services come from the IT supplement of the American Hospital Association survey, which is self-reported data provided by managers in hospitals across the United States. Adoption of HIE is inferred from specific questions that either explicitly or implicitly evaluate a hospital’s ability to engage in HIE, by measuring the adoption of certified electronic health records (EHRs). Further, while valuable for examining the proportion of hospitals with capabilities to exchange health information, there is no quantification of HIE as a proportion of all clinical encounters. While some studies in the extant literature leveraged log files to measure actual HIE usage, these studies principally examined HIE use within a single setting or system as well as HIE usage over relatively short durations of time.10–22 Additionally, these studies generally focused on examining the correlation between HIE access and specific healthcare outcomes, not on trends in HIE use over time.
The purpose of this descriptive analysis is to examine actual use of health information sharing by investigating user-initiated HIE during clinical encounters. Specifically, we use access log files from a large community HIE network involving multiple health systems in a moderate-sized state to measure the volume of user-initiated HIE usage over time. Further, we also examine the differences in user-initiated HIE in clinical encounters by factors such as care setting, payer type, and whether the HIE participating healthcare organization was located in an urban or rural area. By examining HIE usage using objective measures, across multiple health systems and settings, in a statewide community HIE over a 7-year time frame, we aim to contribute to the understanding of HIE use. Findings from our analysis provide insights into actual HIE within clinical encounters as well as potential factors that may be related to HIE use.
MATERIALS AND METHODS
We utilized access log files from the Indiana Network for Patient Care (INPC), a mature statewide community HIE network.23 The INPC connects 117 hospitals representing 38 hospital systems, over 17 000 practices, and over 48 000 providers, and contains data on roughly 15 million patients with a total of more than 12.5 billion data points.24 The INPC is also representative of the state’s population, with data on 80%-100% of all patients in a majority of counties in Indiana during the study period (2011-2017) (Supplementary Figure 1).
Access log files represent an objective method to measure HIE usage. The INPC makes a record every time a user (ie, clinical or nonclinical staff) logs in to view clinical information. Typically, users click a button within their EHR system, which automatically logs them into the INPC’s CareWeb application (Supplementary Figure 2) to examine a patient’s historical record of care from multiple providers. Therefore, access log files represent actual data exchange at the clinical encounter level due to provider use of “outside records,” rather than just the ability to engage in HIE at the organizational (eg, hospital, clinic) level.
In order to add more information regarding the encounter such as care setting, payer, provider role, and rurality of the hospital, the access log files were linked to encounter-level clinical data using unique IDs assigned to each encounter. When patients used more than 1 payer to pay for services received during a single encounter, only the payer that paid for majority of encounter’s cost (ie, priority payer) was retained.
RESULTS
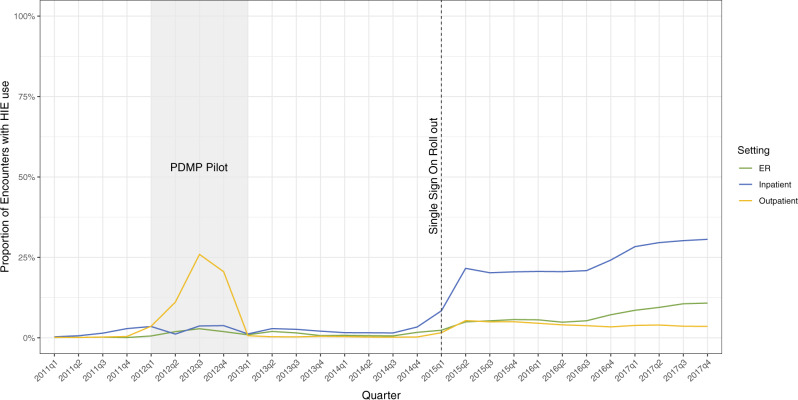
We examined a total of 1 159 144 inpatient, 14 932 164 outpatient, and 3 006 972 ED encounters between 2011 and 2017 from the INPC. Of the encounters examined, 15.5% took place in rural settings. Overall, 4.7% of all encounters across all settings resulted in the user accessing external patient information. Further, HIE use was greatest in the inpatient setting (17.6%), followed by the ED (4.4%) and the outpatient (3.7%) settings (Figure 1). HIE use increased by 29%, 3.5%, and 9% in the inpatient, outpatient, and ED settings, respectively.
Figure 1.
Trends in proportion of encounters in each quarter in which health information exchange (HIE) data were accessed in the emergency department, inpatient, and outpatient care settings. Source: Indiana Network for Patient Care log files, 2011-2017. ER: emergency room; PDMP: prescription drug monitoring program.
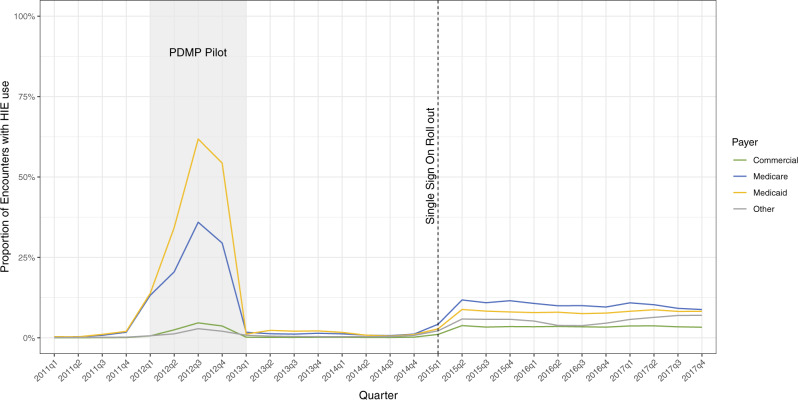
Commercial insurance constituted the largest known payer category (ie, not “Other”), with over 6 million encounters accounting for this payer type. This was followed by Medicaid (2 564 555 encounters) and Medicare (2 344 584 encounters). Payers categorized as “Other” in the log files accounted for about 7.8 million encounters. There was a significant increase in HIE use in each payer type between 2011 and 2017 (Figure 2). Further, HIE use was greatest for encounters in which Medicare (8.8%) or Medicaid (8.2%) was identified as a priority payer. Encounters in which the payer was commercial insurance (3.3%) had the least HIE use among all 4 payer types.
Figure 2.
Trends in the proportion of all encounters with health information exchange (HIE) use by payer type. Source: Indiana Network for Patient Care log files, 2011-2017. PDMP: prescription drug monitoring program.
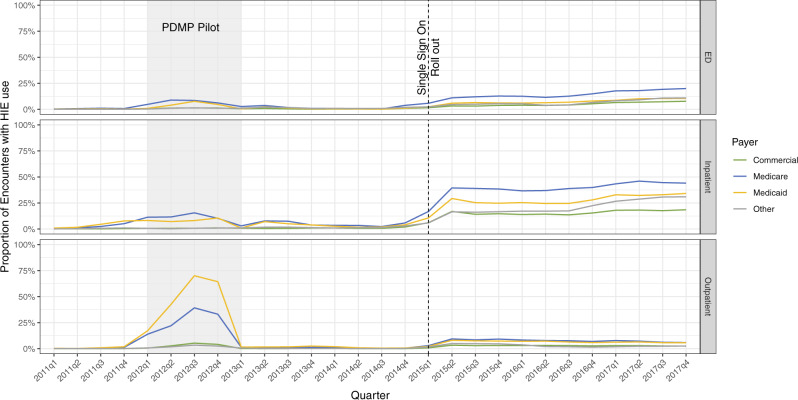
Similar trends of increasing use of HIE in encounters by payer type were also seen in each of the 3 settings examined (Figure 3). The least change was observed in the outpatient setting, in which average HIE use across all payer types, although significant, increased by 4%, compared with an increase of 31.5% and12.1% in the inpatient and ED settings, respectively. HIE use was greatest when Medicare was at least 1 of the payer types for a given encounter in all 3 care settings approaching 44.1%, 6%, and 20% in the inpatient, outpatient, and ED settings, respectively, by the fourth quarter of 2017.
Figure 3.
Trends in the proportion of all encounters with health information exchange (HIE) use by care setting and payer type. Source: Indiana Network for Patient Care log files, 2011-2017. ED: emergency department; PDMP: prescription drug monitoring program.
We next examined HIE usage by the rurality of the healthcare organization. In both rural and urban environments, HIE use increased over time. Furthermore, usage was highest in urban inpatient setting, followed by ED and outpatient settings (Supplementary Figure 3). By the fourth quarter of 2017, HIE use in urban inpatient setting had increased by 32.5%, compared with 12% and 4% in similar ED and outpatient settings, respectively.
Overall, HIE use increased between 2011 and 2017 based on care setting, rurality, and payer type (Figures 1–3 and Supplementary Figure 3). Further, the data also suggest 2 sharp increases in HIE use at 2 time points: once in the first quarter of 2012 and again in the fourth quarter of 2014. The increase in HIE use in 2012 was predominantly observed in the outpatient setting for encounters with either Medicare or Medicaid as the payer. However, this increase in HIE use returned to normal trends by first quarter of 2013. The upward trend in HIE use observed in first quarter of 2015 was most prominent in the inpatient setting, seen across all payer types and showed a steady increase through fourth quarter of 2017.
DISCUSSION
Since 2009, the federal government has invested in several initiatives with the goal of increasing interoperability among health information systems. A key finding from our analysis of access log files was that HIE use in clinical encounters increased in Indiana between 2011 and 2017. While this finding remains true for all settings, the greatest increase was seen in the inpatient setting, followed by the ED and the outpatient settings. Further, HIE use and increases over time were greater in clinical encounters in urban locations, as well as in those in which at least 1 payer was either Medicaid or Medicare. Finally, HIE use saw a dramatic increase in 2012 before returning to normal in 2013, followed by another steady increase starting late 2014, which continued through 2017.
These findings are potentially attributable to several plausible causes. First, HIE adoption increased over time, owing to the success of federal incentives and programs. As such, adoption of HIE capability by hospitals and clinics through participation in the INPC resulted in greater abundance of healthcare organizations that could exchange data. Therefore, data exchange with the INPC became more valuable over time due to increasing availability of patient data from more sources. Providers responded by using the system to access clinical data more often.
A related, but distinct, cause might have been the emphasis in the Health Information Technology for Economic and Clinical Health Act on the Centers for Medicare and Medicaid Services (CMS) financial incentives for HIE use. Greater HIE use for Medicare and Medicaid populations may be due to provider awareness regarding CMS-provided incentives to hospitals and clinics for the adoption and meaningful use of HIE. However, it is equally likely that providers use the HIE for Medicare and Medicaid populations, because these populations often possess higher acuity or more complex medical needs. This may be especially true for Medicare populations who may be sicker and have more comorbidities than younger patients.25 Providers may take additional steps to find a comprehensive and more complete medical history for individuals who are admitted with a complex set of comorbidities.
Some changes in HIE use may also be related to incremental functional and user experience–related changes over time. According to the Indiana HIE, enhancements to CareWeb occurred independently with each health system therefore it is likely that any changes in HIE use due to enhancements were subsumed by the overall trend.26 On the other hand, the sharp increase in HIE use in 2012 was likely due to a pilot interoperability program implemented in a large safety net hospital in Indianapolis. In this program, data from the state prescription drug monitoring program (PDMP) were integrated with the INPC, and providers were encouraged to use the HIE network to access prescription drug histories.26 Further, prescription history was automatically extracted from the PDMP at registration for all patients in all care settings. This pilot was terminated at the end of 2012, coinciding with the HIE use trends returning to normal, further supporting the role of this program in causing the increase.
In late 2014, the INPC introduced a “single sign-on” (SSO) feature, making it easier for providers to access “outside information” on patients. Instead of opening a web browser, navigating to the HIE site, logging into the INPC, and looking up the patient using information such as a name and birthdate, the SSO functionality allows providers to click on a button within their EHR system and automatically login to the INPC to view medical records for the patient. This increased ease of use may likely be the reason for the steady rise in INPC use starting in late 2014, which continued through 2017. Further, SSO was incrementally rolled out to hospitals, thus accounting for bumps in HIE use seen later in 2016 and 2017 as more hospitals adopted this feature.26
Future research may focus on additional value-added features that promote HIE usage. For instance, HIE use may be facilitated by using the latest data sharing standards such as Fast Healthcare Interoperability Resources to automatically retrieve relevant clinical data.27 However, we note that the use of Fast Healthcare Interoperability Resources and other approaches to integrate data across clinical systems may make measuring HIE use more difficult, as it may become harder to distinguish end user interaction with HIE services from tools embedded directly in the EHR.
Limitations
While the access log files permitted the distinction between clinical encounters that did and did not access external data from the HIE, it was not possible to determine the type of patient information that was viewed. Further, our data are limited to Indiana, which may be different from other states owing to its mature HIE.
Conclusions
Our analysis found that HIE use increased over time in all care settings. Further, this increase was greatest for encounters in urban locations and those paid for by CMS. These increases might be due to the federal incentives for meaningful use of HIT systems. However, in agreement with the adage of former Agency for Healthcare Research and Quality Director Carolyn Clancey, “making the right thing to do, the easy thing to do”; the dramatic increase in HIE use following the introduction of SSO suggests that features making HIE access easier may be a stronger influence on provider behavior.
Further, as log files are increasingly being recognized as a “new source of insights, which cannot be gleaned from claims data or clinical data,”28 our analysis capitalizes on the objective nature of this data to present trends in user-initiated HIE over a 7-year period. Future research should examine the effect of increase in HIE use on healthcare outcomes, including that of interoperability interventions like the PDMP pilot that occurred in 2012. Evidence from our analysis and future studies could help inform policymakers on how to strategically leverage interoperability policy, as well as interventions, to improve healthcare outcomes and quality of care.
FUNDING
This work was supported by Agency for Healthcare Research and Quality Grant No. R21HS025502. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. This research was supported in part by Lilly Endowment, through its support for the Indiana University Pervasive Technology Institute. This material is based on work supported by the National Science Foundation under Grant No. CNS-0521433.
AUTHOR CONTRIBUTIONS
SR contributed to the conception, design, data acquisition, and interpretation, and drafted and critically revised the manuscript. JRV contributed to the conception, design, data acquisition, and interpretation, and critically revised the manuscript. JTF contributed to the design, data acquisition, and interpretation, and critically revised the manuscript. BED contributed to the conception, design, data acquisition, and interpretation, and drafted and critically revised the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Ashley Wiensch at the Regenstrief Institute and Will Tarver at the Ohio State University for their assistance in reviewing this manuscript. The authors acknowledge the Indiana University Pervasive Technology Institute for providing Carbonate and database storage resources that contributed to the research results reported within this article.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
REFERENCES
- 1. Dixon BE. What is health information exchange? In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. 1st ed. Waltham, MA: Academic Press; 2016: 3–20. [Google Scholar]
- 2. Menachemi N, Rahurkar S, Harle CA, Vest JR.. The benefits of health information exchange: an updated systematic review. J Am Med Inform Assoc 2018; 25 (9): 1259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Devore S, Champion RW.. Driving population health through accountable care organizations. Health Aff (Millwood) 2011; 30 (1): 41–50. [DOI] [PubMed] [Google Scholar]
- 4. Williams C, Mostashari F, Mertz K, Hogin E, Atwal P.. From the Office of the National Coordinator: the strategy for advancing the exchange of health information. Health Aff (Millwood) 2012; 31 (3): 527–36. [DOI] [PubMed] [Google Scholar]
- 5. Jackson CT, Trygstad TK, DeWalt DA, DuBard CA.. Transitional care cut hospital readmissions for North Carolina Medicaid patients with complex chronic conditions. Health Aff (Millwood) 2013; 32 (8): 1407–15. [DOI] [PubMed] [Google Scholar]
- 6. Thune J, Alexander L, Roberts P, Burr R, Coburn T, Enzi M. REBOOT: Re-examining the Strategies Needed to Successfully Adopt Health IT. White Paper, U.S. Senate. 2013. https://www.amia.org/sites/default/files/files_2/EHR-White-Paper.pdf Accessed May 24, 2020.
- 7. Vest J, Martin E.. Creating a 21st century health information technology infrastructure: New York’s Health Care Efficiency and Affordability Law for New Yorkers Capital Grant Program. In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. 1st ed. Waltham, MA: Academic Press: 2016: 295–312. [Google Scholar]
- 8. Henry J, Pylypchuk Y, Searcy T, Patel V. Adoption of Electronic Health Record Systems among U.S. Non-Federal Acute Care Hospitals: 2008-2015. ONC Data Brief, no.35. Washington, DC: Office of the National Coordinator for Health Information Technology; 2016.
- 9. Cross DA, Cohen GR, Nong P, et al. Improving EHR capabilities to facilitate stage 3 meaningful use care coordination criteria. AMIA Annu Symp Proc 2015; 2015: 448–55. [PMC free article] [PubMed] [Google Scholar]
- 10. Boockvar KS, Ho W, Pruskowski J, et al. Effect of health information exchange on recognition of medication discrepancies is interrupted when data charges are introduced: results of a cluster-randomized controlled trial. J Am Med Inform Assoc 2017; 24 (6): 1095–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cross DA, McCullough JS, Banaszak-Holl J, Adler-Milstein J.. Health information exchange between hospital and skilled nursing facilities not associated with lower readmissions. Health Serv Res 2019; 54 (6): 1335–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Everson J, Kocher KE, Adler-Milstein J.. Health information exchange associated with improved emergency department care through faster accessing of patient information from outside organizations. J Am Med Inform Assoc 2017; 24 (e1): e103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jung HY, Vest JR, Unruh MA, Kern LM, Kaushal R, Investigators H.. Use of health information exchange and repeat imaging costs. J Am Coll Radiol 2015; 12 (12 Pt B): 1364–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Politi L, Codish S, Sagy I, Fink L.. Use patterns of health information exchange systems and admission decisions: reductionistic and configurational approaches. Int J Med Inform 2015; 84 (12): 1029–38. [DOI] [PubMed] [Google Scholar]
- 15. Politi L, Codish S, Sagy I, Fink L.. Balancing volume and duration of information consumption by physicians: the case of health information exchange in critical care. J Biomed Inform 2017; 71: 1–15. [DOI] [PubMed] [Google Scholar]
- 16. Shabtai I, Assuli OB, Leshno M.. The connection between viewing medical historical information and using-clinical tests. Int J Netw Virtual Organ 2016; 16 (2): 157–70 . [Google Scholar]
- 17. Stockwell MS, Natarajan K, Ramakrishnan R, et al. Immunization data exchange with electronic health records. Pediatrics 2016; 137 (6): 1–8. [DOI] [PubMed] [Google Scholar]
- 18. Vest JR, Hilts KE, Ancker JS, Unruh MA, Jung HY.. Usage of query-based health information exchange after event notifications. JAMIA Open 2019; 2 (3): 291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vest JR, Kaushal R, Silver MD, Hentel K, Kern LM.. Health information exchange and the frequency of repeat medical imaging. Am J Manag Care 2014; 20 (11 Spec No. 17): eSP16–24. [PubMed] [Google Scholar]
- 20. Vest JR, Kern LM, Silver MD, Kaushal R, Investigators H.. The potential for community-based health information exchange systems to reduce hospital readmissions. J Am Med Inform Assoc 2015; 22 (2): 435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yaraghi N. An empirical analysis of the financial benefits of health information exchange in emergency departments. J Am Med Inform Assoc 2015; 22 (6): 1169–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yaraghi N, Du AY, Sharman R, Gopal RD, Ramesh R.. Health Information exchange as a multisided platform: adoption, usage, and practice involvement in service co-production. Info Syst Res 2015; 26 (1): 1–18.[published Online First: Epub Date]|. [Google Scholar]
- 23. Overhage JM. The Indiana Health Information Exchange. In: Dixon BE, ed. Health Information Exchange: Navigating and Managing a Network of Health Information Systems. 1st ed.Waltham, MA: Academic Press, 2016: 267–79. [Google Scholar]
- 24.Indiana Health Information Exchange. 2019. https://go.osu.edu/ihie. Accessed May 24, 2020.
- 25.American Hospital Association. Are Medicare patients getting sicker? AHA TrendWatch. 2012. https://www.aha.org/system/files/2018-06/2012-are-medicare-pts-getting-sicker-trendwatch.pdf Accessed June 24, 2020.
- 26. Kelley K. Letter for Response to JAMIA Revisions. In: Dixon BE, ed.2020. [Google Scholar]
- 27. Schleyer TKL, Rahurkar S, Baublet AM, et al. Preliminary evaluation of the Chest Pain Dashboard, a FHIR-based approach for integrating health information exchange information directly into the clinical workflow. AMIA Jt Summits Transl Sci Proc 2019; 2019: 656–64. [PMC free article] [PubMed] [Google Scholar]
- 28. Adler-Milstein J, Adelman JS, Tai-Seale M, Patel VL, Dymek C.. EHR audit logs: a new goldmine for health services research? J Biomed Inform 2020; 101: 103343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.