Abstract
Background
The coronavirus disease 2019 (COVID-19) has affected all countries in the world. Hospital workers are at high risk of mental illness, such as anxiety and depression. Furthermore, they also face many social stresses, such as deterioration of human relations and income reduction. Apart from mental illness, these social stresses can reduce motivation and lead to voluntary absenteeism, which contribute to a collapse of medical systems. Thus, for maintaining medical systems, it is crucial to clarify risk factors for both mental illness and increased social stress among hospital workers. However, little attention has been paid to factors affecting social stress, and thus, we aimed to address this gap.
Methods
In this cross-sectional survey of 588 hospital workers, the levels of anxiety, depression, and social stress were assessed using the 7-item Generalized Anxiety Disorder scale (GAD-7), 9-item Patient Health Questionnaire (PHQ-9), and Tokyo Metropolitan Distress Scale for Pandemic (TMDP). Multiple regression analyses were conducted to identify the demographic variables affecting these problems.
Results
Older age and female sex were common risk factors for anxiety, depression, and social stress. Moreover, occupational exposure to COVID-19 and hospital staff other than doctors/fewer non-work days were risk factors for increased anxiety and depression, respectively. Furthermore, living with families/others was a risk factor for increased social stress during this pandemic.
Conclusion
Our findings could be useful for developing policies and practices to minimize the risk of mental illness and increased social stress among hospital workers, highlighting that attention should be paid to social factors, such as an individual's household situation.
Keywords: COVID-19, Risk factor, Mental illness, Voluntary absenteeism, Social stress
1. Introduction
The coronavirus disease 2019 (COVID-19) has affected all countries around the world, after the epidemic was confirmed in China in December 2019 (An et al., 2020; Rajkumar, 2020; Xiang et al., 2020). Since April 2020, Japan has also been severely affected by COVID-19 (Shigemura et al., 2020; Shiwaku et al., 2020; Ueda et al., 2020). Many general hospitals treated COVID-19 patients while limiting other medical services (Lai et al., 2020; Pappa et al., 2020; Shiwaku et al., 2020). The impact of the COVID-19 pandemic can be expected to last for a long time, thus ensuring the smooth functioning of medical systems is of the utmost importance (Chen et al., 2020; Lai et al., 2020; Liu et al., 2020; Pappa et al., 2020; Shanafelt et al., 2020; Shiwaku et al., 2020).
Hospital workers are at high risk of mental illness, such as increased anxiety and depressive symptoms (Chen et al., 2020; Lai et al., 2020; Liu et al., 2020; Pappa et al., 2020; Shanafelt et al., 2020; Shiwaku et al., 2020). In addition, hospital workers may also face many social stresses during the COVID-19 pandemic (An et al., 2020; Rajkumar, 2020; Shigemura et al., 2020; Shiwaku et al., 2020; Ueda et al., 2020; Xiang et al., 2020). For example, hospital workers might experience a downturn in human relations and a decline in income as a result of stigma and fear of contagion (Shiwaku et al., 2020; Xiang et al., 2020). Some hospital workers were encouraged by their families to quit their jobs, some of them were avoided by others owing to the nature of their work, and some of them were eventually prevented from working in multiple facilities, leading to financial issues (Shiwaku et al., 2020; Xiang et al., 2020).
These social stresses reduce motivation, which can result in voluntary absenteeism (Chen et al., 2020; Chong et al., 2004; Imai et al., 2010; Shiwaku et al., 2020; Tei et al, 2014, 2015; Valdez and Nichols, 2013; Xiang et al., 2020). Apart from mental illness, voluntary absenteeism can also contribute to a collapse of medical systems (Chen et al., 2020; Chong et al., 2004; Imai et al., 2010; Shiwaku et al., 2020; Tei et al, 2014, 2015; Valdez and Nichols, 2013; Xiang et al., 2020). To ensure the smooth functioning of medical systems, both mental illness and social stress among hospital workers need to be understood, and individuals who may be more vulnerable to these problems during the COVID-19 pandemic should be identified.
To date, a number of studies (Lai et al., 2020; Liu et al., 2020; Pappa et al., 2020) have examined mental illness among hospital workers during the COVID-19 pandemic using the scales of general anxiety and depression, such as the 7-item Generalized Anxiety Disorder scale (GAD-7; Spitzer et al., 2006) and the 9-item Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001). The studies revealed several risk factors, such as female sex and occupational exposure to COVID-19, for increased anxiety and depressive symptoms (Lai et al., 2020; Liu et al., 2020; Pappa et al., 2020). Yet, little attention has been paid to factors affecting social stresses, partially because the general anxiety and depression scales (e.g., GAD-7 and PHQ-9) do not include pandemic-specific elements (Kroenke et al., 2001; Spitzer et al., 2006).
To estimate social stress among hospital workers during the COVID-19 pandemic, we developed a novel scale, the Tokyo Metropolitan Distress Scale for Pandemic (TMDP; Shiwaku et al., 2020). The TMDP consists of nine items specifically for a pandemic, such as the risk of infection, anxiety concerning transmitting the virus to others, whether the work environment can control the infection, a deterioration of human relationships related to engaging in medical practice for the infection, and financial issues (Shiwaku et al., 2020). Our previous study confirmed that TMDP consists of two factors, concerns for infection and social stress during the COVID-19 pandemic, and that these factors can be easily and reliably assessed (Shiwaku et al., 2020).
In the present study, we investigated mental illness and social stress during the COVID-19 pandemic in hospital workers in Japan using GAD-7 (Spitzer et al., 2006), PHQ-9 (Kroenke et al., 2001), and TMDP (Shiwaku et al., 2020). Significant factors affecting these problems were examined using multiple regression analyses.
2. Methods
2.1. Ethics statement
The Institutional Ethics Committee of Tokyo Medical and Dental University approved this study, which was conducted in accordance with the Code of Ethics of the World Medical Association. Because this study was an observational retrospective study using anonymized data from the below-mentioned medical records, an opt-out procedure was used. The university's website provided information about the research in order to give participants the option to refuse participation in this study.
2.2. Study cohort
All samples were selected from staff members who work in the Tokyo Medical and Dental University Hospital and who received mental health assessments between April 20, 2020 and June 12, 2020 at the Department of Psychiatry in the same hospital. The assessments were conducted for the purpose of maintaining the mental health and wellbeing of staff members now and following the COVID-19 pandemic. Participants with incomplete responses to the variables necessary for the analysis were excluded. The samples partially overlapped with those included in our previous study (Shiwaku et al., 2020).
2.3. Data collection
The following variables were investigated as background characteristics: age, sex, job title [doctors, other medical staff (nurses, rehabilitation staff, technologists, and paramedics), or clerks/other staff], living conditions (living alone or with others), and non-work days (<2 days/week or ≥ 2 days/week). Additionally, we investigated the experience of occupational exposure to COVID-19 and being quarantined.
To assess the symptoms of anxiety and depression, GAD-7 (Spitzer et al., 2006) and PHQ-9 (Kroenke et al., 2001), which are well-validated tools, were used, respectively. High scores indicate high levels of depression and anxiety, respectively, in the two scales.
Furthermore, we also collected the data using the TMDP (Shiwaku et al., 2020). The TMDP is comprised of nine items specifically for a pandemic, such as the risk of infection, anxiety about transmitting virus to other individuals, whether the working environment can control infection, deterioration of human relationships related to engaging in medical practice for infection, and financial issues. Response options for all items were: “Never,” “Rarely,” “Occasionally,” “Often,” and “Most of the time,” scored as 0, 1, 2, 3, and 4, respectively. High scores indicate high levels of stressful conditions. Our previous study confirmed that the TMDP is composed of two factors: concerns for infection and social stress during the COVID-19 pandemic (Shiwaku et al., 2020).
2.4. Statistical analysis
Statistical analyses were performed using SPSS 24 (IBM Corp., Armonk, NY). Results were considered statistically significant at p < 0.05 (two-tailed). Correlation analysis was performed to verify the relationships between the levels of TMDP and those of GAD-7 and PHQ-9.
To explore potential risk factors for symptoms of anxiety and depression (i.e., GAD-7 and PHQ-9, respectively), we performed separate multiple logistic regression analyses based on previous studies (Lai et al., 2020; Pappa et al., 2020; Shiwaku et al., 2020). Factors including age, sex, job title (reference: doctors), living condition, non-work days, occupational exposure to COVID-19, and experience of being quarantined were included as independent variables in the backward elimination model. Probabilities of 0.05 and 0.10 were used as entry and removal criteria, respectively (SPSS's default values). Based on previous studies (Kroenke et al., 2001; Shiwaku et al., 2020; Spitzer et al., 2006), we adopted the cutoff for GAD-7 and PHQ-9 as 10 for both scales. A GAD-7 cutoff of 10 is regarded as moderate anxiety, and the sensitivity and specificity for anxiety disorder, as defined by the Diagnostic and Statistical Manual of Mental Disorders-IV-TR (DSM-IV-TR), are 89% and 82%, respectively (Spitzer et al., 2006). A PHQ-9 cutoff of 10 is also regarded as moderate depression, and the sensitivity and specificity for major depressive disorder, as defined by DSM-IV-TR, are 88% and 88%, respectively (Kroenke et al., 2001).
Multiple linear regression analysis (stepwise model) was used to examine significant factors associated with each of the TMDP total scores and the scores of two subscales (concerns for infection and social stress), because of the continuous nature of this scale (Shiwaku et al., 2020). As in the above-mentioned analyses, age, sex, job title, living condition, non-work days, occupational exposure to COVID-19, and experience of being quarantined were included as independent variables. The probabilities of 0.05 and 0.10 were used as entry and removal criteria, respectively (SPSS's default values).
3. Results
3.1. Demographic characteristics
In this study, 588 staff members [mean age: 35.4 ± 10.1 (S.D.) years, 291 (49.5%) females] of the Tokyo Medical and Dental University Hospital were analyzed. The characteristics of the participants are shown in Table 1 . Among the participants, 296 (50.3%) of them were doctors, 185 (31.5%) of them were other medical staff, and 107 (18.2%) of them were clerks or other staff members. Over 50% of the participants [343 (58.3%)] lived with families or others, and 21.6% (127) of the participants had experienced occupational exposure to COVID-19.
Table 1.
Demographic characteristics of the study cohort.
| Total (n = 588) | |
|---|---|
| Age, years: mean ± S.D. | 35.4 ± 10.1 |
| Sex: n (%) | |
| Male | 297 (50.5) |
| Female | 291 (49.5) |
| Job title: n (%) | |
| Doctor | 296 (50.3) |
| Other medical staff | 185 (31.5) |
| Clerk/Others | 107 (18.2) |
| Living condition: n (%) | |
| Living alone | 245 (41.7) |
| With family/others | 343 (58.3) |
| Non-work days: n (%) | |
| ≥2 days/week | 397 (67.5) |
| <2 days/week | 191 (32.5) |
| Occupational exposure: n (%) | |
| No/Not sure | 461 (78.4) |
| Yes | 127 (21.6) |
| Quarantined: n (%) | |
| No/No information | 555 (94.4) |
| Yes | 33 (5.6) |
3.2. Relationships between scores of TMDP and GAD-7/PHQ-9
The TMDP total scores and GAD-7 scores were significantly correlated (r = 0.57, p < 0.001). The TMDP total scores and PHQ-9 scores were also significantly correlated (r = 0.50, p < 0.001).
3.3. Risk factors detected by GAD-7 and PHQ-9
Among the 588 participants, 47 (8.0%) individuals reported GAD-7 scores of 10 or higher. Multiple logistic regression analysis (backward elimination model) showed that age, female sex, and experience of occupational exposure to COVID-19 were significant risk factors for anxiety (Table 2 ). Regarding depression, 40 (6.8%) individuals reported PHQ-9 scores of 10 or higher. Multiple logistic regression analysis (backward elimination model) showed that age, female sex, job title (other medical staff and clerk/others), and non-work days (<2) were significant risk factors for depression (Table 3 ). We confirmed that multiple logistic regression analyses (forced entry model) did not greatly change the results (Tables S1 and S2).
Table 2.
Results of logistic regression analysis of the 7-item Generalized Anxiety Disorder scale scores.
| B (SE) | Wald | p | Exp(B) | 95%CI | |
|---|---|---|---|---|---|
| Age | 0.06 (0.01) | 17.81 | <0.01 | 1.06 | 1.03–1.09 |
| Sex (female) | 1.59 (0.39) | 16.26 | <0.01 | 4.91 | 2.27–10.65 |
| Occupational exposure (yes) | 0.97 (0.36) | 7.30 | <0.01 | 2.63 | 1.30–5.30 |
Table 3.
Results of logistic regression analysis of the 9-item Patient Health Questionnaire scores.
| B (SE) | Wald | p | Exp(B) | 95%CI | |
|---|---|---|---|---|---|
| Non-work days (<2) | 1.27 (0.44) | 8.53 | <0.01 | 3.58 | 1.52–8.42 |
| Sex (female) | 1.18 (0.43) | 7.43 | <0.01 | 3.25 | 1.39–7.59 |
| Job title (clerk/others) | 1.46 (0.59) | 6.19 | 0.01 | 4.29 | 1.36–13.51 |
| Age | 0.04 (0.02) | 6.05 | 0.01 | 1.04 | 1.01–1.08 |
| Job title (other medical staff) | 1.28 (0.52) | 6.02 | 0.01 | 3.61 | 1.29–10.06 |
| Occupational exposure (yes) | 0.74 (0.41) | 3.25 | 0.07 | 2.09 | 0.94–4.64 |
3.4. Risk factors detected by TMDP
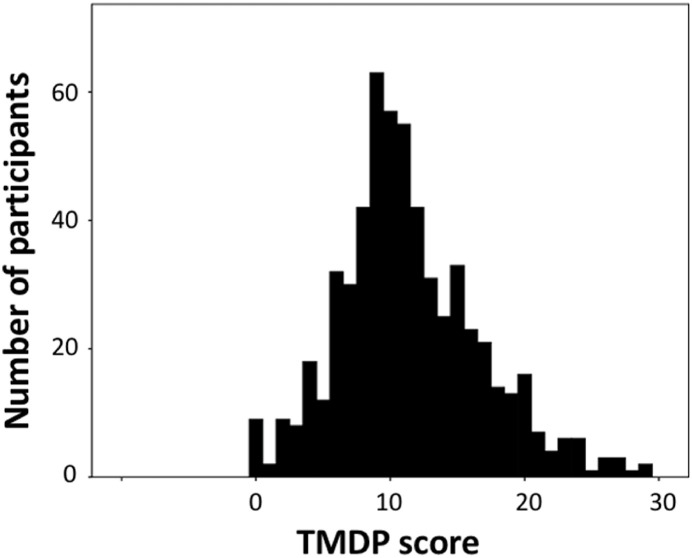
The mean TMDP score was 11.5 ± 5.3. Almost all [579 (98.5%)] the participants provided ratings higher than a score of 0. Fig. 1 shows the distribution of the scores. Multiple linear regression analysis (stepwise model) showed that age, female sex, and living with families or others were significant factors associated with TMDP scores (Table 4 ). Multiple linear regression analysis (forced entry model) did not greatly change the results (Table S3). In the multiple regression analysis conducted for the two subscales of TMDP (concerns regarding infection and social stress), significant factors associated with concerns for infection were female sex, job title (other medical staff), and living with families or others (Table S4); the significant factors associated with social stress were age, female sex, non-work days (<2), and living with families or others (Table S5).
Fig. 1.
Distribution of the Tokyo Metropolitan Distress Scale for Pandemic (TMDP) scores.
Table 4.
Results of linear regression analysis of the total scores of the Tokyo Metropolitan Distress Scale for Pandemic.
| Unstandardized Coefficient |
Standardized Coefficient |
||||
|---|---|---|---|---|---|
| B (SE) | β | t | p | 95%CI | |
| Sex (female) | 2.05 (0.42) | 0.19 | 4.88 | <0.01 | 1.23–2.88 |
| Living condition (with family/others) | 1.66 (0.47) | 0.16 | 3.51 | <0.01 | 0.73–2.59 |
| Age | 0.06 (0.02) | 0.11 | 2.55 | 0.01 | 0.01–0.10 |
4. Discussion
In this study, we investigated significant factors affecting mental illness and social stress during the COVID-19 pandemic in a relatively large number of hospital workers in Japan. Our findings could help develop policies and practices for maintaining mental health and preventing voluntary absenteeism of hospital workers during the COVID-19 pandemic.
Among 588 participants, 47 (8.0%) and 40 (6.8%) individuals showed moderate to severe anxiety and depressive symptoms, respectively. These prevalence rates, although they are lower than the prevalence rates of previous studies performed in China (Lai et al., 2020; Zhang et al., 2020), are comparable to the prevalence rates reported in Singapore (Tan et al., 2020). When considered in combination with the TMDP results of almost all [579 (98.5%)] the participants providing ratings with a score higher than 0, our findings emphasize the urgent need for psychological monitoring and support for hospital workers.
The levels of TMDP scores were significantly correlated with the levels of GAD-7 and PHQ-9 scores. The results indicate that TMDP can reliably assess depression and anxiety using pandemic-specific items, which is consistent with our previous study (Shiwaku et al., 2020).
Multiple regression analyses revealed that older age and female sex were common risk factors for all three scales (i.e., GAD-7, PHQ-9, and TMDP) during the COVID-19 pandemic. That is, older or female hospital workers are more vulnerable to both mental illness and social stress during the COVID-pandemic. Compared to younger adults, older adults are usually prone to experiencing physical discomforts and chronic physical diseases that could contribute to mental illness (Dai et al., 2013; Jeong et al., 2014; Lin et al., 2016; Zhou et al., 2020). With respect to female sex, several previous studies have also shown that female sex is a significant risk factor for mental illness in hospital workers during a pandemic, and the authors proposed that female sex as a risk factor may partially reflect the already established sex gap for anxiety and depressive symptoms (Albert, 2015; Lai et al., 2020; Pappa et al., 2020). It is noteworthy that older age and female sex are also risk factors for increased social stress during a pandemic. Numerous older adults have many household responsibilities and economic burdens (Dai et al., 2013; Jeong et al., 2014; Lin et al., 2016; Zhou et al., 2020), and human relations, communication, and cooperation tend to be more important to women than to men (Christov-Moore et al., 2014; Fujino et al., 2020; Wilson and Liu, 2003). Therefore, older people and women may be more vulnerable to social stress during the COVID-19 pandemic. Our results indicate that older and female hospital workers should be closely monitored as individuals at high risk for both mental illness and social stress, and early intervention should be provided for these problems.
Consistent with previous studies, we also found that occupational exposure to COVID-19 was a risk factor for increased anxiety (Liu et al., 2020; Xiao et al., 2020). Participating in treatments or procedures for infected patients was challenging for hospital workers because they were at high potential risk of infection (Liu et al., 2020; Xiao et al., 2020). High rates of mortality from COVID-19 pneumonia can intensify the perception of personal danger (Liu et al., 2020; Xiang et al., 2020; Xiao et al., 2020). Moreover, the time between infection and the onset of COVID-19 pneumonia could be relatively long; as a consequence, sustained and cumulative stress over time can turn into anxiety (Liu et al., 2020; Xiang et al., 2020; Xiao et al., 2020).
Additionally, having fewer non-work days was a significant risk factor for depression; this finding emphasizes that sufficient rest and non-work activity are important for maintaining mental health (Chen et al., 2020; Hallgren et al., 2017; Xiang et al., 2020). Further, we found that other medical staff and clerks or others reported a higher prevalence of depression than doctors. Previous studies have shown that nurses and medical technicians exhibited higher rates of depression than doctors; this finding could be attributed to the fact that nurses experience more and closer contact with COVID-19 patients than doctors (Lai et al., 2020; Pappa et al., 2020; Zhu et al., 2020). Clerks and other non-medical staff are reported to experience reduced access to medical information and formal psychological support than doctors (Matsuishi et al., 2012; Tan et al., 2020). Thus, limited knowledge regarding the COVID-19 virus, medical supplies, and self-care may cause their vulnerability to depression. It is important to spread sufficient information about infection, proper training for self-protection, and effective psychological intervention to all hospital workers.
Notably, analysis with TMDP identified that living conditions were a significant factor for social stress, which was not detected in the analyses with the other two scales (i.e., GAD-7 and PHQ-9). Living conditions were a significant risk factor not only for the TMDP total score, but also for the scores of its two subscales: concerns for infection and social stress. That is, hospital workers living with families or other individuals felt extremely high social stress during the COVID-19 pandemic. The COVID-19 virus demonstrates a high transmission rate, and, thus, hospital workers worry about bringing the virus home and passing it on to loved ones and family members, especially elderly parents, newborns and immunocompromised relatives (Chen et al., 2020; Tsamakis et al., 2020). Furthermore, hospital workers often feel fearful and guilty because of social stigma imposed on their families (Chen et al., 2020; Tsamakis et al., 2020). In addition, during the COVID-19 pandemic, the Japanese government is requesting that people refrain from going outside unless they urgently need to do so. People spend additional time with family members at home, which could lead to increased family conflicts during this hardship (Shiwaku et al., 2020; Guo et al., 2020). It should be noted that living with family, which in general is a normally protective factor for well-being (Miki et al., 2021), could be a risk factor for increased social stress during a pandemic.
In a similar manner, hospital workers experience many social stressors related to COVID-19. Apart from anxiety and depression, the social stresses can lead to reduced motivation and voluntary absenteeism, which can contribute to a collapse of medical systems (Chen et al., 2020; Chong et al., 2004; Imai et al., 2010; Shiwaku et al., 2020; Tei et al, 2014, 2015; Valdez and Nichols, 2013; Xiang et al., 2020). For this reason, early detection of these problems during a pandemic is vital. Our findings highlight the fact that attention should be paid to social factors, such as an individual's household composition and family relationships. Considering these issues, organizations should provide reasonable work arrangements and sufficient logical support for hospital workers.
This study has several limitations. First, this study was performed in only one hospital, which may limit the generalizability of the findings. Second, more than half of the participants were doctors, which may bias the findings. Third, this study used a cross-sectional study design, and thus causality between variables could not be established. Longitudinal follow-up studies could help reveal causality in the future.
In summary, our findings emphasize the urgent need for psychological monitoring and support for hospital workers during the COVID-19 pandemic, and it could be useful for developing policies and practices to minimize their risk of mental illness and increased social stress. In conclusion, comprehensive assessments of both mental and social factors are crucial for maintaining mental health and preventing voluntary absenteeism of hospital workers during a pandemic.
Role of the funding sources
This work was supported by a grant-in-aid for Scientific Research on Innovative Areas (16H06572) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT). The agency had no further role in the study design, collection, analysis, and interpretation of data, writing of the report, or in the decision to submit the paper for publication.
Authors' contributions
YM: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. JF: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. HS: Data curation, Formal analysis, Writing – review & editing MM: Data curation, Formal analysis, Writing – review & editing SD: Data curation, Formal analysis, Writing – review & editing.NH: Data curation, Writing – review & editing. DJ: Data curation, Writing – review & editing. ST: Data curation, Writing – review & editing. TT: Data curation, Writing – review & editing. TM: Data curation, Writing – review & editing. YS: Data curation, Writing – review & editing. NK: Data curation, Writing – review & editing. MI: Data curation, Writing – review & editing. SN: Data curation, Writing – review & editing. KO: Data curation, Writing – review & editing. TT: Data curation, Writing – review & editing. GS: Data curation, Writing – review & editing. TO: Data curation, Writing – review & editing .TF: Conceptualization, Writing – review & editing, Project administration. HT: Conceptualization, Writing – review & editing, Funding acquisition, Project administration.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Acknowledgements
We would like to thank those who participated in the study. We would also like to thank the staff for collaborating for mental health care during the COVID-19 pandemic.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.03.007.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Albert P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015;40:219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-Z., An F.-R., Xiang Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong M.-Y., Wang W.-C., Hsieh W.-C., Lee C.-Y., Chiu N.-M., Yeh W.-C., Huang T.-L., Wen J.-K., Chen C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Christov-Moore L., Simpson E.A., Coudé G., Grigaityte K., Iacoboni M., Ferrari P.F. Empathy: gender effects in brain and behavior. Neurosci. Biobehav. Rev. 2014;46:604–627. doi: 10.1016/j.neubiorev.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai J., Chiu H.F., Xiang Y.-T., Chan S.S., Yu X., Hou Z.-J., Ungvari G.S., Caine E.D. The prevalence of insomnia and its socio-demographic and clinical correlates in older adults in rural China: a pilot study. Aging Ment. Health. 2013;17:761–765. doi: 10.1080/13607863.2013.781117. [DOI] [PubMed] [Google Scholar]
- Fujino J., Tei S., Itahashi T., Aoki Y.Y., Ohta H., Kubota M., Hashimoto R.i., Takahashi H., Kato N., Nakamura M. Role of the right temporoparietal junction in intergroup bias in trust decisions. Hum. Brain Mapp. 2020;41:1677–1688. doi: 10.1002/hbm.24903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y., Cheng C., Zeng Y., Li Y., Zhu M., Yang W., Xu H., Li X., Leng J., Monroe-Wise A. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: cross-sectional study. J. Med. Internet Res. 2020;22 doi: 10.2196/20328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren M., Stubbs B., Vancampfort D., Lundin A., Jääkallio P., Forsell Y. Treatment guidelines for depression: greater emphasis on physical activity is needed. Eur. Psychiatry. 2017;40:1–3. doi: 10.1016/j.eurpsy.2016.08.011. [DOI] [PubMed] [Google Scholar]
- Imai H., Matsuishi K., Ito A., Mouri K., Kitamura N., Akimoto K., Mino K., Kawazoe A., Isobe M., Takamiya S. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Publ. Health. 2010;10:672. doi: 10.1186/1471-2458-10-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H.G., Han C., Park M.H., Ryu S.H., Pae C.U., Lee J.Y., Kim S.H., Steffens D.C. Influence of the number and severity of somatic symptoms on the severity of depression and suicidality in community‐dwelling elders. Asia Pac. Psychiatry. 2014;6:274–283. doi: 10.1111/appy.12138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X., Haralambous B., Pachana N.A., Bryant C., LoGiudice D., Goh A., Dow B. Screening for depression and anxiety among older Chinese immigrants living in Western countries: the use of the geriatric depression scale (GDS) and the geriatric anxiety inventory (GAI) Asia pac. Psychiatry. 2016;8:32–43. doi: 10.1111/appy.12191. [DOI] [PubMed] [Google Scholar]
- Liu C.-Y., Yang Y.-z., Zhang X.-M., Xu X., Dou Q.-L., Zhang W.-W., Cheng A.S. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol. Infect. 2020;148:e98. doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuishi K., Kawazoe A., Imai H., Ito A., Mouri K., Kitamura N., Miyake K., Mino K., Isobe M., Takamiya S. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin. Neurosci. 2012;66:353–360. doi: 10.1111/j.1440-1819.2012.02336.x. [DOI] [PubMed] [Google Scholar]
- Miki T., Yamamoto S., Inoue Y., Fukunaga A., Islam Z., Ishiwari H., Ishii M., Miyo K., Konishi M., Ohmagari N., Mizoue T. Association between living with others and depressive symptoms in Japanese hospital workers during the COVID‐19 pandemic. Psychiatry Clin. Neurosci. 2021 doi: 10.1111/pcn.13206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. J. Am. Med. Assoc. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020;74:281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiwaku H., Doi S., Miyajima M., Matsumoto Y., Fujino J., Hirai N., Jitoku D., Takagi S., Tamura T., Maruo T., Shidei Y., Kobayashi N., Ichihashi M., Noguchi S., Oohashi K., Takeuchi T., Sugihara G., Okada T., Fujiwara T., Takahashi H. A novel brief screening scale, Tokyo Metropolitan Distress Scale for Pandemic (TMDP), for assessing mental and social stress of medical staffs in COVID-19 pandemic. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13168. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tan B.Y., Chew N.W., Lee G.K., Jing M., Goh Y., Yeo L.L., Zhang K., Chin H.-K., Ahmad A., Khan F.A. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020;173:317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tei S., Becker C., Sugihara G., Kawada R., Fujino J., Sozu T., Murai T., Takahashi H. Sense of meaning in work and risk of burnout among medical professionals. Psychiatry Clin. Neurosci. 2015;69:123–124. doi: 10.1111/pcn.12217. [DOI] [PubMed] [Google Scholar]
- Tei S., Becker C., Kawada R., Fujino J., Jankowski K.F., Sugihara G., Murai T., Takahashi H. Can we predict burnout severity from empathy-related brain activity? Transl. Psychiatry. 2014;4:e393. doi: 10.1038/tp.2014.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsamakis K., Rizos E., Manolis A.J., Chaidou S., Kympouropoulos S., Spartalis E., Spandidos D.A., Tsiptsios D., Triantafyllis A.S. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp. Ther. Med. 2020;19:3451–3453. doi: 10.3892/etm.2020.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda M., Stickley A., Sueki H., Matsubayashi T. Mental health status of the general population in Japan during the COVID‐19 pandemic. Psychiatry Clin. Neurosci. 2020;74(9):505–506. doi: 10.1111/pcn.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdez C., Nichols T. Motivating healthcare workers to work during a crisis: a literature review. J. Manag. Policy Pract. 2013;14:43–51. [Google Scholar]
- Wilson M.S., Liu J.H. Social dominance orientation and gender: the moderating role of gender identity. Br. J. Soc. Psychol. 2003;42:187–198. doi: 10.1348/014466603322127175. [DOI] [PubMed] [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao X., Zhu X., Fu S., Hu Y., Li X., Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J. Affect. Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Yang Y., Shi T., Song Y., Zhou Y., Zhang Z., Guo Y., Li X., Liu Y., Xu G. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front. Psychiatry. 2020;11:520. doi: 10.3389/fpsyt.2020.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W. 2020. COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. (MedRxiv) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.