Abstract
Introduction
The COVID-19 pandemic has forced telehealth to be the primary means through which patients interact with their providers. There is a concern that the pandemic will exacerbate the existing disparities in overall healthcare utilization and telehealth utilization. Few national studies have examined the changes in telehealth use during the COVID-19 pandemic.
Methods
Data on 6.8 and 6.4 million employer-based health plan beneficiaries in 2020 and 2019, respectively, were collected in 2020. Unadjusted rates were compared both before and after the week of the declaration of the COVID-19 pandemic as a national emergency. Trends in weekly utilization were also examined using a difference-in-differences regression framework to quantify the changes in telemedicine and office-based care utilization while controlling for the patient's demographic and county-level sociodemographic measures. All analyses were conducted in 2020.
Results
More than a 20-fold increase in the incidence of telemedicine utilization after March 13, 2020 was observed. Conversely, the incidence of office-based encounters declined by almost 50% and was not fully offset by the increase in telemedicine. The increase in telemedicine was greatest among patients in counties with low poverty levels (β=31.70, 95% CI=15.17, 48.23), among patients in metropolitan areas (β=40.60, 95% CI=30.86, 50.34), and among adults than among children aged 0–12 years (β=57.91, 95% CI=50.32, 65.49).
Conclusions
The COVID-19 pandemic has affected telehealth utilization disproportionately on the basis of patient age and both the county-level poverty rate and urbanicity.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has precipitated a mass digital transition in the U.S. healthcare system. In March 2020, the Centers for Disease Control and Prevention called for nonemergent medical care to prioritize telehealth consultations.1 This was quickly followed by state and federal statutes relaxing Health Insurance Portability and Accountability Act of 1996 regulations and expanding reimbursement guidelines for telehealth.2
Preliminary evidence indicates that in-person visits have declined and that telehealth utilization has increased dramatically.3, 4, 5 More than 40% of Medicare fee-for-service primary care visits were provided through telehealth compared with <1% provided before the coronavirus disease 2019 (COVID-19) pandemic.6 Similarly, New York University's Langone Health reported a 700% increase in telehealth visits between March 2, 2020 and April 14, 2020 alone.7
Before the COVID-19 pandemic, disparities—including disparities related to geography, income, race/ethnicity, and age—in healthcare access and utilization have long pervaded.8 , 9 During the pandemic, within an individual healthcare system, there were disparities in telehealth utilization by the mean income of the patient's ZIP code.10 Without additional policies, disparities may widen in access to telehealth care.11 This study examines whether SARS-CoV-2 has changed the disparities in the utilization of telemedicine and office-based visits among a sample of >6 million commercially insured individuals.
METHODS
The RAND IRB approved this study and a waiver of informed consent. The study population—representing 6.8 million health plan beneficiaries in 2020 and 6.4 million in 2019—was derived from medical claims data collected by Castlight Health on approximately 200 employers across all the 50 U.S. states.12 In 2018, approximately half of the Castlight Health sample was female, and the average age was 33.4 years. Both the age and sex distribution for the Castlight Health sample are similar to the 2018 American Community Survey.
This study quantified healthcare utilization as the number of people receiving procedures per 10,000 eligible individuals weekly from January 2019 through July 2020. Incidence rates were aggregated across procedures, with separate rates calculated for telemedicine and office-based encounters. Telemedicine visits were defined using Current Procedural Terminology (CPT) codes and site of service fields. This included video and telephone encounters. The CPT codes used for office-based visits include facility visits, inpatient consults, outpatient consults, and preventive care. A full list of CPT codes is available in Appendix Table 1 (available online). Patient age, sex, and CPT codes were abstracted from claims. Patient county of residence was linked with sociodemographic measures from the 2018 American Community Survey,13 along with metropolitan status from the National Center for Health Statistics,14 number of COVID-19 cases from USAFacts,15 and broadband access from the Federal Communications Commission.16 The National Center for Health Statistics classifies counties as urban or rural.14
Trends in weekly utilization were calculated with a difference-in-differences regression framework to quantify the changes in telemedicine and office-based care utilization before versus those after March 13, 2020 when the COVID-19 pandemic was declared a national emergency. Models included measures for the patient's age and sex. Also included were the county's urbanicity, percentage of White residents, percentage of Black residents, percentage of Hispanic residents, percentage of individuals below the federal poverty line, total number of weekly COVID-19 cases per 10,000 residents, the unemployment rate in July, percentage of households without broadband Internet, and percentage not speaking English only in their household. Finally, fixed effects for the state of residence, calendar year, and the week of the year were also included. SEs were clustered at the state level. Estimates are reported using 2-sided 95% CIs. All data were collected and analyzed in 2020. The unit of analysis is the number of individuals within each age group, sex, and county for a specific week. The analysis was done using Stata, version 15.1.
RESULTS
Table 1 shows a summary of weekly healthcare utilization per 10,000 eligible people before versus the summary after March 13, 2020 according to the site of service and demographic characteristics. More than a 20-fold increase in the incidence of telemedicine utilization was observed after March 13, 2020. Conversely, the incidence of office-based encounters declined by almost 50% and was not fully offset by the increase in telemedicine. Appendix Table 2 (available online) includes the rates for all the covariates included in the regression models.
Table 1.
Rates of Telemedicine and Office-Based Healthcare Utilization Before Versus After Start of COVID-19
| Demographic characteristics | Total visits |
Telemedicine |
In-person care |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Rate before COVID-19 | Rate after COVID-19 | Change in rate | Ratea before COVID-19 | Rateb after COVID-19 | Change in rate | Ratec before COVID-19 | Rated after COVID-19 | Change in rate | |
| Age group | |||||||||
| Young children (0‒12 years) | 754.3 (1,409.1) | 490.1 (1,126.2) | ‒264.2 | 2.7 (80.6) | 63.2 (338.6) | 60.6 | 751.7 (1,406.4) | 426.9 (1,070.5) | ‒324.8 |
| Teenagers (13‒18 years) | 489.2 (964.0) | 377.7 (826.3) | ‒11.5 | 3.0 (71.5) | 103.2 (415.9) | 100.2 | 486.1 (960.7) | 274.5 (709.0) | ‒211.7 |
| Younger adults (19‒45 years) | 456.2 (964.0) | 421.6 (742.1) | ‒34.5 | 4.4 (78.9) | 101.1 (334.2) | 96.6 | 451.7 (812.6) | 320.5 (653.2) | ‒131.1 |
| Older adults (≥46 years) | 796.1 (1,111.2) | 659.8 (985.6) | ‒136.3 | 2.8 (64.9) | 121.4 (376.7) | 118.6 | 793.3 (1,108.7) | 538.4 (907.5) | ‒254.9 |
| % Below poverty linee | |||||||||
| 1st quartile (lowest) | 620.8 (1,067.1) | 489.6 (934.4) | ‒131.2 | 3.6 (71.2) | 116.1 (380.9) | 112.5 | 617.2 (1,063.8) | 373.6 (848.2) | ‒243.6 |
| 2nd quartile | 622.0 (1,088.2) | 489.4 (918.3) | ‒132.6 | 3.4 (71.1) | 99.6 (362.0) | 96.1 | 618.6 (1,085.6) | 389.8 (837.0) | ‒228.7 |
| 3rd quartile | 646.5 (1,077.5) | 511.5 (904.5) | ‒135.0 | 3.4 (78.4) | 90.9 (330.6) | 87.5 | 643.1 (1,074.3) | 420.5 (839.8) | ‒222.6 |
| 4th quartile (highest) | 671.9 (1,223.7) | 527.8 (1,029.0) | ‒144.2 | 2.7 (76.6) | 83.5 (372.5) | 80.7 | 669.2 (1,220.8) | 444.3 (949.7) | ‒224.9 |
| Ruralityf | |||||||||
| Metropolitan | 661.2 (574.3) | 522.8 (462.1) | ‒138.4 | 3.4 (28.9) | 125.9 (182.7) | 122.5 | 657.8 (573.4) | 396.9 (431.9) | ‒260.9 |
| Not metropolitan | 630.1 (1,284.8) | 496.1 (1,092.6) | ‒134.0 | 3.2 (87.6) | 85.0 (415.7) | 81.7 | 626.9 (1,281.2) | 411.2 (1,002.0) | ‒215.7 |
Number of persons receiving telemedicine care per 10,000 eligible beneficiaries weekly for all of 2019 and Weeks 1–10 in 2020.
Number of persons receiving telemedicine care per 10,000 eligible beneficiaries weekly from Weeks 11–31.
Number of persons receiving office-based care per 10,000 eligible beneficiaries weekly for all of 2019 and Weeks 1–10 in 2020.
Number of persons receiving office-based care per 10,000 eligible beneficiaries weekly from Weeks 11–31.
Share of U.S. county (%) living below the federal poverty line in the county where the patient resides (https://www.census.gov/topics/income-poverty/poverty/data/tables/acs.html).
U.S. county metropolitan classification according to the county where the patient resides (https://www.cdc.gov/nchs/data_access/urban_rural.htm).
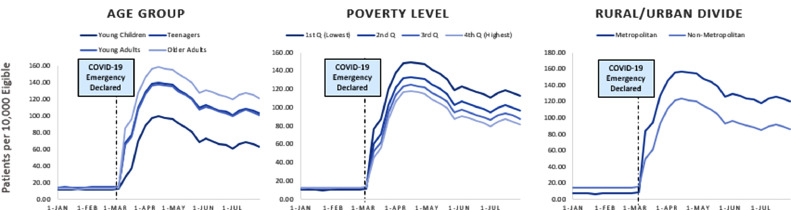
Figure 1 shows the covariate-adjusted rates for telemedicine visits from the regression analyses. The increase in telemedicine was greatest among patients in counties with low poverty levels (β=31.70, 95% CI=15.17, 48.23), among those in metropolitan areas (β=40.60, 95% CI=30.86, 50.34), and among adults than among children aged 0–12 years (β=57.91, 95% CI=50.32, 65.49). The full regression results can be found in Appendix Table 3 (available online).
Figure 1.
Adjusted rates of telemedicine utilization before versus that after the start of COVID-19 pandemic.
Note: The graph shows the number of persons receiving telemedicine care per 10,000 eligible beneficiaries. Young children represent ages 0‒12 years, teenagers represent ages 13‒18 years, young adults represent ages 19‒45 years, and older adults represent ages ≥46 years. Q represents the share of U.S. county (%) living below the federal poverty line in the county where the patient resides (https://www.census.gov/topics/income-poverty/poverty/data/tables/acs.html). The highest Q represents the counties that have the highest share of the population who are below the federal poverty line, whereas the lowest Q represents the counties that have the lowest share of the population who are below the federal poverty line. U.S. county metropolitan classification was done on the basis of the county where the patient resides (https://www.cdc.gov/nchs/data_access/urban_rural.htm). The full regression results for the figure can be found in Appendix Table 3 (available online).
APR, April; FEB, February; JAN, January; JUL, July; JUN, June; MAR, March; Q, quartile.
DISCUSSION
On the basis of a large sample of commercially insured individuals, there was a substantial increase in telemedicine utilization during the COVID-19 pandemic. The increase disproportionately benefited higher-income, metropolitan-dwelling adults. Other studies have reported that before the pandemic, communities with poor geographic access to health care disproportionately utilized telemedicine.17 The results indicate that there was an increase in telemedicine use in metropolitan and nonmetropolitan counties. The increase in telemedicine use was slightly higher in metropolitan counties. There was also evidence that low-income communities have exhibited lower uptake of telemedicine. Possible mediators for the differences in the subgroups could be cultural/political factors and differences in educational levels. Finally, it appears that telemedicine use for children is lagging behind that for adults. More intensive training for parents and pediatricians and like-minded efforts to address barriers to children's access to telemedicine may be necessary.
Limitations
Study limitations include that data are from a single employer-insured sample, and the results are unlikely to represent those of other payers. Similarly, the results are limited to the 200 national employers in the data. Thus, the results may not be the same for other local employers. The study did not examine what the purpose of the visit was, nor whether there were changes in the reason for the visit both before and after the pandemic. Because the study sample includes those with employer-based insurance, the results will not be generalizable to low-income individuals on Medicaid and older individuals on Medicare. This is particularly concerning given that both low-income individuals18 , 19 and older adults are at a heightened risk of infection and severe illness from COVID-19.19 The results did not account for multiple testing on the interaction terms. The analyses failed to account for changes in enrollment patterns both before and during the COVID-19 pandemic. Recent estimates have reported that declines in employer-sponsored insurance are lower than expected. Finally, the results do not fully capture the shifts in providers offering telehealth services.
CONCLUSIONS
This study is an important first step in the collective understanding of telehealth utilization as the COVID-19 pandemic progresses. There is uncertainty in whether the current rates and disparities in telehealth will continue. Similarly, the future of the current telehealth policy is unknown.20 Policymakers should continue to expand reimbursement for telehealth services and also update clinical guidelines to encourage healthcare practitioners to use telehealth.21 Given the results, policymakers should make a more concerted effort to reach populations who are deferring in-office care and not replacing it with telehealth visits.
This study provides evidence on the increased use of telehealth during the COVID-19 pandemic by using national claims data for >6 million individuals. There are substantial disparities in the use of telehealth by patient age and county-level measures for poverty rate and urbanicity.
ACKNOWLEDGMENTS
The funding sources of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or the preparation, review, and decision to submit the manuscript.
Support was provided by the National Institute on Aging (1K01AG061274, CW) and the Robert Wood Johnson Foundation.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.01.030.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Hartnett KP, Kite-Powell A, DeVies J. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375–2376. doi: 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
- 3.Wosik J, Fudim M, Cameron B. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the U.S. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whaley CM, Pera MF, Cantor J. Changes in health services use among commercially insured U.S. populations during the COVID-19 pandemic. JAMA Network Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Office of the Assistant Secretary for Planning and Evaluation, HHS . Office of the Assistant Secretary for Planning and Evaluation, HHS; Washington, DC: 2020. ASPE issue brief: Medicare beneficiary use of telehealth visits: early data from the start of the COVID-19 pandemic.https://aspe.hhs.gov/pdf-report/medicare-beneficiary-use-telehealth#:∼:text=the%20analysis%20found%20medicare%20primary,before%20the%20phe%20in%20february Published July 28, 2020. Accessed October 2, 2020. [Google Scholar]
- 7.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147–2149. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 10.Chunara R, Zhao Y, Chen J. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(1):33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta A, Nguyen AM, Chang JE, Lai AY, Berry C, Shelly DR. Five ways—beyond current policy—to truly integrate telehealth into primary care practices. Bethesda, MD: Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20200903.597561/full/. Published September 9, 2020. Accessed October 2, 2020.
- 12.Our story. Castlight Health. https://www.castlighthealth.com/about/. Accessed September 24, 2020.
- 13.U.S. Census Bureau. American community survey 5-year data 2009-2018. Suitland-Silver Hill, MD: U.S. Census Bureau. https://www.census.gov/data/developers/data-sets/acs-5year.html. Published December 10, 2020. Accessed July 19, 2020.
- 14.NCHS urban rural classification scheme for counties. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Updated June 1, 2017. Accessed July 18, 2020.
- 15.Coronavirus outbreak stats & data. USAFacts. https://usafacts.org/issues/coronavirus/. Updated July 25, 2020. Accessed July 25, 2020.
- 16.Mapping broadband health in America. Federal Communications Commission. https://www.fcc.gov/health/maps. Updated June 8, 2017. Accessed August 4, 2020.
- 17.Jetty A, Moore MA, Coffman M, Petterson S, Bazemore A. Rural family physicians are twice as likely to use telehealth as urban family physicians. Telemed J E Health. 2018;24(4):268–276. doi: 10.1089/tmj.2017.0161. [DOI] [PubMed] [Google Scholar]
- 18.James MK, Kishore M, Lee SW. Demographic and socioeconomic characteristics of COVID-19 patients treated in the emergency department of a New York City hospital. J Community Health. 2020 doi: 10.1007/s10900-020-00937-2. In press. Online October 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu HE, Ashe EM, Silverstein M. Race/ethnicity, underlying medical conditions, homelessness, and hospitalization status of adult patients with COVID-19 at an Urban Safety-Net Medical Center - Boston, Massachusetts, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):864–869. doi: 10.15585/mmwr.mm6927a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lucia K, Blumberg LJ, Curran E, et al. The COVID-19 pandemic – insurer insights into challenges, implications, and lessons learned. Washington, DC: Urban Institute. https://www.urban.org/research/publication/covid-19-pandemic-insurer-insights-challenges-implications-and-lessons-learned. Published June 29, 2020. Accessed August 10, 2020.
- 21.Uscher-Pines L. Moving on from telehealth-by-desperation: what will make telehealth stick. Bethesda, MD: HealthAffairs. https://www.healthaffairs.org/do/10.1377/hblog20200810.737666/full/. Published August 14, 2020. Accessed November 22, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.