Abstract
Objectives
COVID-19 infection has been compared to seasonal influenza as an argument against non-pharmacological population-based infection control measures known as “lockdowns”. Our study sought to compare disease severity measures for patients in Ireland hospitalised with COVID-19 against those hospitalised with seasonal influenza.
Study design
This is a retrospective population-based cohort study.
Methods
COVID-19 hospital episodes and seasonal influenza hospital episodes were identified using relevant International Classification of Disease (ICD-10) codes from the Irish national hospitalisation dataset. The occurrences of key metrics of disease severity, length of stay, intensive care admission, ventilatory support, haemodialysis and in-hospital mortality were measured and compared between the two groups using odds ratios with 95% confidence intervals (CIs), stratified by age.
Results
Hospitalised COVID-19 episodes had a mean length of stay more than twice as long as hospitalised influenza episodes (17.7 days vs 8.3 days). The likelihood of all measures of disease severity was greater in COVID-19 episodes, and the odds of in-hospital mortality were five-fold higher in this group compared with seasonal influenza episodes (OR 5.07, 95% CI 4.29–5.99, P < 0.001). Greater likelihood of increased disease severity was observed for COVID-19 episodes in most age groups.
Conclusions
COVID-19 is a more severe illness than seasonal influenza in hospitalised cohorts. It is imperative that public health professionals ensure that evidence-based advocacy is part of the response to COVID-19 to tackle a dangerous “infodemic” that can undermine public health control measures.
Keywords: COVID-19 [MeSH]; Influenza, Human [MeSH]; Disease severity [MeSH]; Hospital mortality [MeSH]; “Infodemic”
Introduction
In late December 2019, a cluster of pneumonia cases of unknown aetiology were identified in Wuhan, China.1 The cause of this outbreak was subsequently identified as a novel strain of coronavirus named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS CoV-2).2 Patients with SARS Cov-2 presented with acute respiratory illness, which progressed to pneumonia and acute respiratory failure in many cases. This presentation came to be known as Coronavirus Disease 2019 (COVID-19).2
COVID-19 has become a pandemic affecting millions of people worldwide with the first case in Ireland notified on February 29th 2020.3 , 4 Similar to other countries, subsequent rapid spread in the Irish population mandated the introduction of significant non-pharmacological interventions including severe societal restrictions, known as “lockdowns”, in mid-March 2020.5 , 6 Whilst effective in limiting cases,7 , 8 relaxation of restrictions during the summer in Ireland was followed by a further surge of cases from late autumn 2020,9 resulting in the reintroduction of a modified lockdown on October 21st 2020.10 These restrictions were released again in December 2020, with an expectation of re-introduction in early 2021 to deal with a resurgence of cases following the holiday period.
Given the substantial impact lockdowns have had on wider social, economic and educational spheres,11 , 12 counter-arguments against their use are emerging. A common counter-argument is that COVID-19 is essentially “a bad flu” and that similar lockdowns are not implemented during influenza seasons. This argument has featured in the debate on pandemic response in Ireland and has even been used by leading medical professionals to advocate against the use of population-based restrictions for COVID-19 control.13 The World Health Organization (WHO) has identified misinformation and the “infodemic” as a critical challenge in addressing COVID-19.14 It undermines political leadership for difficult decision-making, as well as public support for public health measures, including potentially driving vaccine hesitancy in the future.15 , 16 Critical reviews of scientific evidence are central to building carefully designed and delivered COVID-19-specific risk communication strategies, which are essential to control both the disease and the associated “infodemic”.17
Current evidence indicates that hospitalised cases of COVID-19 were more likely to be male, younger and have fewer comorbidities than hospitalised cases of seasonal influenza.18 Hospitalised COVID-19 patients tended to have a longer mean length of hospital stay (14 days; 95% Confidence Interval (CI) 12–16, P < 0.001) when compared to hospitalised influenza A (6.5 days; 95% CI 6–8, P < 0.001) and hospitalised influenza B cases (6.7 days; 95% CI 5.3–8, P < 0.001).19 Mortality amongst hospitalised COVID-19 patients (6.5%; 95% CI 4.5–9, P < 0.001) was found to be similar to that of influenza A patients (6%; 95% CI 5–6.5, P < 0.001) but higher than that of influenza B patients (3%; 95% CI 2–4, P < 0.001); however, significant variability in mortality rates of influenza A was observed depending on the subtype of the virus involved as well as the reporting country.19
The assertion that COVID-19 was “just a bad flu” can be tested empirically to challenge the “infodemic” and better inform key decision-makers and the public. WHO's Pandemic Influenza Severity Assessment (PISA) document identifies three concepts in order to determine the severity of infection with pandemic influenza: transmissibility, disease seriousness and impact.20 The objective of this study was to measure the disease seriousness and impact of COVID-19 from the perspective of the Irish healthcare sector through descriptive epidemiological analysis of COVID-19-related hospital episodes with a specific focus on mean length of hospital stay, resource use during hospital stay and in-hospital mortality and benchmarking these results against influenza-related hospital episodes.
Methods
Data source
The Hospital In-Patient Enquiry (HIPE) system, managed by the Health Service Executive (HSE) Healthcare Pricing Office, was the data source for this study and was accessed via the Health Atlas Ireland system maintained by the HSE National Health Intelligence Unit.21 This database is a well-established, quality assured, national hospital care information system that uses International Classification of Disease-10 Australian Modification (ICD10 AM), Australian Classification of Health Interventions (ACHI) and Australian Coding Standards (ACS) coding to capture demographic, clinical and care data at discharge on all episodes of emergency and elective care across publicly funded hospitals in Ireland. While private hospital activity in Ireland is not captured in the system, in terms of in-patient care, that sector is focused almost exclusively on provision of elective care so HIPE is likely to have high completeness for acute hospital episodes related to COVID-19 and influenza in Ireland.
Inclusion criteria
The COVID-19 data included in this study consisted of episodes of hospitalisation discharged up to August 10th 2020; these data effectively captured the “first wave” of COVID-19 in Ireland.22 COVID-19-related discharge episodes were defined by the presence of any of the following (ICD-10) codes: U07.1, B34.2 or B97.2. Influenza-related discharge episodes were identified between January and December of both 2018 and 2019 with the following ICD-10 codes: J09, J10.0, J10.1, J10.8, J11.0, J11.1 or J11.8. For both clinical conditions, relevant codes were identified across any of the 30 diagnostic fields on the episode's HIPE record. The timeframe of influenza-related discharge episodes included in this study was selected with reference to national epidemiological surveillance information to assure it was both current and representative of recent variation in influenza seasonal severity.23 , 24
Statistical analysis
In order to identify the impact of both COVID-19 and influenza on acute hospital services, the following variables were examined: mean length of hospital stay (days), Intensive Care Unit (ICU) admission requirement (number; %), haemodialysis requirement (ACHI Codes 131000-131008) (number, %) and invasive and non-invasive ventilation requirement (ACHI Codes 1388200/1388201/1388202 or 9220900/9220901/9220902) (number, %). The number and proportion of in-hospital mortality in both cohorts were also measured. To take account of potential differences in age-profiles of cases, data were stratified according to the following age-groups: 0–19 years, 20–39 years, 40–64 years, 65–84 years and 85 years and older. This age stratification allowed an analysis of COVID-19 patients that aligned with age categories commonly used for health service planning in Ireland: child and adolescent (0–19 years), early adulthood (20–39 years), middle adulthood (40–64 years), late adulthood (65–84 years) and elderly (85 years and older). This grouping also enabled statistical disclosure control. Odds ratios (ORs), with 95% CIs and significance tests for each variable measured, were also calculated using standard procedures to compare the likelihood of adverse outcomes in COVID-19-related episodes relative to influenza episodes.25 For statistical disclosure control purposes, where observed cases were less than 5, these are not reported and are displayed as “<5”.
Results
In total, 4,837 COVID-19 and 5,369 influenza discharge episodes were identified, and the disease severity and impact were described and compared by age group.
Mean length of stay
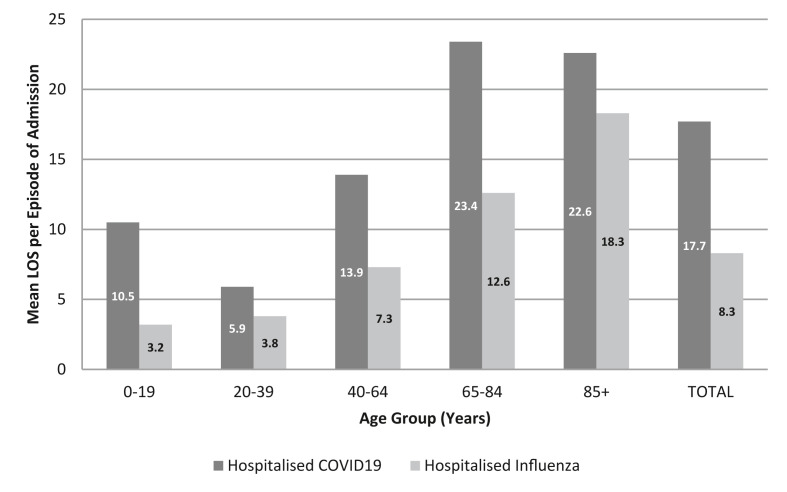
Fig. 1 displays the mean length of stay for hospitalised episodes of COVID-19 and influenza stratified by age-group. Across all age-groups, hospitalised episodes of COVID-19 had longer lengths of stay compared to influenza episodes. In adult cases, this difference was most pronounced in the 65–84 year age group. In total, hospitalised COVID-19 episodes had a mean length of stay more than twice as long as hospitalised influenza (17.7 days vs 8.3 days).
Fig. 1.
Mean lengths of stay (LOS) in days per episode of admission for hospitalised COVID-19 and influenza patients, stratified by age group.
Hospital resource requirement
Table 1 provides the proportion of COVID-19 and influenza hospital episodes requiring ICU admission, invasive and non-invasive ventilation and haemodialysis stratified by age group and compares the odds of each adverse outcome.
Table 1.
Comparison of age-stratified descriptive epidemiology and unadjusted odds ratios for ICU admission, invasive and non-invasive ventilation, haemodialysis and in-hospital mortality in episodes of COVID-19 and influenza hospitalisations.
| Age Group (Years) | Disease | ICU Admission |
Ventilation |
Haemodialysis |
In-Hospital Mortality |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | ORa (95% CI) | P-valueb | n (%) | ORa (95% CI) | P-valueb | n (%) | ORa (95% CI) | P-valueb | n (%) | ORa (95% CI) | P-valueb | ||
| 0–19 | Influenza | 56 (4.0) | 1.0 | 60 (4.3) | 1.0 | <5 | 1.0 | <5 | 1.0 | ||||
| COVID-19 | 9 (10.2) | 2.73 (1.30–5.72) | P = 0.008 | 5 (5.7) | ns | <5 | 8.03 (0.72–89.41) | ns | <5 | 8.03 (0.72–89.41) | ns | ||
| 20–39 | Influenza | 33 (4.5) | 1.0 | 14 (1.9) | 1.0 | 7 (0.9) | 1.0 | <5 | 1.0 | ||||
| COVID-19 | 44 (7.5) | 1.70 (1.06–2.70) | P = 0.03 | 35 (6.0) | 3.21 (1.71–6.03) | <0.001 | 7 (1.2) | 1.24 (0.43–3.55) | ns | 9 (1.5) | 2.80 (0.86–9.15) | ns | |
| 40–64 | Influenza | 100 (9.0) | 1.0 | 80 (7.1) | 1.0 | 33 (2.9) | 1.0 | 24 (2.2) | 1.0 | ||||
| COVID-19 | 298 (18.0) | 2.22 (1.74–2.82) | <0.001 | 297 (17.9) | 2.82 (2.17–3.65) | <0.001 | 82 (4.9) | 1.70 (1.13–2.57 | P = 0.011 | 79 (4.8) | 2.27 (1.43–3.61) | <0.001 | |
| 65–84 | Influenza | 173 (10.2) | 1.0 | 147 (8.7) | 1.0 | 26 (1.5) | 1.0 | 108 (6.4) | 1.0 | ||||
| COVID-19 | 210 (11.2) | 1.11 (0.90–1.37) | ns | 252 (13.5) | 1.64 (1.32–2.03) | <0.001 | 72 (3.8) | 2.56 (1.63–4.04) | <0.001 | 417 (22.3) | 4.21 (3.36–5.26) | <0.001 | |
| 85+ | Influenza | 24 (5.4) | 1.0 | 24 (5.4) | 1.0 | <5 | 1.0 | 47 (10.6) | 1.0 | ||||
| COVID-19 | 14 (2.2) | 0.40 (0.20–0.77) | P = 0.007 | 38 (6.0) | 1.12 (0.66–1.89) | ns | 13 (2.1) | 19.33 (1.15–326.03) | P = 0.039 | 235 (37.2) | 4.99 (3.54–7.03) | <0.001 | |
| All | Influenza | 385 (7.2) | 1.0 | 325 (6.0) | 1.0 | 67 (1.2) | 1.0 | 185 (3.4) | 1.0 | ||||
| COVID-19 | 575 (11.9) | 1.75 (1.53–2.00) | <0.001 | 627 (13.0) | 2.31 (2.01–2.66) | <0.001 | 175 (3.6) | 2.97 (2.24–3.95) | <0.001 | 741 (15.3) | 5.07 (4.29–5.99) | <0.001 | |
ns: Not Significant; ICU: Intensive Care Unit; OR: Odds Ratio; COVID-19: Coronavirus Disease 2019; CI: confidence interval.
ORs were calculated with 95% confidence intervals and P values based on Chi-squared tests of proportions.
Significance level set at a p-value ≤0.05. Characteristics meeting this significance threshold are shaded in grey.
In general, a higher proportion of COVID-19-related hospital episodes were admitted to ICU than influenza-related hospital episodes, except for those aged 85 and older where the proportion of ICU admission was greater for influenza-related hospital episodes. The likelihood of ICU admission was significantly higher for COVID-19-related hospital episodes than influenza-related episodes in age groups under 65 years and overall. Compared with influenza, COVID-19-related hospital episodes were almost two times more likely to be admitted to ICU (odds ratio [OR] 1.75, 95% CI 1.53–2.0, P < 0.001).
A similar pattern was observed when the requirement for ventilation and haemodialysis in COVID-19 episodes was compared to that for influenza. In general, the likelihood of invasive or non-invasive ventilation was greater among COVID-19 hospital episodes compared with influenza hospital episodes across all age groups (OR 2.31, 95% CI 2.01–2.66, P < 0.001), and statistically increased odds of ventilation were observed for COVID-19 hospital episodes in the 20–84 year age groups. The likelihood of haemodialysis was also greater among COVID-19 hospital episodes compared with influenza hospital episodes across all age groups (OR 2.97, 95% CI 2.24–3.95, P < 0.001), and statistically increased odds of haemodialysis were observed for COVID-19 hospital episodes aged older than 40 years.
In-hospital mortality
Table 1 also provides the proportion of COVID-19 and influenza hospital episodes where in-hospital mortality was recorded, stratified by age-group. Overall, across all age groups, 15.3% of COVID-19-related hospital episodes experienced in-hospital mortality compared with 3.4% of influenza-related hospital episodes indicating a five-fold increased likelihood of in-hospital mortality for hospital episodes related to COVID-19 (OR 5.07, 95% CI 4.29–5.99, P < 0.001). While an increased likelihood of in-hospital mortality was observed for COVID-19-related hospital episodes in each age group, the difference was significant in age groups older than 40 years, with ORs increasing from 2.27 (95% CI 1.43–3.61, <0.001) in the 40–64 year group to 4.99 (95% CI 3.54–7.03, <0.001) in the 85 years and older group.
Discussion
This study was undertaken to help tackle the “infodemic” threatening the public health response to the COVID-19 pandemic in Ireland. Using Irish national inpatient data, it identified that COVID-19-related episodes had a greater likelihood of more intense resource requirement and adverse outcomes than influenza episodes. These differences were significant for the overall population and remained significant in most age-groups following stratification.
Comparison with other studies
Our findings are similar to other comparisons of COVID-19 and influenza patients. In Pormohammad et al.’s systematic review, COVID-19 patients had longer mean lengths of hospitalisation compared to influenza A and B patients (14 days vs 6.5 and 6.7 days respectively),19 which is similar to the findings of this study (17.7 vs 8.3 days for COVID-19 and influenza respectively). Pormohammad et al. reported similar rates of mortality in COVID-19 and influenza A patients (6.5% vs 6%) but higher rates of mortality in COVID-19 versus influenza B patients (6.5% vs 3%).19 This study did not distinguish between influenza strains as this was not recorded in the ICD coding in the data source, but a much higher rate of in-hospital mortality in COVID-19 compared with influenza patients (15.3% vs 3.4%) was found. Influenza patients admitted to hospitals in Ireland in 2018 and 2019 were examined and data were included from influenza seasons where influenza B was the predominant circulating strain (2017/2018 season) and where influenza A was the predominant circulating strain (2018/2019) in Ireland,23 , 24 resulting in outcomes where both influenza strains are captured. We report higher mortality rates to those reported by Pormohammad et al., which reflects our focus on hospitalised cases, and we provide greater detail on age patterning of mortality for COVID-19 hospitalisations relative to seasonal influenza.19
COVID-19 patients aged 65–84 years in this study did not have significantly higher odds of ICU admission compared to similarly aged influenza patients. However, COVID-19 patients aged 85 years and older were significantly less likely to be admitted to ICU compared to influenza patients in the same age group. This was an unexpected finding, but should be interpreted with caution given the small numbers and the lack of full adjustment for comorbidities and other factors related to clinical decisions regarding ICU admission. While the finding raises potential questions about clinical prioritisation for scarce ICU resources, compared to influenza patients, COVID-19 patients in this age group had similar odds of receiving ventilator support. This included non-invasive ventilation support delivered outside the ICU setting, which may have been a more clinically appropriate care given these patients’ individual needs. Furthermore, COVID-19 patients in this age group were more likely to receive haemodialysis care than influenza patients.
Auvinen et al. reported higher proportions of ICU admission (29% vs 6%), invasive ventilation (29% vs 3%) and in hospital mortality (4% vs 0%) in COVID-19 patients compared to influenza patients.26 While we also reported higher rates of these adverse outcomes for COVID-19 hospitalisations, as discussed above, our age-specific findings on ICU admission are different, possibly reflecting differences in local resource availability and clinical practices. Cobb et al. examined COVID-19 and influenza patients admitted to ICUs.27 Logistic regression modelling reported no difference in the odds of renal replacement therapy and mechanical ventilation in COVID-19 patients compared to influenza patients, but did report an almost two-fold increase in odds of in hospital mortality for COVID-19 patients compared to influenza patients following adjustment for age, gender and a number of comorbidities. These findings are similar to those reported in this study in terms of increased likelihood of adverse outcome for COVID-19 hospitalised patients; however, we reported unadjusted ORs and used stratification to confirm the age-patterning of risk. Neither Auvinen et al. nor Cobb et al. stratified their outcomes analysis by age group.26 , 27 This comparison shows that our study supports many of the findings in medical literature comparing COVID-19 patients and influenza patients, specifically longer lengths of hospitalisation and higher rates of mortality, ICU admission and ventilation in COVID-19 patients. It also provides a valuable insight into the impact of COVID-19 on Irish hospitals during the “first wave” of the pandemic.
Strengths and weaknesses
This study is the first to provide a comparison of COVID-19 and influenza episodes of hospitalisation in the Irish population. A robust and definitive national dataset was used to identify large numbers of episodes of hospitalisation in both the COVID-19 (n = 4,837) and influenza cohorts (n = 5,369).21 This dataset is quality assured and has been used by other groups to produce epidemiological studies.28
While we have not adjusted for all potential prognostic factor differences between the two groups compared, our view is that our approach of age-stratification is epidemiological and clinically useful since it provides an opportunity to examine the effect of age-group on the relative likelihood of adverse outcome within each age stratum. Most other prognostic factors, such as co-morbidity, are likely to be age-related and similar between the two groups. This is supported by Pormohammad et al.’s finding of a similar occurrence of comorbidities such as cardiovascular/cerebrovascular disease, chronic respiratory disease and diabetes amongst COVID-19 and influenza cohorts.19
Identification of influenza episodes focused on 2018 and 2019, and the question of representativeness and comparability may arise. The majority of COVID-19 episodes included in this study were notified from March 2020 onwards and while data on influenza hospitalisations in the same period was available, we chose not to use this since the influenza season in Ireland was ending when COVID-19 arose and we have since observed significant changes in influenza activity to patterns expected owing to the wider impact of non-pharmacological measures.29 The 2017/2018 influenza season in Ireland was severe due to a mismatch between the vaccine used and the circulating strain that season.23 The 2018/2019 season in Ireland was a moderate season where the circulating strain matched the vaccine used that season.24 Using aggregated data from both years allowed us to incorporate outcomes from both a severe and moderate season and allowed us to estimate a “typical” influenza season.
A limitation of HIPE data on both influenza and COVID-19 hospitalisations was that in order to maintain patient anonymity, geo-location of individual episodes was limited to their county of residence, which is used in Ireland to assign an area-based deprivation index so as to examine the effect of socio-economic status on health.21 Additionally, ethnicity of episodes of hospitalisation was not recorded in the HIPE database.21 As a result, analysis of episode distribution according to deprivation indices or patient ethnicity was not possible.
Data on hospitalised episodes of influenza sourced from HIPE were not stratified according to the serotype of influenza identified because the ICD-10 coding does not distinguish this detail. Mortality rates varied when COVID-19 was compared to influenza A and influenza B.19 However, as our study's cohort of hospitalised influenza episodes included a season where influenza A was the dominant circulating strain and a season where influenza B was the dominant circulating strain, although influenza mortality rates were not stratified by serotype, they are likely to be representative of both strains. Finally, seasonal influenza vaccine may have attenuated resource use and outcomes of hospitalised episodes. However, the uptake of seasonal influenza vaccines by individuals in high risk groups in Ireland has consistently failed to reach the target of 75% as set by WHO.30 HPSC reported influenza vaccine uptake for those aged 65 years and older in the 2017/2018 season to be 57.6% and in the 2018/2019 season to be 65.9% both far below the target.31 Influenza vaccine uptake amongst attendees at a respiratory outpatient clinic in Ireland was as low as 54%.32 Uptake of influenza vaccine in patients aged over 65 actually fell in Ireland between the 2004/2005 season and the 2014/2015 season.33 Therefore, whilst influenza vaccination may have played a role in limiting the numbers of influenza hospitalisations and the clinical severity of these cases, it is unlikely to explain the increased disease severity and poorer outcomes observed in this study in COVID-19 patients compared with influenza patients, especially in patients aged less than 65 years.
Summary and conclusion
Our study adds to existing evidence confirming that COVID-19 is overall more severe than influenza amongst hospitalised patients. It corroborates this evidence in the Irish population using a robust national dataset and develops it by providing an epidemiologically and clinically relevant examination of the comparison of the two diseases by age group. It supports important public health efforts, such as targeting protective measures for higher-risk groups. Crucially, it provides evidence to counter arguments that COVID-19 is “just a bad flu”. In the era of misinformation and “infodemics”, public health professionals must not only combat the disease but must also ensure that they are positively engaged in evidence-based public health advocacy with accurate and relevant information to underpin discussion on measures to limit the impact of COVID-19.
Author statements
Acknowledgements
HIPE data were sourced from the HSE Healthcare Pricing Office. We are grateful to Dr Howard Johnson, Clinical Lead Health Intelligence, HSE, who enabled access to HIPE data via the Health Atlas Ireland health analytics platform. We are also grateful to Dr Siobhan Ní Bhriain, Lead for Integrated Care, Health Service Executive (HSE), and Dr Colm Henry, Chief Clinical Officer, HSE, who provided helpful comments on draft versions of the work presented in this article.
Ethical approval
Ethical review was not required for this study. The data used in the study are controlled by the Health Service Executive (HSE) in Ireland. The study authors are registered medical professionals. Legal duties, organisational policies and good practices were observed in data handling and the data processing for the study was conducted for medical purposes by the authors to inform the statutory function of the HSE in Ireland to improve, promote and protect the health and welfare of the public (Section7, Health Act 2004), thus consistent with General Data Protection Regulations and their application in Ireland.34 HIPE data are anonymised for users and usual practices regarding statistical disclosure control were applied.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
None declared.
References
- 1.World Health Organization (WHO) 2020. Timeline: WHO's COVID-19 response.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline [Google Scholar]
- 2.Zheng J. SARS-CoV-2: an emerging coronavirus that causes a global threat. Int J Biol Sci. 2020;16(10):1678–1685. doi: 10.7150/ijbs.45053. Published 2020 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) 2020. Coronavirus disease (COVID-19) pandemic; Numbers at a glance.https://covid19.who.int/ [Google Scholar]
- 4.RTE . 2020. First case of Covid-19 diagnosed in east of Ireland.https://www.rte.ie/news/coronavirus/2020/0229/1119357-coronavirus-ireland/ [Google Scholar]
- 5.European Centre for Disease Prevention and Control (ECDC) 2020. Risk assessment on COVID-19, 4 December 2020.https://www.ecdc.europa.eu/en/current-risk-assessment-novel-coronavirus-situation [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.RTE . 2020. Timeline: six months of Covid-19.https://www.rte.ie/news/newslens/2020/0701/1150824-coronavirus/ [Google Scholar]
- 7.Flaxman S., Mishra S., Gandy A., Unwin H., Mellan T., Coupland H. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 8.Davies N.G., Kucharski A.J., Eggo R.M., Gimma A., Edmunds W.J., Jombart T. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Heal. 2020;5(7):e375–e385. doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Protection Surveillance Centre . 2020. Epidemiology of COVID-19 in Ireland.https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/casesinireland/epidemiologyofcovid-19inireland/september2020/COVID-19_Daily_epidemiology_report_(NPHET)_20200928 - Website.pdf [Google Scholar]
- 10.Government of Ireland . 2020. Ireland placed on level 5 of the plan for living with COVID-19.https://www.gov.ie/en/press-release/66269-ireland-placed-on-level-5-of-the-plan-for-living-with-covid/ [Google Scholar]
- 11.Government of Ireland . 2020. Report on social implications of COVID-19 in Ireland; preliminary assessment.https://assets.gov.ie/74373/5cc1bbfe59b447d3b841fa43cecfc79d.pdf [Google Scholar]
- 12.Economic and Social Research Institute . 2020. The environmental and economic impacts of the COVID-19 crisis on the Irish economy.https://www.esri.ie/system/files/publications/RS106_2.pdf [Google Scholar]
- 13.The Irish Times . 2020. Draconian’ restrictions around Covid-19 condemned by HSE doctor.https://www.irishtimes.com/news/health/draconian-restrictions-around-covid-19-condemned-by-hse-doctor-1.4352701 [Google Scholar]
- 14.World Health Organization (WHO) 2020. Managing the COVID-19 infodemic: promoting healthy behaviours and mitigating the harm from misinformation and disinformation.https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation [Google Scholar]
- 15.The Lancet The truth is out there, somewhere. Lancet. 2020;396(10247):291. doi: 10.1016/S0140-6736(20)31678-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Lancet Infectious Diseases The COVID-19 infodemic. Lancet Infect Dis. 2020;20(8):875. doi: 10.1016/S1473-3099(20)30565-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. How to fight an infodemic: the four pillars of infodemic management. J Med Internet Res. 2020;22(6) doi: 10.2196/21820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burn E., You S.C., Sena A.G., Kostka K., Abedtash H., Abrahao M.T.F. An international characterisation of patients hospitalised with COVID-19 and a comparison with those previously hospitalised with influenza. medRxiv. 2020 doi: 10.1101/2020.04.22.20074336. 2020.04.22.20074336. [DOI] [Google Scholar]
- 19.Pormohammad A., Ghorbani S., Khatami A., Razizadeh M.H., Alborzi E., Zarei M. Comparison of influenza type A and B with COVID-19: a global systematic review and meta-analysis on clinical, laboratory and radiographic findings. Rev Med Virol. 2020:e2179. doi: 10.1002/rmv.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO) 2017. Pandemic Influenza Severity Assessment (PISA): a WHO guide to assess the severity of influenza epidemics and pandemics.https://apps.who.int/iris/bitstream/handle/10665/259392/WHO-WHE-IHM-GIP-2017.2-eng.pdf?sequence=1 [Google Scholar]
- 21.Healthcare Pricing Office . 2016. Hospital in patient Enquiry instruction manual.http://www.hpo.ie/hipe/hipe_instruction_manual/HIPE_Instruction_Manual_1.1.2016.pdf [Google Scholar]
- 22.Health Protection Surveillance Centre . 2020. Epidemiology of COVID-19 in Ireland.https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/casesinireland/epidemiologyofcovid-19inireland/july2020/COVID-19_Daily_epidemiology_report_(NPHET)_31072020%20-%20Website.pdf [Google Scholar]
- 23.Health Protection Surveillance Centre . 2020. Annual Epidemiological Report; Influenza and other seasonal respiratory viruses in Ireland, 2017/2018.https://www.hpsc.ie/a-z/respiratory/influenza/seasonalinfluenza/surveillance/influenzasurveillancereports/seasonsummaries/Influenza%202017-2018%20Annual%20Summary_Final.pdf [Google Scholar]
- 24.Health Protection Surveillance Centre . 2020. Annual Epidemiological Report; Influenza and other seasonal respiratory viruses in Ireland, 2018/2019.https://www.hpsc.ie/a-z/respiratory/influenza/seasonalinfluenza/surveillance/influenzasurveillancereports/seasonsummaries/Influenza%202018-2019%20Season_Summary.pdf [Google Scholar]
- 25.Lewis G., Sheringham J., Lopez Bernal J., Crayford T. 2nd ed. CRC Press; Florida: 2017. Mastering public health; p. 650. [Google Scholar]
- 26.Auvinen R., Nohynek H., Syrjänen R., Ollgren J., Kerttula T., Mantyla J. Comparison of the clinical characteristics and outcomes of hospitalized adult COVID-19 and influenza patients - a prospective observational study. Infect Dis. 2020:1–11. doi: 10.1080/23744235.2020.1840623. (Lond) [DOI] [PubMed] [Google Scholar]
- 27.Cobb N.L., Sathe N.A., Duan K.I., Seitz K.P., Thau M.R., Sung C.C. Comparison of clinical features and outcomes in critically Ill patients hospitalized with COVID-19 versus influenza. Ann Am Thorac Soc. 2020 doi: 10.1513/AnnalsATS.202007-805OC. doi:10.1513/AnnalsATS.202007-805OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moloney E.D., Smith D., Bennett K., O'Riordan D., Silke B. Do consultants differ? Inferences drawn from hospital in-patient enquiry (HIPE) discharge coding at an Irish teaching hospital. Postgrad Med J. 2005;81(955):327–332. doi: 10.1136/pgmj.2004.026245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health Service Executive . 2020. Influenza surveillance in Ireland- weekly report; week 49 2020 (30th November-6th December 2020)https://www.hpsc.ie/a-z/respiratory/influenza/seasonalinfluenza/surveillance/influenzasurveillancereports/20202021season/Influenza_Surveillance_Report_Week%2049%202020_Finalv1.0_10122020.pdf [Google Scholar]
- 30.World Health Organization (WHO). Fifty-sixth World Health Assembly: Prevention and control of influenza pandemics and annual epidemics. Available at: https://www.who.int/immunization/sage/1_WHA56_19_Prevention_and_control_of_influenza_pandemics.pdf. [Accessed on 27 January 2021].
- 31.Health Protection Surveillance Centre. Seasonal influenza vaccine uptake (provisional) in older people in Ireland, September 2019-May 2020. Available at: https://www.hpsc.ie/a-z/respiratory/influenza/seasonalinfluenza/influenzaandadults65yearsandolder/Seasonal%20Flu%20Vacc%20Uptake_65%20report_Sep%202019%20May%202020%20provisional%20for%20website.pdf. [Accessed 27 January 2021].
- 32.Rossiter A., O'Morain N.R., Varghese C., Lane S. Seasonal influenza vaccine uptake in a respiratory outpatients clinic. Ir Med J. 2017 Feb 10;110(2):517. PMID: 28657262. [PubMed] [Google Scholar]
- 33.Chaintarli K., Barrassa A., Cotter S., Mereckiene J., O'Donnell J., Domegan L. Decrease in the uptake of seasonal influenza vaccine in persons aged 65 Years and older in Ireland since the 2009 influenza A (H1N1) Pdm09 pandemic. Ir Med J. 2017 Oct 10;110(9):630. PMID: 29372945. [PubMed] [Google Scholar]
- 34.Irish Statute Book . 2020. Health Act 2004.http://www.irishstatutebook.ie/eli/2004/act/42/section/7/enacted/en/html#sec7 [Google Scholar]