Abstract

Peripancreatic lymph node tuberculosis is a rare disease. Correct diagnosis is a challenge, and endoscopic ultrasound and fine‐needle aspiration biopsy (FNB) allow rapid diagnosis with high precision. In this report, we present a 45‐year‐old female patient with abdominal pain and the presence of peripancreatic adenopathy who underwent FNB, which diagnosed peripancreatic lymph node tuberculosis.
Introduction
Tuberculosis continues to be a significant health problem with the World Health Organization estimates of 10 million new cases and 1.45 million deaths in 2018. 1 , 2 , 3 In humans, there are many factors associated with the development of infection; some of them are related to intrinsic conditions of the patient, and others are related to the environment in which they are immersed. 2 , 4
The majority of clinical cases are asymptomatic, called latent tuberculosis infection (LTBI); a smaller subset of infected individuals presents with symptomatic or active tuberculosis (TB). Mycobacterium mainly affects the lungs, causing pulmonary tuberculosis in the symptomatic cases, but it can also affect the intestine, meninges, bones, joints, lymph nodes, skin, and other tissues, causing extrapulmonary tuberculosis, which represents up to 20% of all tuberculosis cases; 10% of these extrapulmonary cases are abdominal tuberculosis. 2 , 5 , 6 , 7 Peripancreatic lymph node tuberculosis, for example, constitutes a diagnostic challenge because it is a pathology with nonspecific symptoms. The main clinical presentation is abdominal pain, pancreatitis in some cases, and biliary obstruction associated with the presence of a peripancreatic mass. For diagnostic confirmation, both histopathological study and microbiological isolation are required.
Endoscopic ultrasound (EUS) is a minimally invasive and safe technique, which allows us to study pancreatic pathologies with high precision; this varies between 82 and 90%, with a low rate of complications. It results in images of high resolution and permits fine‐needle aspiration biopsy (FNB). This brief clinical case aims to show how the diagnosis of peripancreatic lymph node tuberculosis was reached in a patient without known TB who presented with symptoms suggestive of other pathologies.
Case report
A 45‐year‐old female patient, with no relevant clinic history, had 15 days of abdominal pain in the right upper quadrant, and abdominal ultrasound was performed to rule out cholelithiasis; instead, a peripancreatic adenopathy was observed, confirmed by abdominal computed tomography (CT) (Fig. 1, CT scan.tiff) and magnetic resonance (MRI) (Fig. 2, MRI.tiff). She was then referred to the gastroenterologist to undergo an EUS and rule out pancreatic tumor.
Figure 1.

Abdominal computed tomography scan shows a lesion with solid characteristics, located at the peripancreatic level adjacent to the head of the pancreas.
Figure 2.
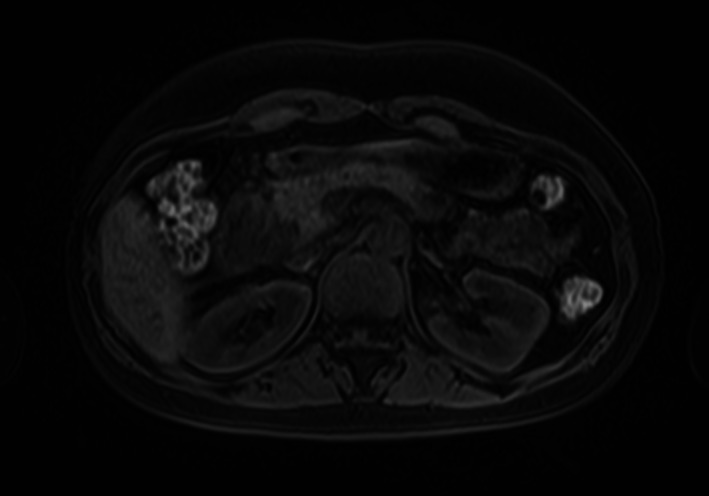
Abdominal magnetic resonance imaging shows a solid lesion located at the peripancreatic level adjacent to the head of the pancreas.
The EUS (Fig. 3, EUS.tiff) showed a normal pancreatic parenchyma and a 38x20‐mm hypoechoic, heterogeneous adenopathy, with a hyperechoic center, located in the peripancreatic region close to the pancreatic head, with a green elastography pattern suggestive of an inflammatory and benign adenopathy. EUS‐guided FNB using the new 20G ProCore needle through the duodenal bulb was performed using fanning technique and suction. Two passes were made without complications, and pathology analysis found extensive chronic granulomatous inflammation with geographic necrosis; the culture was positive for rifampicin‐resistant Mycobacterium tuberculosis.
Figure 3.

Endoscopic ultrasound image shows a hypoechoic, heterogeneous lesion with a hyperechoic center peripancreatic lymph node, with green heterogenous elastography pattern.
We confirm that informed consent was obtained from the patient for the publication of her information and imaging.
Discussion
Classic tuberculosis infection usually affects the lung, and the clinical presentation is clear with specific symptoms. In the case of abdominal tuberculosis, it is not so clear because it is a rare disease, it is not always associated with active pulmonary tuberculosis, the clinical presentation is unusual, it occurs mainly in immunocompromised patients, and it can be confused with other entities. Even with advanced imaging techniques, the diagnosis may still be unclear. 5
Abdominal tuberculosis primarily affects solid organs such as the liver and spleen, and can even affect the distal ileum, peritoneum, and lymph nodes. Otherwise, pancreatic and peripancreatic tuberculosis are rare pathologies, which have a reported incidence of less than 4.7%. 6 , 7
Peripancreatic lymph node tuberculosis is a diagnostic challenge as it is a pathology with unspecified symptoms whose main clinical presentation is abdominal pain and biliary obstruction associated with the presence of a pancreatic or peripancreatic mass and, rarely, pancreatitis. Given the rarity of this pathology, pancreatic neoplasia is often misdiagnosed, and these patients can undergo surgery with significant morbidity and mortality. 8
On imaging, pancreatic tuberculosis most often presents as a solid or cystic lesion. Abdominal CT shows the presence of a low‐density mass with ring enhancement, which is considered a characteristic finding. T1‐weighted fat‐suppressed MRI shows hypointense pancreatic TB lesions, while T2‐weighted images show heterogeneous signal intensities. With FDG PET‐CT images, it is difficult to distinguish tuberculous lymphadenitis from pancreatic malignancy because both conditions can result in increased fluorodeoxyglucose (FDG)‐positron emission tomography uptake. 9 , 10
In the case presented, EUS was performed, demonstrating a peripancreatic lesion with normal pancreatic tissue, ruling out pancreatic neoplasic lesions. Adequate tissue for histology and culture was obtained through FNB. Therefore, it is important to highlight that, in the study of pancreatic and peripancreatic tuberculosis, fine needle aspiration allows the presence of necrotizing granulomas to be demonstrated, with a sensitivity of approximately 76% with a low rate of complications. With the advent of new and better‐quality biopsy needles that allow us to obtain a greater quantity of tissue, called FNB needles, the performance and diagnostic precision have increased significantly, reaching 82–90% in the different studies. 11
Author contribution
Renzo Pinto Carta contributed to planning and conducting the case, performed the collection process and interpreted data, and drafted the manuscript. He has approved the final draft submitted. Fernando Sierra‐Arango contributed to planning and conducting the case, collecting and interpreting data, and drafting the manuscript. He has approved the final draft submitted. Mariana Vásquez‐Roldan contributed to collecting data and drafting the manuscript. She has approved the final draft submitted. Erika D Pérez‐Riveros contributed to collecting data and drafting the manuscript. She has approved the final draft submitted.
Declaration of conflict of interest: None.
Guarantor of the article: Fernando Sierra‐Arango.
References
- 1. Khan MK, Islam MN, Ferdous J, Alam MM. An overview on epidemiology of tuberculosis. Mymensingh Med. J. 2019; 28: 259–266. [PubMed] [Google Scholar]
- 2. Ankrah AO, Glaudemans AWJM, Maes A et al. Tuberculosis. Semin. Nucl. Med. 2018; 48: 108–130. [DOI] [PubMed] [Google Scholar]
- 3. Ndege R, Ngome O, Bani F et al. Ultrasound in managing extrapulmonary tuberculosis: a randomized controlled two‐center study. BMC Infect. Dis. 2020; 20: 349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Narasimhan P, Wood J, Macintyre CR, Mathai D. Risk factors for tuberculosis. Pulm. Med. 2013; 2013: 828939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abu‐Zidan FM, Sheek‐Hussein M. Diagnosis of abdominal tuberculosis: lessons learned over 30years: pectoral assay. World J. Emerg. Surg. 2019; 14: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yamada R, Inoue H, Yoshizawa N et al. Peripancreatic tuberculous lymphadenitis with biliary obstruction diagnosed by endoscopic ultrasound‐guided fine‐needle aspiration biopsy. Intern. Med. 2016; 55: 919–923. [DOI] [PubMed] [Google Scholar]
- 7. Kim J‐B, Lee SS, Kim S‐H et al. Peripancreatic tuberculous lymphadenopathy masquerading as pancreatic malignancy: a single‐center experience: Peripancreatic tuberculosis. J. Gastroenterol. Hepatol. 2014; 29: 409–416. [DOI] [PubMed] [Google Scholar]
- 8. Ray S, Das K, Mridha AR. Pancreatic and peripancreatic nodal tuberculosis in immunocompetent patients: report of three cases. J. Pancreas. 2012; 13: 667–670. [DOI] [PubMed] [Google Scholar]
- 9. De Backer AI, Mortelé KJ, Bomans P, De Keulenaer BL, Vanschoubroeck IJ, Kockx MM. Tuberculosis of the pancreas: MRI features. Am. J. Roentgenol. 2005; 184: 50–54. [DOI] [PubMed] [Google Scholar]
- 10. Obama K, Kanai M, Taki Y, Nakamoto Y, Takabayashi A. Tuberculous lymphadenitis as a cause of obstructive jaundice: report of a case. Surg. Today. 2003; 33: 229–231. [DOI] [PubMed] [Google Scholar]
- 11. Song TJ, Lee SS, Park DH et al. Yield of EUS‐guided FNA on the diagnosis of pancreatic/peripancreatic tuberculosis. Gastrointest. Endosc. 2009; 69(3 Pt 1): 484–491. [DOI] [PubMed] [Google Scholar]


