Abstract
Reinfection with SARS-CoV-2 is a rare phenomenon. To date, there has been some cases reported from countries such as United States, Ecuador, Hong Kong, the Netherlands and Belgium. This case report presents the first case of reinfection from Saudi Arabia, and probably the first dental student to have been re-infected with COVID-19. A 24-year-old male dental student presents with reinfection after a period of three months since he was first infected with COVID-19. The signs and symptoms reported by the patient were similar in both instances, except that he developed fever only at the time of reinfection. The infection and reinfection were confirmed with a RT-PCR test reports. This report highlights how it is necessary to continue to observe all the prescriptions recently indicated in the literature in order to avoid new contagion for all health workers after healed from covid-19 or asymptomatic positive, since as seen sometimes the infection does not ensures complete immunity in 100% of cases.
Keywords: Coronavirus, Reinfection, Case-report, COVID-19, SARS-CoV-2, Dental healthcare worker
Introduction
SARS-CoV-2 outbreak since the December of 2019 has continued to exhibit devastating consequences, and was declared as pandemic by the World Health Organization in the early 2020. In Saudi Arabia, clusters of healthcare workers positive for COVID-19 have been identified in hospital settings and long-term care facilities, but till date no clusters have yet been reported in dental settings or personnel [1].
Although, millions of cases have been reported worldwide, reinfection of SARS-CoV-2 is considered a rare phenomenon from the first case reported at Hong Kong in august 2020 [2]. There is no report of reinfection from Saudi Arabia and this is first case of reinfection in an arabian dental student.
Case report
First incidence of infection
A 24-year-old male dental student at Jazan University, Saudi Arabia reported a contact with an infected COVID-19 family member on the 10th of June 2020. A nasopharyngeal swab test was performed on the dental student and the real time polymerase chain reaction test (RT-PCR) confirmed the infection on the 11th of June 2020. However, the student reported symptoms only after the third day. The symptoms were consistent to the SARS-CoV-2 infection, comprise sore throat, cough, headache, nausea, diarrhea, loss of taste and smell, insomnia, loss of appetite, and fatigue. The patient had no history of underlying diseases including physical and psychological conditions. However, during the first few days of self-isolation the patient reported fear and anxiety, increased insomnia, and increased body ache. No chest radiography was advised to the patient at the primary healthcare center, as there was no complains of breathlessness. The symptoms gradually subsided after the tenth day, and the patient carried out another swab test at the end of the 14th day of self-isolation which was negative.
Incidence of reinfection
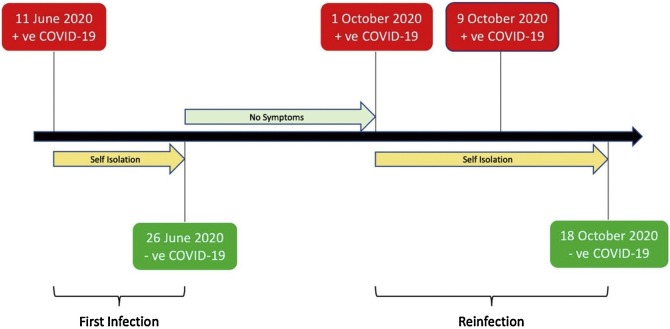
The dental student contacted the Infection Control (IC) unit, School of Dentistry on the 30th September 2020 (three days after the contact with an infected COVID-19 case), about three months after recovering from his first infection (Fig. 1 ).
Fig. 1.
Timeline of events during the first infection and reinfection.
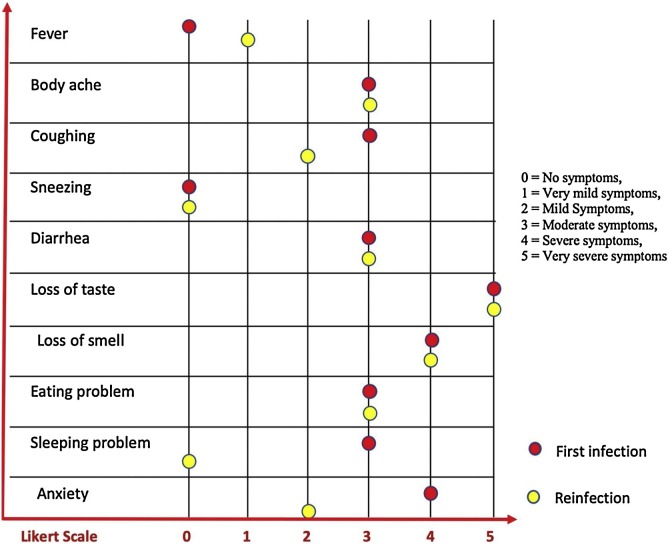
The IC unit performed the nasopharyngeal test for a confirmation, and requested him not to attend the college. During the history taking, he reported a close contact with another relative with confirmed COVID-19. The signs and symptoms reported by the patient were similar to the first instance, except that he developed fever with no loss of appetite and sleep. The patient was asked to rate his symptoms in both instances on a Likert scale adapted from the one used by the from American College of Emergency Physicians (ACEP) to compare the severity of symptoms between the first infection and the reinfection (Fig. 2 ).
Fig. 2.
Comparing the severity of symptoms between the first infection and reinfection.
No medications were taken by the student at the time of infection and the reinfection. The doctor at the Ministry of Health (MoH), Saudi Arabia did not advise for any blood tests. The infection and reinfection reports were registered in the MoH database. In this case the genome sequencing reports were not available for comparisons.
The MoH, Saudi Arabia had strictly advised not to allow any healthcare worker, including students to carry out their work or education at the universities if they have come in contact with a suspected case (specific definition of contact is mentioned in the MoH website: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/MOH-Guidelines-for-re-opening-June-.pdf). These protocols were strictly followed at the premises. Therefore, the student prior to symptoms followed the protocols to prevent transmission of infection, once the symptoms appeared he stopped seeing the patients and rejoined the university only after a confirmed negative report from the doctor at MoH. There were no cases of cross-infection reported at the site during that particular period.
Discussion
A distinction must be made between prolonged shedding/reactivation and true reinfection [3], in fact one of the features of SARS-CoV-2 infection is prolonged virus shedding. Several studies reported persistent or recurrent elimination of viral RNA in nasopharyngeal samples starting from first contact with a positive subject [[4], [5], [6]]. For this reason, recently the Center for Disease Control and Prevention (CDC) released a guidance protocol designed to identify cases of real SARS-CoV-2 re-infection [7]. This guidance defines some criteria about sequencing parameters, epidemiological data and laboratory diagnostic data. Specifically, investigative criteria include a positive RT-PCR test more than 90 days after the initial test or a positive RT-PCR test more than 45 after the initial test that is accompanied by compatible symptoms or epidemiological exposure, such as in this case.
This study presents the first incidence of reinfection from Saudi Arabia, and possibly the first dental student globally to have been re-infected with COVID-19. The symptoms were similar to the earlier reported reinfection cases, such as that from Hong Kong [2]. The Likert scale indicated that the symptoms were slightly less severe in the second instance, and the patient was less anxious and slept well. The patient did not experience shortness of breath in both the instances. Coughing, body ache, loss of taste and smell, and diarrhea were the symptoms at the first- and second-time infection, and also to the earlier case reports [2,[8], [9], [10]]. Other noticeable difference was that the patient had reported fever only at the time of reinfection.
A recent review of the literature [11] analyzed 16 reported cases of reinfection confirmed by sequencing, 10 of which were in pre-print [2,10,[12], [13], [14], [15], [16], [17], [18]]. Among the 16 described cases, the median duration between the first and second infection was 66 with a range of 19–142 days [11]. The severity of the reinfection episode itself was asymptomatic/mild in 12 cases (75%) and moderate/severe in 4 cases (25%) [11]. Among the 12 cases in which symptomatology could be compared across episodes, 6 had less severe disease during the second infection [11]. If the second time the symptoms are generally reduced, as in the Hong Kong [2], Belgium and the Netherlands [10] patients, this suggests that the immune system is responding as it should. But if symptoms are consistently more severe during a second COVID-19 attack, as in the cases of Nevada [12] or Ecuador [16], there could be some possible causes, even if the mechanisms that could account for a more severe secondary infection can only be speculated. Firstly, a very high dose of virus might have led to the second instance of infection and induced more severe disease [19]. Secondly, it is possible that reinfection was caused by a more virulent variant of the virus, or more virulent in the patient context [12]. At last, antibody-dependent enhancement (ADE) may be considered as an additional pathway which may lead to an increase of patient' symptoms in case of reinfection. This mechanism has been already reported to occur in several in-vitro models of infection [20], although there is still lack of evidence [21]. While ADE has been descripted in MERS and SARS, further studies are needed to assess its role in SARS-Cov-2 infection.
It is to note that our patient had no underlying medical illnesses prior to the infection and reinfection instances, therefore reducing the likelihood of known loss of immunity.
An important question raised by these cases is: SARS-COV-2 can re-infect a patient after recovery and why? Because the cases of reinfection have only been reported by a few earlier studies, there are less facts and more assumptions. However, according to our knowledge the possibility of the patient being in continuous infection involving deactivation and reactivation is less, as assumed by the experts in earlier studies [8]. This is because of the two positive and two negative PCR test reports along with three symptomless months.
Another possibility is the infection of the patient with two different specimens/strands of SARS-CoV-2. Among 16 published reinfection cases, 5 (31%) had a different clade or lineage detected between initial infection and reinfection [11]. Eight (50%) were infected with the same clade but had >2 substitutions/month difference between them, compatible with CDC criteria [11]. Three cases (19%) had low quality genome sequences but were found to harbor different D614G alleles between the initial and reinfection strains, and therefore were considered to represent reinfection [11]. Given the challenge of detecting reinfection by closely-related viruses, it is important to conduct further studies characterizing the within-host evolution of SARS-CoV-2, to better understand the diversity expected over time [11]. This could have only been proven upon genome sequencing which was not carried out in the current study due to lack of resources.
Another major limitation of the current study is that the immune response of the patient was not carried out. In fact, immune response or its duration can be one of the possible causes for viral reinfection [22]. Recent findings suggested that protective immunity does not occur in all infected individuals [23], supporting the possibility of reinfection [24], even if 93% of the infected produce neutralizing antibodies [25]. Seroconversion of IgM and IgG antibodies occur the first week after onset of symptoms, seroconversion rates rise until the fourth week and decline thereafter, by the seventh week IgM antibodies are not detected in most cases, whereas IgG antibodies persist longer for a period of time yet unknown [26]. Immunoglobulins alone are not truly sufficient to confer long-term immunity to coronavirus [22].
The interval between the 2 incidences of infection in the same subject reported in literature suggests ample time for the development of neutralizing antibodies [27] and cellular immune responses [28]. 10/16 cases reported results of serology testing at the time of the second infection, 6 of which had a positive total immunoglobulin (Ig) or IgG result [11]. None of the patients had a known immunodeficient state. Beyond assessing IgG levels, very little examination of these patients’ immune response has been performed. In one case, neutralizing antibody levels were measured at time of the second infection, and were comparable to those observed after boosted vaccination [15]. Further investigation of immune parameters in patients who experience reinfection is critical to understanding its implications for the future of the pandemic [29].
For all these reasons it is important to identify cases of reinfection to understand if the “immunological memory” affects the symptoms during a second infection, a crucial fact, in particular, to predict the effectiveness of the vaccination campaign.
Conclusion
The current study indicates the first case of reinfection in Saudi Arabia. The genetic analysis of all the new cases reported as re-infection would help in understanding if the reinfection would be due to a new infection by a different SARS-CoV-2 or a reinfection by the same virus for a decline of immune response, but unfortunately genomic analysis is not available for some of these cases. These data could be useful and contribute towards the role of vaccination in response to the COVID-19 infections. This report highlights how it is necessary to continue to observe all the prescriptions recently indicated in the literature [[30], [31], [32]] in order to avoid new contagion for all health workers after healed from covid-19 or asymptomatic positive, since as seen sometimes the infection does not ensure complete immunity in 100% of cases and the necessity of vaccination for all subjects with or without a prior infection depending on their antibody titer.
Funding
The current case report is self-funded and has not received funds from any external organizations.
Competing interests
None declared.
Ethical approval
Not required.
Author contributions
All authors contributed equally in conceptualizing, carrying out, and drafting the research.
Acknowledgements
The authors would like to thank the dental student (name confidential) for his willingness to participate and also for providing the consent. A prior permission from the Institutional Review Board at Jazan University and a signed consent from the study participant precedes the data collection and interview for the current case report.
References
- 1.Ministry of Health M . 2020. Media center. Saudi Arabia. [Google Scholar]
- 2.To K.K., Hung I.F., Ip J.D., Chu A.W., Chan W.M., Tam A.R., et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020;71 doi: 10.1093/cid/ciaa1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falahi S., Kenarkoohi A. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes New Infect. 2020;38 doi: 10.1016/j.nmni.2020.100812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xiao A.T., Tong Y.X., Gao C., Zhu L., Zhang Y.J., Zhang S. Dynamic profile of RT-PCR findings from 301 COVID-19 patients in Wuhan, China: a descriptive study. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lan L., Xu D., Ye G., Xia C., Wang S., Li Y., et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323:1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gombar S., Chang M., Hogan C.A., Zehnder J., Boyd S., Pinsky B.A., et al. Persistent detection of SARS-CoV-2 RNA in patients and healthcare workers with COVID-19. J Clin Virol. 2020;129 doi: 10.1016/j.jcv.2020.104477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prevention C.f.D.C.a . 2020. Common Investigation Protocol for Investigating Suspected SARS-CoV-2 Reinfection. [cited 30 December 2020] [Google Scholar]
- 8.Tillett R., Sevinsky J., Hartley P., Kerwin H., Crawford N., Gorzalski A., et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet. 2020;2020 doi: 10.1016/S1473-3099(20)30764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prado-Vivar B., Becerra-Wong M., Guadalupe J.J., Marquez S., Gutierrez B., Rojas-Silva P., et al. Covid-19 re-infection by a phylogenetically distinct SARS-CoV-2 variant, first confirmed event in South America. SSRN Electron J. 2020;20 doi: 10.2139/ssrn.3686174. [DOI] [Google Scholar]
- 10.Van Elslande J., Vermeersch P., Vandervoort K., Wawina-Bokalanga T., Vanmechelen B., Wollants E., et al. Symptomatic SARS-CoV-2 reinfection by a phylogenetically distinct strain. Clin Infect Dis. 2020;71 doi: 10.1093/cid/ciaa1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Babiker A., Marvil C., Waggoner J.J., Collins M., Piantadosi A. The importance and challenges of identifying SARS-CoV-2 reinfections. J Clin Microbiol. 2020;58 doi: 10.1128/JCM.02769-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tillett R.L., Sevinsky J.R., Hartley P.D., Kerwin H., Crawford N., Gorzalski A., et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis. 2021;21:52–58. doi: 10.1016/S1473-3099(20)30764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta V., Bhoyar R.C., Jain A., Srivastava S., Upadhayay R., Imran M., et al. Asymptomatic reinfection in two healthcare workers from India with genetically distinct SARS-CoV-2. Clin Infect Dis. 2020;71 doi: 10.1093/cid/ciaa1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larson D., Brodniak S.L., Voegtly L.J., Cer R.Z., Glang L.A., Malagon F.J., et al. A case of early re-infection with SARS-CoV-2. Clin Infect Dis. 2020;71 doi: 10.1093/cid/ciaa1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldman J.D., Wang K., Roltgen K., Nielsen S.C.A., Roach J.C., Naccache S.N., et al. Reinfection with SARS-CoV-2 and failure of humoral immunity: a case report. medRxiv. 2020 doi: 10.1101/2020.09.22.20192443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prado-Vivar B., Becerra-Wong M., Guadalupe J.J., Marquez S., Gutierrez B., Rojas-Silva P., et al. A case of SARS-CoV-2 reinfection in Ecuador. Lancet Infect Dis. 2020;20 doi: 10.1016/S1473-3099(20)30910-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shastri J., Parikh S., Agarwal S. Whole genome sequencing confirmed SARS-CoV -2 reinfections among healthcare workers in India with increased severity in the second episode. Preprint SSRN. 2020 doi: 10.2139/ssrn.3688220. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3688220 [DOI] [Google Scholar]
- 18.Abu-Raddad L.J., Chemaitelly H., Malek J.A., Ahmed A.A., Mohamoud Y.A., Younuskunju S., et al. Assessment of the risk of SARS-CoV-2 reinfection in an intense re-exposure setting. Clin Infect Dis. 2020;71 doi: 10.1093/cid/ciaa1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guallar M.P., Meirino R., Donat-Vargas C., Corral O., Jouve N., Soriano V. Inoculum at the time of SARS-CoV-2 exposure and risk of disease severity. Int J Infect Dis. 2020;97:290–292. doi: 10.1016/j.ijid.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee W.S., Wheatley A.K., Kent S.J., DeKosky B.J. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat Microbiol. 2020;5:1185–1191. doi: 10.1038/s41564-020-00789-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arvin A.M., Fink K., Schmid M.A., Cathcart A., Spreafico R., Havenar-Daughton C., et al. A perspective on potential antibody-dependent enhancement of SARS-CoV-2. Nature. 2020;584:353–363. doi: 10.1038/s41586-020-2538-8. [DOI] [PubMed] [Google Scholar]
- 22.Chaturvedi R., Naidu R., Sheth S., Chakravarthy K. Efficacy of serology testing in predicting reinfection in patients with SARS-CoV-2. Disaster Med Public Health Prep. 2020:1–3. doi: 10.1017/dmp.2020.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao J., Yuan Q., Wang H., Liu W., Liao X., Su Y., et al. Antibody responses to SARS-CoV-2 in patients with novel coronavirus disease 2019. Clin Infect Dis. 2020;71:2027–2034. doi: 10.1093/cid/ciaa344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Munoz Mendoza J., Alcaide M.L. COVID-19 in a patient with end-stage renal disease on chronic in-center hemodialysis after evidence of SARS-CoV-2 IgG antibodies. Reinfection or inaccuracy of antibody testing. IDCases. 2020;22 doi: 10.1016/j.idcr.2020.e00943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Del Fante C., Franchini M., Baldanti F., Percivalle E., Glingani C., Marano G., et al. A retrospective study assessing the characteristics of COVID-19 convalescent plasma donors and donations. Transfusion. 2020;60 doi: 10.1111/trf.16208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sethuraman N., Jeremiah S.S., Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020;323:2249–2251. doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 27.Suthar M.S., Zimmerman M., Kauffman R., Mantus G., Linderman S., Vanderheiden A., et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. medRxiv. 2020;1(3) doi: 10.1101/2020.05.03.20084442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dan J.M., Mateus J., Kato Y., Hastie K.M., Yu E.D., Faliti C.E., et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;370 doi: 10.1126/science.abf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Overbaugh J. Understanding protection from SARS-CoV-2 by studying reinfection. Nat Med. 2020;26:1680–1681. doi: 10.1038/s41591-020-1121-z. [DOI] [PubMed] [Google Scholar]
- 30.Bizzoca M.E., Campisi G., Lo Muzio L. An innovative risk-scoring system of dental procedures and safety protocols in the COVID-19 era. BMC Oral Health. 2020;20:301. doi: 10.1186/s12903-020-01301-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bizzoca M.E., Campisi G., Lo Muzio L. Covid-19 pandemic: what changes for dentists and oral medicine experts? A narrative review and novel approaches to infection containment. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17113793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Campisi G., Bazzano M., Mauceri R., Panzarella V., Di Fede O., Bizzoca M.E., et al. The patient-doctor relationship: new insights in light of the current Ministerial recommendations regarding phase 2 of the COVID-19 pandemic. Minerva Stomatol. 2020;69:251–255. doi: 10.23736/S0026-4970.20.04396-4. [DOI] [PubMed] [Google Scholar]