Abstract
Objective
Acute aortic thrombosis and floating aortailiac thrombus are infrequent clinical conditions with high morbidity and mortality rates. It was observed that; SARS-CoV-2 coronavirus disease (Covid-19) caused a hyperinflammation and hyperimmune state and these conditions can result in a hypercoagulation and eventually thrombotic events might occur.
Methods
Here we presented two covid-19 positive patients with rare aortic thrombotic events.
Results
Two patients underwent emergent diagnostic tests including computerized tomographic angiography. Total aortic thrombosis just below the renal arising point was evaluated in one patient, and aortic floating thrombus was evaluated in other patient. But despite initial medical therapies, the clinical conditions of the cases worsened and both patients died while on medical therapy before planned surgical intervention applied.
Conclusions
Covid-19 is not only the disease of lungs and inflammatory system also the disease of coagulation and vascular system. Aortic thrombosis is rare and must be kept in mind in Covid-19 patients with peripheral circulation impairment.
Keywords: Aortic Thrombus, Covid-19, Hypercoagulability
INTRODUCTION
Coronavirus disease 2019 (Covid-19) is a viral respiratory illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2), which was first described in Wuhan, China, and later declared by the World Health Organization as pandemic.1 Acute respiratory distress syndrome (ARDS) is the main complication in patients with severe disease, but other complications, including thromboembolic events, have also been described.2 , 3 Covid-19 may predispose patients to an increased risk of thrombotic complications through various pathophysiological mechanisms, such as inflammation, immobilization, hypoxia, endothelial dysfunction, and a hypercoagulable state.3 Covid-19 could predispose to both venous and arterial thrombotic events, especially in mild and severe patients.4 Currently, a large number of publications report many Covid-19 positive patients have been diagnosed with pulmonary embolism (PTE); however, there are few publications on cases with arterial thrombosis.5 There are limited cases reported as acute total aortic occlusion and floating aortic thrombus seen in patients with Covid-19.
Here we present two cases diagnosed as Covid-19, one with acute total aortic occlusion of abdominal aorta and the other with floating aortic thrombus. Informed consent was obtained from the relatives of both patients.
MATERIAL-METHOD
Case 1
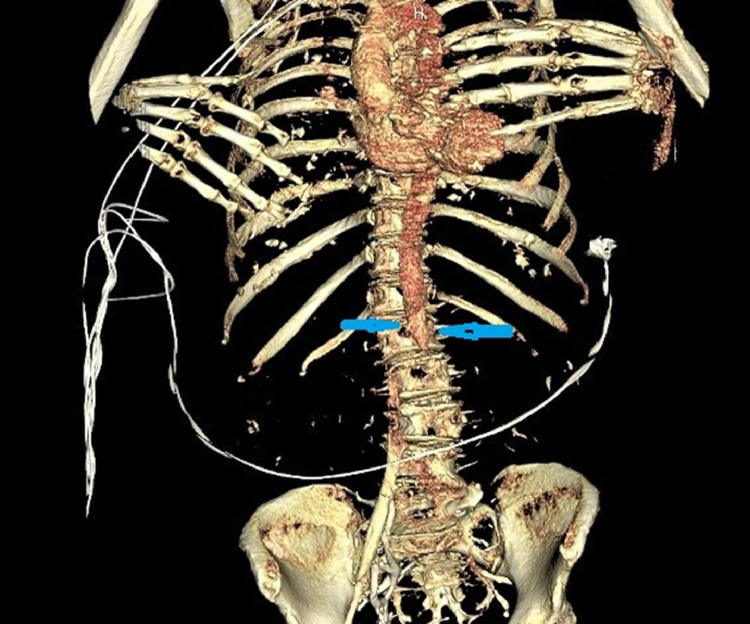
A 74-years-old woman with the symptoms of fatigue, cough, abdominal and bilateral leg pain was admitted to the emergency service. Clinical examination was normal, apart from a core temperature of 37.9 °C. She was diagnosed with Covid-19 by thorax computed tomography (CT) and reverse transcription polymerase chain reaction (PCR) test. She had a normal abdominal CT angiography performed in June 2020. Patient was taken to intensive care unit (ICU), antibiotherapy, low molecular weight heparin (LMWH), asetilsalisilic acid (ASA) therapy started. For the persistent pain on her both legs, cardiovascular surgery consultation asked from our clinic. On physical examination; both legs were pale but non cyanotic, no palpable pulses on both legs from femoral to dorsalis pedis and also no pulses diagnosed with hand Doppler. Emergent abdominal and lower extremity CT angiography performed. Total aortailiac thrombosis starting just below from the renal artery arising point was evaluated (Image 1 ). Emergent operation was planned. But patient's saturation continued to decrease and intubated. After short period, she had cardiac arrest and dead before performing an emergent operation.
Image 1.
Aortic total thrombosis.
Case 2
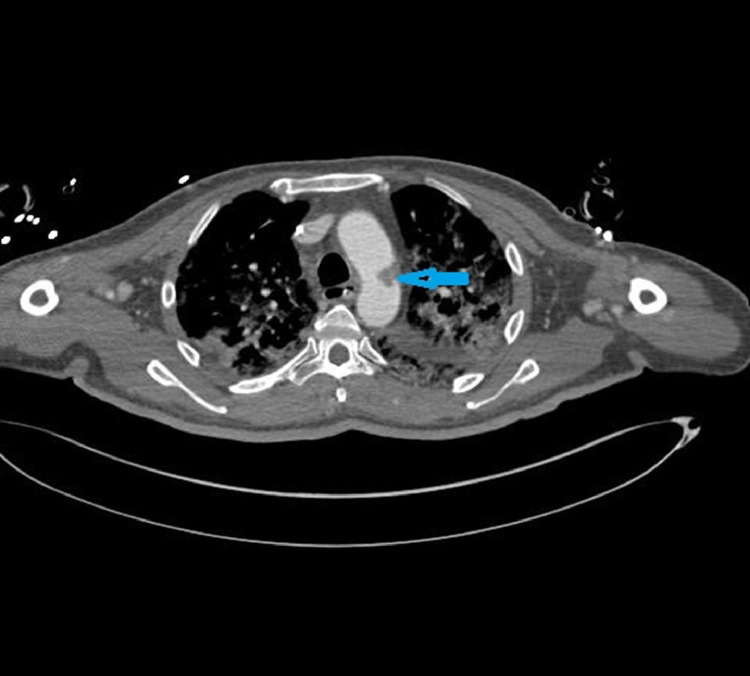
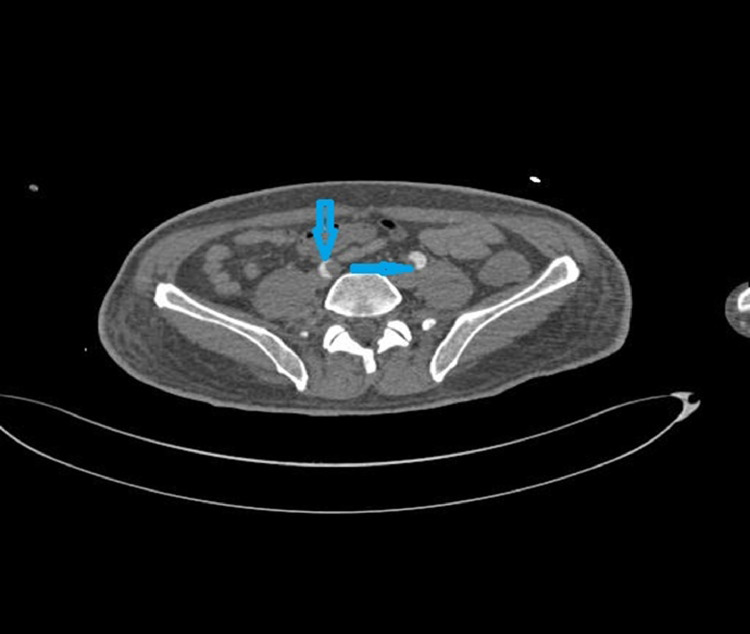
A 53-years-old male patient admitted to emergency service with shortness of breath and fever. Type 2 diabetes was diagnosed on history, physical examination is normal except weak pulses on both legs and feet. Routine blood tests, PCR test and thorax CT scan was performed. Thorax CT scan revealed covid-19, his PCR was positive and patient hospitalized and started medical therapy included LMWH and ASA. On follow ups, patient's clinic worsened and taken to ICU and intubated. Antibiotherapy, LMWH and ASA therapy continued in ICU. On follow up, patient was consulted by our clinic for bilateral cyanosis on distal phalanges. No atrial fibrillation detected, distal phalangeal cyanosis on both extremities was observed, distal pulses were palpable on both lower extremities. Patient was still on LMWH and ASA. Thoraco-abdominal CT angiography performed, floating thrombus detected in arcus aorta and iliac arteries (Images 2 and 3 ). Embolectomy applied to both legs but no thrombus obtained and pentoxyphylline therapy added patient's ongoing medical therapy after operation. Distal pulses were palpable after operation but septic shock arose and deepened, hemodynamic status decompensated and patient was dead result of multiorgan failure.
Image 2.
Floating thrombus in arcus aorta.
Image 3.
Thrombus in iliac arteries.
DISCUSSION
Covid-19 infection activates an inflammatory response, releasing inflammatory mediators and activating the endothelium and hemostatic systems resulting in diffuse endothelial inflammation and microvascular damage, which can result in widespread thrombosis.3 In addition to activating the inflammatory response, hyperimmune condition also accompanies inflammation in thrombogenic event.6 , 7 In reports, it is pointed that, with an unknown mechanism Covid-19 infection triggers especially humoral immunity rather than cell-mediated immunity. This results in excessive accumulation of immune complexes and this condition leads the development of type-3 hypersensitivity.8 Excessive amount of antigen-antibody complexes accumulated inside the tissues, especially blood vessel endothelium inducing a severe inflammatory state. On histopathology the result of this process called “hypersensitivity vasculitis” or “leukocytoclastic vasculitis.”9 And this form of tissue injury can be considered as immune-mediated vasculitidis from type-3 hypersensitivity.10 Following this endothelial injury, platelet aggregation and fibrin formation developed and hypercoagulability and thrombosis occurred.11
The other mechanism of thrombosis in Covid-19 infection is direct invasion of endothelial cells by SARS-Cov-2.12 By this invasion, endothelial cells loose ability of their physiologic functions like nitric oxide (NO) synthesis. The damage of the endothelium results in procoagulant changes of vascular lumen and formation of immunothrombosis.13
This hypercoagulable state may further worsened with Covid-19 mediated hypoxemia resulted from lung involvement by cytokine storm.
Although Covid-19 hypercoagulable pattern most frequently involves in the venous system, arterial involvement especially aortic involvement resulting in aortic thrombus is very rare clinical condition and its prevalence was about 0.75% in moderate to severe Covid-19 cases reported in some series.4 The reason for excessive venous involvement of venous system is due to the components of Virchow's triad of blood stasis, endothelial activation and hypercoagulability and these conditions especially seen in mild to severe Covid-19 patients which were treated in intensive care units (ICU).14 But arterial thrombosis commonly related with the previously damaged endothelium, especially by atherosclerosis, and for this reason arterial involvement mostly seen in hypertensive, diabetic or tobacco smokers.14
This clinic could cause multiple systemic embolus and complicated Covid-19 course with multiple embolic events. And these embolic events could resulted in central nervous system complications (stroke etc.), pulmonary embolus, splanchnic infarctions (renal infact etc) or limb ischemias predisposing multiorgan failure and limb loss. Also, Covid-19 infection lockdown periods had significant effects on non-covid-19 vascular patient care.15 And these conditions have also resulted in an increased number of limb loss in Covid-19 pandemic.15
CONCLUSION
In conclusion; Covid-19 is not only the disease of lungs and inflammatory system also the disease of coagulation and vascular system. Aortic thrombosis is rare and must be kept in mind in Covid-19 patients with peripheral circulation problem and for this reason we think that aggressive anticoagulation and antiaggregation should applied to the patients from the point of diagnosis, especially to mild and severe cases, for avoiding mortal conditions as splanchnic infarcts or morbidities like major amputations.
Declaration of Competing Interest
There is no conflict of interests.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) pandemic. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed May15, 2020.
- 2.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carranza M, Salazar DE, Troya J, et al. 2020. Aortic Thrombus in patients with Severe Covid-19. Review of three cases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baeza C, González A, Torres P, et al. Acute aortic thrombosis in COVID-19. J Vasc Surg Cases Innov Tech. 2020;6:483–486. doi: 10.1016/j.jvscit.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roncati, L, Ligabue G, Fabbiani L, et al. "Type 3 hypersensitivity in COVID-19 vasculitis." (2020): 108487-108489. [DOI] [PMC free article] [PubMed]
- 7.Roncati L, Ligabue G, Nasillo V, et al. A proof of evidence supporting abnormal immunothrombosis in severe COVID-19: naked megakaryocyte nuclei increase in the bone marrow and lungs of critically ill patients. Platelets. 2020;31(8):1085–1089. doi: 10.1080/09537104.2020.1810224. [DOI] [PubMed] [Google Scholar]
- 8.Janeway CA, Jr, Travers P, Walport M, et al. Immunobiology: The Immune System in Health and Disease. 5th edition. Garland Science; 2001. The complement system and innate immunity. [Google Scholar]
- 9.Baigrie, D, Bansal, P, Goyal, A, et al. "Leukocytoclastic vasculitis (hypersensitivity vasculitis)." StatPearls [Internet] (2020).
- 10.Kumar V, Abbas AK, Aster JC. Elsevier Health Sciences; 2017. Robbins Basic Pathology e-book. [Google Scholar]
- 11.Kollias A, Kyriakoulis KG, Dimakakos E, et al. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action. Br J Haematol. 2020;189(5):846–847. doi: 10.1111/bjh.16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wichmann Dominic, Sperhake JP, Lütgehetmann M, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;173(4):268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iba T, Connors JM, Levy JH. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm Res. 2020:1–9. doi: 10.1007/s00011-020-01401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castro-Verdes M, Gkouma A, Wort J, et al. Corona Virus Disease 2019 in situ arterial and venous thrombosis in critically ill patients: a case series. Eur Heart J Case Rep. 2020;4:1. doi: 10.1093/ehjcr/ytaa470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuivens PME, Buijs M, Boonman-de Winter L, et al. Impact of the COVID-19 lockdown strategy on vascular surgery practice: more major amputations than usual. Ann Vasc Surg. 2020;69:74–79. doi: 10.1016/j.avsg.2020.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]