Abstract
Purpose
The purpose of this study was to elucidate the relationship between cytokeratin 19 (CK19) expression and levels of circulating tumor cells (CTCs) in preoperative peripheral blood of patients with hepatocellular carcinoma (HCC), and the potential influence of that relationship on prognosis.
Patients and Methods
CanPatrol™ CTC-enrichment technique and in situ hybridization (ISH) were used to enrich and classify CTCs undergoing the epithelial–mesenchymal transition (EMT) from blood samples of 105 HCC patients. CK19 immunohistochemistry staining was performed on HCC tissues and compared with demographic and clinical data.
Results
In total, 27 of 105 (25.7%) HCC patients were CK19-positive. CK19-positive patients had significantly lower median tumor-free survival (TFS) than CK19-negative patients (5 vs 10 months, P = 0.047). In total, 98 (93.3%) patients showed pre-surgery peripheral blood CTCs (range: 0–76, median: 6), and 57 of 105 (54.3%) patients displayed CTC counts ≥6. Furthermore, CK19-positive patients with CTC count ≥6 showed significantly higher percentage than CK19-negative ones (77.8% vs 46.2%, P = 0.004). CK19-positive patients showed a significantly higher proportion of mesenchymal CTCs among CTCs undergoing EMT than CK19-negative patients (mean rank: 62.28 vs 49.79, P = 0.046). We also found that CK19-positive patients with high CTC count showed significantly shorter median tumor-free survival than CK19-negative patients with low CTC count (5 vs 16 months, P = 0.039).
Conclusion
High CTC count and high percentage of mesenchymal CTCs are closely related to the expression of CK19, which is associated with poor prognosis in HCC patients.
Keywords: hepatocellular carcinoma, cytokeratin 19, circulating tumor cells, prognosis, tumor-free survival
Introduction
Hepatocellular carcinoma (HCC) is one of the most frequent cancers and the second leading cause of death in China.1,2 HCC shows several characteristics of malignant progression that are associated with poor prognosis, including fast growth, strong invasion, easy infiltration into blood vessels and spreading through blood, as well as progression through the epithelial–mesenchymal transition (EMT).3 Despite improvement in surveillance and treatment, prognosis remains poor due to the high incidence of recurrence and metastasis.4 Currently, the concept of “precision medicine” recommends treating each patient with liver cancer differently in order to maximize the chances of survival.5,6 Therefore, early diagnosis, optimization of treatment strategies and post-treatment monitoring are very important for the management and survival of HCC patients.
Conventional imaging techniques, such as computed tomography or magnetic resonance imaging, lack sensitivity for small lesions. Serum alpha-fetoprotein (AFP) is currently an important biomarker for the early screening of HCC and monitoring after treatment,7 but it can be inaccurate.8,9
A growing body of research indicates that the monitoring of circulating tumor cells (CTCs) may be useful for the diagnosis of malignant tumors, assessment of disease, selection of treatment methods, and evaluation of prognosis.10–15 In patients with breast, rectal, or lung cancer, high numbers of CTCs in peripheral blood have been associated with higher rate of postoperative recurrence and worse response to radio- and chemotherapy.11,14,16 CTCs are rare cancer cells that have escaped from the primary solid tumor and entered the circulatory system. They function as seeds for metastases and can be classified as epithelial type (E-CTC), mesenchymal type (M-CTC), or an intermediate type in transition from epithelial to mesenchymal (E/M-CTC). These subtypes can be distinguished based on expression of surface markers. E-CTCs can be transformed into M-CTCs and vice versa.17,18
In HCC, cytokeratin 19 (CK19) is a marker of hepatic progenitor cells and acts as a key player in tumor invasion, indicating poor prognosis.19,20 Over the past years, many studies have shown that CK19-positive HCC has unique biological characteristics regarding tumor stem cells, angiogenesis, invasiveness, and tumor cell apoptosis.21–25 CK19 is closely related to epithelial–mesenchymal transition (EMT), CK19-positive cells acquire mesenchymal characteristics through the EMT and strongly proliferate due to the activation of transforming growth factor beta (TGFb)/Smad signaling.26 However, the relationship between CK19 expression and CTCs in HCC is unclear.
Therefore, based on the biological characteristics of CK19-positive tumors and the process of CTCs generation, we hypothesized that CK19 may involve in EMT transformation and increase the number of CTCs, which can result in poor prognosis of HCC patients. Therefore, the aim of our study was to investigate the potential relationship between CTC levels in peripheral blood and CK19 expression in HCC patients, and assess the potential influence of this relationship on prognosis.
Patients and Methods
Patient Samples
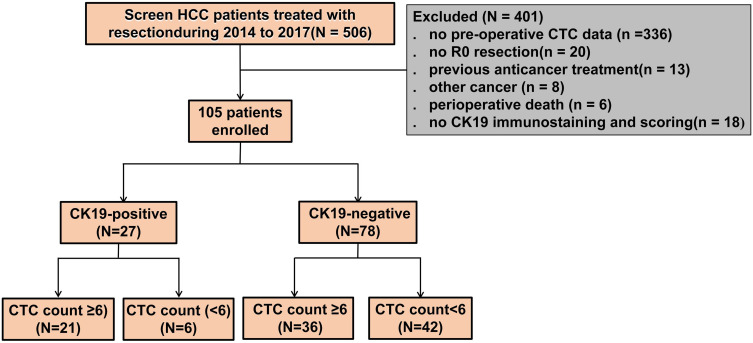
From March 2014 to May 2017, a total of 105 HCC patients treated with R0 resection at the Guangxi Medical University Cancer Hospital, Nanning, Guangxi Province, China, were enrolled. Flow chart of patient enrollment is shown in Figure 1. Those patients were retrospectively enrolled in the current study if they satisfied all the following inclusion criteria: (1) definitive pathological diagnosis of HCC based on the World Health Organization criteria;27 (2) Child-Pugh A stage and Performance Status Test (PST) score of 0–1; (3) no prior anticancer treatment, such as transarterial chemoembolization or radiation; and (4) R0 resection, defined as complete macroscopic removal of the tumor, negative resection margins, and no detectable intra- or extrahepatic metastatic lesions. Other relevant clinical data were obtained for each patient from medical records.
Figure 1.
Flow chart of patient enrollment.
Notes: The 105 patients were divided into two sub-groups based on median CTC counts: patients were classified as having low total CTC count (>6) and as having high total CTC count (≥6)
This study was conducted in accordance with the Declaration of Helsinki guidelines, and the protocol of this trial was approved by the Ethics Committee of the Tumor Hospital of Guangxi Medical University. On admission, all patients provided written consent for their medical data to be analyzed and published for research purposes.
CTC Isolation and in situ Hybridization
The CanPatrolTM system was used to isolate CTCs as previously described.28–31 Blood samples were collected 1 or 2 days before surgery. Peripheral blood samples (5 mL, anticoagulated with ethylenediaminetetraacetic acid) were collected after discarding the first 2 mL to avoid contamination with skin cells. Red blood cell lysis buffer (Sur Exam, Guangzhou, China) was used to remove erythrocytes, and the cells were resuspended in phosphate-buffered saline (PBS) with 4% formaldehyde (Sigma, St. Louis, MO, USA) for 5 min. Next, the blood was filtered using a system including a filtration tube containing a 8-μm pore membrane (Sur Exam), a manifold vacuum plate with valve settings (SurExam), an E-Z96 vacuum manifold (Omega, Norcross, GA, USA), and a vacuum pump (Auto Science, Tianjin, China). The pumping pressure was 0.08 MPa.32
In situ hybridization was used to detect mRNAs encoding EpCAM, CK8/18/19 (as epithelial biomarkers), or Vimentin and Twist (as mesenchymal biomarkers). The assay was performed in a 24-well plate (Corning, NY, USA), and the cells on the membrane were treated with a protease (Qiagen, Hilden, Germany) before hybridization with probe as previously described.11,31,33
CK19 Immunostaining and Scoring
Immunohistochemistry of HCC tissue samples after surgery was performed as previously described.34 Postoperative specimens were fixed in 10% formalin, embedded in paraffin, cut into 4-μm sections, deparaffinized in xylene and rehydrated through graded alcohol solutions. Antigen retrieval was performed for 2–3 min at 100°C in 10 mmol/L citrate buffer (pH 6.0) in a microwave oven. Endogenous peroxidases were blocked by immersing the sections in 3% hydrogen peroxide for 15 min. Sections were then incubated at 37°C for 1 hour with mouse antibody against CK19 (diluted 1:200; Kit-0030, Maixin, Fuzhou, China). Tissue sections were rinsed with PBS, incubated with anti-rabbit or -mouse immunoglobulin (Kit-5030; Maixin) diluted in PBS for 20 min at 25°C, and rinsed again with PBS. Finally, the samples were incubated with horseradish peroxidase-conjugated antibody for 10 min, rinsed in PBS, incubated with diaminobenzidine for 10 min, and counterstained with hematoxylin. CK19-positive tissue slices supplied with the immunostaining kits were analyzed in parallel with patient samples as positive controls and negative controls (by replacing primary antibody with PBS).
The proportion of all cells in the field of view of a section that stained for CK19 was determined independently by two senior pathologists who were blinded to clinical and follow-up data. When the proportion was >5%, the section was considered CK19-positive. Proportions of 5–10% were considered weak expression, while proportions >10% were considered strong expression.
Patient Follow-Up
The 105 patients were followed up every 1–2 months for the first year and every 3 months thereafter, with a final follow-up date of September 30, 2019. Postoperative follow-up consisted of one or more of the following tests: serum AFP measurement, ultrasonography, dynamic computed tomography (CT), and magnetic resonance imaging (MRI). Recurrence was diagnosed based on elevated AFP levels and findings on at least one of the three imaging modalities.35
Statistical Analysis
All statistical analyses were performed with SPSS version 25 for Windows (IBM, Armonk, NY, USA). Scatter plots were plotted using GraphPrism Version 5.0 (GraphPad Software, La Jolla, CA, USA).
The rates of individuals with a given clinical or pathological characteristic, including a certain CTC count, were reported as n (%). Differences between groups were assessed for significance using the Pearson chi-squared test or Fisher’s exact tests if any cell number less than 5. Differences between patients with other CTC levels were assessed using the Mann–Whitney U-test because the data were not normally distributed.
A Kaplan–Meier curve with a Log rank test was performed to compare the tumor-free-survival (TFS) time between levels of CK19 expression or other groups. All statistical assessments were two-tailed, and differences associated with p < 0.05 were considered statistically significant.
Results
Patient Characteristics and Clinical Outcomes
A total of 105 HCC patients with R0 resection (91 males and 14 females) with a mean age of 46.2 years (range: 20–72 years) were enrolled. Nearly half (43, 41.0%) were younger than 45 years, 75 (71.4%) had HBV-DNA levels ≥5.0×102, 59 (56.2%) had AFP levels ≥400 ng/mL, 40 (38.1%) presented multiple tumors, 48 (45.7%) were in BCLC stages B-C and 41 (39.0%) were incomplete tumor capsule. The demographic and clinical characteristics of the enrolled patients are summarized in Table 1.
Table 1.
Demographic and Clinical Characteristics of the 105 HCC Patients
| Variables | Categories | n (%) |
|---|---|---|
| Age (years) | <45 vs. ≥45 | 43 (41) vs 62 (59) |
| Sex | Male vs. Female | 91 (86.7) vs 14 (13.3) |
| HBsAg | Negative vs. Positive | 12 (11.4) vs 93 (88.6) |
| HBV-DNA | <5.0×102 vs. ≥5.0×102 | 30 (28.6) vs 75 (71.4) |
| AFP (ng/mL) | <400 vs. ≥400 | 46 (43.8) vs 59 (56.2) |
| Tumor size (cm) | <5 vs. ≥5 | 23 (21.9) vs 82 (78.1) |
| Tumor number | Single vs. Multiple | 65 (61.9) vs 40 (38.1) |
| Liver cirrhosis | Negative vs. Positive | 4 (3.8) vs 101 (96.2) |
| Edmondson Grade | I–II vs. III–IV | 63 (60.0) vs 42 (40.0) |
| BCLC stage | 0-A vs. B-C | 57 (54.3) vs 48 (45.7) |
| Tumor Capsule | Complete vs. Incomplete | 64 (61.0) vs 41 (39.0) |
| MVI | Negative vs. Positive | 33 (31.4) vs 72 (68.6) |
| PVTT | Negative vs. Positive | 82 (78.1) vs 23 (21.9) |
Abbreviations: AFP, alpha-fetoprotein; BCLC stage, Barcelona Clinic Liver Cancer stage; HBsAg, hepatitis B surface antigen; HBV-DNA, hepatitis B virus DNA; HCC, hepatocellular carcinoma; MVI, microvascular invasion; PVTT, portal vein tumor thrombosis.
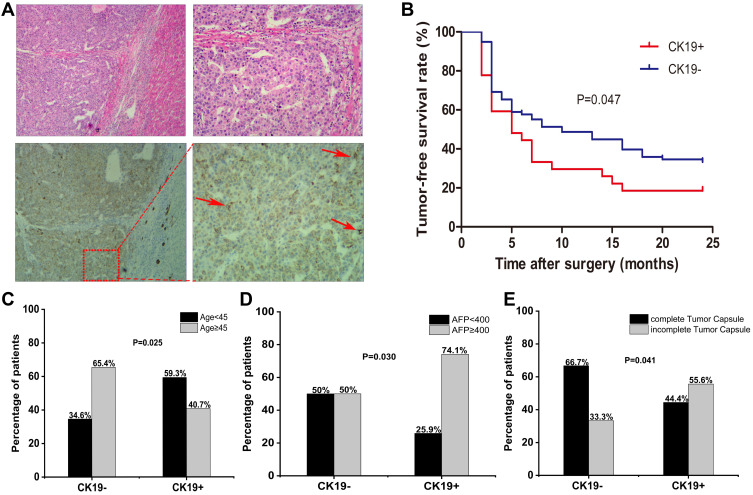
CK19 Immunostaining Levels and TFS
CK19 expression was detected in 27 of 105 (25.7%) HCC cases (Table 2, Figure 2A). TFS analyses showed that CK19-positive HCC patients had significantly shorter TFS than patients with CK19-negative tumors (median TFS:5 vs 10 months, P = 0.047) (Figure 2B). We also found that the characteristics of age<45, AFP≥400 ng/mL, and incomplete tumor capsule were more frequent among CK19-positive patients than CK19-negative ones (Table 2, Figure 2C–E). However, CK19 expression did not vary significantly with patient sex, HBsAg level, HBV-DNA level, tumor size, number of tumors, liver cirrhosis, Edmondson grade, BCLC stage, microvascular invasion (MVI) or portal vein tumor thrombus (PVTT) (Table 2).
Table 2.
Comparison of Clinicopathological Characteristics Between HCC Patients Positive or Negative for CK19
| Variables | CK19-Negative | CK19-Positive | P value |
|---|---|---|---|
| n = 78 | n = 27 | ||
| Age (years) | |||
| <45 | 27 (34.6) | 16 (59.3) | 0.025* |
| ≥45 | 51 (65.4) | 11 (40.7) | |
| Sex | |||
| Male | 67 (85.9) | 24 (88.9) | 0.693 |
| Female | 11 (14.1) | 3 (11.1) | |
| HBsAg | |||
| Negative | 8 (10.3) | 4 (14.8) | 0.771 |
| Positive | 70 (89.7) | 23 (85.2) | |
| HBV-DNA | |||
| <5.0×102 | 24 (30.8) | 6 (22.2) | 0.397 |
| ≥5.0×102 | 54 (69.2) | 21 (77.8) | |
| AFP (ng/mL) | |||
| <400 | 39 (50.0) | 7 (25.9) | 0.030* |
| ≥400 | 39 (50.0) | 20 (74.1) | |
| Tumor size (cm) | |||
| <5 | 19 (24.4) | 4 (14.8) | 0.301 |
| ≥5 | 59 (75.6) | 23 (85.2) | |
| Tumor number | |||
| Single | 48 (61.5) | 17 (63.0) | 0.895 |
| Multiple | 30 (38.5) | 10 (37.0) | |
| Liver cirrhosis | |||
| Negative | 4 (5.1) | 0 | 0.538 |
| Positive | 74 (94.9) | 27 (100) | |
| Edmondson grade | |||
| III–IV | 28 (35.9) | 14 (51.9) | 0.145 |
| I–II | 50 (64.1) | 13 (48.1) | |
| BCLC stage | |||
| 0–A | 42 (53.8) | 15 (55.6) | 0.878 |
| B–C | 36 (46.2) | 12 (44.4) | |
| Tumor capsule | |||
| Complete | 52 (66.7) | 12 (44.4) | 0.041* |
| Incomplete | 26 (33.3) | 15 (55.6) | |
| MVI | |||
| Negative | 26 (33.3) | 7 (25.9) | 0.475 |
| Positive | 52 (66.7) | 20 (74.1) | |
| PVTT | |||
| Negative | 63 (80.8) | 19 (70.4) | 0.260 |
| Positive | 15 (19.2) | 8 (29.6) | |
Notes: Values are n (%); P < 0.05 was considered significant; *p < 0.05.
Abbreviations: AFP, alpha-fetoprotein; BCLC stage, Barcelona Clinic Liver Cancer stage; CK19, cytokeratin 19; HCC, hepatocellular carcinoma; HBV-DNA, hepatitis B virus DNA; HBsAg, hepatitis B surface antigen; MVI, microvascular invasion; PVTT, portal vein tumor thrombosis.
Figure 2.
Immunostaining and prognostic significance of CK19. (A) Tumor sections of the same patient were analyzed by hematoxylin and eosin staining (top) and immunohistochemical staining against CK19 (bottom). The arrowheads was used to indicate a few strong examples of CK19 staining. (B) Tumor-free survival after surgery among patients in CK19- or CK19+ patients. The Kaplan–Meier curve was determined by the Log rank test. Comparison of CK19 expression between CK19- or CK19+ patients stratified by age (C), alpha-fetoprotein (AFP) level (D) or complete of tumor capsule (E). Difference analysis were assessed for significance using the Pearson chi-squared test.
CTC Subpopulations in Blood and Relationships to Clinical Characteristics
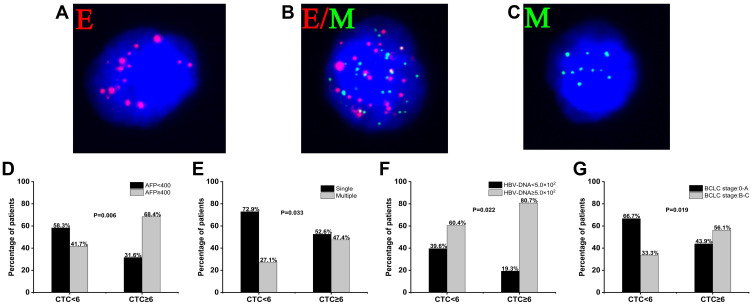
Using the CanPatrol™ CTC-enrichment technique, we measured the number of CTCs in the blood samples of 105 HCC patients before surgery. The green and red fluorescent signals represent mesenchymal or epithelial gene expression, respectively. Three subpopulations were identified: E-CTCs (Figure 3A), E/M-CTCs (Figure 3B), and M-CTCs (Figure 3C).
Figure 3.
Circulating tumor cell (CTC) subpopulations and their relationship with survival. CTCs were stained for epithelial markers (EpCAM and CK8/18/19, red fluorescence) and mesenchymal markers (Vimentin and Twist, green fluorescence) and classified as epithelial CTCs (E-CTCs) (A), epithelial/mesenchymal hybrid CTCs (E/M-CTCs) (B) or mesenchymal CTCs (M-CTCs) (C). Comparison of CTC counts in patients stratified by alpha-fetoprotein (AFP) level (D), tumor number (E), hepatitis B virus (HBV) DNA (F), and Barcelona Clinic Liver Cancer (BCLC) stage (G). Difference analysis were assessed for significance using the Pearson chi-squared test.
CTCs were detected in 98 (93.33%) of the 105 HCC patients. The preoperative median CTC count was 6 (range, 0–76). The 105 patients were divided into two sub-groups based on median CTC count: 48 (45.7%) patients were classified as having low total CTC count (<6) and 57 (54.3%) as having high CTC count (≥6) (Table 3).
Table 3.
Comparison of Clinicopathological Characteristics Between HCC Patients with Low (<6) or High (≥6) CTC Counts
| Variables | CTC<6 | CTC≥6 | P value |
|---|---|---|---|
| n = 48 | n = 57 | ||
| Age (years) | |||
| <45 | 15 (31.2) | 28 (49.1) | 0.064 |
| ≥45 | 33 (68.8) | 29 (50.9) | |
| Sex | |||
| Male | 40 (83.3) | 51 (89.5) | 0.356 |
| Female | 8 (16.7) | 6 (10.5) | |
| HBsAg | |||
| Negative | 6 (12.5) | 6 (10.5) | 0.751 |
| Positive | 42 (87.5) | 51 (89.5) | |
| HBV-DNA | |||
| <5.0×102 | 19 (39.6) | 11 (19.3) | 0.022* |
| ≥5.0×102 | 29 (60.4) | 46 (80.7) | |
| AFP (ng/mL) | |||
| <400 | 28 (58.3) | 18 (31.6) | 0.006* |
| ≥400 | 20 (41.7) | 39 (68.4) | |
| Tumor size (cm) | |||
| <5 | 13 (27.1) | 10 (17.5) | 0.239 |
| ≥5 | 35 (72.9) | 47 (82.5) | |
| Tumor number | |||
| Single | 35 (72.9) | 30 (52.6) | 0.033* |
| Multiple | 13 (27.1) | 27 (47.4) | |
| Liver cirrhosis | |||
| Negative | 4 (8.3) | 0 | 0.087 |
| Positive | 44 (91.7) | 57 (100) | |
| Edmondson grade | |||
| III–IV | 16 (33.3) | 26 (45.6) | 0.201 |
| I–II | 32 (66.7) | 31 (54.4) | |
| BCLC stage | |||
| 0–A | 32 (66.7) | 25 (43.9) | 0.019* |
| B–C | 16 (33.3) | 32 (56.1) | |
| Tumor capsule | |||
| Complete | 34 (70.8) | 30 (52.6) | 0.057 |
| Incomplete | 14 (29.2) | 27 (47.4) | |
| MVI | |||
| Negative | 17 (35.4) | 16 (28.1) | 0.419 |
| Positive | 31 (64.6) | 41 (71.9) | |
| PVTT | |||
| Negative | 41 (85.4) | 41 (71.9) | 0.096 |
| Positive | 7 (14.6) | 16 (28.1) | |
Notes: Values are n (%); P < 0.05 was considered significant; *p < 0.05.
Abbreviations: AFP, alpha-fetoprotein; BCLC stage, Barcelona Clinic Liver Cancer stage; CTCs, circulating tumor cells; HCC, hepatocellular carcinoma; HBV-DNA, hepatitis B virus DNA; HBsAg, hepatitis B surface antigen; MVI, microvascular invasion; PVTT, portal vein tumor thrombosis.
Significantly higher CTC counts were found in patients with AFP≥ 400 ng/mL, multiple tumors, HBV DNA≥5.0×102 and advanced HCC (BCLC B-C stage) (Table 3, Figure 3D–G). However, CTC counts did not vary significantly with patient age, sex, HBsAg level, tumor size, liver cirrhosis, Edmondson grade, tumor capsule, MVI or PVTT.
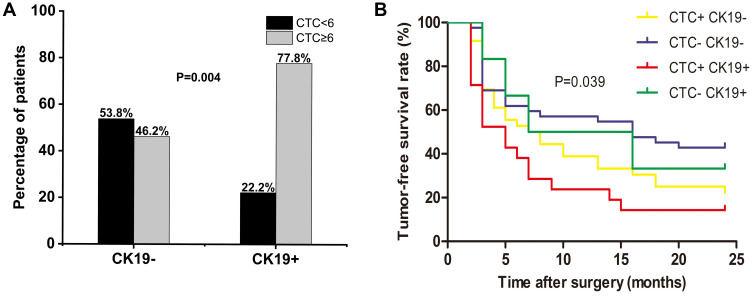
Association of CK19 Levels with CTC Count or Type
CK19-positive patients with high CTC count showed significantly higher CTC percentage (77.8%) than CK19-negative patients (46.2%, P = 0.004) (Figure 4A). Further analysis revealed that CTCs in peripheral blood of CK19-positive patients were mainly of the M-CTC type, whereas more CTCs were of the E-CTC type in CK19-negative patients (Table 4).
Figure 4.
Association of CTC counts with CK19 immunostaining, and survival analysis based on this association. (A) Comparison of CK19- or CK19+ patients stratified by CTC count <6 or ≥6. Difference analysis were assessed for significance using the Pearson chi-squared test. P<0.05 was considered statistically significant. (B) Tumor-free survival after surgery among patients stratified by both CK19 expression and CTC count. The Kaplan–Meier curve was determined by the Log rank test.
Table 4.
Distribution of CTCs’ Types in 105 HCC Patients Positive or Negative for CK19
| CTCs’ Type | Mean Rank | U | Z | P value | |
|---|---|---|---|---|---|
| CK19 Positive | CK19 Negative | ||||
| All CTCs | 65.54 | 48.66 | 714.50 | −2.488 | 0.013* |
| E-CTC | 56.00 | 51.96 | 972.00 | −6.04 | 0.546 |
| M-CTC | 62.28 | 49.79 | 802.50 | −1.991 | 0.046* |
| E/M-CTC | 62.50 | 49.71 | 796.50 | −1.896 | 0.058 |
Notes: P < 0.05 was considered significant; *p < 0.05.
Abbreviations: CK19, cytokeratin 19; CTCs, circulating tumor cells; E-CTC, epithelial CTCs; M-CTC, mesenchymal CTCs; E/M-CTC, epithelial/mesenchymal hybrid CTCs.
Our analysis found that the median TFS of the different groups were 5.0 months for CK19-positive patients with high CTC count, 7.0 months for CK19-negative patients with high CTC count, 7.0 months for CK19-positive patients with low CTC count, and 16.0 months for CK-negative patients with low CTC count. Among the four groups, patients who had high CTC count and were CK19-positive had significantly lower TFS (p<0.05) (Figure 4B).
Discussion
The high recurrence and metastasis rates of HCC after radical surgery reduce survival. Therefore, early diagnosis of HCC and post-treatment monitoring are key for comprehensive treatment and management of these patients. At present, clinical indicators to predict postoperative recurrence are rare. Therefore, we explored the postoperative prognosis of HCC through the evaluation of preoperative peripheral blood CTCs levels as well as CK19 expression in postoperative cancer tissues.
CK19-positive HCC cells show a high degree of malignancy, including invasion and other aggressive behaviors.26,36–38 A previous study showed that the median disease-free survival time of CK19-positive HCC patients was significantly shorter than that of CK19-negative patients among those undergoing radiofrequency ablation.39 Consistently, we found that TFS was shorter for CK19-positive patients than for CK19-negative ones. Hepatocellular carcinoma recurrence is divided into early recurrence (less than 2 years) and late recurrence (more than 2 years) according to the time to recurrence after surgery.40–42 The mechanisms of early and late recurrence are different.43–46 The presence of CTCs reflects the aggressiveness of a solid tumor. A previous study by our group showed that high CTC counts before resection were significantly associated with early recurrence of HCC.31 The current work showed that CK19-positive patients had higher CTC counts than CK19-negative ones. We extended those findings in the present study by showing that high CTC count and CK19 express positive showed significantly lower tumor-free survival than patients with low CTC count and CK19-negative. These results suggest that CK19 contributes to poor prognosis.
We also found that CTCs in peripheral blood of CK19-positive patients were mainly of the M-CTC type, whereas more CTCs were of the E-CTC type in CK19-negative patients. M-CTCs are regarded as the most malignant CTC.31 A previous study revealed that CK19-positive cells in HCC possess Cancer stem cells (CSCs) characteristics are closely related to the EMT, and that CK19-positive cells express several genes associated with the EMT and show higher motility and migration than CK19-negative cells.26 EMT enhances tumor mobility and invasiveness and is believed to facilitate metastasis.47–49 During EMT, cancer cells lose some of their epithelial characteristics and acquire more migratory mesenchymal cell-like characteristics, undergoing major changes in their cytoskeleton.50,51 Our results suggest that high levels of M-CTCs are closely related to the expression of CK19 and lead to a poor prognosis in patients with CK19-positive HCC. CK19 may regulate EMT and promote an increase in the number of CTCs, ultimately leading to poor prognosis.
Interestingly, we found from the postoperative clinical results of HCC patients that those with CK19-positive HCC were younger, had higher serum AFP levels and showed lower rates of tumor envelope formation than those with CK19-negative HCC. These results suggest that the expression of CK19 in HCC increases tumor invasiveness.
This study presents several limitations. First, our cohort was relatively small. To overcome this limitation, we will further verify this conclusion in follow-up research and will conduct research in a multi-center cohort. In addition, the present study was conducted only at the clinical level. Molecular studies are needed to elucidate the causes of poor prognosis in CK19-positive patients with high CTCs in peripheral blood. This may help to find a new target for “precise therapy” for CK19-positive HCC patients with high preoperative CTC counts.
Conclusion
High CTC count and high M-CTC percentage are closely related to the expression of CK19 in HCC, which in turn is associated with recurrence. The preoperative number of CTCs undergoing EMT may be significantly higher in CK19-positive HCC patients than in CK19-negative patients. In CK-19 positive patients, the main CTC type may be mesenchymal. Preoperative CTC analysis combined with postoperative analysis of CK19 expression may be a new method for predicting prognosis of HCC patients after surgery.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (81960450), National Major Special Science and Technology Project (2017ZX10203207), The Key Research and Development Project of Guangxi (AA18221001, AB18050020), High-level innovation team and outstanding scholar program in Guangxi Colleges and Universities,“139” projects for training of high-level medical science talents from Guangxi(G201903001). The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Zhou M, Wang H, Zeng XY, et al. Mortality, morbidity, and risk factors in China and its Provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;10204:1145–1158. doi: 10.1016/S0140-6736(19)30427-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang B, Li M, Tang W, et al. Dynamic network biomarker indicates pulmonary metastasis at the tipping point of hepatocellular carcinoma. Nat Commun. 2018;9(1):678. doi: 10.1038/s41467-018-03024-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Llovet JM, Hernandez-Gea V. Hepatocellular carcinoma: reasons for phase III failure and novel perspectives on trial design. Clin Cancer Res. 2014;20(8):2072–2079. doi: 10.1158/1078-0432.CCR-13-0547 [DOI] [PubMed] [Google Scholar]
- 5.Liang Q, Shen X, Sun G. Precision medicine: update on diagnosis and therapeutic strategies of hepatocellular carcinoma. Curr Med Chem. 2017;8(17):1999–2008. doi: 10.2174/0929867325666180117101532 [DOI] [PubMed] [Google Scholar]
- 6.Llovet JM, Montal R, Sia D, Finn RS. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat Rev Clin Oncol. 2018;15(10):599–616. doi: 10.1038/s41571-018-0073-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kudo M. Evidence and consensus on the management of hepatocellular carcinoma: update 2015. Oncology. 2015;89(2):1–3. doi: 10.1159/000440624 [DOI] [PubMed] [Google Scholar]
- 8.Mehta NJ, Celik AD, Peters MG. Screening for hepatocellular carcinoma: what is missing? Hepatol Commun. 2017;1(1):18–22. doi: 10.1002/hep4.1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morimoto M, Numata K, Nozaki A, et al. Novel lens culinaris agglutinin-reactive fraction of α-fetoprotein: a biomarker of hepatocellular carcinoma recurrence in patients with low α-fetoprotein concentrations. Int J Clin Oncol. 2012;17(4):373–379. doi: 10.1007/s10147-011-0306-3 [DOI] [PubMed] [Google Scholar]
- 10.Sun Y, Xu Y, Yang X, et al. Circulating stem cell–like epithelial cell adhesion molecule–positive tumor cells indicate poor prognosis of hepatocellular carcinoma after curative resection. Hepatology. 2013;4:1458–1468. doi: 10.1002/hep.26151 [DOI] [PubMed] [Google Scholar]
- 11.Yu M, Bardia A, Wittner BS, et al. Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science. 2013;339(6119):580–584. doi: 10.1126/science.1228522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alix-Panabières C, Pantel K. Challenges in circulating tumour cell research. Nat Rev Cancer. 2014;14(9):623–631. doi: 10.1038/nrc3820 [DOI] [PubMed] [Google Scholar]
- 13.Bruix J, Reig M, Sherman M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology. 2016;150(4):835–853. doi: 10.1053/j.gastro.2015.12.041 [DOI] [PubMed] [Google Scholar]
- 14.Sun W, Li G, Wan J, Zhu J, Shen W, Zhang Z. Circulating tumor cells: a promising marker of predicting tumor response in rectal cancer patients receiving neoadjuvant chemo-radiation therapy. Oncotarget. 2016;7(43):69507–69517. doi: 10.18632/oncotarget.10875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Wang H, Li T, et al. Circulating tumor DNA/circulating tumor cells and the applicability in different causes induced hepatocellular carcinoma. Curr Probl Cancer. 2019;2:100516. [DOI] [PubMed] [Google Scholar]
- 16.Hou JM, Krebs M, Ward T, et al. Circulating tumor cells as a window on metastasis biology in lung cancer. Am J Pathol. 2011;3:989–996. doi: 10.1016/j.ajpath.2010.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bednarzknoll N, Alixpanabieres C, Pantel K. Plasticity of disseminating cancer cells in patients with epithelial malignancies. Cancer Metastasis Rev. 2012;3:673–687. doi: 10.1007/s10555-012-9370-z [DOI] [PubMed] [Google Scholar]
- 18.Nieto MA, Huang RYJ, Jackson RA, Thiery JP. Emt: 2016. Cell. 2016;1:21–45. [DOI] [PubMed] [Google Scholar]
- 19.Durnez A, Verslype C, Nevens F, et al. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology. 2006;2:138–151. doi: 10.1111/j.1365-2559.2006.02468.x [DOI] [PubMed] [Google Scholar]
- 20.Kim H, Choi GH, Na DC, et al. Human hepatocellular carcinomas with “stemness”‐related marker expression: keratin 19 expression and a poor prognosis. Hepatology. 2011;5:1707–1717. doi: 10.1002/hep.24559 [DOI] [PubMed] [Google Scholar]
- 21.Roskams T, Katoonizadeh A, Komuta M. Hepatic progenitor cells: an update. Clin Liver Dis. 2010;14(4):705–718. doi: 10.1016/j.cld.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 22.Ji HN, Rhee H, Kim H, et al. Increased expression of stemness markers and altered tumor stroma in hepatocellular carcinoma under TACE-induced hypoxia: a Biopsy and Resection Matched Study. Oncotarget. 2017;59:99359–99371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takano M, Shimada K, Fujii T, et al. Keratin 19 as a key molecule in progression of human hepatocellular carcinomas through invasion and angiogenesis. Bmc Cancer. 2016;16(1):903. doi: 10.1186/s12885-016-2949-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoneda N, Sato Y, Kitao A, et al. Epidermal growth factor induces cytokeratin 19 expression accompanied by increased growth abilities in human hepatocellular carcinoma. Lab Invest. 2011;91(2):262–272. doi: 10.1038/labinvest.2010.161 [DOI] [PubMed] [Google Scholar]
- 25.Ku N-O, Strnad P, Bantel H, Omary MB. Keratins: biomarkers and modulators of apoptotic and necrotic cell death in the liver. Hepatology. 2016;64(3):966–976. doi: 10.1002/hep.28493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kawai T, Yasuchika K, Ishii T, et al. Keratin 19, a cancer stem cell marker in human hepatocellular carcinoma. Clin Cancer Res. 2015;21(13):3081–3091. doi: 10.1158/1078-0432.CCR-14-1936 [DOI] [PubMed] [Google Scholar]
- 27.The International Agency for Research on Cancer. WHO Classification of Tumours of the Digestive System (IARC WHO Classification of Tumours). 4th ed. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. World Health Organization; 2010:p5771–418. [Google Scholar]
- 28.Liu Y, Hu B, Li Z, He X, Li Y, Lu L. An improved strategy to detect the epithelial-mesenchymal transition process in circulating tumor cells in hepatocellular carcinoma patients. Hepatol Int. 2016;10(4):640–646. doi: 10.1007/s12072-016-9732-7 [DOI] [PubMed] [Google Scholar]
- 29.Li TT, Liu H, Li FP, et al. Evaluation of epithelial-mesenchymal transitioned circulating tumor cells in patients with resectable gastric cancer: relevance to therapy response. World J Gastroenterol. 2015;21(47):13259–13267. doi: 10.3748/wjg.v21.i47.13259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao R, Cai Z, Li S, et al. Expression and clinical relevance of epithelial and mesenchymal markers in circulating tumor cells from colorectal cancer. Oncotarget. 2017;8(6):9293–9302. doi: 10.18632/oncotarget.14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qi L, Xiang B, Wu F, et al. Circulating tumor cells undergoing EMT provide a metric for diagnosis and prognosis of patients with hepatocellular carcinoma. Cancer Res. 2018;78(16):4731–4744. doi: 10.1158/0008-5472.CAN-17-2459 [DOI] [PubMed] [Google Scholar]
- 32.Wu S, Liu S, Liu Z, et al. Classification of circulating tumor cells by epithelial-mesenchymal transition markers. PLoS One. 2015;4:e123976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Si Y, Lan G, Deng Z, et al. Distribution and clinical significance of circulating tumor cells in nasopharyngeal carcinoma. Jpn J Clin Oncol. 2016;46(7):622–630. doi: 10.1093/jjco/hyw046 [DOI] [PubMed] [Google Scholar]
- 34.Guo Z, Li L, Jiang J, Ou C, Zeng L, Xiang B. Cancer stem cell markers correlate with early recurrence and survival in hepatocellular carcinoma. World J Gastroenterol. 2014;8:2098–2106. doi: 10.3748/wjg.v20.i8.2098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qi L-N, Ma L, Chen -Y-Y, et al. Outcomes of anatomical versus non-anatomical resection for hepatocellular carcinoma according to circulating tumour-cell status. Ann Med. 2020;52(1–2):21–31. doi: 10.1080/07853890.2019.1709655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yasufumi S. The vasohibin family: a novel family for angiogenesis regulation. J Biochem. 2013;1:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Govaere O, Komuta M, Berkers J, et al. Keratin 19: a key role player in the invasion of human hepatocellular carcinomas. Hepatology. 2013;4:674–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim H, Yoo JE, Cho JY, et al. Telomere length, TERT and shelterin complex proteins in hepatocellular carcinomas expressing “stemness”-related markers. J Hepatol. 2013;59(4):746–752. doi: 10.1016/j.jhep.2013.05.011 [DOI] [PubMed] [Google Scholar]
- 39.Tsuchiya K, Komuta M, Yasui Y, et al. Expression of keratin 19 is related to high recurrence of hepatocellular carcinoma after radiofrequency ablation. Oncology. 2011;80(3–4):278–288. doi: 10.1159/000328448 [DOI] [PubMed] [Google Scholar]
- 40.Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–207. doi: 10.1016/S0168-8278(02)00360-4 [DOI] [PubMed] [Google Scholar]
- 41.Poon RT, Fan ST, Ng IO, Lo CM, Liu CL, Wong J. Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma. Cancer. 2000;89:500–507. [PubMed] [Google Scholar]
- 42.Portolani N, Coniglio A, Ghidoni S, et al. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg. 2006;243(2):229–235. doi: 10.1097/01.sla.0000197706.21803.a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng J, Chou JF, Gönen M, et al. Prediction of hepatocellular carcinoma recurrence beyond Milan criteria after resection: validation of a clinical risk score in an international cohort. Ann Surg. 2017;266(4):693–701. doi: 10.1097/SLA.0000000000002360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Poon RTP. Differentiating early and late recurrences after resection of HCC in cirrhotic patients: implications on surveillance, prevention, and treatment strategies. Ann Surg Oncol. 2009;16(4):792–794. doi: 10.1245/s10434-009-0330-y [DOI] [PubMed] [Google Scholar]
- 45.Du Z-G, Wei Y-G, Chen K-F, Li B. Risk factors associated with early and late recurrence after curative resection of hepatocellular carcinoma: a single institution’s experience with 398 consecutive patients. Hepatobiliary Pancreat Dis Int. 2014;13(2):153–161. doi: 10.1016/S1499-3872(14)60025-4 [DOI] [PubMed] [Google Scholar]
- 46.Xu X-F, Xing H, Han J, et al. Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: a Multicenter Study From China. JAMA Surgery. 2019;154(3):209–217. doi: 10.1001/jamasurg.2018.4334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14(6):818–829. doi: 10.1016/j.devcel.2008.05.009 [DOI] [PubMed] [Google Scholar]
- 48.Thiery JP, Acloque H, Huang RYJ, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139(5):871–890. doi: 10.1016/j.cell.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 49.Lee JM, Dedhar S, Kalluri R, Thompson EW. The epithelial–mesenchymal transition: new insights in signaling, development, and disease. J Cell Biol. 2006;172(7):973–981. doi: 10.1083/jcb.200601018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kang Y, Massagué J. Epithelial-mesenchymal transitions twist in development and metastasis. Cell. 2004;118(3):277–279. doi: 10.1016/j.cell.2004.07.011 [DOI] [PubMed] [Google Scholar]
- 51.Thiery JP, Sleeman JP. Complex networks orchestrate epithelial–mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;2:131–142. doi: 10.1038/nrm1835 [DOI] [PubMed] [Google Scholar]