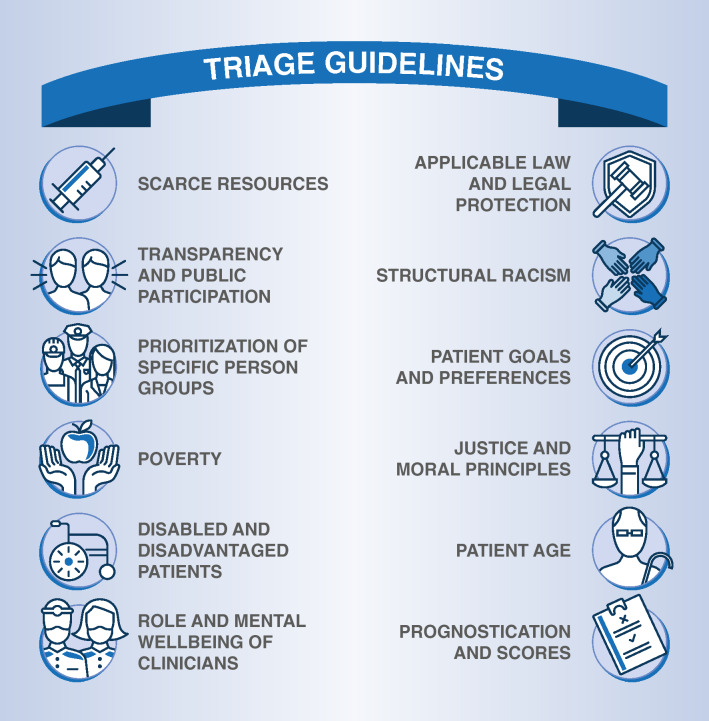
The coronavirus disease 2019 (COVID-19) pandemic has reaffirmed the need for establishing an ethical basis for rationing decisions during pandemics. In some jurisdictions, medical resources, intensive care unit (ICU) beds, or healthcare workers (HCWs) became scarce and rationing of life-sustaining treatment was needed [1]. Principles and processes for triage have been proposed and guidelines developed [2–4]. Concurrently, critiques arose pertaining to legal issues, equity concerns, and the practicality of these recommendations, given many unprecedented features of this pandemic [5, 6]. The goal of this commentary is to provide additional guidance to support and enhance the development and implementation of such guidelines through the identification of ten elements critical for consideration in rationing decisions during crises. These ten elements incorporate principles important to clinicians, administrators and society at large (Fig. 1 and Online Supplement for Supplementary References).
Fig. 1.
Elements critical for consideration in rationing decisions during crises. Detailed explanations for the elements displayed are given in the text. Supplementary references for all elements can be found in the Online Supplement
Identify the resources that are scarce
Before rationing occurs, a thorough needs assessment is required. The scarce resources must be clearly identified. Only then may effective measures be taken to address resource scarcity. For instance, when capacity to provide mechanical ventilation is limited, we must understand whether this is due to a shortage of ventilators, component parts, ICU beds, or ICU staff. Further, resources that are scarce may change from moment to moment and may include a range of resources, such as personal protective equipment, devices, or specific supplies.
All avenues to supplement resources must be exhausted before rationing begins
Rationing entails withholding a necessary treatment from patients in need. This could potentially result in further deterioration or death. Therefore, every reasonable effort must be made to use available resources efficiently and to transfer patients to settings where resources are still available, before rationing commences [6]. Guidelines should incorporate provisions to guarantee the use of all potentially available resources, including repurposing of resources, personnel, or structures not traditionally designated for the intended use.
Importance of transparency and public participation
Decisions about sustaining life are often emotionally charged, complicating rationing guidelines. The application of different moral principles may lead to different and conflicting recommendations in the context of rationing. While utilitarian reasoning prioritizes outcome maximization, egalitarian reasoning prioritizes equity of opportunities, and communitarian reasoning prioritizes the relation between the individual and the community. Each community or society should agree on prioritization of the principles that form the basis for rationing decisions. Ideally, this should be done in a transparent public debate before entering into a crisis. Although this may be impractical in many circumstances, every effort should be made to engage with key stakeholders in the enumeration of these principles.
Role of prognostic scores and age
The use of prognostic scores is frequently recommended to assist rationing decisions based on outcome maximization. However, it is not self-evident that outcome maximation should be the primary guiding principle for rationing. Furthermore, when such scores are used, they should be both applicable and validated for the specific clinical context. This is challenging in a novel pandemic.
Patient age is prognostic parameter for many health conditions and correlates with other prognostically relevant factors, such as burden of chronic disease [7]. Rationing by age alone may be considered unacceptable discrimination. On the other hand, some argue that people should have an equal opportunity to pass through the different stages of life, which prioritizes the young [8]. Incorporating age is inevitable: the key is to come to an explicit agreement regarding the appropriate role of age in rationing.
Responsibility for the rationing decision
During the COVID-19 pandemic, clinical teams at the bedside may be confronted with a variety of rationing decisions throughout the day. Triage committees have been proposed to relieve bedside physicians of this burden. However, under the circumstances when triage committees are most likely to be needed in this complex and prolonged pandemic, such teams are likely to be overwhelmed and rendered ineffective by the complexity, duration, and time-sensitive nature of the multiple and highly-varied decisions required. We therefore recommend that triage committees be responsible for setting standards and developing guidelines and structures while the responsibility for individual bedside decisions may need to remain with the treating clinicians [6].
Importance of patient goals and preferences
When rationing must be considered, patient advance directives and expressions of a patient’s goals and preferences regarding potential treatment limitations are more relevant than ever. Therefore, rationing guidelines must pay attention to the early collection of the patient’s goals and preferences, especially for the elderly and those with chronic life-limiting illnesses [9]. For patients without decisional capacity, involvement of surrogate decision-makers should be considered at an early stage.
Accounting for disabled and disadvantaged patients, poverty, and structural racism
Rationing decisions must consider the perspective of vulnerable populations. Poverty and low formal education levels are associated with poorer health status [10]. The same is true for racial and ethnic minorities and patients with disabilities [11]. A focus of rationing decisions on long-term outcomes could further disadvantage these groups and should therefore be adjusted to address these disparities [12]. Recently, a process for mitigation of inequities through triage decisions has been presented that may serve as a blueprint for practical applications of triage guidelines [13].
Prioritization of defined person groups
For specific contexts like the distribution of vaccines, some propose prioritization of defined person groups, such as healthcare workers, based on their instrumental value [3]. If such prioritization occurs, it must be thoroughly justified and transparent. Care must be taken to ensure that prioritization based on a perceived instrumental value of a specific group is not abused to the disproportionate detriment of other groups.
Important legal protections
Rationing decisions take place within a given jurisdiction and must comply with applicable law. However, in many regions, legislation on rationing and end-of-life decisions is incomplete and therefore provides no sound legal basis for rationing. This lack of legal regulations cannot be replaced by triage guidelines, and healthcare workers making rationing decisions while working under crisis standards of care must be able to rely on societal and legal support for appropriate rationing decisions, making this an urgent issue to address.
Impact of triage and rationing on clinicians
When rationing of life-sustaining treatments is required, HCWs participating in triage in the context of stressful working will bear witness to the suffering and death of many patients—this can have an impact on the mental health of HCWs [14]. Triage guidelines should take into account the role of HCWs and incorporate provisions for their support and assistance [15].
We present ten elements intended to supplement existing and developing rationing guidelines. These elements should be addressed in the implementation of such guidelines. The incorporation of these elements is complex and will require adaptation for individual societies through transparent debate.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was provided specific to this work.
Declarations
Conflicts of interest
All authors have completed the ICMJE form (available upon request from the corresponding author). AS reports research grants and lecture fees from CytoSorbents and lecture fees from Abiomed, both outside the submitted work. DB reports grants from ALung Technologies, personal fees from Baxter, personal fees from Xenios, personal fees from Abiomed, and unpaid consultancy for Hemovent outside the submitted work. JRC reports grants from the National Institutes of Health and the National Palliative Care Research Center and grants and personal fees from Cambia Health Foundation outside the submitted work.
Ethical approval
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the Epidemic’s front line. N Engl J Med. 2020;382:1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence (2020) COVID-19 rapid guideline: critical care in adults. www.nice.org.uk/guidance/ng159 (last visit 25.01.2021) [PubMed]
- 3.Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, Phillips JP. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 4.Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, Salluh J, Meyfroidt G, Alshamsi F, Oczkowski S, Azoulay E, Price A, Burry L, Dzierba A, Benintende A, Morgan J, Grasselli G, Rhodes A, Moller MH, Chu L, Schwedhelm S, Lowe JJ, Bin D, Christian MD. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46:1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liddell K, Martin S, Palmer S. Allocating medical resources in the time of Covid-19. N Engl J Med. 2020;382:e79. doi: 10.1056/NEJMc2009666. [DOI] [PubMed] [Google Scholar]
- 6.Supady A, Curtis JR, Abrams D, Lorusso R, Bein T, Boldt J, Brown CE, Duerschmied D, Metaxa V, Brodie D. Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(20)30580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellelli G, Rebora P, Valsecchi MG, Bonfanti P, Citerio G, members C-MT Frailty index predicts poor outcome in COVID-19 patients. Intensive Care Med. 2020;46:1634–1636. doi: 10.1007/s00134-020-06087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams A. Intergenerational equity: an exploration of the 'fair innings’ argument. Health Econ. 1997;6:117–132. doi: 10.1002/(SICI)1099-1050(199703)6:2<117::AID-HEC256>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 9.Curtis JR, Kross EK, Stapleton RD. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19) JAMA. 2020;323:1771–1772. doi: 10.1001/jama.2020.4894. [DOI] [PubMed] [Google Scholar]
- 10.Case A, Deaton A. Deaths of despair and the future of capitalism. Princeton: Princeton University Press; 2020. [Google Scholar]
- 11.Evans MK. Covid’s color line—infectious disease, inequity, and racial justice. N Engl J Med. 2020;383:408–410. doi: 10.1056/NEJMp2019445. [DOI] [PubMed] [Google Scholar]
- 12.Sen A. Why health equity? Health Econ. 2002;11:659–666. doi: 10.1002/hec.762. [DOI] [PubMed] [Google Scholar]
- 13.White DB, Lo B, (2020) Mitigating Inequities and Saving Lives with ICU Triage During the COVID-19 Pandemic. AJRCCM online ahead of print [DOI] [PMC free article] [PubMed]
- 14.Tsang JLY, Binnie A, Fowler RA. Twenty articles that critical care clinicians should read about COVID-19. Intensive Care Med. 2021 doi: 10.1007/s00134-020-06329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Supady A, Curtis JR, Brown CE, Duerschmied D, von Zepelin LA, Moss M, Brodie D. Ethical obligations for supporting healthcare workers during the COVID-19 pandemic. Euro Resp J. 2021;57(2):2100124. doi: 10.1183/13993003.00124-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.