Abstract
Background
In the UK, consultations for prescription medicines are available via private providers such as online pharmacies. However, these providers may have lower thresholds for prescribing certain drugs. This is a particular concern for antibiotics, given the increasing burden of antimicrobial resistance. Public preferences for consultations with online providers are unknown, hence the impact of increased availability of online consultations on antibiotic use and population health is unclear.
Objective
To conduct a discrete choice experiment survey to understand UK public preferences for seeking online consultations, and the factors that influence these preferences, in the context of having symptoms for which antibiotics may be appropriate.
Methods
In a survey conducted between July and August 2018, general population respondents completed 16 questions in which they chose a primary care consultation via either their local medical centre or an online provider. Consultations were described in terms of five attributes, including cost and similarity to traditional ‘face-to-face’ appointments. Choices were modelled using regression analysis.
Results
Respondents (n = 734) placed a high value on having a consultation via their local medical centre rather than an online provider, and a low value on consultations by phone or video. However, respondents characterised as ‘busy young professionals’ showed a lower strength of preference for traditional consultations, with a higher concern for convenience.
Conclusion
Before COVID-19, the UK public had limited appetite for consultations with online providers, or for consultations that were not face-to-face. Nevertheless, prescriptions from online providers should be monitored going forward, particularly for antibiotics, and in key patient groups.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40258-021-00642-8.
Key Points for Decision Makers
| There is rising concern that online pharmacies may have lower thresholds for prescribing medicines such as antibiotics. This is a particular concern as antimicrobial resistance is increasing. |
| In our discrete choice experiment, the general public placed a high value on consultations with primary care physicians taking place via their local medical centre rather than an online provider, and a low value on consultations by phone, video or instant messaging service. |
| However, one subgroup (‘busy young professionals’) showed a lower strength of preference for traditional consultations, with a higher concern for convenience, suggesting that antibiotic prescriptions from online providers should be monitored going forward in key patient groups. |
Introduction
In many countries, primary care physicians are the main point of contact for healthcare services. Typically, patients attend a face-to-face consultation at a local medical centre in which a physician (commonly a General Practitioner—GP) listens to their concerns, reviews their symptoms, assesses any clinical signs and suggests a management strategy. If required, the physician may issue a prescription for medicine that the patient can collect from a pharmacy. In the UK, consultations with a GP in the National Health Service (NHS) are free. Prescriptions in England are usually charged at £9.15/item, although some patient groups (e.g. children, the elderly, those with specific health conditions such as cancer) are exempt from charges, and all prescriptions are free in the rest of the UK (Scotland, Wales and Northern Ireland) [1].
Over the past 2 decades, there has been a vast increase in the use of online services in all aspects of our daily lives, from internet banking to online grocery shopping. Public expectations regarding consultations for prescription medicines have also evolved, prompted in part by these technological advances. Such consultations are now available in a range of formats in a patient’s local medical centre. The traditional face-to-face consultation is still widely offered, but consultations are also now possible in some medical centres via video call, voice call, instant messaging service or by submitting an electronic form. To support these developments, NHS England has launched the GP Online Consultation Systems Fund and developed an implementation toolkit for online consultations in primary care [2, 3]. In addition, the NHS long-term plan now includes a commitment that every patient will have the right to be offered digital-first primary care by 2023–2024 [4]. At the same time, there has been an increase in the availability of consultations with private providers, including online pharmacies. These providers can dispense medications following a paid-for, virtual consultation with a GP, and may also offer patients more flexible consultation times and a wider selection of GPs. However, these providers operate on a for-profit basis outside the NHS, so there is some concern that they may have lower thresholds for prescribing some drugs, for example, due to less rigorous safety checks or not requiring detailed medical histories [5–7].
Some of the most frequently prescribed drugs in primary care are antibiotics (39 million items prescribed in 2015 in England; eighth most frequently prescribed class of medicines) [8]. However, antimicrobial resistance is increasing, driven by widespread, often inappropriate, antibiotic use, and poses a major threat to public health [9]. Between 9 and 23% of all antibiotic prescriptions in England are inappropriate [10], while in the USA up to 50% of antibiotics are not optimally prescribed [11, 12]. In the UK, around half of all antibiotics are prescribed to adults aged 19–64 years (i.e. patients who generally pay for prescriptions) [13]. The GP ‘gatekeeper’ approach is intended to ensure appropriate use of drugs like antibiotics, and there is evidence that this role can contribute to explaining observed differences in antibiotic use and resistance levels across countries [14]. However, if this approach does not meet patient expectations (for example, if patients expect advice on symptomatic treatment but do not get it, or if they are not prescribed medicines they think they need), this can lead to frustration [15, 16]. In such a scenario, patients might instead seek a consultation with an alternative, online, provider. This could increase overall antibiotic use, with a negative impact on antimicrobial resistance, and on population health in general [17–19]. The preferences of the general public regarding such services are, however, unknown, and data on the use of online consultations are unavailable (outside a research context) [20–22], so the likely scale of this impact is unclear.
We aimed to understand public preferences for seeking online consultations in the UK, in the context of having symptoms for which antibiotics may be appropriate. In the absence of revealed preference data, our approach was to conduct a discrete choice experiment (DCE). A DCE is a quantitative survey-based approach that has been widely used in health economics in a variety of clinical contexts [23–25]. The method involves asking a series of questions in which respondents state their preference for healthcare interventions or services in hypothetical alternative scenarios. In so doing, respondents implicitly make trade-offs between the attributes of these interventions or services. Regression analysis is then used to model respondents’ preferences based on their choices.
Here we present the results of a DCE conducted online amongst members of the UK public. We investigate the preferences of respondents for seeking antibiotic treatment via a consultation with a primary care physician, either via their local medical centre or online. We quantify the relative preferences of respondents for attributes such as consultation format and cost, and examine preference heterogeneity amongst respondents.
Materials and Methods
The design, administration and analysis of the DCE survey followed good practice guidelines [26].
Specifying the Choice Alternatives
Attributes (described in the DCE as ‘pieces of information’ or ‘categories of information’) and levels (the values that an attribute can take) for the choice alternatives were identified via a literature review. This identified studies providing information on attributes that might be relevant to members of the public when seeking a consultation regarding possible antibiotic treatment. We identified 11 potentially relevant attributes (Appendix 1). A convenience sample of seven colleagues (including health economists, clinicians and clinical scientists) rated and commented on the importance of each attribute when seeking a consultation (such convenience samples have been used in other healthcare DCEs [27–29]). Mean importance scores were calculated and five attributes were selected that were ranked highly by all participants and captured the key characteristics of potential choice alternatives: consultation waiting time, GP reputation, consultation cost, the process by which antibiotics would be collected, and the similarity of the consultation to a traditional ‘face-to-face’ appointment.
Each choice question presented two alternatives: a consultation with a GP who is based at the respondent’s local medical centre (which could be face-to-face or virtual) or a consultation with a GP via an online provider. Levels were then identified for each attribute, informed by the literature search, comments from the ranking exercise, and the nature of the choice alternatives. For some attributes, these levels were not common to both choice alternatives, because of fundamental differences in the nature of traditional and online consultations. For example, the cost of a consultation was always £0 at the respondent’s local medical centre (because such appointments are free in the NHS), but could vary between £0 and £45 for an online consultation (these levels were set after reviewing current online providers; for example, The GP Service currently charge £25 for a 10-min consultation) [30]. Similarly, consultations via the respondent’s local medical centre could be face-to-face (in person), or take place via video call or voice call, whereas online consultations could take place via video call, voice call, instant messaging service or by submitting an electronic form. The attributes and levels that were presented to respondents are described in Table 1.
Table 1.
Attributes and levels presented to respondents for each choice alternative
| Attributea | Levela | This level is an option for a consultation… | |
|---|---|---|---|
| …at your local medical centre | …via the internet | ||
| How similar your consultation is to a traditional ‘face-to-face’ appointment |
1. Exactly the same [FACETOFACE1] You have a face-to-face consultation in person. This either takes place at your local medical centre or at your home. You can see and hear the GP, and they can conduct a physical examination |
✔ | ✘ |
|
2. Very similar [FACETOFACE2] You have a consultation over the phone via video call. This could be via a mobile phone or via the internet (e.g. Skype). You can see and hear the GP, but they cannot conduct a physical examination |
✔ | ✔ | |
|
3. Somewhat similar [FACETOFACE3] You have a consultation over the phone via voice call (i.e. no video). This could be via a landline, a mobile phone or the internet (e.g. Skype). You can hear the GP, but you cannot see them, and they cannot conduct a physical examination |
✔ | ✔ | |
|
4. Not very similar [FACETOFACE4] Your consultation takes place via an instant messaging service. You cannot see or hear the GP, and they cannot conduct a physical examination |
✘ | ✔ | |
|
5. Not similar at all [reference level—variable not labelled] You submit an electronic form describing your symptoms, then receive a response later by email. You cannot see or hear the GP, and they cannot conduct a physical examination |
✘ | ✔ | |
| How long you wait for a consultation [TIME] | 0.25 h (15 min) | ✘ | ✔ |
| 2 h | ✘ | ✔ | |
| 6 h | ✔ | ✔ | |
| 24 h | ✔ | ✔ | |
| 72 h | ✔ | ✘ | |
| 168 h (1 week) | ✔ | ✘ | |
| The reputation of the GP | Two stars [REPUTATION1] | ✔ | ✔ |
| Three stars [REPUTATION2] | ✔ | ✔ | |
| Four stars [REPUTATION3] | ✔ | ✔ | |
|
Five stars [reference level—variable not labelled |
✔ | ✔ | |
| Collecting your antibiotics |
1. It is very convenient to collect the antibiotics that you have been prescribed [COLLECTION1] The antibiotics would be sent to you by post (next day delivery), either to your workplace or your home. You would not need to visit the pharmacy yourself |
✘ | ✔ |
|
2. It is somewhat convenient to collect the antibiotics that you have been prescribed [COLLECTION2] You would be given a paper prescription at your local medical centre. There is a pharmacy located in the same building as your local medical centre. You would be able to take your prescription to this pharmacy to collect your antibiotics |
✔ | ✘ | |
|
3. It is somewhat inconvenient to collect the antibiotics that you have been prescribed [COLLECTION3]. Your prescription would be sent by email to a pharmacy of your choice at the end of your consultation. You would need to visit this pharmacy to collect your antibiotics. This pharmacy is not located in the same building as your local medical centre |
✔ | ✔ | |
|
4. It is very inconvenient to collect the antibiotics that you have been prescribed [reference level—variable not labelled] You would be given a paper prescription at your local medical centre. There is not a pharmacy located in the same building as your local medical centre. You would have to take your prescription to a pharmacy at a different location to collect your antibiotics |
✔ | ✘ | |
| The cost of the consultation [COST] | £0 | ✔ | ✔ |
| £15 | ✘ | ✔ | |
| £30 | ✘ | ✔ | |
| £45 | ✘ | ✔ | |
aThe label used for each attribute coefficient in the choice model is given in the format: [COEFFICIENT LABEL]. When this label appears in the ‘Attribute’ column, it indicates that this attribute was assumed to be linear and thus treated as a continuous variable in regression models. When the label appears in the ‘Level’ column, this indicates that this attribute was treated as an effects-coded categorical variable in regression models
Constructing the Choice Questions
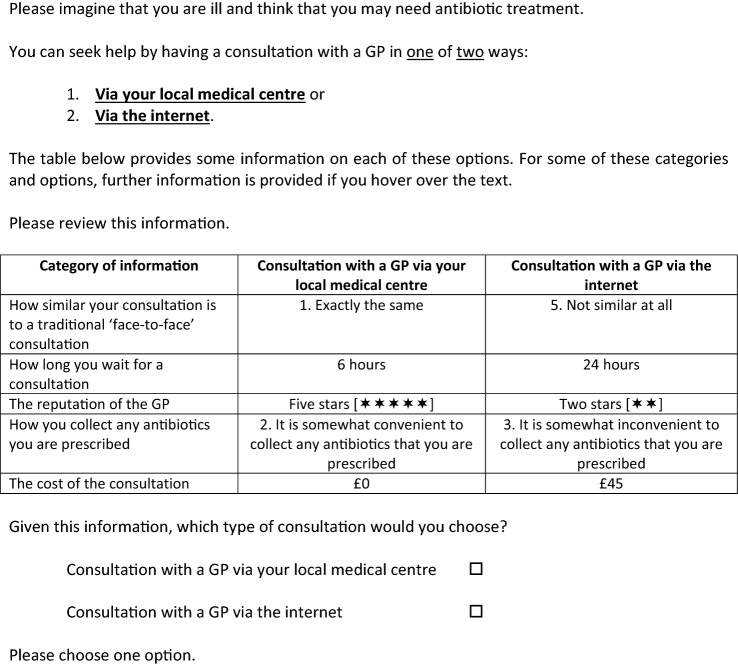
In each choice question, respondents were presented with the same hypothetical situation (Fig. 1), in which they were asked to imagine they were ill and thought that they might need antibiotic treatment. They could seek help by having a consultation with a GP at their local medical centre (face-to-face or virtually) or via an online provider. Respondents were presented with five attributes for the two choice alternatives (the levels for these attributes varying in each choice question). Respondents could view full descriptions of the attribute levels by hovering over these levels with their mouse. The alternatives were labelled ‘Consultation with a GP via your local medical centre’ and ‘Consultation with a GP via the internet’. These labels allowed the strength of respondents’ preferences for each type of consultation to be estimated, independent of the attributes of that type of consultation in each choice. Finally, respondents were asked which type of consultation they would choose. Overall, respondents were presented with 16 choice questions, which is considered an acceptable number [23, 31, 32].
Fig. 1.
Hypothetical choice situation presented to respondents—practice question
Producing the DCE Design
The levels that were presented for the two alternatives in each choice question were generated using an experimental design, produced using Ngene [33]. This was a d-efficient design that exhibited level balance. The design was not blocked, and question order was not randomised (further details presented in Appendix 2).
Assembling the Survey
The DCE was conducted as an online survey (Appendix 3). Respondents viewed a welcome page (where they provided informed consent), followed by information on antibiotics and antibiotic prescribing, instructions on how to complete the survey and a description of the attributes and levels. Respondents were then asked to rank the attributes in terms of their relative importance when making the choice decisions, and to complete a practice choice question (Fig. 1). This practice question was designed so that a consultation with a GP via the respondent’s local medical centre was unequivocally the best choice that respondents could make given the levels presented for each attribute, unless they had strong preferences for a consultation with an online provider, regardless of the associated attributes. Respondents then completed the 16 choice questions and undertook a second ranking exercise to enable us to ascertain whether their rankings changed during survey completion. Finally, information was collected on respondent characteristics to help interpret the DCE results, including antibiotic use, healthcare seeking behaviour, understanding of the symptoms that are associated with needing antibiotics and socio-demographics.
Piloting and Data Collection
The DCE was conducted using a general population panel, accessed via Research Now SSI, an online market research provider. Data collection took place online in July and August 2018. Panel members were recruited by email, and were sampled to be representative of the UK population in terms of gender, age, ethnicity and geographic region. Respondents could complete the survey via desktop or laptop computers (but not smartphones or tablets). A pilot study was undertaken in 81 panel members. The results of this pilot study were used to optimise the experimental design of the main survey (details in Appendix 2). In both the pilot and the main survey, respondents were excluded if they were ‘speeders’ (completed the survey in less than 33% of the median completion time) or provided irrelevant answers to free-text questions.
Data Analysis
Data analysis was undertaken using Stata [34]. The choices made by each respondent were reviewed to determine whether respondents had dominant preferences (i.e. always selected the choice alternative with the best level of a particular attribute, for example, the lowest cost alternative, or the alternative with the shortest waiting time). Further details on the dominance calculations are provided in Appendix 4.
Two models of choice behaviour were estimated using regression analysis (model development described in Appendix 5). In both models, the magnitude of the coefficients indicated the strength of respondents’ preferences for the various attributes and levels (often referred to as the ‘utility’ that respondents derive from these attributes and levels in a choice alternative). Two of the five attributes (TIME and COST) were assumed to be linear and thus coded as continuous variables. Categorical coding (effects coding) was used for the other three attributes.
Model 1 used mixed logit regression analysis. This approach allowed for preference heterogeneity, which was anticipated in this sample population and clinical context [35, 36]. A step-by-step process was applied to determine the specification of this model, described in Appendix 5. The final model used 200 Halton draws, allowed for correlation between attributes, and treated six attributes as random parameters (the constant for a consultation at the respondent’s local medical centre, FACETOFACE1, TIME, REPUTATION1, COLLECTION1 and COST). This model was used to evaluate the impact of different attributes and levels on the probability of selecting either ‘Consultation with a GP via your local medical centre’ or ‘Consultation with a GP via the internet’. We also calculated respondent willingness-to-pay for different attributes of the choice alternatives (by dividing the coefficient for the attribute (or attribute level) of interest by the negative of the coefficient for the COST attribute), estimated the extent to which respondents were prepared to trade off one attribute for another and calculated the value (or utility) attached to different combinations of attribute levels. Finally, we evaluated the number of correct choice predictions made by the model by using the coefficient estimates to calculate the utility associated with each choice alternative, then predicting choices assuming that respondents selected the alternative with the highest utility. These choices were then compared with the actual choices made by respondents.
Model 2 explored whether the heterogeneity identified in Model 1 could be explained by categorising respondents into different groups (latent class analysis). Respondents were allocated into groups based on information on model fit and interpretability of class membership (further detail provided in Appendix 5). In both models, a positive (negative) coefficient indicated that a respondent would be more (less) likely to choose an alternative with that attribute or attribute level.
Results
A total of 987 members of the UK general public accessed the survey in July and August 2018 (Appendix 6). Of those who started the survey, 200 did not complete it, 41 did not progress past the screening questions, and 12 were excluded for being ‘speeders’ or providing irrelevant answers to the open-ended questions. In total, 734 respondents (74%) successfully completed the survey and were included in the analysis.
Respondent Characteristics
The respondents’ gender distribution, age, ethnicity and geographic region were comparable to those of the UK as a whole (Table 2 and Appendix 6) [37]. Respondents had used antibiotics a mean 0.8 times in the past 12 months (Table 3). Two-thirds of respondents (68%) lived within 15 min of the medical centre where they would usually consult a GP, and half (52%) could arrange a consultation at this medical centre within 24 h. Most respondents (57%) would usually collect their prescriptions from a pharmacy in a different building to their local medical centre. Half of the respondents had previously consulted with a GP at their local medical centre by telephone, and few had ever had any type of consultation with a GP online. Respondents who had experienced an online consultation were younger, more likely to have dependent children living with them and less likely to live within 15 min of their medical centre. Appendix 6 presents further information on differences between these groups of respondents, as well as information on their personality traits and the symptoms that they associated with needing antibiotic treatment. Most respondents found the survey easy to complete: the mean difficulty score was 2.4 on a 0–7 scale (where 1 = very easy and 7 = very difficult).
Table 2.
Descriptive statistics for respondents
| Variable | Value |
|---|---|
| Male, n (%) | 359 (49%) |
| Age (years) of respondents, n (%) | |
| 18–24 | 86 (12%) |
| 25–34 | 121 (16%) |
| 35–44 | 127 (17%) |
| 45–54 | 133 (18%) |
| 55–64 | 109 (15%) |
| ≥ 65 | 158 (22%) |
| Mean age (SD) | 47 (17) |
| Ethnicity, n (%) | |
| White | 633 (86%) |
| Mixed/multiple ethnic groups | 16 (2%) |
| Black/African/Caribbean/Black British | 21 (3%) |
| Asian/Asian British | 55 (7%) |
| Other ethnic groups | 4 (1%) |
| Prefer not to say | 5 (1%) |
| Geographic region, n (%) | |
| England | 613 (84%) |
| Northern Ireland | 21 (3%) |
| Scotland | 63 (9%) |
| Wales | 37 (5%) |
| Employment status, n (%) | |
| Employeda | 406 (55%) |
| Student | 31 (4%) |
| Long-term sick or disabled | 32 (4%) |
| Carer | 49 (7%) |
| Retired | 160 (22%) |
| Unemployed | 55 (7%) |
| Otherb | 1 (< 1%) |
| Level of education, n (%) | |
| None | 3 (< 1%) |
| Up to GCSEs level | 168 (23%) |
| Post-16 educationc | 253 (34%) |
| Degree level educationd | 291 (40%) |
| Othere | 3 (< 1%) |
| Currently married, in a civil partnership or living with a partner, n (%) | 463 (63%) |
| Gross household income, n (%) | |
| Up to £9999 | 61 (8%) |
| £10,000–£19,999 | 147 (20%) |
| £20,000–£29,999 | 140 (19%) |
| £30,000–£39,999 | 114 (16%) |
| £40,000–£49,999 | 83 (11%) |
| £50,000–£74,999 | 78 (11%) |
| £75,000–£99,999 | 30 (4%) |
| £100,000 or more | 11 (2%) |
| Prefer not to say | 70 (10%) |
| Number of adults living in household, mean (SD) | 2.2 (1.0) |
| Respondents with dependent children living with them, n (%) | 195 (27%) |
| Number of dependent children living with respondents, mean (SD)f | 1.8 (0.8) |
| Risk score out of 10, mean (SD)g | 4.9 (2.7) |
N = 734 unless stated
SD standard deviation
aIncludes respondents who were employed or self-employed, either full-time or part-time
bUnemployed and part-time student
cIncludes those who selected international baccalaureate, higher education certificate or diploma, technical or vocational qualification, transition year programme, or ‘A’ levels or ‘AS’ levels or Scottish Higher Grade
dIncludes those who selected undergraduate degree, postgraduate degree, postgraduate certificate or diploma, professional qualification comparable to undergraduate degree, or doctorate
eSecondary school (N = 2); unclear (N = 1)
fN = 195
gRespondents were asked to rate their attitude to risk on a zero to ten scale, where zero means “risk averse” and ten means “fully prepared to take risks”
Table 3.
Healthcare consumption by respondents
| Variable | Value |
|---|---|
| Number of times respondents had used antibiotics in the past 12 months, mean (SD)a | 0.8 (1.4) |
| Time it takes respondents to travel to their usual medical centre, n (%) | |
| 0–15 min | 498 (68%) |
| 16–30 min | 182 (25%) |
| 31–45 min | 29 (4%) |
| 46–60 min | 12 (2%) |
| 61–75 min | 4 (1%) |
| 76–90 min | 3 (< 1%) |
| > 90 min | 6 (1%) |
| Usual mode of transport taken to visit this medical centre, n (%) | |
| Public transport (e.g. privately arranged taxi, bus, train) | 81 (11%) |
| Hospital arranged transport (e.g. ambulance, hospital arranged taxi) | 4 (1%) |
| Private transport (e.g. private car, motorcycle, bicycle) | 342 (47%) |
| Walk | 307 (42%) |
| Waiting time to get a consultation at your local medical centre, n (%) | |
| Less than 6 h | 177 (24%) |
| Between 6 h and 24 h (1 day) | 205 (28%) |
| Between 24 h (1 day) and 72 h (3 days) | 184 (25%) |
| Between 72 h (3 days) and 168 h (7 days) | 93 (13%) |
| More than 168 h (7 days) | 75 (10%) |
| Number (%) of respondents that have had different types of consultations | |
| Face-to-face consultation with a GP at your local medical centre | 721 (98%) |
| Phone consultation with a GP at your local medical centre | 365 (50%) |
| Video consultation with a GP at your local medical centre | 17 (2%) |
| Phone consultation with a GP via the internet | 48 (7%) |
| Video consultation with a GP via the internet | 22 (3%) |
| Consultation using an instant messaging service with a GP via the internet | 30 (4%) |
| Consultation with a GP via the internet in which you submit a form describing your symptoms and receive a response by email | 40 (5%) |
| Pharmacy in the same building as respondent’s local medical centre, n (%) | |
| Yes | 310 (42%) |
| No | 405 (55%) |
| Not sure | 19 (3%) |
| Normal method of collecting prescriptions, n (%) | |
| My prescriptions are sent to me in the postb | 55 (7%) |
| I collect my prescriptions from a pharmacy that is in the same building as my local medical centre | 236 (32%) |
| I collect my prescriptions from a pharmacy that is not in the same building as my local medical centre | 415 (57%) |
| Otherc | 28 (4%) |
N = 734
GP general practitioner, SD standard deviation
aMedian = 0; interquartile range 0–1
bThis category includes respondents whose prescriptions are delivered to their door by a local pharmacy
cPick up prescription directly from surgery (N = 13); Collect prescription from pharmacy of their choice (N = 7); Have never needed a prescription (N = 4); Collected by third party on behalf of respondent (N = 2); I don’t know (N = 2)
Appendix 7 presents the results of the ranking exercise. There were only minor differences in attribute rankings before and after completing the choice questions
DCE Results
In the practice question, 699 respondents (95%) chose a consultation via their local medical centre. This question was designed so that this was the best choice that respondents could make given the levels presented for each attribute (Appendix 7). All respondents completed all 16 choice questions, yielding 11,744 choices in total. ‘Consultation at your local medical centre’ was selected in 8288 (71%) of these choices. Appendix 4 reports the results of the dominance calculations (i.e., whether respondents always selected the choice alternative with the best level of a particular attribute). Two hundred and seventy-nine respondents (38%) always selected the choice alternative that was cheapest, while 195 (27%) selected ‘Consultation at your local medical centre’ in every choice question.
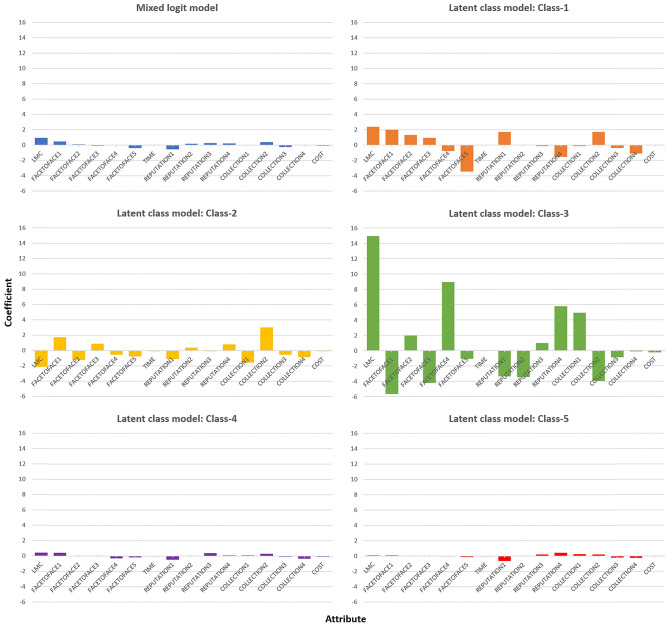
Model 1 The mixed logit regression model (Table 4, Fig. 2 and Appendix 8) was a good fit for the underlying data; it correctly predicted 90% of the choices made by respondents. The estimated effect for a consultation with a GP via the respondent’s local medical centre (denoted ‘LMC’ in Table 4) had the highest value, indicating that respondents had a strong preference for this alternative rather than an online consultation. The levels for the FACETOFACE attribute were ordered from one to five by decreasing similarity to a traditional ‘face-to-face’ appointment. Preferences for consultations broadly decreased as these levels increased, indicating that people preferred consultations that were most like traditional consultations. Negative coefficients were also observed for the TIME and COST attributes, indicating that people preferred to wait less and pay less. The levels for the REPUTATION attribute were ordered from one to four by improving GP reputation. Preferences for consultations broadly increased as these levels increased, indicating a preference for GPs with a better reputation. Finally, the levels for the COLLECTION attribute were ordered by increasing inconvenience to collect any antibiotics that are issued. However, preferences for consultations did not decrease as these levels increased, as might have been expected: COLLECTION2 (taking a paper prescription to a pharmacy located in the same building as your local medical centre) had the largest coefficient, and was the only positive COLLECTION coefficient, indicating a preference for this approach.
Table 4.
Attributes that affect preferences for seeking online consultations—mixed logit and latent class regression analysis results
| Attributea | Coefficientb | |||||
|---|---|---|---|---|---|---|
| Model 1 (mixed logit) | Model 2 (latent class) | |||||
| Mixed logit | Class-1 | Class-2 | Class-3 | Class-4 | Class-5 | |
| LMC | 0.920* | 2.367* | − 2.150 | 14.959 | 0.418* | 0.082 |
| FACETOFACE1 | 0.449* | 1.992 | 1.726* | − 5.637* | 0.444* | 0.095 |
| FACETOFACE2 | 0.071 | 1.312* | − 1.232 | 1.970 | 0.013 | 0.053 |
| FACETOFACE3 | 0.087* | 0.915* | 0.867 | − 4.220 | 0.006 | 0.012 |
| FACETOFACE4 | − 0.054 | − 0.774 | − 0.584 | 8.943 | − 0.294 | − 0.039 |
| FACETOFACE5c | − 0.380 | − 3.445 | − 0.777 | − 1.056 | − 0.169 | − 0.121 |
| TIME (per additional hour) | − 0.012* | 0.004 | − 0.079* | − 0.039* | − 0.026* | − 0.003* |
| REPUTATION1 | − 0.557* | 1.703 | − 1.096* | − 3.343 | − 0.463* | − 0.645* |
| REPUTATION2 | 0.142* | 0.005 | 0.394 | − 3.434* | 0.013 | 0.029 |
| REPUTATION3 | 0.237* | − 0.150 | − 0.084 | 0.973 | 0.369* | 0.198* |
| REPUTATION4c | 0.178 | − 1.558 | 0.787 | 5.804 | 0.081 | 0.419 |
| COLLECTION1 | − 0.042 | − 0.156 | − 1.581* | 4.942 | 0.103 | 0.265* |
| COLLECTION2 | 0.358* | 1.680 | 3.013* | − 3.932 | 0.302* | 0.215* |
| COLLECTION3 | − 0.255* | − 0.420 | − 0.556 | − 0.895 | − 0.080 | − 0.221* |
| COLLECTION4c | − 0.061 | − 1.105 | − 0.876 | − 0.115 | − 0.325 | − 0.260 |
| COST (per additional £) | − 0.085* | − 0.003 | − 0.077* | − 0.262 | − 0.099* | − 0.014* |
| Mean class share (standard deviation) | N/A | 31% (45%) | 16% (35%) | 14% (32%) | 22% (39%) | 18% (35%) |
N/A not applicable
aAttribute descriptions: LMC = constant for local medical centre; FACETOFACE = How similar your consultation is to a traditional ‘face-to-face’ appointment (1 = Exactly the same, 2 = Very similar,3 = Somewhat similar, 4 = Not very similar, 5 = Not similar at all [reference level].); TIME = How long you wait for a consultation; REPUTATION = The reputation of the GP (1 = Two stars, 2 = Three stars,3 = Four stars, 4 = Five stars [reference level].); COLLECTION = How you collect any antibiotics you are prescribed (1 = very convenient, 2 = Somewhat convenient, 3 = Somewhat inconvenient, 4 = very inconvenient [reference level]); COST = The cost of the consultation
bCoefficients that are starred were significant at p < 0.05
cThese attributes were coded as effects-coded categorical variables. The coefficients of the reference levels (FACETOFACE5, REPUTATION4 and COLLECTION4) were calculated as the negative sum of the coefficients of the other levels
Fig. 2.
Mixed logit and latent class regression analysis results
The inclusion of a cost attribute allowed us to estimate respondents’ implicit willingness-to-pay for different attributes and levels. Respondents were willing to pay £11 (95% confidence interval: £8–£14) for a consultation with a GP via their local medical centre if the alternative was a consultation with an online provider. They were also willing to pay a further £4–£10 if this was a traditional face-to-face consultation instead of one of the alternative consultation formats (video call, voice call, instant messaging service, electronic form) (Appendix 8). When trade-offs between attributes were quantified using the TIME attribute, respondents required a 77-h (~ 3 day) reduction in waiting time to accept a consultation with a GP via an online provider instead of via their local medical centre. When the model coefficients were used to calculate the value attached to different combinations of attribute levels, there were no scenarios in which a consultation via an online provider had a higher value than a consultation via the respondent’s local medical centre, unless the cost of a consultation via an online provider is £3.41 or lower (Appendix 8).
Model 2 The latent class analysis identified five groups of respondents with different preferences (Table 4 and Fig. 2). Descriptive statistics for these five groups are presented in Appendix 9. Two groups are particularly notable. Respondents in Class-1 (31% of all respondents) had a strong preference for ‘traditional’ face-to-face appointments at their local medical centre and for convenience when collecting their prescription. Other attributes were not important to these respondents. Compared to the whole sample, these respondents were more likely to be male, of older age, of white ethnicity, retired and living close to the medical centre where they would usually consult a GP.
Conversely, respondents in Class-5 (18% of all respondents) did not have strong preferences concerning type of consultation or consultation location: ‘Consultation at your local medical centre’ was only selected in 50% of the choices made by these respondents. However, they did have strong preferences for consulting a GP with a good reputation, for convenience when collecting a prescription, for short waiting times and for minimising consultation cost. Compared to the whole sample, respondents in this group were more likely to be female, younger (mean age 36 years), of non-white ethnicity, working full-time and unmarried. They were also more likely to use antibiotics frequently, have a high household income, have dependent children living with them, live further away from the medical centre where they would usually consult a GP and have a waiting time of a day or less to get a consultation at this medical centre. These respondents could be described as ‘busy young professionals’.
Discussion
We investigated the preferences of members of the UK general public for seeking online consultations from different providers, in the context of having symptoms for which antibiotics may be appropriate. We found that members of the public placed a high value on having a consultation with a GP via their local medical centre rather than via an online provider, and also valued shorter consultation waiting times, cheaper consultations and clinicians with good reputations. Notably, respondents were willing to pay £11 for a consultation with a GP via their local medical centre (although such consultations are free in the UK), regardless of consultation format, rather than have a consultation via an online provider. They were willing to pay a further £5 if this was a traditional face-to-face consultation. Respondents were, however, unwilling to pay for consultations by telephone, video, instant messaging service, or by submitting an electronic form and receiving a response by email. This was regardless of the type of provider.
Interestingly, respondent preferences exhibited marked heterogeneity; five population subgroups were identified with different preferences. In particular, one group who could be characterised as ‘busy young professionals’ showed a lower strength of preference for traditional consultations and a higher strength of preference for convenience, prioritising a quick consultation outcome. This finding is potentially important. One interpretation is that these individuals may be more willing to accept alternative consultation formats (e.g., video, phone) via their local medical centre. However, for the same reasons, these individuals might also be willing to seek a consultation with an online provider. If such providers adopt a more permissive approach to antimicrobial stewardship than the NHS, as has been suggested [5–7], this may lead to increased antimicrobial resistance, negatively impacting on population health. Indeed, evidence is emerging that children with acute respiratory infections are more likely to receive antibiotics via online consultations [38]. The impact of this prescribing behaviour could be exacerbated by the fact that the general public have a relatively poor understanding of the symptoms that indicate a need for antibiotic treatment [39, 40].
The characteristics of survey respondents differed by previous experience of online providers; those with experience were younger and less likely to be of white ethnicity. This could have implications for equity of access. Although the provision of primary care consultations in a wider variety of formats (as per recent commitments by NHS England) [4] could improve access for some patient subgroups, if this leads to a reduction in the availability of face-to-face consultations, this could have negative consequences for other patients [41]. Such variations in access to care can have notable health consequences; a Scottish study found that patients with worse access to care had more long-term illness, more multimorbidity and more chronic health problems [42].
Overall, our results suggest that in mid-2018 there was little appetite amongst the UK general public to seek consultations with GPs via online providers, or to seek consultations via their local medical centre that are not face-to-face. That said, we did observe heterogeneity in respondents’ preferences. Primary care physicians might therefore find it beneficial to collect information on the preferences of their patients for different consultation formats. This would allow access to different formats to be tailored according to patient preferences, which could allow limited GP time to be allocated more efficiently to patients. In addition, this survey presents a snapshot of general public preferences at one point in time. Both technology and the social norms that guide the use of technology are constantly evolving, so it is possible that preferences for seeking alternative consultation formats will also change. These changes may be accelerated in light of the 2019–2021 COVID-19 pandemic, during which face-to-face primary care appointments were largely suspended and replaced with virtual appointments in the UK and elsewhere [43]. There have already been calls for research into how appropriate video consultations are for dealing with the COVID-19 pandemic [44], and the impact of this pandemic on patient preferences should also be explored.
For policymakers attempting to minimise inappropriate use of antibiotics, these results suggest that interventions aiming to discourage the public from seeking antibiotic treatment from online providers may have little effect on the inappropriate use of antibiotics, unless such interventions are targeted at population subgroups more inclined to accept alternative types of consultations. Other approaches may be more successful than general public health messages, such as providing social norm feedback to high prescribers of antibiotics in general practice [11], or shared decision-making between patients and doctors [45].
To our knowledge, this is the first study to quantify the trade-offs that members of the public are willing to make when seeking a medical consultation via a variety of formats in a primary care setting. Study strengths include the recruitment of a large nationally representative sample, and the use of regression approaches that allowed us to identify population subgroups with different preferences. These results may facilitate the design of targeted interventions in the context of antibiotic treatment, although qualitative research work that examines the motivations and potential behaviours of the UK public is required to more fully understand preference heterogeneity in this context.
Our study has several limitations. First, attribute interactions were not considered in the experimental design of our DCE because they could not be specified for all choice alternatives. In addition, constraints preventing specific combinations of attribute levels could not be accommodated by the experimental design. These two factors may have reduced the face validity of the choice questions in our DCE. Appendix 2 discusses these limitations in more detail.
Second, the setting for this study was the UK NHS. In countries where patients more frequently pay directly for healthcare, or where over-the-counter sales are possible for a wide range of drugs, preferences for paid-for online consultations with private providers may differ [18]. In addition, there may be between-country differences in thresholds to consult—as previously observed for uncomplicated urinary tract infections, for example [46]—that should be borne in mind when generalising these results beyond the UK setting [47].
Third, the choice questions in our survey did not indicate a specific illness, which ensures that our results are broadly generalisable to different clinical contexts. However, preferences may differ by type of infection, or according to whether a patient is seeking treatment with antibiotics or another class of drug. For example, patients with recurrent urinary tract infections might be more willing to seek antibiotic treatment via an online or phone consultation.
Fourth, survey respondents were recruited from an online panel. This meant that, unfortunately, we could not conduct interviews with respondents after they had completed the survey to review their understanding of the choice questions, or to collect information on any assumptions they made about the choice context beyond the description that we provided (for example, regarding severity of illness or the likelihood of getting the right treatment for their condition). Furthermore, respondents might not have been representative of the general population in terms of use of online resources. However, even in this experienced population there was little appetite for consultations via online providers, so our conclusion regarding population appetite for such consultations may be conservative.
Fifth, it has been suggested that scale-adjusted latent class models could be estimated to allow for scale heterogeneity when defining latent class models [48]. However, it was not possible to estimate such a model using Stata. A further issue related to model specification is that we assumed linearity for the TIME attribute, but this assumption may not hold as the attribute level varies between 15 min and 1 week. A model that formally tested this assumption by adding an additional quadratic term for TIME yielded inconclusive results: the model fit improved in terms of AIC, but not in terms of BIC, and the quadratic term was not significant.
Sixth, Hole and Kolstad [36] have suggested that a willingness-to-pay space model is used when the cost attribute in a DCE is included as a random parameter, instead of estimating willingness-to-pay in preference space. However, none of our models applying this approach converged.
Finally, we did not collect data on the expectations of respondents regarding likelihood of antibiotic receipt, or on their ability to access consultations in different formats. Such information would allow subgroups of respondents with an appetite for different consultation formats—and the ability to access these formats—to be identified more precisely. Moreover, reported actions in a survey may not reflect physical choices in practice.
Conclusions
There has been a vast increase in the use of online services in all aspects of life since the start of the twenty-first century, and primary care is no exception; consultations with physicians are now available in a variety of formats, including video calls. However, there is rising concern that private providers such as online pharmacies—whose existence has been enabled by these technological advances—may have lower thresholds for prescribing certain drugs, which could impact on population health. This is a particular consideration for antibiotic prescriptions. If patients increasingly seek consultations with private providers regarding antibiotic treatment, and these providers adopt a more permissive approach to antimicrobial stewardship than national healthcare systems, this could have a negative impact on antimicrobial resistance. This study suggests that in the pre-coronavirus UK, there was limited appetite amongst the general public to seek antibiotic treatment from such providers, and a strong preference for face-to-face appointments. However, this population-level finding masks considerable preference heterogeneity, and specific population subgroups might be more open to using private online services. There is therefore a non-negligible risk that these services could increase the burden of antimicrobial resistance, impacting on population health. Given this, it will be important to monitor prescriptions from online providers going forward, and any interventions aiming to discourage the public from seeking antibiotic treatment via these providers could be targeted at those who are more inclined to accept these alternative types of consultation.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the members of the general public who completed the discrete choice experiment (DCE), and Research Now SSI for conducting the DCE. We also thank the members of our convenience sample at the University of Oxford for assisting with the specification of the choice questions and the selection of attributes and levels.
Declarations
Funding
This research was funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Healthcare Associated Infections and Antimicrobial Resistance at the University of Oxford in partnership with Public Health England (PHE) [HPRU-2012-10041 and NIHR200915], and supported by the NIHR Oxford Biomedical Research Centre. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health or PHE. DWC, TP, CB and ASW are NIHR Senior Investigators.
Conflict of interest
None.
Ethical approval
This study was approved by the University of Oxford Central University Research Ethics Committee [R57626/RE001].
Consent to participate
All participants were provided with participant information when they entered the online survey and consented to participate in the study.
Consent for publication
All participants were provided with participant information when they entered the online survey and consented to publication of the results of this study.
Author contributions
JB: methodology, formal analysis, investigation, writing—original draft, project administration. LSJR: methodology, investigation, writing—review and editing. LM: methodology, investigation, writing—review and editing. KBP: methodology, investigation, writing—review and editing. JVR: writing—review and editing. LA: methodology, investigation, writing—review and editing. DWC: conceptualization, writing—review and editing, supervision, project administration, funding acquisition. TP: conceptualization, writing—review and editing, supervision, project administration, funding acquisition. CCB: conceptualization, writing—review and editing. ASW: conceptualization, writing—review and editing, supervision, project administration, funding acquisition. SW: methodology, conceptualization, writing—review and editing, supervision, project administration, funding acquisition
Data Availability Statement
De-identified data that were collected for this study can be obtained from the Oxford University Research Archive.
Code Availability Statement
Available on request.
References
- 1.National Health Service. Am I entitled to free prescriptions? https://www.nhs.uk/using-the-nhs/help-with-health-costs/get-help-with-prescription-costs/. Accessed 06 May 20.
- 2.National Health Service. Online consultation funding. https://www.england.nhs.uk/gp/digital-first-primary-care/online-consultation-funding/. Accessed 06 May 20.
- 3.National Health Service. Using online consultations in primary care: implementation toolkit. https://www.england.nhs.uk/publication/using-online-consultations-in-primary-care-implementation-toolkit/. Accessed 06 May 20.
- 4.National Health Service. Digital First Primary Care. https://www.england.nhs.uk/gp/digital-first-primary-care/. Accessed 06 May 20.
- 5.Limb M. Regulator takes action against four online pharmacies. BMJ. 2017;357:j1784. doi: 10.1136/bmj.j1784. [DOI] [PubMed] [Google Scholar]
- 6.Iacobucci G. Online GP service prescribed drugs without safety checks, says CQC. BMJ. 2017;357:j3194. doi: 10.1136/bmj.j3194. [DOI] [PubMed] [Google Scholar]
- 7.Stewart K. Are private online GP consultations safe? Prescriber. 2016;27(10):22–29. doi: 10.1002/psb.1504. [DOI] [Google Scholar]
- 8.House of Commons Library. Medicine statistics: GP prescribing by constituency, 2015. https://commonslibrary.parliament.uk/research-briefings/cbp-7161/. Accessed 06 May 20.
- 9.The Review on Antimicrobial Resistance. Tackling drug-resistant infections globally: Final report and recommendations, 2016.
- 10.Smieszek T, Pouwels KB, Dolk FCK, et al. Potential for reducing inappropriate antibiotic prescribing in English primary care. J Antimicrob Chemother. 2018;73(suppl_2):ii36–ii43. doi: 10.1093/jac/dkx500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gong CL, Hay JW, Meeker D, Doctor JN. Prescriber preferences for behavioural economics interventions to improve treatment of acute respiratory infections: a discrete choice experiment. BMJ Open. 2016;6(9):e012739. doi: 10.1136/bmjopen-2016-012739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chemother. 2014;69(1):234–240. doi: 10.1093/jac/dkt301. [DOI] [PubMed] [Google Scholar]
- 13.Dolk FCK, Pouwels KB, Smith DRM, Robotham JV, Smieszek T. Antibiotics in primary care in England: which antibiotics are prescribed and for which conditions? J Antimicrob Chemother. 2018;73(suppl_2):ii2–ii10. doi: 10.1093/jac/dkx504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blommaert A, Marais C, Hens N, et al. Determinants of between-country differences in ambulatory antibiotic use and antibiotic resistance in Europe: a longitudinal observational study. J Antimicrob Chemother. 2013;69(2):535–547. doi: 10.1093/jac/dkt377. [DOI] [PubMed] [Google Scholar]
- 15.Ashworth M, White P, Jongsma H, Schofield P, Armstrong D. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pract. 2016;66(642):e40–e46. doi: 10.3399/bjgp15X688105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cabral C, Ingram J, Hay AD, Horwood J. “They just say everything's a virus”—Parent's judgment of the credibility of clinician communication in primary care consultations for respiratory tract infections in children: a qualitative study. Patient Educ Couns. 2014;95(2):248–253. doi: 10.1016/j.pec.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 17.Safe, Secure and Controlled: Managing the Supply Chain of Antimicrobials: Wellcome Trust and HM Government, London, 2015.
- 18.Hayhoe B, Greenfield G, Majeed A. Is it getting easier to obtain antibiotics in the UK? Br J Gen Pract. 2019;69(679):54–55. doi: 10.3399/bjgp19X700829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyd SE, Moore LSP, Gilchrist M, et al. Obtaining antibiotics online from within the UK: a cross-sectional study. J Antimicrob Chemother. 2017;72(5):1521–1528. doi: 10.1093/jac/dkx003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards HB, Marques E, Hollingworth W, et al. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open. 2017;7(11):e016901-e. doi: 10.1136/bmjopen-2017-016901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Banks J, Farr M, Salisbury C, et al. Use of an electronic consultation system in primary care: a qualitative interview study. Br J Gen Pract J R Coll Gen Pract. 2018;68(666):e1–e8. doi: 10.3399/bjgp17X693509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cowie J, Calveley E, Bowers G, Bowers J. Evaluation of a digital consultation and self-care advice tool in primary care: a multi-methods study. Int J Environ Res Public Health. 2018;15(5):896. doi: 10.3390/ijerph15050896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buchanan J, Wordsworth S, Schuh A. Patients’ preferences for genomic diagnostic testing in chronic lymphocytic leukaemia: a discrete choice experiment. Patient. 2016;9(6):525–536. doi: 10.1007/s40271-016-0172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker F, Anokye N, de Bekker-Grob EW, et al. Women's preferences for alternative financial incentive schemes for breastfeeding: a discrete choice experiment. PLoS ONE. 2018;13(4):e0194231. doi: 10.1371/journal.pone.0194231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Regier DA, Diorio C, Ethier MC, et al. Discrete choice experiment to evaluate factors that influence preferences for antibiotic prophylaxis in pediatric oncology. PLoS ONE. 2012;7(10):e47470. doi: 10.1371/journal.pone.0047470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health J Int Soc Pharmacoecon Outcomes Res. 2011;14(4):403–413. doi: 10.1016/j.jval.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 27.Luyten J, Kessels R, Goos P, Beutels P. Public preferences for prioritizing preventive and curative health care interventions: a discrete choice experiment. Value Health J Int Soc Pharmacoecon Outcomes Res. 2015;18(2):224–233. doi: 10.1016/j.jval.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 28.Shah KK, Tsuchiya A, Wailoo AJ. Valuing health at the end of life: a stated preference discrete choice experiment. Soc Sci Med. 2015;124:48–56. doi: 10.1016/j.socscimed.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 29.Skedgel CD, Wailoo AJ, Akehurst RL. Choosing vs. allocating: discrete choice experiments and constant-sum paired comparisons for the elicitation of societal preferences. Health Expect. 2015;18(5):1227–1240. doi: 10.1111/hex.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The GP Service. The GP Service—Pricing. https://thegpservice.co.uk/pricing/. Accessed 06 May 20.
- 31.Bech M, Kjaer T, Lauridsen J. Does the number of choice sets matter? Results from a web survey applying a discrete choice experiment. Health Econ. 2011;20(3):273–286. doi: 10.1002/hec.1587. [DOI] [PubMed] [Google Scholar]
- 32.Lancsar E, Louviere J. Deleting 'irrational' responses from discrete choice experiments: a case of investigating or imposing preferences? Health Econ. 2006;15(8):797–811. doi: 10.1002/hec.1104. [DOI] [PubMed] [Google Scholar]
- 33.ChoiceMetrics. Ngene 1.2.0 User Manual & Reference Guide. Australia, 2018.
- 34.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015.
- 35.Hensher D, Green W. The mixed logit model: the state of practice and warnings for the unwary Working paper (Institute of Transport Studies (Australia)): Institute of Transport Studies, the University of Sydney and Monash University, 2002.
- 36.Hole AR, Kolstad JR. Mixed logit estimation of willingness to pay distributions: a comparison of models in preference and WTP space using data from a health-related choice experiment. Empir Econ. 2012;42(2):445–469. doi: 10.1007/s00181-011-0500-1. [DOI] [Google Scholar]
- 37.Office for National Statistics. 2011 Census: Key Statistics and Quick Statistics for local authorities in the United Kingdom—Part 1. 2013.
- 38.Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics. 2019;143(5):e20182491. doi: 10.1542/peds.2018-2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roope LSJ, Tonkin-Crine S, Butler CC, et al. Reducing demand for antibiotic prescriptions: evidence from an online survey of the general public on the interaction between preferences, beliefs and information, United Kingdom, 2015. Euro Surveill. 2018;23(25):1700424. doi: 10.2807/1560-7917.ES.2018.23.25.1700424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.European Commission. Special Eurobarometer 445. Report. Antimicrobial resistance. Brussels: European Commission, 2016.
- 41.Brassel S, Zhang K, Jofre-Bonet M. The Digitalisation of Health Care During COVID-19: Consideration of the Long-Term Consequences. https://www.ohe.org/news/digitalisation-health-care-during-covid-19-consideration-long-term-consequences. Accessed 06 May 20.
- 42.Mercer SW, Watt GC. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5(6):503–510. doi: 10.1370/afm.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.The Health Foundation. How might COVID-19 have affected people’s ability to see their GP? https://www.health.org.uk/news-and-comment/charts-and-infographics/how-might-covid-19-have-affected-peoples-ability-to-see-GP. Accessed 10 May 20.
- 44.Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ. 2020;368:m998. doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 45.Brabers AEM, Hek K, van Dijk L, Verheij RA, van Esch TEM, de Jong JD. Does shared decision-making reduce antibiotic prescribing in primary care? J Antimicrob Chemother. 2018;73(11):3199–3205. doi: 10.1093/jac/dky321. [DOI] [PubMed] [Google Scholar]
- 46.Butler CC, Francis N, Thomas-Jones E, et al. Variations in presentation, management, and patient outcomes of urinary tract infection: a prospective four-country primary care observational cohort study. Br J Gen Pract. 2017;67(665):e830–e841. doi: 10.3399/bjgp17X693641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pouwels KB, Dolk FCK, Smith DRM, Smieszek T, Robotham JV. Explaining variation in antibiotic prescribing between general practices in the UK. J Antimicrob Chemother. 2018;73(suppl_2):ii27–ii35. doi: 10.1093/jac/dkx501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vass CM, Wright S, Burton M, Payne K. Scale heterogeneity in healthcare discrete choice experiments: a primer. Patient. 2018;11(2):167–173. doi: 10.1007/s40271-017-0282-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
De-identified data that were collected for this study can be obtained from the Oxford University Research Archive.