ABSTRACT
The influence of social norms on child feeding is recognized, but guidance is lacking on how to address norms and related perceptions that hinder or support positive nutrition practices. We reviewed recent peer-reviewed and grey literature to summarize social norms relevant to complementary feeding (CF), intervention approaches that address norms, and their impacts on social norms and CF outcomes. Many reports described various norms, customs, and perceptions related to appropriate foods for young children, parenting practices, gender, and family roles, but rarely explored how they motivated behavior. Community engagement and media interventions addressed norms through facilitated discussions, challenging negative norms, portraying positive norms, engaging emotions, and correcting misperceptions. Evaluations of norms-focused interventions reported improved CF practices, but few assessed impacts on social norms. Although multiple contextual factors influence CF practices, evidence suggests the feasibility and effectiveness of addressing social norms as one component of programs to improve CF practices.
Keywords: multisectoral nutrition, gender norms, child feeding interventions, cultural beliefs, infant and young child nutrition, community engagement, low- and lower-middle income countries
Review of the scope of social norms related to complementary feeding, intervention approaches for addressing relevant social norms in low-income and low-middle income countries, and evidence of intervention effectiveness.
Introduction
Complementary feeding (CF) is the period of dietary transition from 6 mo to 2 y of age when exclusive breastfeeding is no longer sufficient to meet all nutritional requirements and children need to consume increasing amounts of a variety of appropriate foods. Adequate CF is essential for child growth and cognitive development, with long-term implications for productive adult lives (1). However, in low- and low–middle- income countries overall, only 1 in 5 children this age receive minimally adequate diets; even lower proportions of children consume adequate diets in parts of South Asia and sub-Saharan Africa (2).
There is widespread consensus on key dimensions that determine the appropriateness of “what young children eat” and “how and when they are fed” (1), as well as global guidance on recommended CF practices (3). Less is known about how to design and deliver effective programs and facilitate sustained uptake of practices that improve the amount, frequency, and diversity of foods consumed by young children in accordance with changing nutrient and developmental needs from 6 to 24 mo of age, and encourage responsive feeding, and hygienic storage and preparation of complementary foods.
Despite decades of effort to identify and address barriers and promote improved CF, success lags behind widespread promotion of exclusive breastfeeding (4, 5). The relative neglect of CF in nutrition research and programming may reflect perceptions that these practices are complex and difficult to improve, and a lack of consensus on effective interventions. CF involves a constellation of behaviors, reflecting multiple determinants. As with other caregiving practices, it involves not only mothers or primary caregivers, but others who can create “enabling environments” such as families, health workers, community leaders, and policy makers (6–8).
One mechanism by which family and community members influence behaviors is through communicating, upholding, or questioning social norms (9, 10). Social norms are “beliefs about which behaviors are appropriate or typical within a given group” (11). Attitudes based on individual knowledge and beliefs about the value of a behavior are commonly recognized behavioral determinants, but there is less attention to how group or community norms influence key behaviors around food and care. In contrast to written laws and policies, social norms are informal rules that govern behavior in society and evolve as the “unplanned result of individuals’ interaction” (12). Social norms related to perceptions of what most people do are referred to as descriptive norms, and expectations about what people should do are injunctive norms (11, 13). The influence of norms is often assessed by asking individuals about their perceptions of behavioral expectations; however, social norms are characteristic of groups rather than individual attributes. The unstated, informal nature of social norms makes them difficult to measure, or even to identify and distinguish from the individual beliefs and behaviors they influence.
While it is intuitive that social norms influence behavior, this is not a simple, direct relation. Cialdini and Trost (13) note that social norms have been conceptualized in various ways, and their power depends on the social and cultural context. Examples of relevant factors include the similarity, proximity, and status of the influencer who models or communicates the norm; perceived rewards or sanctions associated with a behavior; and the degree to which individuals have integrated the norm into their personal values and expectations. Normative influence may depend on the degree to which behaviors are public or connected to cultural identity (14) and on individuals’ perceptions of control over their own behaviors (10).
Normative change interventions include strategies to involve communities in reflecting on and challenging existing social norms that influence individual behaviors (15, 16). Such interventions may focus on community-level values, appeal to emotions, address power imbalances, encourage critical reflection, and create enabling environments for social norm change through advocacy, diffusion, social support, and community engagement (11). Working with subgroups most likely to adopt a change can provide a mechanism for diffusing and sustaining new norms and behaviors to larger groups (17). Although norms are included in conceptual frameworks of determinants of child nutrition and development (18, 19) and there is general recognition that cultural beliefs, traditional practices, and norms influence CF behaviors (20), social and behavior change (SBC) approaches to CF often overlook social norms, targeting individual attitudes and beliefs (or focusing solely on structural-level factors) without addressing community rules and shared beliefs. Social norms may hinder or facilitate positive child feeding behaviors; hence, we use the term “norms-focused” for interventions that aim to either shift or build on existing norms.
CF involves an array of behaviors ranging from producing or purchasing food to preparing and feeding it to the child. Nutrition-specific and nutrition-sensitive interventions support different dimensions of improved CF, including dietary diversity, adequate frequency and daily intake, food hygiene, responsive feeding, and parenting practices. Beyond messages specific to what to feed young children, interventions to improve CF could address norms related to early child development; family dynamics; water, sanitation, and hygiene (WASH); agriculture and food security; food processing; and marketing. Many cultures have norms prescribing gender-based roles and responsibilities in these activity areas, so the influence of gender norms and women's status and empowerment cuts across all aspects of this multisectoral approach to CF. To increase awareness of influential social norms and related strategies used to improve young child feeding, we summarized the range of norms-focused approaches relevant to multisectoral nutrition interventions to promote recommended CF practices.
We reviewed the published and unpublished literature to gauge the scope of social norms relevant to CF and the approaches and effectiveness of CF interventions addressing social norms, in low- and lower–middle- income countries. We considered CF broadly, as a household-level activity influenced by sectors beyond health and nutrition, and summarized challenges, gaps, and implications for future research and SBC programming. The following objectives guided this scoping review:
Objective 1: Illustrate the scope of social norms described as relevant to adoption of multisectoral nutrition actions needed to achieve recommended CF practices.
Objective 2: Identify approaches used in nutrition-specific or multisectoral interventions to foster social norms and normative perceptions that support recommended CF practices.
Objective 3: Summarize evidence on the effectiveness of social norms-focused interventions in influencing outcomes related to social norms or CF.
Methods
Scoping reviews address broad questions by including the full range of relevant literature, rather than focusing on a narrow research question using strict study design and quality criteria (21, 22). To meet the 3 objectives outlined above, we conducted a scoping review of peer-reviewed publications and unpublished program documentation (e.g., reports, evaluations) that identified social norms that potentially influence CF practices such as adequate intakes, dietary diversity, responsive feeding, and hygienic food preparation, etc., and/or described CF interventions that addressed social norms. We then reviewed results of qualitative, quantitative, and mixed-methods evaluations of CF interventions that included at least 1 component designed to address social norms or related constructs, as explained below.
Inclusion and exclusion criteria
The inclusion and exclusion criteria we used to determine eligibility for inclusion in this review were based on Peters et al. (23) framework of population, concept, context, and studies.
Participants
We included reports or studies focused on CF practices for children aged 6 to 23 mo old. Participants could be caregivers, family members, or community members expected to engage in or influence CF practices.
Concept
Studies were included if they focused on describing or shifting social norms related to an aspect of CF for children 6 to 23 mo old. We framed CF as including timely introduction at 6 mo; adequate frequency, amounts, and diversity of foods; safe and hygienic preparation; and responsive feeding (24). Social norms were considered relevant if directly related to the “what, when, and how of CF” (1) or influencing time demands, resources, roles, and autonomy needed to adopt recommended CF and care practices, such as social norms related to gender, family roles, and household allocation of food.
Included reports went beyond focusing on individual attitudes and behavior to consider or address traditional or cultural beliefs; used approaches to reach or mobilize groups or communities and engage people in discussion or reflection on perceptions of appropriate behavior, shifting social norms, perceptions, and expectations; or built positive norms. As shown in the search strategy (Supplemental Box 1), we included additional terms related to social norms and did not require explicit mention of norms. Inclusion decisions based on full-text review considered theoretical frameworks, stated goals and rationale, as well as intervention strategies.
Context
Studies were included if conducted in a country meeting the World Bank 2010 definition of low- or lower middle-income economy (25).
Studies
We did not limit based on study design because we were interested in the scope of norms discussed in formative and descriptive “reports” (Objective 1), as well as “intervention” design (Objective 2) and “studies” or “evaluations” of effectiveness (Objective 3) of norms-focused interventions. We included grey literature and program evaluations and did not wish to limit the scope of what was included, given the dearth of literature on social norms and CF. We included publications and reports from the last 10 y (i.e., dated 2010 or more recently).
Exclusion criteria
Publications or reports were excluded if not available in English or dated prior to 2010. Interventions that exclusively used individual or family counseling in clinics or home visits, used group methods only to disseminate information rather than to address social norms, or provided insufficient information about norms-focused components were excluded. We did not include studies solely focused on rehabilitative feeding, continued breastfeeding, or micronutrient supplementation.
Literature search strategy
Our broadly inclusive search strategy was designed to be comprehensive within the peer-reviewed literature. We conducted a structured search of 4 databases—PubMed, Scopus, Web of Science, and CINAHL—in August 2020. The search strategy in Supplemental Box 1 was used for Scopus, and formatting was adapted for searches in other databases.
To identify unpublished grey literature, we sent requests for program documentation to the following electronic mailing lists: CORE Group Nutrition Working Group (26), CORE Group Social and Behavior Change Working Group (27), and Breakthrough ACTION Springboard online community (28). A search was also conducted through the US Agency for International Development's (USAID's) Development Experience Clearinghouse (29), their online repository for all publicly available program materials.
Additional snowball searching was conducted using relevant citations in articles included in our review and other literature reviews, and by reaching out to targeted organizations and programs.
Study selection
For published peer-reviewed articles obtained through database search, the review process was managed in Covidence Online Software (https://www.covidence.org) and abstracts were independently screened by 2 authors (JKM, FMC). Any conflicts during screening were resolved through discussion with KLD. The selected full-text articles were assessed on inclusion and exclusion criteria by at least 1 reviewer (JKM, FMC, KLD), with any uncertainty resolved as a group. The grey literature search identified program evaluations, reports, process documentation, manuals, and briefs for consideration. Using the same inclusion and exclusion criteria, full-text documents were reviewed (KL, JKM) and selected if they described CF-related social norms or a norms-focused intervention. Uncertainty on inclusion and extraction for grey literature was resolved in discussion with the group.
Data extraction and synthesis of results
Articles identified through the search were categorized as relevant to objective 1 (descriptions of social norms), 2 (CF interventions designed to influence social norms), and/or 3 (evaluations of interventions). Data extracted into spreadsheets included the authors’ stated objectives, research methods, study population, theories and models referenced, relevant norms, and degree of attention to social norms. We noted program components (e.g., entry point, activities) for studies that included interventions to address social norms. When comparative trials or quantitative or qualitative program evaluations were conducted, relevant results were extracted. Multiple documents on the same study or project were reviewed together and results were combined.
Results
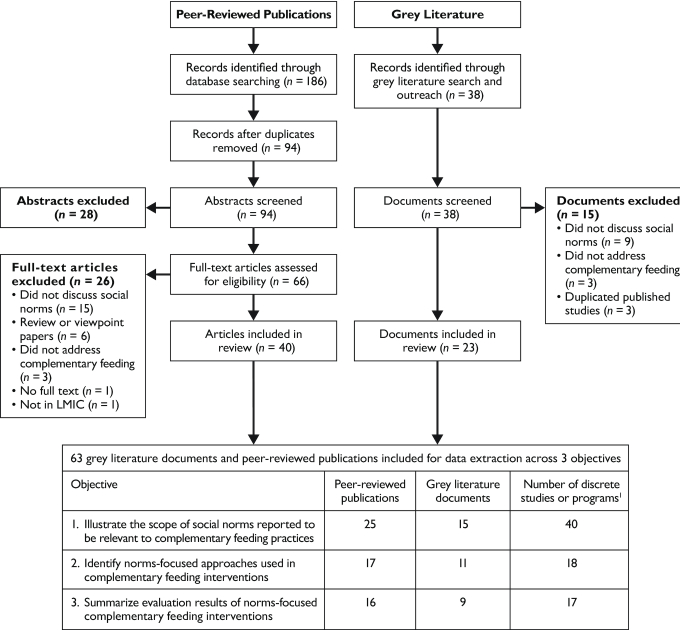
The number of peer-reviewed publications and grey literature reports identified, screened, excluded and reviewed are shown in the flowchart in Figure 1, as well as the number of documents and the number of studies or projects included for each objective. Results are summarized below, by objective.
FIGURE 1.
Flow diagram of search results for peer-reviewed publications and grey literature on social norms related to complementary feeding practices, intervention approaches, and evaluations of norms-focused complementary feeding interventions. LMIC, low- and middle-income country.
Objective 1: Illustrate the scope of social norms described as relevant to adoption of multisectoral nutrition actions needed to achieve recommended CF practices
For Objective 1, we identified the social norms, cultural beliefs, and perceptions of appropriate or accepted behaviors reported to influence CF, extracted from 25 peer-reviewed publications and 15 unpublished or “grey literature” reports. While few reports discussed social norms per se, many described perceptions and beliefs related to child feeding that we deemed indicative of social norms—for example, behaviors viewed as appropriate or “what most people do” or behaviors expected or sanctioned by influential people. Findings are summarized below in relation to the UNICEF programming guidance dimensions of what children should eat (i.e., provide diverse and nutrient-dense foods, animal-source foods (ASFs), and fruits and vegetables and avoid foods with low nutrient value); when and how children are fed (i.e., timely introduction; age-appropriate meal frequency, amount, and consistency; responsive feeding, and hygienic food preparation and use) (1); plus a dimension related to who is responsible for child feeding that emerged as a theme in our analysis. A few examples are described in the text to illustrate the range of norms, and Table 1 summarizes all the social norms and related perceptions extracted from the documents reviewed.
TABLE 1.
Summary of social norms reported to influence CF, across nutrition-specific and nutrition-sensitive sectors1
| Dimensions of CF2 | Social norms or perceptions of norms relevant to child feeding |
|---|---|
| What should children eat? | |
| Nutrient density, dietary diversity,and provision of ASFs, vegetables,and fruits |
|
| Avoiding processed, energy-dense, non–nutrient-densefood | |
| When and how are children fed? | |
| Timely introduction |
|
| Frequency of feeding | ● Women's workload and sole responsibility for children limits time available for child care and feeding, e.g., Nepal (44) |
| Responsive feeding, interaction, andencouragement | |
| Hygienic preparation of foods forchildren | |
| Who is responsible for child feeding? | |
| Food preparation and feeding roles,decisions about child feeding,provision of food for household,and food allocation |
|
ASF, animal-source food; CF, complementary feeding, PDR, People's Democratic Republic.
Dimensions of CF adapted from UNICEF Programming Guidance (1).
Many of the social norms or perceptions of acceptable CF practices were nutrition-specific and related directly to child nutrition and physical health and well-being. Other norms identified were related to nutrition-sensitive sectors such as cognitive development and socialization, culture or religion, sanitation and hygiene, as well as family dynamics and gender roles.
The most commonly identified norms were about what children are fed, notably pervasive norms identifying the most appropriate complementary foods as soft, dilute cereal-based gruels because young infants were perceived to be unable to chew and liable to choke (30–35). These primarily descriptive norms that everyone feeds infants easily chewed and digested foods shaped practices such as avoiding or delaying animal-source and other nutritious foods (30–34) or, in Laos, premasticating meat and other foods before feeding to the child (36). Willingness to adopt new behaviors that increase dietary diversity can be constrained by social norms related to fear of being perceived as not providing appropriate care or food to children, because certain foods were thought to promote or interfere with physical development and well-being (32, 33, 39, 41–43). Beliefs about how foods affect child psychosocial development and behavior were also reported. For example, concerns in West Africa that feeding eggs or meat to children makes them liable to beg or steal (38) may reflect social norms against having children become accustomed to desirable foods that may not be affordable.
Interviews of rural and peri-urban Ghanaian mothers found consensus on ranking healthiness as the most important factor in CF decisions and on many foods perceived as healthy (40). Interestingly, these caregivers of children aged 6–8 mo tended to think they fed different foods than others fed (i.e., that their practices differed from the norm), but this lessened as children began to eat more family foods. Perhaps due to prestigious images used in marketing, norms are shifting in urban areas toward preference for commercial cereal–based foods (6) and energy-dense packaged foods and snacks are often perceived as appropriate for young children (6, 30, 44, 50, 55, 62).
While there were few mentions of religious or cultural norms linked specifically to foods for young children, broader religious and cultural norms may influence CF through their impacts on food preparation and consumption in the larger household. In Ethiopia, for example, while children are exempt from the Orthodox Christian fasting practice of not consuming meat on Wednesdays, Fridays, and multiple religious holidays, few caregivers prepare ASFs for children on these days out of concern for cross-contamination of family foods or being judged by neighbors (43, 47, 48). Cultural or religious groups may adhere to a variety of dietary norms such as limiting consumption of fish or meat (37, 49). In some settings, particularly in Asia, social norms about appropriate foods for young children reflect cultural hot and cold humoral typologies linking certain foods to diseases (44–46).
Fewer reports described norms related to when and how children are fed. No norms related to feeding frequency were reported, beyond noting the constraints on women's time availability (44), discussed below in relation to gender norms. Decisions about when to introduce CF were reported to reflect norms around developmental readiness. This is generally appropriate, except when a child needs more encouragement to eat sufficient amounts. Norms around child autonomy relative to parental directiveness vary across cultures and would be expected to affect how children are fed, specifically responsive feeding practices, but we found few mentions of norms related to responsive feeding. In 1 study in Tanzania, some mothers reported singing or talking to encourage children to eat, but responsive strategies were not the norm and most mothers said they would not push a child who refused to eat (35). Social norms related to valuing child autonomy may interfere with responsive feeding and become problematic as children become more independent or develop unhealthy preferences. For example, in Indonesia, parents expressed that children should be given whatever they wanted to eat, leading to children consuming packaged, sweetened foods (55).
A few studies reported norms related to how children are fed, in terms of hygienic preparation and serving of CF. In a doer/non-doer study in Malawi, washing utensils with soap, keeping utensils on a raised place, and handwashing with soap at key times were more strongly associated with perceiving these behaviors as practiced and approved by influential others than with perceptions of risk (56). In Bangladesh, food contamination was linked to visibly dirty hands and soap was not available for handwashing prior to food preparation, indicating lack of norms supporting this practice, despite the presence of soap in other areas of most homes (57).
In addition to the dimensions above, we found ample evidence of the influence of social norms related to who is responsible for various aspects of child feeding. Social norms designating mothers as primary caregivers are almost universal, and when mothers alone are responsible for child feeding and health, the stress and pressure to be “a good mother” or caregiver, as reflected in children's health and development (30), and the stigma associated with child undernutrition and illness may limit willingness to seek care (58). Traditional norms prescribing family roles mean heavy workloads for mothers of young children, limiting their ability to practice CF recommendations (44).
Across multiple contexts in Africa and Asia, social norms respecting the wisdom and experience of elders, as well as the traditional power dynamics within the family, sustain the role of grandmothers (maternal or paternal) or other female elders as decision makers, advisors, and monitors of child feeding (32, 38, 51, 52, 54, 59). This varies by cultural context and household structure, but grandmothers often strongly influence child feeding whether positively or negatively, directly and indirectly.
Similarly, norms related to fathers’ roles were influential and varied somewhat across contexts. Fathers’ involvement in child feeding (54) counters social norms about male roles that are sometimes enforced by mockery (31). Gender norms, including perceptions that male decision making and exercise of power in the family are appropriate, reduce the scope for shared parenting, joint decision making, and support for child feeding and caregiving (60). However, in many cultures, men are viewed as providers and hence feel responsible for making household decisions, including ones that impact child feeding (6, 32, 54, 59–61), and may be directly involved in child feeding when mothers are working away from home or ill (61). Family roles and gender norms such as serving valued foods to men (33, 43) also affect intrahousehold food allocation; thus, social norms can influence access to food for children (37) even when food security at the household level is largely determined by economic status, agricultural production, and food systems.
Objective 2: Identify approaches used in nutrition-specific or multisectoral interventions to foster social norms and normative perceptions that support recommended CF practices
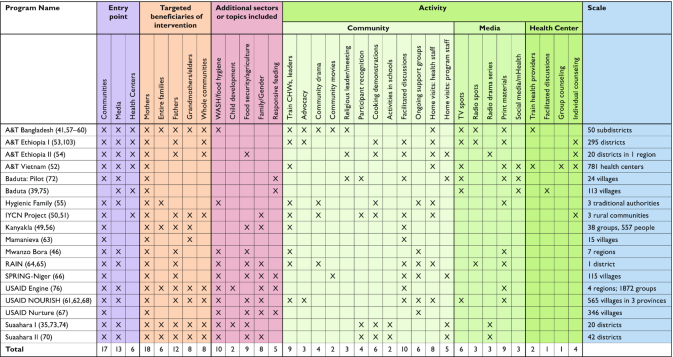
The review identified 18 programs that included interventions with at least 1 component addressing social norms (or cultural practices and perceptions) related to CF: 9 implemented in sub-Saharan Africa and 9 in Southeast Asia. Table 2 compiles the characteristics of all interventions, and Table 3 summarizes additional details on target behaviors, basis for intervention approaches, and norms-focused activities, by intervention. Most studies aimed to impact a range of CF practices, including dietary diversity, amounts consumed, and timing of introduction, by addressing norms-related beliefs on appropriate foods for children, cultural traditions and taboos, and family and gender roles. This section describes how intervention activities operationalized norms-focused strategies, illustrating possible approaches. Some interventions were based on formative research and/or conceptual models (Table 3). For example, an intervention addressing hygiene behaviors in Malawi (56) used the Risk, Attitude, Norms, Ability, and Self-regulation model, including perceptions of usual or acceptable behavior, personal obligation, and how family and community members view and value behaviors (63). Intervention targets were key normative behaviors identified in formative research comparing doers with non-doers (56).
TABLE 2.
Summary of intervention characteristics, scope, and activities
|
TABLE 3.
Descriptions of norms-focused components of CF interventions1
| Program, country (references) | Target CF-related behaviors, intervention approach, and activities related to social norms |
|---|---|
| Alive & Thrive, Bangladesh (53, 57, 64–66) | Target behaviors: WHO CF practices, handwashing.Large-scale, multilevelcommunication strategy guided by behavioral theories such as stages of change, self-efficacy, and diffusion of innovations and tailored to the local context based on formative research
|
| Alive & Thrive, Ethiopia (I & II) (67, 68, 82) | Target behaviors: WHO CF practices.Multisectoral approach to operationalize the National Nutrition Plan, combining nutrition-sensitive agricultural, community mobilization, behavior-change communication based on formative research, and training health extension workers and volunteers
|
| Alive & Thrive, Vietnam (69, 83) | Target behaviors: WHO CF practices, use of health services.Social franchising model using brand name “Mặt Trời Bé Thơ” to standardize and monitor quality of IYCF counseling and ensure utilization and sustainability of health services; based onformative research, reasoned action model, and ecological model (7) |
| Baduta Program, Indonesia (62, 84) | Target behaviors: reduction of unhealthy snacking, dietary diversity.Behavior Centered Design theory: used emotional drivers, such as affiliation, nurture, anddisgust, to motivate behavior change; based on formative research
|
| Hygienic Family Intervention, Malawi (70, 85) | Target behaviors: washing hands and kitchen utensils with soap, safe utensil storage, reheating leftovers, feeding by caregivers.Informed by risk, attitude, norms, ability, self-regulation model, and formative research on key psychosocial behavioral drivers
|
| IYCN project (father and grandmother peer dialogue groups), Kenya (59, 71) | Target behaviors: WHO CF practices.Engaged fathers and grandmothers to support improved feeding practices, using a group dialogue approach to building social support, based on formative research and the socioecological model
|
| Kanyakla, Kenya (72, 73) | Target behaviors: dietary diversity, meal frequency, ASFs in diet, feeding children during and after illness, improved food security. Social network approach engaging family members to support IYCF in community
|
| Mamanieva, Sierra Leone (74) | Target behaviors: minimum dietary diversity, minimum acceptable diet.Family-centered approach that built on cultural roles of grandmothers as advisors and caregivers; based on formative research
|
| Mwanzo Bora, Tanzania (60) | Target behaviors: minimum dietary diversity, minimum meal frequency, handwashing/safe food handling. Based on diffusion of innovations theory; aimed to promote positive nutritional behaviors at household level
|
| RAIN, Zambia (77, 78) | Target behaviors: WHO CF practices.Multisectoral gender-sensitive agriculture program and nutrition behavior-changecommunication to improve norms on gender equality and women's empowerment/status, to lead to positive changes in child feeding practices.
|
| SPRING, Niger (79) | Target behaviors: dietary diversity, meal frequency, responsive feeding, handwashing.Community-led video to strengthen spousal communication and male involvement in childfeeding; based on formative research
|
| USAID Engine, Ethiopia (86) | Target behaviors: dietary diversity, timely introduction of CF, ASF consumption, handwashing and sanitation, responsive feeding.Family-centered communication through community conversations to frame nutrition as “a family affair”; informed by Household Agriculture-Nutrition Doable Actions Framework and formative research
|
| USAID NOURISH, Cambodia (75, 76, 80) | Target behaviors: feeding frequency, dietary diversity including ASFs (fish), hygiene and sanitation practices. Community systems strengthening and communication linked to marketing of services and products, shaping social norms by targeting audiences at all levels, and fostering empowerment, positive role models, and collective engagement
|
| USAID Nurture, Lao PDR (81) | Target behaviors: minimum dietary diversity, minimum meal frequency, minimum acceptable diet, handwashing and hygiene. Communication and collective engagement, with improved quality of nutrition services and marketing of soap and latrines
|
| USAID Suaahara, Nepal (44, 87–89) | Target behaviors: dietary diversity, handwashing, continued feeding during illness.Multisectoral design, based on formative research, to influence enabling environment for change and strengthen self-efficacy
|
ASF, animal-source food; CCA, community change agent; CF, complementary feeding; CHW, community health worker; IFA, iron-folic acid supplements; IYCF, infant and young child feeding; IYCN, infant and young child nutrition; NGO, nongovernmental organization; PDR, People's Democrative Republic; RAIN, Realigning Agriculture for Improved Nutrition; SPRING, Strengthening Partnerships, Results, and Innovations in Nutrition Globally; USAID, US Agency for International Development.
An attribute of normative approaches is engagement of people at multiple levels (11). In addition to mothers of young children, all but 4 interventions targeted other household members (e.g., fathers, grandmothers), the entire community, and/or community leaders. The 2 main entry points were community engagement and various types of media. All of the interventions included multiple components, although not all components addressed social norms. Many included interpersonal communication through home visits or facility-based group or individual counseling focused on knowledge and attitudes. These activities were not usually designed to address norms so are noted in Table 2 but not described in detail; they complemented norms-focused community and media activities by providing information and problem-solving support.
Community engagement
As shown in Table 2, all but 1 of the 18 interventions targeting social norms implemented components at the community level, engaging community members to reflect on existing social norms and, in some cases, promote supportive social norms for recommended CF practices.
Community and religious leaders and, in some contexts, community health workers (CHWs) may enforce existing norms or encourage shifts in social norms through their influential roles and status. Nine interventions trained community or religious leaders or health workers to advocate, mobilize, and implement activities to influence CF behaviors and norms in communities (53, 59, 60, 64–76). For example, the Kanyakla Nutrition Program trained CHWs to facilitate community discussions and serve as community ambassadors promoting nutrition practices through modeling and informal conversations (72, 73).
Facilitated group discussions among community members provide opportunities not only to disseminate information about optimal CF practices but also to create positive new norms. Ten interventions used facilitated discussions during one-time or occasional community gatherings to reflect on existing and/or potential shifts in social norms related to CF. Most discussion groups engaged mothers, fathers, and grandparents separately, but a few engaged the broader community in dialogues or public forums. Some groups reinforced social norms supportive of CF practices, such as cultural roles of grandmothers as advisors and caregivers, aiming to strengthen grandmothers’ knowledge and self-efficacy (74). Others reflected on how to shift social norms to be more positive—for example, improving grandmothers’ and fathers’ relationships and communication with mothers (59, 71).
Six interventions (60, 70, 75–81) used community support groups that met regularly—typically monthly—to discuss and provide mutual support on infant and young child feeding (IYCF) behaviors, led by trained peer facilitators. Three were mothers-only, one was fathers-only, and one had separate mothers’ and fathers’ groups. A few added IYCF topics to ongoing group programming on agriculture, livestock, and reproductive health, while others established new groups. Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING)–Niger produced and disseminated videos depicting male involvement in key IYCF behaviors such as responsive feeding and dietary diversity, challenging normative beliefs (79). Trained facilitators led fathers belonging to established “Husband Schools” in discussions of videos on maternal and child nutrition behaviors. In Malawi, the Hygienic Family intervention included biweekly “cluster meetings” targeting psychosocial determinants of handwashing and food hygiene, including social norms, alternating with home visits by community volunteers to reinforce messages and strengthen descriptive norms and social capital among caregivers (70, 85).
Ten interventions used community events to sensitize the public and mobilize collective encouragement for CF behaviors through interaction and information sharing and to organize diffusion of positive norms (44, 59, 67, 68, 70, 71, 77–79, 87, 90). Activities included community dramas, movie screenings, demonstrations, messages during religious gatherings, and school activities. For example, Realigning Agriculture for Improved Nutrition held drama performances to improve gender-equality norms and promote positive change in child feeding (78).
Another approach was to create positive new norms by publicly recognizing people who practiced recommended behaviors and encouraged others to challenge norms or change their behavior (44, 59, 71,84, 87–89). These interventions relied on “champions” or credible community members to set the example and encourage shifts in social norms. To influence social norms and empower women, Suaahara organized community events celebrating key life events and recognizing “ideal families” practicing target behaviors (87–89).
Media
Thirteen interventions included some form of media (Table 2) to disseminate information and potentially address norms at a large scale through print, audio, and visual media. Approaches included radio dramas, TV spots, mHealth, social media, and distribution of print materials, to portray and promote positive norms, correct misperceptions, or counter social norms seen as barriers to improving practices. All media interventions were implemented in conjunction with community activities, engaging with target audiences at multiple levels.
Ten interventions used TV or radio to reinforce messages on optimal CF behaviors (Table 2), and a few targeted mass media to challenge social norms directly or support positive norms. Suaahara I radio dramas had call-in segments featuring a mother-in-law character who modeled and praised optimal nutrition behaviors in the first 1000 days. In Indonesia, TV spots featuring “Mrs. Gossip” aimed to tap into peer influences and emotional drivers of behavior (55, 62, 84). Three interventions used social media or mobile applications for discussion and peer support, capitalizing on these normative influences to correct misperceptions and reinforce optimal practices. In Vietnam, a mobile app for smartphones allowed mothers to access and share news on child nutrition (7) and other programs used online groups to help mothers feel part of a movement adopting new practices (62, 84).
Mid-media approaches (i.e., media with more limited reach than radio and TV) (91) depicting positive CF practices to family or community audiences were often based on formative research on social norms. Nine interventions used mid-media materials, including brochures promoting fathers’ role in ensuring good nutrition for family members (77, 78), reminder and invitation cards (69, 75, 80), and kits for new parents with print materials on optimal nutrition practices by stage of infancy (60). NOURISH developed a series of “Curious Chenda” children's books with engaging illustrations and inspirational stories about protecting children's health and future, appealing to families on an emotional level and conveying key messages on parenting and ASFs (75, 76, 80). In Ethiopia, USAID Engine promoted transformative gender roles in households by distributing role model testimonial cards with photographs and stories of real people (86).
Objective 3: Summarize evidence on the effectiveness of social norms–focused interventions in influencing outcomes related to social norms or CF
Of the 18 interventions reviewed for Objective 2 and described in Tables 2 and 3, 17 had some type of evaluation (8 mixed methods, 8 quantitative, 1 qualitative). Notably, very few studies assessed social norms outcomes or how norms-focused components were received. The 2 studies (53, 70) that assessed perceptions of social norms are summarized first, as they are most relevant to our objectives. Then we present key qualitative findings from 5 studies that provided information on barriers and facilitators of behavior change. Finally, we briefly summarize evaluations of overall effectiveness, including impacts on indicators of CF practices (92), CF knowledge, and prevalence of stunting (details in Table 4). The latter results shed light on the effectiveness of interventions that include a norms-focused component but are less directly relevant to Objective 3 because these evaluations assessed the overall impacts of complex interventions without comparing components that did and did not address norms.
TABLE 4.
Summary of evaluation designs, methods, and quantitative and qualitative results1
| Project name, country; (reference) | Study design and evaluation methods | Quantitative results: norms, CF knowledge and practices, growth Qualitative or implementation results |
|---|---|---|
| Alive & Thrive, Bangladesh (53, 64–66) | RCT: I: intensive program (n = 1001 mothers of children <2 y); C: nonintensive program (n = 1200 mothers of children <2 y)T2: endline (2014); T3: follow-up (2016)T2 vs. T3; I vs. C; DID: T2 vs. T3 for I vs. C; path analysis | Descriptive IYCF norms (I vs. C for T2 and T3; T2 vs. T3 for I and C; DID): greater prevalence (%) of mothers who believe other mothers in the community feed mashed family food after 6 mo in I in T2, but greater improvement in C from T2 to T3 (T2: I: 74.7 vs. C: 57.6**; T3–T2: I: 14.7**; C: 28.2***; DID: −13.5*), nonsignificant I vs. C difference at T3; greater % of mothers who believe mothers in the community feed ASFs after 6 mo at in I in T2 and T3, but greater improvement in C from T2 to T3 (T2: I: 74.7 vs. C: 57.6***; T3–T2: I: nonsignificant, C: 27.1**; DID: −19.3**), nonsignificant at T3.Injunctive IYCF norms (I vs. C in T2): nonsignificant difference in prevalence (%) of mothers who agree that people important to them think that they should give ASFs every day starting at 7 mo, feed their baby mashed family cooked foods along with breast milk after 6 mo, or approve of feeding their child after 6 mo at least 3 meals/d.IYCF knowledge sharing (I vs. C for T2 and T3; DID): greater prevalence (%) of mothers who shared about feeding mashed foods after 6 mo in I for T2 (T2: I: 46.6 vs. C: 25.5***); greater % of mothers who shared about feeding ASFs to children >6 mo in I for T2 (T2: I: 48.2 vs. C: 26.7***); difference at T3 and DID for either indicator, NS.Social networks of adopters (T2 vs. T3 for I and C): increase in prevalence (%) of mothers who knew other mothers who adopted ASF feeding in I & C (I: T2: 57.8 vs. T3: 94.3*; C: T2: 45.1 vs. T3: 83.8*); increase in mean number of known adopters of optimal IYCF practices in I and C (I: T2: 1.0 vs. T3: 2.2**; C: T2: 0.7 vs. T3: 1.7**).Path analysis: 24%, 42%, and 43% of the total effects of IPC, mass media, and community mobilization on MDD, respectively, were explained by improved social networks, diffusion of information, and social norms |
| RCT: I: intensive program (n = 500 children, 6–23.9 mo); C: nonintensive (n = 503 children, 6–23.9 mo)T1: baseline (2010); T2: endline (2014)Dose-response; DID: T1 vs. T2 for I vs. C | IYCF knowledge (dose-response): strong dose-response relation between exposure to multiple intervention platforms and knowledge of CF practices (OR: no vs. high exposure: 0.83***).CF indicators (DID for T1 vs. T2): increased prevalence (%) of MMD, MMF, MAD, and consumption of iron-rich foods for I (DID: 16.3*, 14.7**, 22.0**, 24.6**); SSSF timely introduction, NS.ECD (DID for T1 vs. T2): greater improvement in language and motor development scores for I (DID: 1.05***, 0.85*) | |
| RCT: I: intensive program (n = 600 children, 6–23.9 mo); C: nonintensive (n = 600 children, 6–23.9 mo)T1: baseline (2010); T2: endline (2014); T3: follow-up (2016)DID: T1 vs. T2 and T1 vs. T3 for I vs. C | IYCF knowledge (DID for T1 vs. T3 and T1 vs. T2): NS.CF indicators (DID for T1 vs. T3): increased prevalence (%) of SSSF timely introduction and consumption of iron-rich foods for I (DID: 16.6**, 11.8*); MMD and MMF, NS | |
| Alive & Thrive, Ethiopia I (67) | QE: I: program (n = 1494 children, 0–23.9 mo); no control group | CF indicators (T1 vs. T2; dose-response): increased prevalence (%) of SSSF timely introduction, MDD, MMF, MAD, and consumption of iron-rich foods at T2 (T2–T1: 22.2***, 3.3*, 26.2***, 3.5*, 2.7**); increased number of food groups consumed |
| T1: baseline (2010); T2: endline (2014)T1 vs. T2; dose-response | (T2–T1: 0.3***, see paper for breakdown of food groups); strong dose-response relation between exposure to SBCC channels and MDD and MAD (OR: no vs. high exposure: 18.75**, 14.19**); MMF or consumption of iron-rich foods, NS.Anthropometric indicators (T1 vs. T2): no significant change in child stunting, underweight, or wasting prevalence, HAZ, WAZ, or WHZ mean scores | |
| Alive & Thrive, Ethiopia II (68) | RCT: I: Intensive program (n = 1360 children, 6–23.9 mo); C: nonintensive program (n = 1360 children, 6–23.9 mo)T1: baseline (2015); T2: endline (2017)DID: T1 vs. T2 for I vs. C; dose-response; path analysis | IYCF knowledge (DID; dose-response): improved CF knowledge score for I (DID: 0.7**); strong dose-response relation between exposure to multiple intervention platforms and CF knowledge (OR: no vs. high exposure: 1.16***).CF indicators (DID; dose-response): nonsignificant DID for SSSF timely introduction, MDD, MMF, or MAD; increased number of vitamin A–rich foods for I (DID: 8.99*); strong dose-response relation between exposure to multiple intervention platforms and MDD and MMF (OR: no vs. high exposure: 3.15***, 1.93***).Anthropometric indicators (DID; dose-response): decreased prevalence of child stunting for I (DID: −5.9*); nonsignificant DID for child underweight, or wasting prevalence, HAZ, WAZ, or WHZ mean scores; strong dose-response relation between exposure to multiple intervention platforms and HAZ mean score (OR: no vs. high exposure: 0.24*); nonsignificant dose-response for stunting.Path analysis: strong relation between designating a chicken whose eggs are prioritized for a child <2 y (promoted in intervention), egg consumption, and increased MDD (see supplementary data in paper for details) |
| Alive & Thrive, Vietnam (69) | RCT: I: intensive program (n = 506 children, 6–23.9 mo); C: nonintensive program (n = 504 children, 6–23.9 mo)T1: baseline (2010); T2: endline (2014)DID: T1 vs. T2 for I vs. C | CF indicators (DID): increased prevalence (%) of MDD and MAD for I (DID: 6.4*, 8.0*); nonsignificant DID for SSSF timely introduction, MMF, consumption of iron-rich foods, number of food groups, or number of meals.Anthropometric indicators (DID): nonsignificant for child stunting, underweight, or wasting prevalence, mean HAZ, WAZ, or WHZ |
| Baduta Pilot Program, Indonesia (84) | RCT: I1: mass media and community activities (n = 243 mothers of children <2 y); I2: mass media only (n = 171 mothers of children <2 y); C: unexposed (n = 150 mothers of children <2 y)T1: baseline (April 2014); T2: endline (September 2014)I1 vs. I2. vs. C at T2, all combinations (adjusted for baseline values) | CF indicators (I1 vs. I2. vs. C at T2): greater DDS for children 6–24 mo in I1 and I2 (T2: I1-C: 1.0; CI: 0.6–1.4; I2-C: 0.8; CI: 0.4–1.2), no significant difference between I1 and I2; greater frequency of vegetable and fruit intake for I1 and I2 vs. C (T2: I1-C: 0.59; CI: 0.10–1.07; I2-C: 0.37; CI: 0.11–0.85).Unhealthy snacking (I1 vs. I2 vs. C): no reduction in unhealthy snacking for I1 and I2 |
| Baduta Program, Indonesia (84) | QE: I: mass media and community activities; C: mass media only (children 6–23 mo, n not provided) | CF indicators (I vs. C): greater prevalence (%) of MAD, and consumption of iron-rich foods, adequate number of food groups, ASFs, and micronutrient-rich fruits and vegetables for I (report states outcomes were significant at P < 0.05, but does not present details of statistical analysis, limiting interpretation). |
| T1: baseline (2015); T2: endline (2017)I vs. C | Anthropometric indicators (I vs. C): no significant changes in prevalence of stunting or anemia | |
| Hygienic Family Intervention, Malawi (70) | RCT: I: behavior-change intervention area (n = 240 households with a child <2 y); C: comparison area (n = 80 households with a child <2 y)T1: baseline (2017); T2: follow-up (2018)DID: T1 vs. T2 for I vs. C; multiple mediation analysis | Descriptive WASH norms (DID): significant DID between I and C in reporting that others’ behavior in the household or village was a significant factor for handwashing with soap at key times and washing kitchen utensils with soap, and others’ behavior in the village was a significant factor for keeping kitchen utensils in a safe place (DID measure not recorded, significant and positive effect of I).Injunctive WASH norms (DID): significant DID between I and C in reporting that others’ approval was a significant factor for handwashing with soap at key times, and both others’ approval or personal obligation was a significant factor for keeping kitchen utensils in a safe place; nonsignificant DID of others’ approval or personal obligation on washing kitchen utensils with soap (DID measure not recorded, significant and positive effect of I).WASH practices (DID): significant DID between I and C on handwashing with soap at critical times, washing kitchen utensils with soap, keeping kitchen utensils on an elevated place, reheating of leftover food, and feeding of child by the caregiver (DID measure not recorded, significant and positive effect of I).Multiple mediation analysis: others’ behavior in the household mediated the relation between I and changes in handwashing with soap at key times and washing kitchen utensils with soap (b = 0.2850; CI: 0.1120–0.4854; b = 0.1574; CI: 0.0461–0.3019); others’ behavior in the village mediated the relation between I and changes in keeping kitchen utensils in a safe place (b = 0.3507; CI: 0.0825–0.6260) |
| IYCN peer dialogue project, Kenya (59, 71) | QE: I1: father intervention area (n = 70 mothers, 75 fathers); I2: grandmother intervention area (n = 71 mothers, 81 grandmothers); C: comparison area (n = 76 mothers, 73 grandmothers, 63 fathers)T1: baseline (2011); T2: endline (2012)DID: T1 vs. T2 for I1 and I2 vs. C; FGD (8 fathers’ groups, 10 grandmothers’ groups) | Social support (DID): increased prevalence (%) of mothers reporting 5+ support actions received from father or grandmothers for I1 and I2 (DID: I1 vs. C: 25.8**; I2 vs. C: 32.7***), fathers reporting they provided 5+ social, 5+ physical, or 3+ material support actions (DID: I1 vs. C: 37.1***, 54.5***, 33.0***), and grandmothers reporting they provided 5+ physical or 3+ material support actions (DID: I2 vs. C: 36.6**, 28.4**); nonsignificant DID for grandmothers reporting 5+ social support actions.CF indicators (DID): increased prevalence (%) of ASF consumption for I1 (DID: I1 vs. C: 31.0**) and I2 (DID: I2 vs. C: 27.4*) and adequate consistency of food consumed for I2 (DID: I2 vs. C: 44.0***); nonsignificant DID for I1 or I2 for minimum number of meals provided in past 24 h, MAD, or dietary diversity.QualitativeCF practices: FGD found improved relations with spouses or daughters-in-law, increased support for IYCF practices; fathers reported providing nutritious foods for their families.Male involvement: fathers reported helping their wives with chores and childcare, accompanying their wives and bringing their children to the health center, and enjoying learning about infant feeding.WASH: grandmothers reported improved hygiene practices.Facilitators to IYCF: grandmothers appreciated involvement, recognition for their roles and infant feeding advisors, and cooking demonstrations with locally available foods |
| Kanyakla, Kenya (72, 73) | QE: I: intervention participants (n = 47 primary caregivers, 48 children; T4: n = 22 CHWs, 43 community members); C: comparison participants (n = 176 primary caregivers, 179 children; T4: n = 64 CHWs, 149 community members)FGD: 4 mothers’ group, 1 fathers’ groupT1: baseline (January–March 2014); T2: 1 mo postintervention (June–August 2014); T3: 6 mo postintervention (February–April 2014); T4: 2 y postintervention (2016) (intervention was from June–August 2014)DID: T1 vs. T2 vs. T3 for I vs. C; I vs. C at T4; FGD | IYCF knowledge (I vs. C at T4): higher mean knowledge scores in overall nutrition, CF practices, and caregiver confidence and behavior score for CHWs in I (I vs. C: 24.7 vs. 21.2***, 10.3 vs. 9.2*, 6.1 vs. 5.0**); higher mean score in overall nutrition knowledge for community members in I (I vs. C: 21.9 vs. 20.3**); CF feeding practice knowledge, caregiver confidence and behavior for community members, NS.CF indicators (DID): increased mean number of food meals/day from T1 to T2 for I (DID for T2 vs. T1: 0.31; CI: 0.03–0.60); nonsignificant DID for T3 vs. T2 or T1; number of food groups per day, MDD, MMD, MAD, or consumption of iron-rich foods, NS.QualitativeChanges in behaviors: FDG reported greater male involvement in IYCF, increased sharing of food/information about DD at community level, improved community perceptions of optimal nutrition and support for DD.Facilitators to IYCF: increased knowledge due to program (among men and women), changes to personal misperceptions and misbeliefs, increased confidence, stronger community ties and networks, participation in kitchen gardens and poultry projects.Barriers to IYCF: access to food, access to funds, climate/weather-related impacts on food production and fish catch |
| Mamanieva Project, Sierra Leone (74) | QE: I: intervention communities; C: comparison communities (n not provided)T1: baseline (2013); T2: endline (2016)I vs. C at T2 | IYCF knowledge and beliefs (I vs. C at T2; DID): higher mean nutrition knowledge scores; greater increase in positive beliefs about specific IYCF practices for I (report states outcomes were significant, but does not present statistical analysis, limiting interpretation).CF indicators (I vs. C at T2): higher prevalence (%) of MDD and MAD (T2: I: 77.2 vs. C: 51.8**; I: 53.8 vs. C: 22.6***).QualitativeChanges in IYCF practices: 82% of WRA and 81% of GM reported introducing cereal at 6 mo; 18% of WRA and 5% of GM reported introducing first foods between 7 and 14 mo.Changes in responsive feeding: WRA and GM reported encouraging child to eat using doll, smiling, dancing, and clapping |
| Mwanzo Bora, Tanzania (60) | Secondary analysis of TDHS data and follow-up SSI, FGD, KII studies: I: MBNP area C: comparison area(n = 290 SSI with women, 39 FGD with fathers, grandmothers, community members; 51 KII with leaders, health facility staff, program staff)T1: 2010 TDHS; T2: 2015 TDHS; T3: follow-up surveys (2017) (intervention was from 2011–2018) | CF indicators (I vs. C at T2): higher prevalence (%) of timely introduction of CF in I for children 6–11 mo (T2: I: 51.9 vs. C: 38.9**); lower prevalence (%) of dietary diversity in I for children 12–23 mo (T2: I: 12.1 vs. C: 22.4*); dietary diversity for 6–11 mo, SSSF timely introduction, feeding frequency for children 6–11 mo or 12–23 mo, NS.QualitativeFacilitators to DD: access to money, availability/access to foods, education, keeping small animals, having vegetable garden.Facilitators to IYCF/MCHN: community-level facilitators include changes in adherence to traditional and cultural norms around taboo foods for mothers (e.g., milk, beans), attributed to improved knowledge and engagement of community leaders.Barriers to IYCF/MCHN: household-level barriers include lack of male support and involvement, community-level barriers include traditional/cultural practices and beliefs, patriarchy, and gender norms |
| RAIN, Zambia (78) | RCT: I1: agriculture, gender equity, and women's empowerment, and BCC intervention (n = 634 mothers of child 0–23.9 mo); I2: agriculture and gender equity and women's empowerment intervention (n = 560 mothers of child 0–23.9 mo); C: standard government services (n = 724 mothers of child 0–23.9 mo)T1: baseline (2011); T2: endline (2015)DID: T1 vs. T2 for I1 vs. I2 vs. C | IYCF knowledge (DID): improved mean CF knowledge score for I1 (DID: I1 vs. C: 0.68**); I2 vs. C or I1 vs. I2, NS.CF indicators (DID): MMF, SSSF timely introduction, MDD, MAD, or consumption iron-rich foods for I1 or I2 vs. C, NS.Anthropometric indicators (DID): HAZ, WHZ, stunting, or wasting for I1 or I2 vs. C, NS.Qualitative:Barriers to dietary diversity: barrier analysis identified perceived self-efficacy and perceived social norms as key determinants |
| SPRING-Niger (79) | SSI and FDG (SSI: only wife reached: n = 5 husbands, 5 wives; both husband and wife reached: n = 5 husbands, 5 wives; FGD: 10 FGDs with community members at T1)T1: 2016; T2: 2017 | Qualitative Changes in joint decision making: some husband/wives discussed child's nutrition (e.g., CF, DD) after seeing videos; other husband/wives reported no discussion of family health/nutrition.Changes in male involvement: some husbands reported supporting wives by buying more varied foods; some wives and husbands reported that men purchased and brought home more food, including more diverse foods.Changes in CF knowledge: men reported learning about proper nutrition in the first 1000 days from videos, discussions with neighbors/friends, and from home visits from the peer educators.Barrier to DD: access to income |
| USAID Engine, Ethiopia (86) | QE, FGD, and qualitative observations: I: intervention participants; no comparison group (QE: n = 41 mothers of children 0–6 mo, 30 fathers of children 0–23 mo, FGD: 3 FGDs with mothers, fathers, grandmothers, 4–6 participants each; observations: direct observations of 9 participant mothers as they prepared porridge for children)T1: baseline (2016); T2: endline (2016)T1 vs. T2 | CF indicators (T1 vs. T2): increase in prevalence (%) of timely introduction of CF, MDD, consumption of ASFs (no analysis of statistical significance presented, limiting interpretation).WASH (T1 vs. T2): increase in % of men and women handwashing before serving meals, before preparing food, before eating, after eating, before feeding child, and after feeding child (no analysis of statistical significance presented, limiting interpretation).QualitativeSelf-reported behavior change: FGD mothers reported adding ASF to children's meals, feeding children fruits/vegetables, washing children after latrine/toilet, resting more during pregnancy, increasing DD of pregnant women.Change in IYCF practices: 100% of mothers observed to correctly prepared porridge with ASFs; FGD found improvement in DD of mothers/children attributed to knowledge/skills from program; FGD: mothers learned nutritious foods to buy at market, produce at home, and feed to children.Change in WASH practices: 100% of mothers observed to practice handwashing before preparing and serving porridge; FGD found mothers practiced handwashing at critical points, usage of latrines.Change in joint decision making: FGD mothers found family dialogue on nutrition and nutrition-related decision making led to improvements in children's diets.Program implementation: 73% of mothers understand ASF educational tool (STAR tool); 43% understand DD educational tool (Gulicha tool); 35% understand full meaning of DD educational tool (Gulicha tool) |
| USAID NOURISH, Cambodia (75) | QE: I: intervention area (n = 943 children 6–59 mo); no comparison groupT1: baseline (2016); T2: endline (2018)T1 vs. T2 | CF indicators (T1 vs. T2): increased prevalence (%) of MAD and child consumption of animal origin foods, eggs, vitamin A–rich foods, and small fish (T2–T1: 24.4*, 14.5*, 15.9*, 43.7*, 11.0*); decreased consumption of beans, nuts and seeds, and dairy (T2–T1: −10.2*, −14.2); MDD or grain consumption, NS.Unhealthy foods (T1 vs. T2): decreased prevalence (%) of child consumption of packaged snacks (T2–T1: −18*); child consumption of sugary foods, NS.Responsive feeding (T1 vs. T2): increased prevalence (%) of child telling when s/he feels hungry or full (reported by parent), child signaling hunger to caregiver, caregivers having positive behaviors and attitudes toward involvement in feeding, caregivers encouraging the child to eat, and caregivers re-trying food (T2–T1: 14*, 9.3*, 7.6*, 7.6*, 7.6*).Early Child Development (T1 vs. T2): increased prevalence (%) of caregivers of children <2 y providing age-appropriate stimulation of children according to child care and development standards (T2–T1: 15*).WASH (T1 vs. T2): increase in % of households with soap/water present at handwashing stations (T2–T1: 19*).Anthropometric indicators (T1 vs. T2): decreased prevalence (%) in stunting (T2–T1: −19, significance not reported); increased prevalence of underweight and wasting (T2–T1: 4.4, 1.6, significance not reported); no significant change in anemia prevalence |
| USAID Nurture, Lao PDR (81) | QE, KII, FGDs at midline: I intervention households (QE: n = 1978 households with child <2 y; 41 KII and 12 FGDs: n = 98 total respondents); C: matched control households (QE: n = 1928 households with child <2 y)T1: baseline (2018); T2: midline (2019)I vs. C at T2; DID: T1 vs. T2 for I vs. C | CF indicators (I vs. C at T2): increased likelihood of achieving MMF or MAD (I vs. C: 1.35, 1.67; significant but P values not reported); nonsignificant difference for MDD.Anthropometric indicators (DID): nonsignificant DID for stunting, wasting, and underweight prevalence among children <2 y.WASH (DID): increased prevalence (%) of handwashing after child uses toilet and before preparing children's food (DID: significant but DID or P values not reported); using soap at handwashing stations, giving children safe drinking water, and access to basic sanitation facility, NS.QualitativeBarriers influencing program impact: farm environment challenging for caregiving, limited access to CF, traditional/cultural beliefs on child-led feeding, mother's high workload limits time for feeding, lack of motivation |
| USAID Suaahara II, Nepal (87) | Postintervention analysis: I: households exposed to IPC, CM, MM programs (n = 1268 households with child <5 y); C: unexposed households (n = 2367 households with child <5 y)T: endline (2017)I (IPC, CM, MM) vs. C | CF indicators (I vs. C): positive association between MDD and MM (MM vs. C: OR: 1.38*), nonsignificant association between MDD and IPC or CM; nonsignificant association between DDS and IPC, CM, or MM.QualitativeProgram exposure: 1-y follow-up: one-third of mothers exposed to at least 1 platform (mass media most likely followed by CM events then IPC); two-thirds of mothers listening to mass media reported listening multiple times per month |
*P < 0.05; **P < 0.01; ***P < 0.001. ASF, animal-source food; BCC, behavior-change communication; C, comparison group; CF, complementary feeding; CHW, community health worker; CM, community mobilization; DDS, dietary diversity score; DID, difference-in-difference; FGD, focus group discussion; GM, grandmother; HAZ, height-for-age z score; I, intervention group; I1and I2 used when multiple intervention arms; IDI, in-depth interview; IPC, interpersonal counseling; IYCF, infant young child feeding; IYCN, infant and young child nutrition; KII, key informant interviews; MAD, minimum acceptable diet; MBNP, Mwanzo Bora Nutrition Program; MCHN, maternal child health and nutrition; MDD, minimum dietary diversity; MMF, minimum meal frequency; QE, quasi-experimental; RAIN, Realigning Agriculture for Improved Nutrition; RCT, randomized controlled trial; SPRING, Strengthening Partnerships, Results, and Innovations in Nutrition Globally; SSI, semi-structured interview; SSSF, solid and semi-solid foods; T, time point; TDHS, Tanzania Demographic and Health Survey; USAID, US Agency for International Development; WASH, water, sanitation, and hygiene; WAZ, weight-for-age z score; WHZ, weight-for-height z score.
Norms, perceptions, and diffusion of information
Two studies explicitly evaluated perceived changes in social norms using quantitative measures (53, 70) and both found changes in social and cultural norms supportive of CF practices.
Alive & Thrive Bangladesh found a significantly higher proportion of mothers in intervention areas said they knew other mothers who had adopted optimal IYCF practices (e.g., descriptive norms) at endline, compared with the nonintensive comparison area. There was an increase from endline to 2-y follow-up in the proportion of mothers in both the intervention and comparison areas who said their peers supported appropriate CF practices such as feeding ASFs to children >6 mo old, mashing cooked foods, and feeding children at least 3 times/d (injunctive norms). At endline, there was significantly more IYCF knowledge-sharing by mothers receiving the norms-focused intervention, compared with nonintensive areas; and then, by follow-up, knowledge-sharing increased significantly in both groups. In path analysis, increased knowledge-sharing, mothers’ social networks, and changes in social norms explained 34–43% of total program impact on CF (53).
In Malawi, the Hygienic Families intervention targeting WASH practices related to CF found significantly greater improvements from baseline to endline in intervention area caregivers’ perceptions of positive social norms—that is, others’ behavior in the household, others’ behavior in the village, and others’ approval for handwashing and food hygiene (e.g., washing and storing utensils) behaviors (70). Multiple mediation analysis, used to determine which factors were impacted by the intervention and led to behavior changes, found that perceptions of others’ behavior in the household mediated the effects of the intervention on handwashing and washing utensils with soap. Perceptions of others’ behavior in the village mediated improvements in storing utensils in a safe place. While a range of risk, attitude, norms, ability, and self-regulation factors were measured, these norms were among the few factors found to significantly influence behaviors in mediation models.
Qualitative findings on norms, barriers, and facilitators of behavior change
Five programs described barriers to achieving program impact in their qualitative findings (60, 72, 77, 79, 81), with 3 citing existing cultural norms or traditional beliefs (44, 46, 72).
Mwanzo Bora in Tanzania found that gender norms and traditional patriarchal beliefs were continuing challenges to changing cultural practices or increasing partner support and joint decision making (60). Other programs cited social norms generally as barriers, along with structural and individual-level barriers and environmental changes.
Three programs reported facilitators of program impact, including existing community support and relationships, health and education infrastructure, and access to resources (e.g., home gardens, animal husbandry, income, food) (59, 60, 72). Mwanzo Bora was unique in citing how social norms changes—specifically, fewer food taboos—facilitated improved nutrition practices (60). Analysis of focus group discussions and key informant interviews identified changes in structural and household factors facilitating maternal and child nutrition, including CF practices. Program participants attributed the elimination of harmful cultural taboos to increased IYCF knowledge, although they described general shifts in social norms rather than CF-specific norms.
Male engagement and joint decision making emerged as themes in several qualitative evaluations. Participants in Mwanzo Bora described increases in male support and involvement in IYCF practices, and this change was attributed to SBC promotion activities and inclusion of community leaders (60). Women respondents in the Kanyakla project reported that greater men's participation in nutrition programs led to improvements in nutrition practices (73). SPRING-Niger also found program participation led to increased discussion of child's nutrition and CF among some couples (79). In Kenya, fathers who participated in dialogue groups and discussed gender norms then supported their wives and children by providing nutritious foods, assisting with childcare and chores, and accompanying or bringing them to the health center (71). This infant and young child nutrition (IYCN) dialogue project also reported increased grandmother involvement in child feeding practices, with grandmother group members reporting improved hygiene and child feeding practices and recognition for “their role as infant feeding advisors within their families and communities” (59).
Overall intervention effectiveness on CF outcomes: knowledge, practices, and child growth
As noted above, we did not find evaluations designed to compare intervention arms that differed only by inclusion of norms-focused components. This section summarizes evaluations of overall impacts on CF and child nutrition outcomes of multifaceted interventions that included some focus on social norms (see intervention descriptions in Table 3 and section on Objective 2). To include a comprehensive range of programs, we chose not to exclude evaluations based on research design, and variation in quality must be considered in interpreting results. While 12 program evaluations used cluster-randomized or quasi-experimental evaluation designs with comparison groups and measured preintervention to postintervention change, 3 evaluations had pre-post designs with no comparison groups (67,75, 86) and 2 only compared intervention with nonintervention communities at endline (60, 87). Not all quantitative studies reported rigorous statistical analysis.
Five evaluations assessed changes in CF knowledge: 3 on mothers’ knowledge of CF practices (65, 66, 68, 78), 1 on grandmothers’ nutrition knowledge (74), and 1 in community health volunteers’ nutrition knowledge (73). All included comparison or nonintensive communities and all but 1 study (65) found significant improvements in CF knowledge.
Fourteen evaluations assessed at least 1 WHO indicator for CF (92), including timely introduction of solid, semisolid or soft foods, minimum dietary diversity, minimum meal frequency, minimum acceptable diet, and consumption of iron-rich foods. Five evaluations assessed other CF practices, including consumption of unhealthy foods, ASFs, or fruit and vegetables. Less commonly measured outcomes included responsive feeding practices (1 study) and appropriate handwashing practices or use of soap and water (4 studies). Five programs measured stunting or height-for-age z score (HAZ) (73, 78). As described in more detail in Table 4 and below, 13 of the 15 evaluations that measured CF practices reported improvements in at least some CF practices, with 2 reporting nonsignificant effects or a decrease in optimal practices. All but 4 evaluations (60, 67, 75, 81) compared treatment groups with a control and conducted baseline to endline or follow-up difference-in-difference analyses.
In 8 studies, minimum acceptable diet was significantly higher at endline for intervention as compared with reference groups or, if no comparison, increased from baseline to endline (67, 75). Two exceptions found few, if any, significant impacts on CF indicators (73, 78). Timely introduction of soft foods improved in most programs that measured this indicator. In contrast, minimum dietary diversity, consumption of iron-rich foods, and minimum meal frequency did not significantly improve in about half of the interventions that measured these indicators. Two studies measured consumption of unhealthy foods: one reported a decrease (75) and the other no change (84). All 4 studies reporting ASF consumption found significant increases (62, 71,75, 86). In NOURISH, the only program to assess improvements in responsive feeding, caregivers significantly improved in understanding and responding to children's hunger and satiety cues between baseline and endline (75).
Appropriate handwashing practices were significantly higher in all 4 of the studies that measured this indicator. Three programs reported improvements in handwashing at critical times from baseline to endline (70,81, 86). The Hygienic Family project also found significantly greater improvements in intervention versus control groups in washing kitchen utensils with soap and keeping utensils in a safe place (70). NOURISH found significantly increased presence of soap and water at handwashing stations at endline (75) but Nurture reported no effect (81).
Five programs measured stunting or HAZ and all reported declines in stunting from baseline to endline in both the intervention and control arms. Only one reported a significant intervention impact, finding reduced stunting in intensive versus nonintensive intervention groups (68).
Discussion
To explore normative influences on CF, we reviewed the scope of relevant social norms, the ways they have been addressed in nutrition-specific or multisectoral interventions promoting CF in low-income and low–middle-income country settings, and the evidence of intervention effectiveness. Despite growing attention to how social norms impact health behavior (16), there is limited evidence that social norms have been integrated into research and programs focused on CF.
Increasing recognition of the influence of social norms on CF is captured in a WHO framework on childhood stunting, which lists beliefs and norms among the social and cultural factors underlying inadequate CF and other determinants of stunting (18). Similarly, the Nurturing Care framework includes positive social norms as fundamental to enabling family and community environments that support adequate nutrition and responsive caregiving of young children (8). However, as yet, we lack a specific framework that adequately addresses how and to what extent social norms influence young child feeding and how norms across the relevant sectors can be leveraged to improve nutrition. We hope this review provides a starting point for understanding social norms and their influences on CF that would underlie a more explicit model, but clearly, more real-world implementation research is needed to inform effective norms-focused intervention approaches.
Key dimensions of CF practices identified by UNICEF pertain to “what children should eat” (i.e., providing diverse and nutrient-dense foods, ASFs, fruits and vegetables and avoiding foods with low nutrient value) and to “when and how are children fed” (i.e., timely introduction, age-appropriate meal frequency, amount and food consistency, responsive feeding, and hygienic food preparation and use) (1). Many influential social norms are also related to family roles, decision making, gender, and women's status, which we categorized using the additional dimension, “who is responsible for child feeding.”
To address our first objective, we summarized reports describing social norms and perceptions related to any of these dimensions and thereby likely to support or hinder adoption of recommended CF practices. Most of the reports we identified focused on what children were fed, including views that only dilute cereal-based foods are appropriate, and concerns about negative physical, developmental, and behavioral impacts of ASFs. Norms related to child autonomy in choosing foods can lead to provision of processed, sweetened foods. Strong religious and cultural norms influenced feeding in some contexts. Norms and beliefs about “when” to introduce CF led to early introduction in many contexts. Perceptions of social approval predict practices related to hygienic food preparation. Few studies reported norms related to “how” infants and young children were fed, with little information on norms such as communal meals. The lack of attention to social norms related to responsive feeding was notable, given the cultural complexities in how parental sensitivity and responsiveness is expressed (93) and the relevance of responsive feeding practices to child well-being (94).
Beyond what, how, and when children are fed, social norms around family relationships and gender pertain to “who” feeds children or influences CF via resource and time allocation and food provisioning. Grandmothers’ roles in advising and decision making on child feeding can be negative, creating a need to shift the norms they enforce, or positive, providing a promising intervention strategy. Gender norms affect intrahousehold allocation of food, with implications for the availability of nutritious foods for young children, and women's workload, access to resources, and time to prepare foods and feed children hygienically, responsively, and nutritiously.
It is worth noting that reports rarely referred to social norms per se, and limited depth of information made it challenging to differentiate adherence to social norms from usual patterns of behavior reflecting food availability, affordability, convenience, and familiarity. However, these examples illustrate the variety of social norms and related beliefs to consider and potentially address in SBC interventions on CF.
Our second objective was to describe how interventions aimed to influence social norms and related perceptions to improve CF. Most interventions we identified included multiple entry points, primarily community engagement and media, often complemented by facility-based activities. In an overview of lessons learned in the Alive & Thrive interventions in 3 country contexts, Baker et al. (4) notes the need for IYCF interventions to combine community mobilization to support positive IYCF norms and mass media to reinforce messages and create enabling environments, together with interpersonal communication and capacity building. Activities that used drama, testimonials, facilitated discussion, and support groups seemed intended to leverage norms-shifting strategies (11). However, few reports provided explanation of the theoretical basis of interventions or how they were expected to address social norms.
Objective 3 examined evidence that interventions with norms-related components are effective. It is notable that very few studies measured outcomes related to social norms, perhaps a reflection of measurement challenges and lack of validated indicators of social norms. We identified 2 projects, Alive & Thrive Bangladesh (53) and the Hygienic Family intervention (70) that developed quantitative measures of individual perceptions of social norms and their influence, but there is a clear need for further development of valid and contextually appropriate measures. Qualitative research methods such as those used to evaluate Mwanzo Bora (60) are also useful for understanding shifts in social norms and influences that facilitate or hinder behavior change. The few evaluations that measured impacts on social norms or how they mediated effects on CF practices found evidence of effectiveness of norms-focused interventions.
More broadly, many of the evaluations of interventions that included social norms–focused activities found significant positive impacts on CF behaviors and related outcomes, suggesting effectiveness of including such strategies. An important caveat for interpreting these results is that the interventions used multiple strategies to address numerous drivers of CF practices and did not compare effectiveness with and without norms-related components. As such, we cannot draw conclusions on the relative contribution of the various components, norms-shifting and otherwise, to behavior change. Some evaluation designs lacked adequate comparisons to provide clear evidence that CF changes were due to the program.
The 3 objectives that structured this review align with 3 priorities we have identified as key steps needed to address social norms in nutrition interventions: 1) conducting formative research to understand norms in a given context, 2) designing interventions based on this formative research and theoretical models of behavior change, and 3) developing appropriate measures of social norms and evaluation and implementation research approaches to assess shifts in norms and perceptions that influence behavior.
The first step, conducting formative and participatory research in a given context, is needed to guide intervention design by identifying what norms matter, how they fit within the local culture, who influences child feeding, and how to reach those who influence relevant norms. To be useful, this research must go beyond asking about usual practices to explore behavioral drivers. An influential social norm can be identified at the individual level when a person behaves in a certain way out of fear of disapproval from elders or peers (injunctive norm) or because this is what is always done in their community (descriptive norm). This captures individual perceptions of social norms and their importance, which may be what matters most for changing behavior. Nutrition researchers can draw on resources in other sectors for insights on formative research approaches for identifying and understanding social norms and cultural beliefs (95–98).
Second, norms-focused interventions should be designed to fit the local context (based on formative research and community input) and also reflect theoretical models of social norms and how they work. While some studies discussed the rationale for including specific strategies, few identified theoretical underpinnings for their interventions. Reports on Mwanzo Bora and Alive & Thrive Bangladesh cited “diffusion of innovation” theory (99), which posits that a minority that adopts innovations can spread new behaviors and eventually create new norms for the broader community. Mukuria et al. (71) based the IYCN dialogue project on Gottlieb's (100) model of social support. Use of relevant theoretical frameworks is essential for designing stronger interventions and appropriate measures for evaluating how perceptions and norms influence behavior (16).
The third essential step is to develop valid indicators of relevant social norms and conduct implementation research to examine how and why change results from interventions. Beyond measurement challenges, research designs that permit direct comparisons of norms-shifting interventions with more traditional educational approaches are needed to draw causal conclusions about effectiveness. Such designs are not always feasible when implementing at scale; alternatively, careful assessment of intermediate outcomes, implementation, and coverage can help assess pathways of impact. In this review, interpretation was often constrained because evaluations did not collect data on intermediate variables expected to mediate between the intervention and outcomes, or indicators of fidelity and participation (101). Measuring change in social norms expected to impact behaviors would greatly enhance our understanding of whether and how norms-focused interventions work. Qualitative implementation research capturing the perspectives of those who deliver and participate in the programs, as well as community members who influence adherence to norms, is also important for providing insights on how norms-shifting approaches are viewed.
This review was not designed as a systematic review because we aimed to illustrate the scope of recent work from a range of study and intervention designs, rather than restrict our search to a single question or limited set of studies. We used structured methods to comprehensively search the published, peer-reviewed literature, but given the breadth of our objectives and paucity of published research, we also searched grey literature for examples of intervention approaches and evaluations and used a broad set of terms to capture the full scope of relevant work. Despite using search terms designed to identify projects across the spectrum of multisectoral nutrition, we found few interventions that assessed outcomes in areas such as early child development, WASH, agriculture, and food security. Research in these nutrition-sensitive fields on the impact of social, cultural, and gender norms (93, 102) but not in direct relation to CF would not have been identified in our search. However, a broader multisectoral review found results similar to ours in that many programs acknowledged the importance of norms, but explicit intervention approaches for normative change were rarely evident (103).
Limiting our search to reports since 2010 may have led to gaps in the norms identified. For example, earlier research has highlighted norms relevant to CF such as hand- or force-feeding (104, 105) and laissez-faire feeding styles with limited responsiveness or encouragement for eating (106). Perhaps such social norms were not relevant to CF practices in the communities described in recent reports, were not highlighted because they were reported in previous literature, or did not use terms that were identified by our search. It is also possible for social norms to change over time and become less salient for CF interventions.
One challenge was to identify when social norms were being addressed, even if referred to as traditions, cultural practices, or usual behaviors. A helpful approach for identifying norms-focused interventions was to consider whether the intervention strategies went beyond individual education to include community outreach and mass media activities that involved discussion, advocacy, dramatization, and mobilization related to perceptions of appropriate behavior or expectations.
Traditionally, CF interventions have tended to have a “a nutrition-centered perspective” (p. 4 in 107) with inadequate attention to cultural beliefs, norms, and values that could influence child feeding practices in specific contexts (107). The focus has been on individual knowledge, beliefs, and attitudes as determinants of behavior change, overlooking communal influences on behavior such as social norms even when espousing social and behavior-change strategies. Attitudes and perceptions are closely connected with social norms, but knowledge-based interventions are unlikely to change behaviors if motivations are rooted in perceptions that recommended practices deviate from the “normal” behavior of valued family or community members or could lead to disapproval or sanction from these reference groups (17, 97). It has also been noted in sectors other than nutrition that “programming tends to focus on changing individuals, with the assumption that the cumulative change of enough people's attitudes and beliefs will result in a change of norms…. Power differentials, reproduction of social structures, identity markers, misperceptions and other factors can enforce conformity even when a majority of individuals are ready to welcome change” (97). There is a need for more programming to influence social norms but Petit and Zalk note that this has been limited by lack of knowledge about norms’ importance, perceived complexity of translating the theory into application, difficulties in funding lengthy interventions that may be needed to shift norms, and measurement challenges.
Social norms are closely linked to cultural and social identity, which can raise concerns about the ethics of shifting norms. Some norms-focused strategies involve shaming, which can be harmful, discriminatory, or ineffective (108). These concerns reinforce the need for careful formative research and strong local collaborations to ensure sensitivity and contextually appropriate approaches, and attention to intracultural diversity in influences on child feeding (40). Building on and strengthening existing positive norms is recommended, as deeply rooted behavioral determinants can potentially improve lives beyond the focus of an intervention and impact broader communities (97). Social norms reflect the wider culture, interconnected with beliefs, expectations, traditions, and relationships that encompass much more than nutrition and care practices (109). Norms related to CF are influenced by political, economic, and food-system factors, as well as broader social norms such as those related to communication, socialization, female education, labor market participation, child marriage, domestic violence, and the status of women (110–112).
As noted above, recent conceptual frameworks on factors contributing to child nutrition (18) and nurturing care (8) recognize the salience of social norms as one part of a complex range of behavioral determinants of CF. In concert with social norms, individual factors such as attitudes, skills, and self-efficacy also determine intentions and behaviors, as do environmental and economic constraints, and complex behaviors cannot be changed using norms-responsive intervention strategies alone (16). For CF, relevant determinants include food cost, food access and seasonality, time and fuel for meal preparation and feeding, and access to other resources. For example, we found multiple reports of normative beliefs that led to avoiding feeding ASFs to young children, but it is difficult to ascertain to what extent this actually reflects adherence to social norms, given other important barriers such as cost and availability (6, 113). This may contrast with breastfeeding promotion, if social norms are the primary barrier to changing practices such as delayed initiation or prelacteal feeds and time and expense are less relevant. Reviews on engaging fathers and grandmothers to support exclusive breastfeeding indicate that social norms are often addressed in these breastfeeding interventions through community-based events, facilitated discussions, and support groups to help individuals accept and support nonnormative practices (114, 115).
Thus, despite the important influence of social norms and the need for more and stronger norms-focused research and interventions, individual behaviors are based on multiple factors and it is critical to understand the range of relevant behavioral determinants in a given context before designing an intervention approach. As cautioned by Petit and Zalk (97), “practitioners should not develop ‘social norms strategies’, but behavior change strategies that properly consider, address and leverage social norms.”
In conclusion, social norms and related cultural beliefs are recognized as influential potential barriers or facilitators for adoption of improved CF practices. Promising interventions are being developed that consider social norms and the need for innovative and feasible strategies that reach and mobilize key influencers. There is evidence that interventions with norms-focused components can improve CF practices. However, most research to date was not designed to measure change in norms and related perceptions so cannot assess the direct effect of norms-focused components or gauge whether normative changes played a role in the pathway from intervention to CF practices.
The interventions identified in this review used multiple approaches to shift or build on social norms, primarily through community engagement and mass media. Most interventions focused on CF practices identified in global guidelines, and many addressed norms related to family and gender roles, as well as community perceptions of appropriate child feeding. Results suggest that exploring and addressing social norms to improve CF might have most leverage in areas such as exclusion of foods based on health-related beliefs and typologies, responsive feeding, food hygiene, gender norms, and family roles. Despite a search designed to include multisectoral approaches, we found few norms-focused interventions linking CF to agriculture, parenting and early child development, or other nutrition-sensitive sectors.
To better understand the role of social norms and how to tailor interventions to harness their influence, there is a need for formative research on existing norms and strength of their influence in the broader cultural and community context, design of intervention activities based on principles for normative change, and use of appropriate assessment and evaluation designs. Insights on social norms and perceptions and how they relate to CF outcomes can contribute to the creation of effective, multifaceted, and culturally relevant interventions.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—KLD: designed the research; all authors participated in the design of the search and review of papers; JKM, KL, and FMC conducted data extraction and summarized results; all authors contributed to writing and revising the paper; KLD has primary responsibility for final content. All authors have read and approved the final manuscript. We are very grateful for helpful guidance and contributions that clarified and strengthened the paper from Laura Itzkowitz and Qwamel Hanks (USAID). We thank Lisa Sherburne, (USAID Advancing Nutrition) for her technical support and multiple reviews of drafts. We appreciate the constructive feedback to improve this paper from Ashley Aakesson, Silvia Alayon, Altrena Mukuria, and Kelsey Torres (USAID Advancing Nutrition).
Notes
The US Agency for International Development (USAID) provided financial support for this article through its flagship multisectoral nutrition project, USAID Advancing Nutrition. It was prepared under the terms of contract 7200AA18C00070 awarded to JSI Research & Training Institute, Inc.
Author disclosures: The authors report no conflicts of interest.
The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the US government.
Supplemental Box 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Abbreviations used: ASF, animal-source food; CF, complementary feeding; CHW, community health worker; HAZ, height-for-age z score; IYCF, infant and young child feeding; IYCN, infant and young child nutrition; SBC, social and behavior change; SPRING, Strengthening Partnerships, Results, and Innovations in Nutrition Globally; USAID, US Agency for International Development; WASH, water, sanitation, and hygiene.
Contributor Information
Katherine L Dickin, Email: kld12@cornell.edu, Program in International Nutrition, Division of Nutritional Sciences, Cornell University, Ithaca, NY, USA; USAID Advancing Nutrition, Crystal City, VA, USA.
Kate Litvin, USAID Advancing Nutrition, Crystal City, VA, USA.
Juliet K McCann, Program in International Nutrition, Division of Nutritional Sciences, Cornell University, Ithaca, NY, USA.
Fiona M Coleman, Program in International Nutrition, Division of Nutritional Sciences, Cornell University, Ithaca, NY, USA.
References
- 1. UNICEF . Improving young children's diets during the complementary feeding period. [Internet]. New York: UNICEF Programming Guidance; 2020; [cited 2020 May 13]. Available from: https://www.unscn.org/en/news-events/recent-news?idnews = 2030. [Google Scholar]
- 2. UNICEF . Infant and young child feeding: UNICEF data. [Internet]. New York; 2019. [Cited 2020 Apr 7]. Available from:https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/. [Google Scholar]
- 3. World Health Organization . Complementary feeding. [Internet]. Geneva (Switzerland): World Health Organization; 2018. [Cited 2020 Jan 17]. Available from: https://www.who.int/nutrition/topics/complementary_feeding/en/. [Google Scholar]
- 4. Baker J, Sanghvi T, Hajeebhoy N, Abrha TH. Learning from the design and implementation of large-scale programs to improve infant and young child feeding. Food Nutr Bull. 2013;34(Suppl 3):S226–30. [DOI] [PubMed] [Google Scholar]
- 5. Piwoz EG, Huffman SL, Quinn VJ. Promotion and advocacy for improved complementary feeding: Can we apply the lessons learned from breastfeeding?. Food Nutr Bull. 2003;24(1):29–44. [DOI] [PubMed] [Google Scholar]
- 6. Pelto GH, Armar-Klemesu M, Siekmann J, Schofield D. The focused ethnographic study “assessing the behavioral and local market environment for improving the diets of infants and young children 6 to 23 months old” and its use in three countries. Matern Child Nutr. 2013;9(Suppl 1):35–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sanghvi T, Jimerson A, Hajeebhoy N, Zewale M, Nguyen GH. Tailoring communication strategies to improve infant and young child feeding practices in different country settings. Food Nutr Bull. 2013;34(3):S169–80. [DOI] [PubMed] [Google Scholar]
- 8. World Health Organization; United Nations Children's Fund; World Bank Group . Nurturing care for early childhood development: a framework for helping children survive and thrive to transform health and human potential. [Internet]. Geneva (Switzerland); 2018. [Cited 2020 Dec 29]. Available from: https://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf. [Google Scholar]
- 9. Contento IR. Nutrition education: linking research, theory, and practice. Asia Pac J Clin Nutr. 2008;17(Suppl 1):176–9. [PubMed] [Google Scholar]
- 10. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 11. The Learning Collaborative to Advance Normative Change . Identifying and describing approaches and attributes of norms-shifting interventions. [Internet]. Washington (DC): Institute for Reproductive Health, Georgetown University; 2017. [Cited 2020 May 8]. Available from: http://irh.org/resource-library/identifying-and-describing-approaches-and-attributes-of-normative-change-interventions-background-paper/. [Google Scholar]
- 12. Bicchieri C, Mulddon R, Sontuoso A. Social norms. [Internet]. The Stanford encyclopedia of philosophy. Palo Alto (CA); 2018; . [Cited 2020 Apr 7]. Available from: https://plato.stanford.edu/entries/social-norms/. [Google Scholar]
- 13. Cialdini RB, Trost MR. Social influence: social norms, conformity and compliance. In: Gilbert DT, Fiske ST, Lindzey G, eds. The handbook of social psychology. Vol 2, 4th ed. New York: McGraw-Hill; 1998. p. 151–92. [Google Scholar]
- 14. Stiff JB. Persuasive communication. New York: Guilford Press; 1994. [Google Scholar]
- 15. Institute for Reproductive Health Georgetown University; Save Children for the the US Agency for International Development (USAID) . Scaling up normative change interventions for adolescent and youth sexual and reproductive health: literature review findings and recommendations. [Internet]. Washington (DC); 2016. [Cited 2020 Apr 7]. Available from: http://irh.org/wp-content/uploads/2016/10/Scaling_Up_AYSRH_Norm_Change_Interventions.pdf. [Google Scholar]
- 16. Cislaghi B, Heise L. Using social norms theory for health promotion in low-income countries. Health Promot Int. 2019;34(3):616–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The Learning Collaborative to Advance Normative Change . Social norms and AYSRH: building a bridge from theory to program design. [Internet]. Washington (DC); 2019. [Cited 2020 May 13]. Available from:http://irh.org/wp-content/uploads/LC_Theory__Build_Bridge_Theory_to_Program_Design_07192019.pdf. [Google Scholar]
- 18. Stewart CP, Iannotti L, Dewey KG, Michaelsen KF, Onyango AW. Contextualising complementary feeding in a broader framework for stunting prevention. Matern Child Nutr. 2013;9(Suppl 2):27–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Black MM, Lutter CK, Trude ACB. All children surviving and thriving: re-envisioning UNICEF's conceptual framework of malnutrition. Lancet Glob Heal. 2020;8(6):e766–7. [DOI] [PubMed] [Google Scholar]
- 20. Pelto GH, Levitt E, Thairu L. Improving feeding practices: current patterns, common constraints, and the design of interventions. Food Nutr Bull. 2003;24(1):45–82. [DOI] [PubMed] [Google Scholar]
- 21. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 22. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. [DOI] [PubMed] [Google Scholar]
- 23. Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. Chapter 11: scoping reviews. [Internet]. In: Aromataris E, MunnZ,. Joanna Briggs Institute Reviewer's Manual. JBI; 2020. [Cited 2020 May 13]. Available from:https://reviewersmanual.joannabriggs.org/. [Google Scholar]
- 24. Dewey K. Guiding principles for complementary feeding of the breastfed child. [Internet]. Washington (DC); 2003; . [Cited 2020 Apr 26]. Available from:https://iris.paho.org/handle/10665.2/752. [Google Scholar]
- 25. World Bank Group . World Bank Country and Lending Groups. [Internet]. 2020. [Cited 2020 Jul 8]. Available from:https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. [Google Scholar]
- 26. CORE Group z CORE Group Nutrition Working Group Listserv Archive . [Internet]. Washington (DC); [cited 2020 Feb 18]. Available from: https://lists.coregroup.org/lists/arc/nutrition. [Google Scholar]
- 27. CORE Group . CORE Group SBC Working Group Listserv Archive. [Internet]. Washington (DC); [cited 2020 Feb 18]. Available from: https://lists.coregroup.org/lists/arc/sbc. [Google Scholar]
- 28. Springboard Compass . Breakthrough ACTION Springboard Archive site. [Internet]. [Cited 2020 Feb 18]. Available from:https://springboardforsbc.org/forum. [Google Scholar]
- 29. USAID . Development Experience Clearinghouse. [Internet]. Washington (DC); [cited 2020 Feb 18]. Available from: https://dec.usaid.gov/dec/home/Default.aspx. [Google Scholar]
- 30. The Manoff Group . Understanding the context for promoting nutrition-enhancing behavior among households with severe resource constraints. Phnom Penh (Cambodia): USAID NOURISH Project; 2015. [Google Scholar]
- 31. USAID Engine . Mothers’ infant and young child feeding practices and their determinants in Amhara and Oromia regions. [Internet]. Addis Ababa (Ethiopia): Save the Children; 2014. [Cited 2020 May 13]. Available from: https://gtn-learning.org/node/170. [Google Scholar]
- 32. Kram N, Melgen S, Kedera E, Collison DK, Colton J, Blount W, Grant F, Girard AW. The acceptability of dietary tools to improve maternal and child nutrition in western Kenya. Public Health Nutr. 2016;19(10):1823–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Karigi LN, Mutuli LA, Bukhala PB. Socio-cultural practices and beliefs influencing infant and young child feeding in Lubao sub-location Kakamega County. J Nutr Heal Food Eng. 2016;5(1):568–71. [Google Scholar]
- 34. Reboot & Picture Impact . Alive and Thrive Nigeria Formative Research: Research Findings Report. Alive & Thrive; 2017. [Google Scholar]
- 35. Kinabo J, Mwanri AW, Mamiro P, Bundala N, Picado J, Kulwa K, Msuya J, Ntwenya J, Nombo A, Mzimbiri Ret al. . Infant and young child feeding practices on Unguja Island in Zanzibar, Tanzania: a ProPAN based analysis. Tanzan J Health Res. 2017;19(3). [Google Scholar]
- 36. USAID Nurture . Formative research and gender analysis. [Internet]. Washington (DC); 2017. [Cited 2020 Aug 23]. Available from: https://resourcecentre.savethechildren.net/library/formative-research-and-gender-analysis. [Google Scholar]
- 37. Chege PM, Kimiywe JO, Ndungu ZW. Influence of culture on dietary practices of children under five years among Maasai pastoralists in Kajiado, Kenya. Int J Behav Nutr Phys Act. 2015;12:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schnefke C. Alive & Thrive Nigeria: baseline qualitative data report. Washington (DC): Alive & Thrive; 2017. [Google Scholar]
- 39. Lagerkvist CJ, Mutiso JM, Okello JJ, Muoki P, Oluoch-Kosura W, Heck S. Predictors of intention to integrate biofortified orange-fleshed sweet potato in child feeding: a field information experiment in rural Kenya. Ecol Food Nutr. 2020;1–24. [DOI] [PubMed] [Google Scholar]
- 40. Kalra N, Pelto G, Tawiah C, Zobrist S, Milani P, Manu G, Laar A, Parker M. Patterns of cultural consensus and intracultural diversity in Ghanaian complementary feeding practices. Matern Child Nutr. 2018;14:e12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Oloko M, Ekpo R. Exploring traditional weaning practices in north western Nigeria; food, knowledge and culture: a step towards safeguarding community food security. Acad J Interdiscip Stud. 2018;7(2):97–106. [Google Scholar]
- 42. de Sa J, Bouttasing N, Sampson LS, Perks C, Osrin D, Prost A. Identifying priorities to improve maternal and child nutrition among the Khmu ethnic group, Laos: a formative study. Matern Child Nutr. 2013;9:452–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Haileselassie M, Redae G, Berhe G, Henry CJ, Nickerson MT, Tyler B, Mulugeta A. Why are animal source foods rarely consumed by 6–23 months old children in rural communities of northern Ethiopia? A qualitative study. [Internet]. PLoS One. 2020;15(1):e0225707. Available from: ! 10.1371/journal.pone.0225707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Suaahara . Suaahara Radio Program Design Document: phase I (26 Episodes). [Internet]. Kathmandu (Nepal); 2014; . [Cited 2020 Mar 30]. Available from: https://www.savethechildren.org/content/dam/global/reports/health-and-nutrition/suaahara-radio-design.pdf. [Google Scholar]
- 45. Conrad A. Selected literature review of maternal and child nutrition, and program observations. Washington (DC): USAID NOURISH, Cambodia; 2014. [Google Scholar]
- 46. Iqbal K, Hutchinson C, Tanasugarn C. A social ecological approach to develop a nutrition education program for preventing iron deficiency anemia in young children in rural Pakistan. Ecol Food Nutr. 2018;57(6):473–88. [DOI] [PubMed] [Google Scholar]
- 47. Bazzano AN, Potts KS, Mulugeta A. How do pregnant and lactating women, and young children, experience religious food restriction at the community level? A qualitative study of fasting traditions and feeding behaviors in four regions of Ethiopia. PLoS One. 2018;13(12):e0208408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kumera G, Tsedal E, Ayana M. Dietary diversity and associated factors among children of Orthodox Christian mothers/caregivers during the fasting season in Dejen District, North West Ethiopia. Nutr Metab (Lond). 2018;15(16):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bekele H, Turyashemererwa F. Feasibility and acceptability of food-based complementary feeding recommendations using Trials of Improved Practices among poor families in rural Eastern and Western Uganda. Food Sci Nutr. 2019;7(4):1311–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kavle J, Mehanna S, Saleh G, Fouad MA, Ramzy M, Hamed D, Hassan M, Khan G, Galloway R. Exploring why junk foods are “essential” foods and how culturally tailored recommendations improved feeding in Egyptian children. Matern Child Nutr. 2015;11(3):346–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kogade P, Gaidhane A, Choudhari S, Khatib MN, Kawalkar U, Gaidhane S, Zahiruddin QS. Socio-cultural determinants of infant and young child feeding practices in rural India. Med Sci. 2019;23(100):1015–22. [Google Scholar]
- 52. MacDonald CA, Aubel J, Aidam BA, Girard AW. Grandmothers as change agents: developing a culturally appropriate program to improve maternal and child nutrition in Sierra Leone. Curr Dev Nutr. 2020;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Nguyen PH, Frongillo EA, Kim SS, Zongrone AA, Jilani A, Tran LM, Sanghvi T, Menon P. Information diffusion and social norms are associated with infant and young child feeding practices in Bangladesh. J Nutr. 2019;149(11):2034–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Aubel J, Diallo K. Qualitative study on maternal and child health and nutrition in Guerou and Mbagne, Mauritania. MauritaniaPub: World Vision Mauritania; 2019. [Google Scholar]
- 55. GAIN . Improving childhood nutrition by changing infant feeding practices in Sidoarjo, East Java: a GAIN formative research and design case study. [Internet]. Jakarta (Indonesia); 2016. [Cited 2021 Jan 25]. Available from:https://www.gainhealth.org/resources/reports-and-publications/improving-childhood-nutrition-changing-infant-feeding-practices. [Google Scholar]
- 56. Chidziwisano K, Slekiene J, Kumwenda S, Mosler H-J, Morse T. Toward complementary food hygiene practices among child caregivers in rural Malawi. Am J Trop Med Hyg. 2019;101(2):294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sanghvi T, Haque R, Roy S, Afsana K, Seidel R, Islam S, Jimerson A, Baker J. Achieving behaviour change at scale: Alive & Thrive's infant and young child feeding programme in Bangladesh. Matern Child Nutr. 2016;12(Suppl 1):141–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kodish S, Aburto N, Hambayi M, Kennedy C, Gittelsohn J. Identifying the sociocultural barriers and facilitating factors to nutrition-related behavior change: formative research for a stunting prevention program in Ntchisi, Malawi. Food Nutr Bull. 2015;36(2):138–53. [DOI] [PubMed] [Google Scholar]
- 59. Thuita F, Martin SL, Ndegwa K, Bingham A, Mukuria AG. Engaging fathers and grandmothers to improve maternal and child dietary practices: planning a community-based study in western Kenya. African J Food Agric Nutr Dev. 2015;15(5):10386–405. [Google Scholar]
- 60. ICF and FXBT Health . Assessment of the Mwanzo Bora Nutrition Program Social and Behavior Change Communication Interventions. [Internet]. 2017. [Cited 2020 May 13]. Available from:https://www.africare.org/wp-content/uploads/2018/05/ICF-Final-Assessment-Report-on-MBNP-December-2017-1.pdf. [Google Scholar]
- 61. Kavle J, Pacque M, Dalglish S, Mbombeshayi E, Anzolo J, Mirindi J, Tosha M, Safari O, Gibson L, Straubinger Set al. . Strengthening nutrition services within integrated community case management (iCCM) of childhood illnesses in the Democratic Republic of Congo: evidence to guide implementation. Matern Child Nutr. 2019;15(Suppl 1):e12725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Keats E, Das J, Salam R, Lassi Z, Imdad A, Black R, Bhutta Z. The Baduta Programme in East Java, Indonesia: “What Works in Communicating for Better Nutrition?” GAIN Working Paper Series #1. Geneva (Switzerland): GAIN; 2019. [Google Scholar]
- 63. Mosler H-J. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: a conceptual model, a review, and a guideline. Int J Environ Health Res. 2012;22(5):431–49. [DOI] [PubMed] [Google Scholar]
- 64. Frongillo EA, Nguyen PH, Saha KK, Sanghvi T, Afsana K, Haque R, Baker J, Ruel MT, Rawat R, Menon P. Large-scale behavior-change initiative for infant and young child feeding advanced language and motor development in a cluster-randomized program evaluation in Bangladesh. J Nutr. 2017;147(2):256–63. [DOI] [PubMed] [Google Scholar]
- 65. Menon P, Nguyen PH, Saha KK, Khaled A, Sanghvi T, Baker J, Afsana K, Haque R, Frongillo EA, Ruel MTet al. . Combining intensive counseling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth: results of a cluster-randomized program evaluation in Bangladesh. J Nutr. 2016;146(10):2075–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Kim SS, Nguyen PH, Tran LM, Sanghvi T, Mahmud Z, Haque MR, Afsana K, Frongillo EA, Ruel MT, Menon P. Large-scale social and behavior change communication interventions have sustained impacts on infant and young child feeding knowledge and practices: results of a 2-year follow-up study in Bangladesh. J Nutr. 2018;148(10):1605–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kim SS, Rawat R, Mwangi EM, Tesfaye R, Abebe Y, Baker J, Frongillo EA, Ruel MT, Menon P. Exposure to large-scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLoS One. 2016;11(10):e0164800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kim SS, Nguyen PH, Yohannes Y, Abebe Y, Tharaney M, Drummond E, Frongillo EA, Ruel MT, Menon P. Behavior change interventions delivered through interpersonal communication, agricultural activities, community mobilization, and mass media increase complementary feeding practices and reduce child stunting in Ethiopia. J Nutr. 2019;149(8):1470–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Rawat R, Nguyen PH, Tran LM, Hajeebhoy N, Van Nguyen H, Baker J, Frongillo EA, Ruel MT, Menon P. Social franchising and a nationwide mass media campaign increased the prevalence of adequate complementary feeding in Vietnam: a cluster-randomized program evaluation. J Nutr. 2017;147(4):670–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chidziwisano K, Slekiene J, Mosler H-J, Morse T. Improving complementary food hygiene behaviors using the risk, attitude, norms, ability, and self-regulation approach in rural Malawi. Am J Trop Med Hyg. 2020;102(5):1104–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Mukuria AG, Martin SL, Egondi T, Bingham A, Thuita F. Role of social support in improving infant feeding practices in Western Kenya: a quasi-experimental study. Glob Heal Sci Pract. 2016;4(1):55–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. DeLorme A, Gavenus ER, Salmen CR, Benard GO, Mattah B, Bukusi E, Fiorella KJ. Nourishing networks: a social-ecological analysis of a network intervention for improving household nutrition in Western Kenya. Soc Sci Med. 2018;197:95–103. [DOI] [PubMed] [Google Scholar]
- 73. Fiorella KJ, Gavenus ER, Milner EM, Moore M, Wilson-Anumudu F, Adhiambo F, Mattah B, Bukusi E, Fernald LCH. Evaluation of a social network intervention on child feeding practices and caregiver knowledge. Matern Child Nutr. 2019;15:e12782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. World Vision International . The Mamanieva Project: Executive Summary. A grandmother-inclusive approach to improve maternal nutrition & infant and young child feeding in Sierra Leone. [Internet]. 2017. [Cited 2020 May 13]. Available from:https://www.wvi.org/sites/default/files/Mamanieva Executive Summary for Dissemination with 4 Logos rev for EB April 2017.pdf. [Google Scholar]
- 75. Save the Children . Nourish Project endline survey report. [Internet]. Phnom Penh (Cambodia); 2019. [Cited 2020 May 13]. Available from: https://resourcecentre.savethechildren.net/library/nourish-project-endline-survey-report. [Google Scholar]
- 76. Sherburne L, Math S, Griffiths M, Sacci I. “Grow Together” campaign in Cambodia: a game-changer for children's healthy growth. [Internet]. 2018. [Cited 2020 Mar 30]. Available from:https://www.advancingnutrition.org/resources/grow-together-campaign-cambodia-game-changer-childrens-healthy-growth. [Google Scholar]
- 77. Harris J, Nguyen H, Maluccio J, Rosenberg A, Mai LT, Quabili W, Rawat R. RAIN project: impact evaluation report. [Internet]. Washington (DC); 2016. [Cited 2020 Mar 30]. Available from:https://www.securenutrition.org/sites/default/files/resources/attachment/english/IFPRI_Rain endline survey report final version_2016 May.pdf. [Google Scholar]
- 78. Kumar N, Nguyen PH, Harris J, Harvey D, Rawat R, Ruel MT. What it takes: evidence from a nutrition- and gender-sensitive agriculture intervention in rural Zambia. J Dev Eff. 2018;10(3):341–72. [Google Scholar]
- 79. Dougherty L, Magalona S, Moreaux M, Dadi C, Fisseha T. The father factor: how community video encourages male involvement for better nutrition and hygiene behaviors in Niger: evidence from the SPRING Community Video Experience. [Internet]. Arlington (VA); 2017. [Cited 2020 Mar 30]. Available from:https://www.spring-nutrition.org/sites/default/files/publications/reports/spring_niger_father_factor.pdf. [Google Scholar]
- 80. Save the Children .NOURISH semi-annual progress report. [Internet]. Phnom Penh (Cambodia); 2016. [Cited 2020 May 13]. Available from: https://pdf.usaid.gov/pdf_docs/pa00mm9k.pdf. [Google Scholar]
- 81. Duthie M, Anzoategu L, Hess A, Higgins J, Smith M. Impact evaluation of USAID Nurture in Laos: midline evaluation report. Arlington (VA): Social Impact; 2019. [Google Scholar]
- 82. Kim SS, Ali D, Kennedy A, Tesfaye R, Tadesse AW, Abrha TH, Rawat R, Menon P. Assessing implementation fidelity of a community-based infant and young child feeding intervention in Ethiopia identifies delivery challenges that limit reach to communities: a mixed-method process evaluation study Global health. BMC Public Health. 2015;15(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Nguyen PH, Kim SS, Keithly SC, Hajeebhoy N, Tran LM, Ruel MT, Rawat R, Menon P. Incorporating elements of social franchising in government health services improves the quality of infant and young child feeding counselling services at commune health centres in Vietnam. Health Policy Plan. 2014;29(8):1008–20. [DOI] [PubMed] [Google Scholar]
- 84. White S, Schmidt W, Sahanggamu D, Fatmaningrum D, van Liere M, Curtis V. Can gossip change nutrition behaviour? Results of a mass media and community-based intervention trial in East Java, Indonesia. Trop Med Int Heal. 2016;21(3):348–64. [DOI] [PubMed] [Google Scholar]
- 85. Morse T, Chidziwisano K, Tilley E, Malolo R, Kumwenda S, Musaya J, Cairncross S. Developing a contextually appropriate integrated hygiene intervention to achieve sustained reductions in diarrheal diseases. Sustainability. 2019;11(17):4656. [Google Scholar]
- 86. Clemmons L. Final report on USAID/ENGINE's enhanced community conversations for the first 1000 days of maternal and child nutrition. [Internet]. Washington (DC); 2016. [Cited 2021 Jan 4]. Available from:https://gtn-learning.org/node/338. [Google Scholar]
- 87. Suresh S, Paxton A, Pun BK, Gyawali MR, Kshetri ID, Rana PP, Cunningham K. Degree of exposure to interventions influences maternal and child dietary practices: evidence from a large-scale multisectoral nutrition program. PLoS One. 2019;14(8):e0221260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Suaahara . Annual report, August 1, 2013-July 31, 2014. [Internet]. Kathmandu (Nepal); 2014. [Cited 2020 May 13]. Available from: https://pdf.usaid.gov/pdf_docs/PA00KC2M.pdf. [Google Scholar]
- 89. Suaahara . Annual report, August 1, 2014-July 31, 2015. Kathmandu (Nepal): Save the Children; 2015. [Google Scholar]
- 90. Nguyen PH, Kim SS, Nguyen TT, Hajeebhoy N, Tran LM, Alayon S, Ruel MT, Rawat R, Frongillo EA, Menon P. Exposure to mass media and interpersonal counseling has additive effects on exclusive breastfeeding and its psychosocial determinants among Vietnamese mothers. Matern Child Nutr. 2016;12(4):713–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Health Communication Capacity Collaborative.Designing a social and behavior change communication strategy. [Internet]. 2018; . [Cited 2020 Dec 30]. Available from: https://sbccimplementationkits.org/lessons/step-4-strategic-approaches/. [Google Scholar]
- 92. World Health Organization . Indicators for assessing infant and young child feeding practices. [Internet]. Geneva (Switzerland): WHO; 2008. [Cited 2020 Jun 30]. Available from: https://apps.who.int/iris/bitstream/handle/10665/43895/9789241596664_eng.pdf?sequence=1. [Google Scholar]
- 93. Mesman J, Minter T, Angnged A, Cissé IAH, Salali GD, Migliano AB. Universality without uniformity: a culturally inclusive approach to sensitive responsiveness in infant caregiving. Child Dev. 2018;89(3):837–50. [DOI] [PubMed] [Google Scholar]
- 94. Pérez-Escamilla R, Segura-Pérez S, Hall Moran V. Dietary guidelines for children under 2 years of age in the context of nurturing care. Matern Child Nutr. 2019;15(3):e12855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Weller SC. Cultural consensus theory: applications and frequently asked questions. Field Methods. 2007;19(4):339–68. [Google Scholar]
- 96. Batchelder WH, Anders R, Oravecz Z. Cultural Consensus Theory. : Wixted JT, WagenmakersE-J,. Stevens’ handbook of experimental psychology and cognitive neuroscience. Nashville (TN: ): John Wiley & Sons; 2018. p.201–64. [Google Scholar]
- 97. Petit V, Zalk TN. Everybody wants to belong: practical guide for social norms programming. [Internet]. Amman (Jordan); 2019. [Cited 2020 May 13]. Available from:https://www.unicef.org/mena/everybody-wants-to-belong. [Google Scholar]
- 98. Institute for Reproductive Health Georgetown University . The Social Norms Exploration Tool. [Internet]. Washington (DC); 2020. [Cited 2020 Dec 20]. Available from:https://irh.org/social-norms-exploration/. [Google Scholar]
- 99. Rogers EM. Diffusion of innovations. 5th ed.New York: Free Press; 2003. [Google Scholar]
- 100. Gottlieb BH, Marshaling social support: the state of the art in research and practice. In: Gottlieb BHed. Marshaling social support: formats, processes, and effects. Beverly Hills (CA): Sage Publications, Inc; 1988. p. 11–51. [Google Scholar]
- 101. Mbuya MNN, Jones AD, Ntozini R, Humphrey JH, Moulton LH, Stoltzfus RJ, Maluccio JA; Team for the SHINE Trial . Theory-driven process evaluation of the SHINE trial using a program impact pathway approach. Clin Infect Dis. 2015;61(Suppl 7):S752–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Dumas SE, Maranga A, Mbullo P, Collins S, Wekesa P, Onono M, Young SL. “Men are in front at eating time, but not when it comes to rearing the chicken”: unpacking the gendered benefits and costs of livestock ownership in Kenya. Food Nutr Bull. 2018;39(1):3–27. [DOI] [PubMed] [Google Scholar]
- 103. Gardsbane D, Kohli A, Lundgren R, Mclarnon-Silk C, Roisman L. A landscape review: addressing social norms in six USAID sectors. [Internet]. Washington (DC); 2019. [Cited 2020 May 21]. Available from: http://irh.org/resource-library/a-landscape-review-addressing-social-norms-in-six-usaid-sectors/. [Google Scholar]
- 104. Oni GA, Brown KH, Bentley ME, Dickin KL, Kayode B, Alade I. Feeding practices and prevalence of hand-feeding of infants and young children in Kwara State, Nigeria. Ecol Food Nutr. 1991;25(3):209–19. [Google Scholar]
- 105. Bentley ME, Wasser HM, Creed-Kanashiro HM. Responsive feeding and child undernutrition in low- and middle-income countries. J Nutr. 2011;141(3):502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Engle PL, Bentley M, Pelto G. The role of care in nutrition programmes: current research and a research agenda. Proc Nutr Soc. 2000;59(1):25–35. [DOI] [PubMed] [Google Scholar]
- 107. Mwaseba DJB, Kaarhus R, Mvena ZSK. Food culture and child-feeding practices in Njombe and Mvomero districts, Tanzania. J East African Stud. 2016;10(2):325–42. [Google Scholar]
- 108. Brewis A, Wutich A. Why we should never do it: stigma as a behaviour change tool in global health. BMJ Glob Heal. 2019;4(5):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Edberg M, Krieger L. Recontextualizing the social norms construct as applied to health promotion. SSM Popul Heal. 2020;10:100560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Sraboni E, Quisumbing A. Women's empowerment in agriculture and dietary quality across the life course: evidence from Bangladesh. Food Policy. 2018;81:21–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Richman AL, Miller PM, LeVine RA. Cultural and educational variations in maternal responsiveness. Dev Psychol. 1992;28(4):614–21. [Google Scholar]
- 112. Doyle K, Kato-Wallace J, Kazimbaya S, Barker G. Transforming gender roles in domestic and caregiving work: preliminary findings from engaging fathers in maternal, newborn, and child health in Rwanda. Gend Dev. 2014;22(3):515–31. [Google Scholar]
- 113. Headey D, Hirvonen K, Hoddinott J. Animal sourced foods and child stunting. Am J Agric Econ. 2018;100(5):1302–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Tadesse K, Zelenko O, Mulugeta A, Gallegos D. Effectiveness of breastfeeding interventions delivered to fathers in low- and middle-income countries: a systematic review. Matern Child Nutr. 2018;14(4):e12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Martin SL, McCann JK, Gascoigne E, Allotey D, Fundira D, Dickin KL. Mixed-methods systematic review of behavioral interventions in low- and middle-income countries to increase family support for maternal, infant, and young child nutrition during the first 1,000 days. Curr Dev Nutr. 2020;4(6):nzz085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.