Abstract
Various techniques of reconstruction of deformed Charcot hindfoot using different internal fixation devices have been described in the literature. We present our surgical technique using specific principles that has resulted in improved outcomes to allow correction of deformity, obtain stability and allow progression to weightbearing in orthotic shoes. We describe our preoperative evaluation, planning and surgical timing. We also hope to share some technical pearls and details on the finer points to achieve a satisfactory correction and reduce the learning curve.
Keywords: Charcot, Hindfoot, Neuropathic deformity, Reconstruction
1. Introduction
Charcot neuroarthropathy (CN) affects the ankle and subtalar joints less frequently than midfoot and forefoot regions.1 Hindfoot or ankle CN often results in significant deformity and instability and without adequate offloading measures, can lead to ulceration and infection, and eventually resulting in trans-tibial amputation.2 A major amputation in a patient with diabetes carries a remarkably high mortality rate and hence functional salvage of the limb by offering a reconstruction is desirable. Even though, the techniques of fixation with devices such as Steinmann pins, staples, screws, plates and angled blade plates have been described in the past, the external fixation and hindfoot nail fixation are now considered as the most successful methods for Charcot hindfoot reconstruction.
The objective of Charcot hindfoot reconstruction is to attain a stable and plantigrade foot that can fit in an appropriate shoe or brace for full weight bearing mobilisation and has healthy skin coverage with no abnormal bone prominence. This requires full deformity correction through osteotomies and wedge resections and optimal stabilisation of bones using internal or external fixation until full tibio-talo-calcaneal (TTC) fusion is achieved. Published literature revealed similar outcomes with internal and external fixations options for such procedures and confirmed the vast majority of patients achieved ambulatory status following reconstruction.3 In comparison to the other forms of internal fixation, an intramedullary (IM) hindfoot nail is considered to provide better stability and offer superior resistance to the multiplanar forces across the ankle joint exerted by the long leaver arm of the foot. An IM nail also acts as a load sharing device and thereby can potentially allow earlier return to weight-bearing. In addition, it allows intra-operative axial compression of the bone fragments of both the ankle and subtalar joints providing optimal bone apposition and enhanced rigidity of the fixation construct, along with optional delayed dynamization, thereby improving the bone fusion rates.4 Charcot hindfoot deformity correction and reconstruction using TTC nail has recently gained popularity as a limb salvage procedure with more predictable and successful outcomes reported in the literature. Authors from our unit have previously reported satisfactory short- and medium-term outcomes following such procedures.5 In this article, we describe the fixation principles, surgical techniques, and perioperative patient care, for this procedure.
2. Patient selection and preparation
Charcot foot reconstruction is normally considered when there is gross instability or deformity causing soft tissue tension where conventional offloading is not suitable. The reconstruction is often performed during Eichenholtz stage 2 or 3 of the disease process, however, in limb threatening situations, can be performed during stage 1.6 The patient care is provided by the multidisciplinary foot team (MDFT), and the initial assessment includes glycaemic control, medical comorbidities, vascular status, infection status, and home microenvironment. These are ideally optimised prior to the reconstruction procedure.
2.1. Soft tissue assessment
The foot and ankle unit is examined for associated soft tissue contractures, including gastrocnemius muscle, Achilles and tibialis posterior tendons. Muscle imbalance is also common due to neuropathy, and weakness of peroneus brevis and tibialis anterior are often encountered. Skin and deep soft tissues on the concave side of the deformity are often contracted and the risk of failure of primary closure of surgical wounds in this area should be considered.
2.2. Bone assessment
Weight bearing radiographs and CT imaging of foot and ankle are critical for surgical planning. The deformity pattern at the ankle and subtalar joints and the degree of bone loss are determined for surgical planning. Hindfoot malalignment in varus, valgus or equinus is of common occurrence and joints are examined for the presence of rigid or flexible deformities. This is in combination with identifying the midfoot and forefoot deformities, however this fall outside the remit of this article.
2.3. Infection assessment
In the presence of an infected ulcer, aggressive surgical debridement and targeted antibiotic administration should be performed to achieve infection eradication before considering the definitive hindfoot reconstruction.4 In the absence of an actively infected ulcer, bone biopsies should still be considered if there was any history previous infection or ulcer in the foot and ankle region. Deep tissue and bone biopsies, as an outpatient procedure, are taken from the previously effected areas for microbiology culture and sensitivity and histological studies so that residual infection can be excluded, and optimal peri-operative antibiotics can be chosen if positive.
3. Pre-operative planning
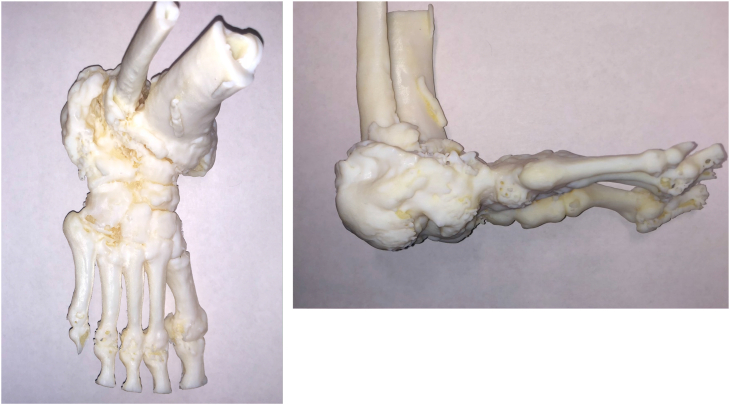
Measurement of calcaneal pitch on the weightbearing lateral radiograph of the ankle is performed to quantify the degree of the deformity, with the aim of restoring this parameter intraoperatively. Digital templating of the weight-bearing radiographs of the ankle with input from and CT 3D reconstruction images is ideally performed for all procedures. We routinely use 3D printed model for surgical planning of complex hindfoot deformities (Fig. 1a Fig. 1b). The location and angulation of distal tibial and subtalar joint wedge resections are planned based on the degree and plane of deformations noted in the ankle and subtalar joints. The vascular status assessment is critical to decide on whether a tourniquet can be used during the procedure.
Fig. 1A and b.
3D printed model used for pre and intraoperative planning.
3.1. Equipment
A hindfoot nail system of surgeon’s preference is chosen. In addition, 6.5–8 mm cannulated screw and 3–4 mm screw locking plate systems are selected. The authors’ preference is to use a straight hindfoot nail with an option to do on-table axial compression before performing locking screw fixation. Oscillating saw, a range of curved osteotomes, 2 mm Kirshner wires and a laminar spreader or similar bone spreader are beneficial. A 5-6 mm Schanz pin inserted in to calcaneum to perform a joystick manouver and an external fixator to apply a temporary distraction, can be considered for achieving deformity correction in some complex deformities.
4. Procedure
4.1. Positioning
The authors preference is positioning the patient supine on a radiolucent table with the foot located at the bottom edge of the table. The procedure is performed under general anaesthetic and we do not routinely recommend nerve blocks for perioperative pain relief as most patients present with severe peripheral neuropathy. Prophylactic antibiotics are withheld until the intraoperative microbiological samples are harvested. A thigh tourniquet and tranexamic acid are used if there are no contra-indications. In severe Charcot deformities and if the pedal pulses are not palpable, we routinely perform on-table doppler examination to identify the course of anterior tibial and posterior tibial arteries, and mark on the skin using indelible ink, so that care is taken during the procedure to avoid any inadvertent damage to these vessels due to their deformity related malposition. Foot scrub is performed prior to standard prepping and draping of the leg to above the knee level. A bolster is placed proximal to the ankle level to elevate the ankle off the table.
4.2. Surgical approach
The reconstruction is usually performed using one major surgical approach, placed on the convex side of the deformity, supplemented with a smaller approach on the opposite side. In chronic Charcot, the soft tissues, including the major arteries are often contracted on the concave side of the deformity. Due to this, it is advisable not to lengthen the bones acutely, with the aim of restoring the leg length, as this may cause significant soft tissue problems, including vascular compromise and wound dehiscence. The skin incisions are deepened to the bone and extended subperiosteally to create full thickness soft tissue flaps. Care is taken to avoid any damage to the vessels in the ankle region. The choice of surgical approaches depends on the deformity pattern of hindfoot Charcot.
In the presence of an ulcer that is not actively infected (absence of clinical signs, negative deep tissue and bone biopsy microbiology culture and sensitivity results), thorough ulcer debridement is performed by by removing all necrotic tissue until the surgeon reaches the underlying healthy tissue. Deep tissue and bone specimens are harvested for microbiology culture and sensitivity tests. The foot is then re-draped, and the instruments used for this part of the procedure are discarded.
A rigid hindfoot varus deformity is corrected using a trans-lateral malleolar approach to access the ankle and subtalar joints (Fig. 2). If the degree of the deformity at the ankle is not severe, only the anterior half of the lateral malleolus can be osteotomised to provide adequate access to the ankle joint, being placed back afterwards and fixed with small fragment screws. This retains the peroneal grove of the intact lateral malleolus. The peroneal tendons are protected throughout. An oblique lateral malleolar osteotomy is done above the level of syndesmosis for larger deformities and the lateral malleolus is removed after freeing it from its soft tissue attachments subperiosteally, and can be subsequently used for bone graft is necessary. The ankle joint is approached laterally by reflecting anteriorly and posteriorly in the subperiosteal plane using Hohmann’s retractors. The subtalar joint is also accessed directly. This approach is often combined with a small dorsomedial approach over the medial ankle gutter used for the preparation of the medial gutter and to perform any soft tissue releases on the medial side of the ankle (Fig. 3). Care is taken to protect saphenous vein and its major tributaries.
Fig. 2.
Trans-lateral malleolar approach to access the ankle and subtalar joints, emphasising full thickness soft tissue flaps.
Fig. 3.
Limited dorsomedial approach over the medial ankle gutter used for the preparation of the medial gutter and to perform any soft tissue releases on the medial side of the ankle.
A rigid hindfoot valgus deformity with contracted skin and soft tissues on the lateral aspect of the ankle warrants a dorsomedial approach to the ankle joint. This is supplemented with a smaller lateral approach over the subtalar joint for its access and preparation.
4.3. Soft tissue releases
The contracted soft tissue releases are performed at the beginning, as this will allow plan the bone cuts and wedge resections more accurately. Most chronic CN deformities develop Achilles tendon contracture, but some develop more profound tightness of gastrocnemius only. In the presence of isolated gastrocnemius contracture, the fascia of the gastrocnemius is released from the medial side using a longitudinal incision placed at the musculotendinous junction in the midcalf region. The Achilles tendon contracture, if present or still preventing adequate correction particularly after bone resection, is released using percutaneous Hoke’s triple hemisection technique.7 Contraction of tibialis posterior tendon is often noted in hindfoot varus deformities. The tendon release (complete tenotomy) using a medial approach results in marked improvement in the deformity in most cases, however, due to scaring, some require a more extensile release of the tendon proximally.
4.4. Osteotomy and bone preparation
Ankle and subtalar components of the Charcot deformity is corrected by performing wedge or rhomboid bone resections on the convex side of the deformity as per the surgical plan and under the guidance of fluoroscopy. The ankle part is corrected first by performing the distal tibial resection at the tibial plafond level, using an oscillating saw, perpendicular to the long axis of tibial shaft in the frontal plane; some degree of posteroinferior slope in the sagittal plane is acceptable and is often needed to prevent excessive shortening of the leg. Care is taken not to extend the osteotomy into the medial malleolus and the saw cut is stopped at the level of the medial gutter. A vertical box cut at the medial gutter is carefully done (through the limited dorsomedial approach if needed) as it allows preservation of the medial malleolus, in addition to preparing the medial gutter by removing the articular cartilage. The talar articular surface in the ankle and medial gutter is cut, and bone wedges are included to correct the deformity and achieve optimal bone opposition (Fig. 4). Intact medial malleolus allows optimal positioning of the talus in the medial gutter corner, providing additional stability. Repeat assessments and bone cut refinements are done to make sure that optimal neutral alignment at the ankle joint in varus-valgus and dorso-plantar planes is achieved and temporarily stabilised using 2 mm Kirshner wires. Subtalar joint is released thoroughly, and joint preparation of the posterior and medial facets and wedge osteotomy cut to the posterior facet are made as per the surgical plan and the residual alignment of the heel following the ankle correction. Care is taken to restore the calcaneal pitch and normal rotational alignment of the calcaneus.
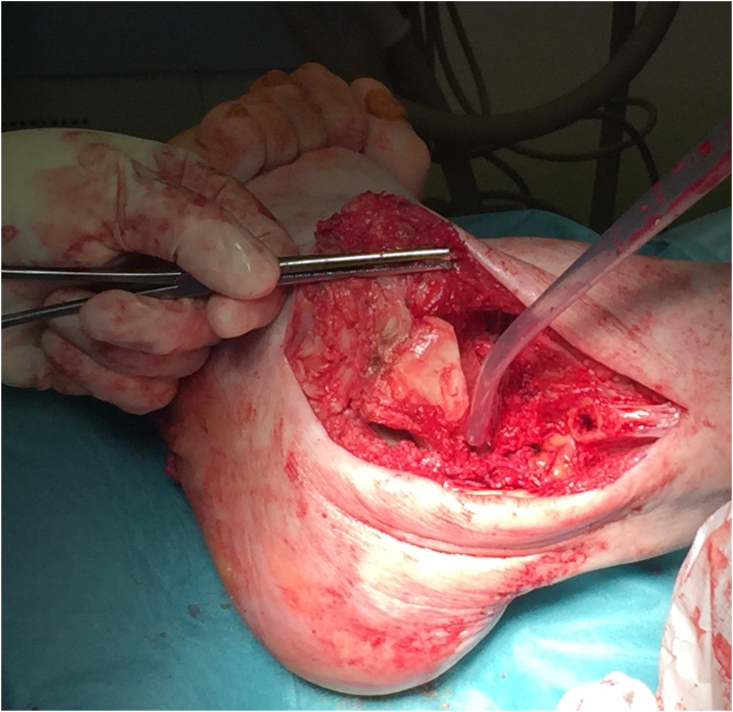
Fig. 4.
The talar articular surface in the ankle and medial gutter is cut, and bone wedges are included to correct the deformity and achieve optimal bone opposition.
4.5. Fixation
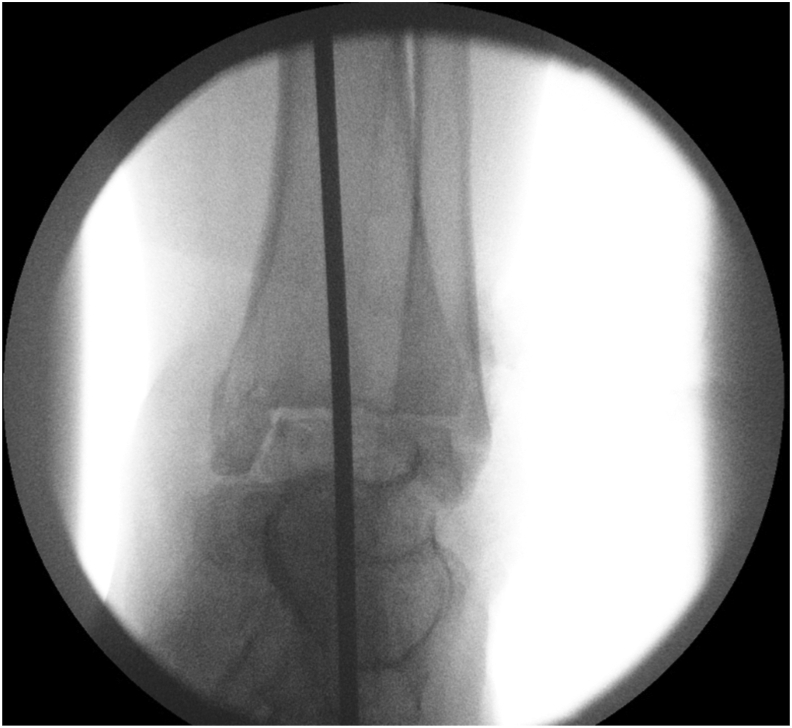
The principle of fixation in Charcot hindfoot reconstruction using internal fixation is-durable long segment rigid fixation with optimal bone opposition.8 After deformity correction, the ankle and subtalar joints are held in optimal position by inserting 2 mm Kirshner wires. The entry point of the hindfoot nail guide wire is determined by placing a long guide wire over the leg and foot along the axis of tibia in the coronal and sagittal planes and screening under fluoroscopy in the anteroposterior and lateral views respectively. The intersection of lines drawn over the skin on the plantar aspect of the heel along the alignment of the rod kept in optimal position on both planes determines the entry point of the nail. A 2-inch longitudinal skin incision is made at the level of the entry point, extended down to bone. The hindfoot nail guide wire is passed on to the inferior cortex of the calcaneus, the entry point is reassessed by feeling the width of the inferior bone and the wire is driven in the middle part of the bone. Once the guide wire is through the middle part of the talus and tibial plafond into the medullary cavity of tibia, sequential reaming is done using the standard surgical technique for the hindfoot nail system used.
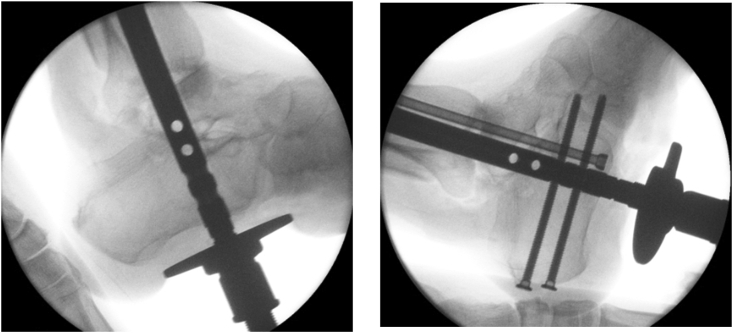
The nail length and diameter are determined based on the size of the medullary cavity. It is crucial that a good isthmal fit of the nail to the cortical bone of the diaphysis is achieved and adequate nail length and diameter are critical to attain this. After inserting the nail to the correct depth, axial compression of the bone fragments over the nail is achieved before complete proximal and distal locking screws are used. Different hindfoot nail systems have different bone compression methods. One hindfoot nail system, the authors often use, allows controlled axial compression of the talar and calcaneal fragments against distal tibia. This requires proximal locking of the nail first, which the authors prefer to achieve by using one dynamic and one static screw. Depending on the amount of gap noted between distal tibia, talus and calcaneal fragments, the depth of the nail insertion is adjusted prior to inserting proximal locking screws, keeping in mind its final position distally and the location of calcaneal locking screw slots following axial compression. Following insertion of proximal locking screws, the calcaneal fragment is compressed proximally by using a compressive device until optional bone opposition is reached, as noted from direct vision of the bone fragments, and under fluoroscopy. Distal locking screws into calcaneus and talar fragments are inserted to lock the nail in compression (Fig. 5a and b). The compression device is then removed and the rigidity of the fixation contract in all planes is assessed by manipulation.
Fig. 5A and b.
Distal locking screws into calcaneus and talar fragments are inserted to lock the nail in compression.
In the presence of significant bone loss, optimal rotational rigidity is not possible with a standard hindfoot nail construct. In such situations, we recommend using a separate cannulated partially threaded screw inserted from calcaneum into distal tibia (Fig. 6a and b). The authors use a hindfoot nail system that allows inserting a ‘miss-a-nail’ screw using an optional additional jig that can be attached to the existing hindfoot jig that allows rapid insertion of a cannulated screw that misses the existing nail path. Another option of achieving additional rotational rigidity is to use a locking plate across distal tibia and talar body anteromedially (Fig. 7a and b). About 50% of Charcot hindfoot reconstructions require associated midfoot corrections.9 For such procedures, the midfoot medial column reconstruction is performed using dorsomedial approach following hindfoot reconstruction. The medial column plate or beam fixation also provides the desired rotational rigidity to the hindfoot nail construct.
Fig. 6A and b.
A standard hindfoot nail construct with a separate cannulated partially threaded screw inserted from calcaneum into distal tibia to add rotational stability and added compression.
Fig. 7A and b.
For severe deformity another option of achieving additional rotational rigidity is to use a locking plate across distal tibia and talar body anteromedially.
4.6. Closure
Thorough checks are made for any residual bone prominences in the reconstructed area. The tourniquet is released, if used, and haemostasis is achieved. Regular wound washout using normal saline is performed throughout the procedure. In the absence of any history of previous infection in the ankle and hindfoot region, particulate cancellous autograft, harvested from healthy appearing resected bone, can be used to fill any residual bone voids. If there was a previous history of infection, local antibiotic eluting calcium sulphate preparation can be packed in the bone void areas; the choice of the antibiotic is based on the previous microbiology culture and sensitivity results. Closure of critical deep tissue layers, such as tendon sheath, is performed using an absorbable suture and this is followed by interrupted skin closure using a non-absorbable suture material. Negative pressure wound therapy dressing is applied to any open wounds or ulcers that cannot be primarily closed. A suction drain is used by the authors only if there are concerns with significant wound oozing. The foot and leg are wrapped in padded wool and a below knee backslab is applied.
5. Post-operative management
Post-operative management is provided by the MDFT and optimal perioperative medical management, including glycaemic control is overseen by the physicians. If there was a previous history of infection or ulcer debridement was performed during reconstruction, intravenous antibiotics are commenced post-operatively, based on previous microbiology culture sensitivities, and continued until the results of microbiological analysis of the intra-operative bone specimens become available. In the absence of previous infection, the post-operative antibiotics are continued only if the intra-operative microbiology specimens grow pathogens. The operated foot is elevated above heart level and the patient is mobilised non-weight bearing on crutches or a frame. The wound check is performed by the MDFT on the second or third day and a total contact cast (TCC) is applied once the foot swelling reduces considerably. The patient is discharged home when it is safe and regular change of TCC is carried out until the foot volume changes are stabilised. Post-operative ankle radiographs are taken at 6 and 12 weeks and thereafter at regular intervals as required. Non weight-bearing in the TCC is continued for three months post-operatively, when most patients usually progress to partial weight-bearing in the TCC as satisfactory progression of bone healing, ie satisfactory consolidation of 3 or more cortices or bridging across the fusion site, is noted on radiographs. Most patients can progress to full weight bearing in custom made lace-up shoes between 4 and 6 months.
6. Tips, tricks and pitfalls
In the presence of significant osteoporosis, distal locking screw bone purchase can be improved by using a hydroxyapatite coated distal locking screws. This has been shown to reduce screw migration or breakage.5
If the bone healing response is not noted at 3-month post-operative radiograph, dynamization of the nail is recommended to promote bone union.
Wound closure difficulties are often encountered in complex Charcot reconstruction procedures. This is often prevented by achieving adequate shortening through wedge resection of bones. If primary wound closure without tension is not possible, some soft tissue tension at the wound can be relieved by resecting any bone prominences at the wound. If primary wound closure is desired in the presence of some wound tension, meshing of skin through multiple parallel skin-deep cuts, so called ‘pie crusting’, helps reduce skin tension and achieve optimal skin opposition.
Talectomy becomes necessary in some situations and this requires direct calcaneo-tibial fusion. Care is taken to perform the distal tibial bone cut to match the calcaneal cut in optimal calcaneal pitch position to prevent excessive shortening, while maintaining optimal bone opposition. Calcaneo-tibial hindfoot nail fixation construct often has poor rigidity against rotational forces and requires one to two miss-a-nail screws to enhance this. Calcaneo-tibial fixation also results in marked prominence, with distalisation of medial malleolus and it is desirable remove part of the prominent bone to reduce this shape abnormality causing a shoe rub.
Even though, the metal work failure following Charcot hindfoot reconstruction using a hindfoot nail is a common occurrence, most likely due to fatigue failure of the hardware due to delayed or non-union, the functional outcomes are still good in this cohort.9 Dedicated hindfoot nails designed to suit the bone morphology commonly noted in Charcot ankle and improvements in the biomaterials can potentially reduce this complication.
7. Discussion
A straight hindfoot nail is preferred over anatomical bent nail, for Charcot hindfoot reconstruction, as it provides the option of achieving controlled axial compression of bone fragments intraoperatively. Straight nails also resist the axial compression forces better than the bent nails and help distribute these forces evenly over the fusion surfaces. However, a straight nail insertion is surgically more demanding as it is critical this requires accurate plantar nail entry. The length of the nail is still debatable, with a lot of the main hindfoot nails ending around 210 mm with no option of spanning the entire tibia. Our preference is for a good isthmal fit but not spanning the entire tibia.
Following the steps and avoiding the pitfalls outlined above should equip the reader with the necessary principles to negotiate what is a difficult condition to maximise the chances of success.
Acknowledgements
The authors like to acknowledge Michael Edmonds, Maureen Bates, Raju Ahluwalia, Ines Reichert, Prashanth Vas and Christopher Manu for their contribution to the development of peri-operative care in Charcot hindfoot reconstructions.
Contributor Information
Venu Kavarthapu, Email: venu.kavarthapu@nhs.net.
Thomas Hester, Email: thomashester@gmail.com.
References
- 1.Brodsky J., Wagner F.W.W., Kwong P. Patterns of breakdown in the Charcot tarsus of diabetes and relation to treatment. Foot Ankle. 1986;6(5):353. [Google Scholar]
- 2.Sohn M.W., Stuck R.M., Pinzur M., Lee T.A., Budiman-Mak E. Lower-extremity amputation risk after charcot arthropathy and diabetic foot ulcer. Diabetes Care. 2010;33(1):98–100. doi: 10.2337/dc09-1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ha J., Hester T., Foley R. Charcot foot reconstruction outcomes: a systematic review. J Clin Orthop Trauma. 2020 May-Jun;11(3):357–368. doi: 10.1016/j.jcot.2020.03.025. Epub 2020 Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kavarthapu V. Surgical management: internal stabilisation. In: Edmonds M., Sumpio B., editors. Limb Salvage of the Diabetic Foot- an Interdisciplinary Approach. Springer; 2019. pp. 173–184. [Google Scholar]
- 5.Siebachmeyer M., Boddu K., Bilal A. Outcome of one-stage correction of deformities of the ankle and hindfoot and fusion in Charcot neuroarthropathy using a retrograde intramedullary hindfoot arthrodesis nail. Bone Jt J. 2015 Jan;97-B(1):76–82. doi: 10.1302/0301-620X.97B1.34542. [DOI] [PubMed] [Google Scholar]
- 6.Eichenholtz S. In: Charcot Joints. Thomas C., editor. Springfield; IL, USA: 1966. [Google Scholar]
- 7.Hatt R.N., Lamphier T.A. Triple hemisection: a simplified procedure for lengthening the Achilles tendon. N Engl J Med. 1947 Jan 30;236(5):166–169. doi: 10.1056/NEJM194701302360502. [DOI] [PubMed] [Google Scholar]
- 8.Butt D.A., Hester T., Bilal A., Edmonds M., Kavarthapu V. The medial column Synthes Midfoot Fusion Bolt is associated with unacceptable rates of failure in corrective fusion for Charcot deformity: results from a consecutive case series. Bone Jt J. 2015 Jun;97-B(6):809–813. doi: 10.1302/0301-620X.97B6.34844. [DOI] [PubMed] [Google Scholar]
- 9.Kummen I., Phyo N., Kavarthapu V. Charcot foot reconstruction—how do hardware failure and non-union affect the clinical outcomes? Ann Jt. 2020;5 25–25. [Google Scholar]