Abstract
Purpose
To report a case of external ophthalmoplegia due to an uncommon form of amyloidosis exclusively affecting the lateral rectus muscle, and to discuss the clinical manifestation, diagnostic challenges, and management pitfalls of isolated amyloidosis in the extraocular muscle.
Observations
A 64-year-old woman presented with diplopia in her left gaze lasting for six months. She had orthophoria in the primary position and abduction limitation in the left eye. Routine laboratory examinations were unremarkable. Orbital magnetic resonance imaging showed fusiform enlargement of the left lateral rectus muscle, without tendon involvement. Extraocular muscle biopsy was recommended to make a diagnosis, which revealed amyloid deposition in the lateral rectus muscle. A systemic work-up showed no evidence of systemic amyloidosis. Therefore, a diagnosis of primary isolated amyloidosis was made. Orthophoria in the primary position and diplopia in the lateral gaze persisted at the six-month follow-up.
Conclusions and importance
Atypical extraocular muscle enlargement should alert clinicians to the need for tissue biopsy to identify uncommon etiologies, such as amyloidosis. There are no pathognomonic or radiological features to distinguish localized from systemic amyloidosis. Therefore, if amyloidosis of the extraocular muscles is diagnosed, a systemic work-up is needed to rule out systemic amyloidosis, which is potentially life-threatening.
Keywords: External ophthalmoplegia, Diplopia, Extraocular muscle enlargement, Extraocular muscle biopsy, Orbital amyloidosis
1. Introduction
Amyloidosis is a condition that occurs when an abnormal amyloid protein builds up in the organs and tissues and interferes with their normal functions. This condition is classified into systemic or localized types, both of which are typically progressive and sometimes life-threatening. Except for hereditary corneal dystrophies, the occurrence of amyloid deposits in the eyes and their adnexal structures is rare, although it is known to develop in systemic or localized amyloidosis.1 Orbital amyloidosis was reportedly seen in 0.3% of cases of orbital diseases,2 with the deposition being observed in the periorbital fat, extraocular muscles, and lacrimal glands.3 However, primary localized amyloidosis in the extraocular muscle without systemic involvement is extremely rare, and only a few cases have been reported. Herein, we report a case of external ophthalmoplegia caused by isolated amyloidosis in the external ocular muscle and discuss the diagnostic challenges and management pitfalls.
2. Case report
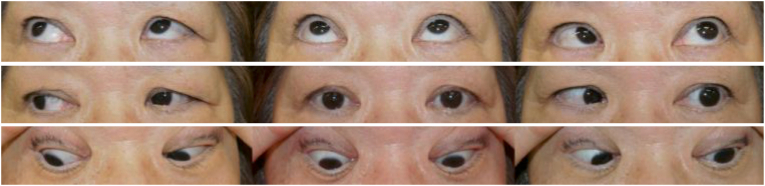
A 64-year-old woman presented to Asahikawa Medical University Hospital with a complaint of diplopia lasting for the past six months. She noticed the diplopia only in the left gaze. The external ocular examination was unremarkable, without any signs of eyelid swelling, proptosis, or ptosis. She was otherwise healthy, except for hyperlipidemia, which had been adequately treated with lipid-lowering medication. Her best-corrected visual acuity was 20/16 in both eyes, and orthophoria was present in the primary position. Ocular motility tests revealed abduction limitation in the left eye (Fig. 1). The pupils were equal, round, and reactive to light, and no evidence of internal ophthalmoplegia was detected. The anterior segment and fundus examinations were unremarkable.
Fig. 1.
Nine diagnostic gaze position photographs of the patient showing limitation of the left lateral gaze. There is no eyelid swelling, proptosis, or ptosis.
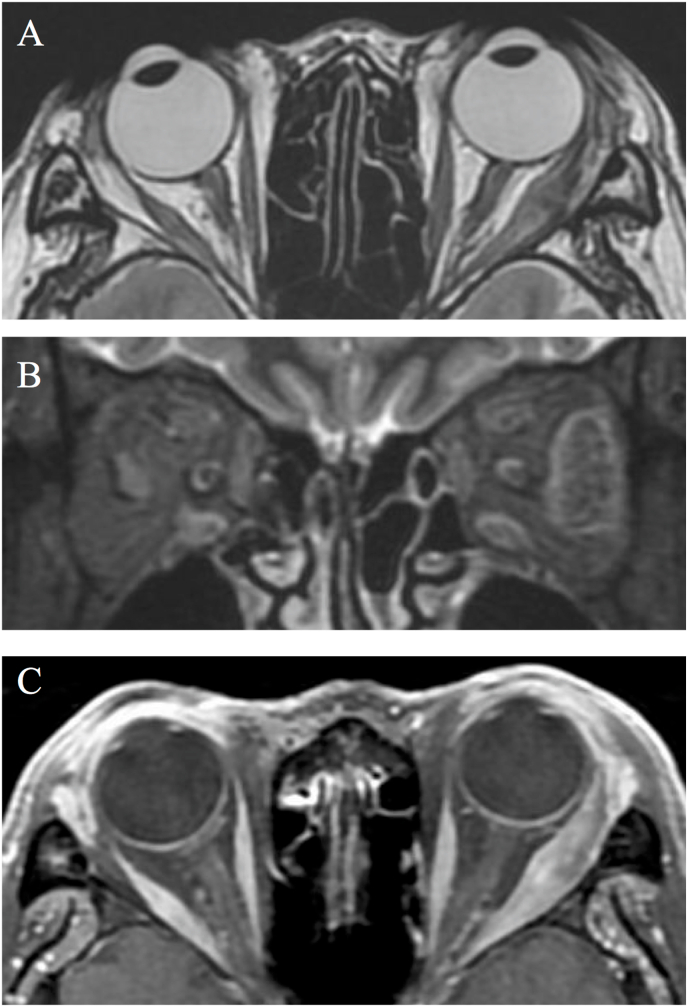
Magnetic resonance imaging (MRI) showed fusiform enlargement of the left lateral rectus muscle with tendon sparing. The enlarged lateral rectus did not show high signal intensity on short-tau inversion-recovery (STIR) MRI or on gadolinium enhancement (Fig. 2). Laboratory work-up revealed that her thyroid-stimulating hormone (TSH) level was slightly elevated (5.79 μIU/ml), but free triiodothyronine, free thyroxine, and TSH receptor antibody levels were normal. Serum C-reactive protein, IgG4, soluble interleukin-2 receptor, angiotensin-converting enzyme, and lysozyme levels were also within the normal ranges.
Fig. 2.
A: T2-weighted MRI showing thickening of the left rectus muscle with tendon sparing. B: Short-tau inversion-recovery (STIR) sequence of the orbital coronal image. There is no enhancement effect in the enlarged left lateral rectus. C: No gadolinium enhancement is seen.
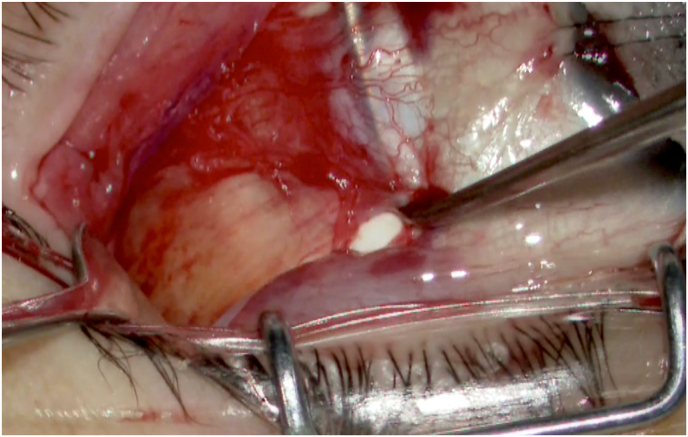
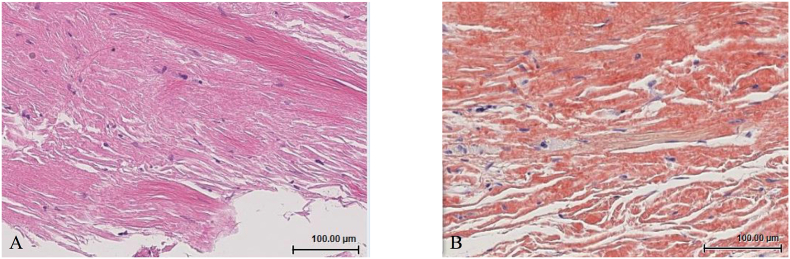
To establish a diagnosis, a left lateral rectus muscle biopsy was performed. During surgery, the left lateral rectus was weak on active force generation testing, and the forced duction test (FDT) was negative. A left lateral limbal-conjunctival incision was made, and the lateral rectus muscle was held with a squint hook. The upper edge of the muscle was then resected to a width of 1–1.5 mm and a length of 10 mm. The muscle and the tendon appeared yellowish and could be torn easily using forceps (Fig. 3). Histopathology revealed atrophy and focal loss of muscle fibers; in addition, deposition of eosinophilic amorphous material was widely observed on hematoxylin and eosin staining (Fig. 4A). The eosinophilic material was positive for direct fast scarlet staining (Fig. 4B) with the amyloid-specific birefringence on polarized microscopy. A systemic work-up was conducted, including serum and urine tests, electrocardiogram, echocardiography, immuno‐electrophoresis, and biopsy of subcutaneous fat from the abdomen, which revealed no evidence of systemic amyloidosis other than a slight increase in the kappa light chain (20.6 mg/L) in the serum. Therefore, a diagnosis of primary isolated amyloidosis was made.
Fig. 3.
Surgeon's view of the left lateral rectus muscle, which appears yellowish and fragile.
Fig. 4.
Histopathological study of the left lateral rectus muscle.
A: Muscle fibers were atrophied and disappearing; eosinophilic amorphous material is widely observed on hematoxylin and eosin staining.
B: The eosinophilic materials is positive for direct fast scarlet stain.
The patient was followed up for six months after the biopsy. Her alignment remained excellent in the primary position and her diplopia in the left gaze persisted, but was not bothersome.
3. Discussion
Primary localized amyloidosis in the extraocular muscle is very rare; only 13 such cases without systemic involvement have been reported over the last four decades.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 In only nine of these was the amyloidosis confined to the extraocular muscles (Table 1),4,5,7,8,10,13, 14, 15, 16 whereas the other four cases also exhibited involvement of the soft tissue mass surrounding the enlarged muscles.6,9,11,12 The nine patients mentioned above ranged from 20 to 80 years old, the enlarged muscles ranged from single to multiple without predilection, and the affected side was unilateral or bilateral. Seven of the nine patients were women; this predominance of affected females is consistent with that of previous reviews of orbital amyloidosis (62.5–65.1%).3,17
Table 1.
Primary isolated amyloidosis in extraocular muscles.
| Authors | Patient characteristics | Symptoms | Affected muscles | Imaging (CT or MRI) |
|---|---|---|---|---|
| Holmström GE et al.4 | 60/F | Diplopia | Right medial rectus | Fusiform |
| Erie JC et al.5 | 29/F | Proptosis, diplopia | Right medial and lateral rectus | Fusiform, insertions involved |
| Okamoto K et al.7 | 47/M | Diplopia, exophthalmos | Left medial and inferior rectus | Fusiform, sharp border, punctate calcification, tendon- sparing |
| Banerjee S et al.8 | 45/F | Eye strain | Right lateral rectus | Not available in detail |
| Hamidi Asl K et al.10 | 27/F | Diplopia, proptosis | Both medial and lateral | Not available in detail |
| Jeon CY et al.13 | 37/F | Exophthalmos | Left medial rectus | Fusiform enlargement |
| Monteiro ML et al.14 | 48/M | Lower eyelid swelling, proptosis, vertical diplopia | Left inferior rectus | Tendon-sparing Calcification |
| Li Y et al.15 | 24/F | Mild periorbital pain, diplopia, bilateral restricted eye movement | Both medial rectus | Fusiform, tendon-sparing |
| Dodd MU et al.16 |
85/F |
Progressive strabismus |
Both rectus muscles except the right lateral rectus |
Enlarged midportion of the muscle Tendon-sparing |
| Present case | 64/F | Diplopia | Left lateral rectus | Fusiform, well-circumscribed Tendon-sparing |
Extraocular muscle involvement in orbital amyloidosis may present with various symptoms such as proptosis, eyelid swelling, restriction of eye movement, or diplopia. Among all the cases, the most common symptom was diplopia. In our case, the diplopia was noticed only in the left gaze. The FDT was negative, and force generation was weak in the left lateral rectus muscle, indicating that the limitation of left abduction was neurogenic rather than mechanical. However, in previous reports, FDT was positive in the direction of the enlarged muscles4,5,16 and/or in the opposite direction.15 The positive FDT may have been due to mass effect or restriction of antagonist muscle extension. The difference between this case and the previous cases is the degree of swelling and the duration of symptoms. The additional symptoms in the previously reported cases were proptosis and eyelid edema. Only one patient reportedly complained of mild eye pain.15 In most of the cases, disease progression was slow.
Careful interpretation of clinical findings is crucial for correct diagnosis; several cases were initially treated as thyroid eye disease (TED)14,15 since these characteristics of muscle hypertrophy resemble those of TED. Upon computed tomography (CT) or MRI, an enlarged extraocular muscle often appears fusiform, and sharply edged, with tendon sparing. This was true in our case as well, as the shape of the muscle on the MRI image was similar to that in TED. However, the direction of restricted eye movement was the opposite of that in TED. Moreover, the involved muscle was the lateral rectus, which is the least likely to be affected in TED. Other possible etiologies for unilateral or bilateral extraocular muscle enlargement include inflammation (orbital inflammatory pseudotumor, IgG4 disease), lymphoma, metastatic disease, and sarcoidosis.18 In this case, blood test results and the lack of high signal intensity on STIR MRI or contrast examination were not suggestive of the above-mentioned inflammatory or neoplastic diseases. Orbital imaging may show distinctive radiographic signs of orbital infiltration or extraocular muscle involvement in orbital diseases; however, imaging alone is not diagnostic. Therefore, enlarged extraocular muscles without typical diagnostic clues require biopsy in a timely manner.
Patients should be screened for systemic amyloidosis, if amyloid deposition is confirmed. Shah et al.1 reported on a review of 14 cases of isolated amyloid deposition in the extraocular muscle, in addition to a case of systemic amyloidosis in a 67-year-old woman. Including their case, eight of 15 (53.3%) patients were found to have systemic amyloidosis. Moreover, six of the seven patients with bilateral diffuse amyloid deposition were found to have systemic amyloidosis.1 However, diffuse bilateral amyloid deposition may not be indicative of systemic amyloidosis, as several bilateral cases without systemic involvement have been reported.10,15,16
The diversity of tissues in which amyloid deposits can form remains an open question. Campos et al.19 reported that the extraocular muscles are the most frequently affected ocular tissues in autopsied individuals with generalized amyloidosis. It has been suggested that certain characteristics of the extraocular muscles, such as their high protein concentration, high metabolic activity, and collagen-based tendinous insertions, favor the formation of amyloid fibrils.1,20
4. Conclusions
In summary, we report a rare case of isolated primary amyloidosis in the extraocular muscle causing external ophthalmoplegia. The lateral rectus muscle was fusiform-enlarged, mimicking TED, although with a different direction of restriction. Amyloid deposition should also be considered as a possible cause of atypical extraocular muscle enlargement, and tissue biopsy should be performed for diagnostic confirmation. There are no pathognomonic or radiological features to distinguish localized from systemic amyloidosis. Therefore, if amyloidosis of the extraocular muscles is diagnosed, a systemic work-up is needed to rule out systemic amyloidosis, which can be life-threatening.
Patient consent
Oral consent to publish the case report was obtained. This case report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support was received for this report.
Authorship
All authors attest that they meet the current ICMJE Criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: NN, YK, AK, YK, HT, and YY.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
References
- 1.Shah V.S., Cavuoto K.M., Capo H., Grace S.F., Dubovy S.R., Schatz N.J. Systemic amyloidosis and Extraocular muscle deposition. J Neuro Ophthalmol. 2016;36(2):167–173. doi: 10.1097/WNO.0000000000000358. [DOI] [PubMed] [Google Scholar]
- 2.Kim U.R., Khazaei H., Stewart W.B., Shah A.D. Spectrum of orbital disease in South India: an Aravind study of 6328 consecutive patients. Ophthalmic Plast Reconstr Surg. 2010;26(5):315–322. doi: 10.1097/IOP.0b013e3181c32f2f. [DOI] [PubMed] [Google Scholar]
- 3.Mora-Horna E.R., Rojas-Padilla R., López V.G., Guzmán M.J., Ceriotto A., Salcedo G. Ocular adnexal and orbital amyloidosis: a case series and literature review. Int Ophthalmol. 2016;36(2):281–298. doi: 10.1007/s10792-015-0138-7. [DOI] [PubMed] [Google Scholar]
- 4.Holmström G.E., Nyman K.G. Primary orbital amyloidosis localised to an extraocular muscle. Br J Ophthalmol. 1987;71(1):32–33. doi: 10.1136/bjo.71.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erie J.C., Garrity J.A., Norman M.E. Orbital amyloidosis involving the extraocular muscles. Arch Ophthalmol. 1989;107(10):1428–1429. doi: 10.1001/archopht.1989.01070020502019. [DOI] [PubMed] [Google Scholar]
- 6.Pasternak S., White V.A., Gascoyne R.D., Perry S.R., Johnson R.L., Rootman J. Monoclonal origin of localised orbital amyloidosis detected by molecular analysis. Br J Ophthalmol. 1996;80(11):1013–1017. doi: 10.1136/bjo.80.11.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okamoto K., Ito J., Emura I. Focal orbital amyloidosis presenting as rectus muscle enlargement: CT and MR findings. AJNR Am J Neuroradiol. 1998;19(9):1799–1801. [PMC free article] [PubMed] [Google Scholar]
- 8.Banerjee S., Bogman J., Reuser T.T. Amyloid deposition in the extraocular muscles. Orbit. 1999;18(2):105–106. doi: 10.1076/orbi.18.2.105.2715. [DOI] [PubMed] [Google Scholar]
- 9.Lacey B., Chang W., Rootman J. Nonthyroid causes of extraocular muscle disease. Surv Ophthalmol. 1999;44(3):187–213. doi: 10.1016/s0039-6257(99)00101-0. [DOI] [PubMed] [Google Scholar]
- 10.Hamidi Asl K., Liepnieks J.J., Nunery W.R., Yazaki M., Benson M.D. Kappa III immunoglobulin light chain origin of localized orbital amyloidosis. Amyloid. 2004;11(3):179–183. doi: 10.1080/1350-6120400000707. [DOI] [PubMed] [Google Scholar]
- 11.Teoh S.C., Liew G.C., Yap W.M. Incidental hypoglobus: primary amyloidosis of the superior rectus. Singap Med J. 2006;47(1):65–67. [PubMed] [Google Scholar]
- 12.Khaira M., Mutamba A., Meligonis G., Rose G.E., Plowman P.N., O'Donnell H. The use of radiotherapy for the treatment of localized orbital amyloidosis. Orbit. 2008;27(6):432–437. doi: 10.1080/01676830802350216. [DOI] [PubMed] [Google Scholar]
- 13.Jeon C.Y., Jin S.Y., Jang J.W., Kim U.S. A case of isolated primary amyloidosis in the medial rectus muscle. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):395–396. doi: 10.1007/s00417-011-1867-6. [DOI] [PubMed] [Google Scholar]
- 14.Monteiro M.L., Gonçalves A.C., Bezerra A.M. Isolated primary amyloidosis of the inferior rectus muscle mimicking Graves' orbitopathy. Einstein. 2016;14(4):553–556. doi: 10.1590/S1679-45082016RC3744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y., Wang Y., Zhang W. A case of isolated amyloidosis in extraocular muscle mimicking thyroid eye disease. J AAPOS. J AAPOS. 2020;24(2):122–124. doi: 10.1016/j.jaapos.2019.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Dodd M.U., Wolkow N., Cunnane M.E., Ma L., Dryja T.P., Hunter D. Isolated orbital amyloidosis causing internal and external ophthalmoplegia. J AAPOS. 2020;24(1):48–51.e1. doi: 10.1016/j.jaapos.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Leibovitch I., Selva D., Goldberg R.A. Periocular and orbital amyloidosis: clinical characteristics, management, and outcome. Ophthalmology. 2006;113(9):1657–1664. doi: 10.1016/j.ophtha.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 18.Eade E.L., Hardy T.G., McKelvie P.A., McNab A.A. Review of extraocular muscle biopsies and utility of biopsy in extraocular muscle enlargement. Br J Ophthalmol. 2018;102(11):1586–1590. doi: 10.1136/bjophthalmol-2017-311147. [DOI] [PubMed] [Google Scholar]
- 19.Campos E.C., Melato M., Manconi R., Antonutto G. Pathology of ocular tissues in amyloidosis. Ophthalmologica. 1980;181(1):31–40. doi: 10.1159/000309022. [DOI] [PubMed] [Google Scholar]
- 20.Merlini G., Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349(6):583–596. doi: 10.1056/NEJMra023144. [DOI] [PubMed] [Google Scholar]