Abstract
Objective:
Determine the latent structure of health literacy in persons living with HIV (PLWH) and its association with health management and decision-making.
Method:
Participants included 220 PLWH and 123 seronegative participants from Southern California and Alabama who completed a battery of well-validated health literacy measures, along with assessments of health management self-efficacy, health-related decision-making, depression, and basic clinical laboratory measures.
Results:
Exploratory factor analysis in HIV− participants showed that the shared variance between a battery of health literacy measures, including health word reading, verbal comprehension, numeracy, and self-reported problems was best explained by a single factor. Similarly, a confirmatory factor analysis in PLWH also supported a single factor structure, but for a re-specified four-test solution based on the core performance-based measures of health literacy. In analyses adjusting for demographics, PLWH demonstrated significantly lower health literacy composite scores as compared to their HIV− counterparts. Among PLWH, lower health literacy was independently associated with lower self-efficacy for health management and poorer health-related decision-making.
Conclusions:
Findings suggest that numeracy, word recognition, and verbal comprehension and reasoning comprise a unitary construct of health literacy that is lower in PLWH as compared to seronegatives and is independently associated with important downstream aspects of health management and decision-making.
Keywords: Health literacy, HIV, health management, decision-making
Objective
Health literacy is a multifaceted, dynamic construct broadly defined as the degree to which individuals can obtain, process, understand, and communicate about health-related information to make informed medical decisions (Berkman et al., 2010). One-third to one-half of the United States population has either marginal or low health literacy (Paasche-Orlow et al., 2005). Limited health literacy is associated with poorer health outcomes (see Berkman et al., 2011 for review), including reduced utilization of preventative medication (Cho et al., 2008), more emergency room visits (Baker et al., 2004) and hospitalizations (Baker et al., 2002), and non-adherence (Kripilani et al., 2010). Individuals with low health literacy also demonstrate lower healthcare management skills and less knowledge about chronic medical conditions (Gazmararian et al., 2003; Schillinger et al., 2002).
Health literacy may play a particularly important role in health outcomes for underserved populations with chronic medical diseases, such as human immunodeficiency virus (HIV) disease. HIV disproportionately affects populations at high risk for low health literacy including racial/ethnic minorities and individuals of low socio-economic status (Centers for Disease Control and Prevention, 2008). Among people living with HIV (PLWH), suboptimal health literacy is consistently associated with lower disease prevention and treatment knowledge, higher rates of non-adherence, and lower self-efficacy for medication management and health behaviors (Reynolds et al., 2019). The empirical evidence for the relationship between health literacy and HIV disease severity indices (i.e., CD4 count and viral load) is mixed (Kalichman et al., 2000; Pellowski & Kalichman, 2016; Paasche-Orlow et al., 2006; Mayben et al., 2007; Walker et al., 2018). Consequently, a better understanding of how health literacy is assessed may be critical for screening at risk PLWH.
There is no current “gold standard” measurement of health literacy, with a recent systematic review finding over 50 different available measures (Haun et al., 2014) across a wide array of subdomains ranging from comprehension of health information to medical decision-making skills. Similarly, a highly cited review by Sorenson et al. (2012) identified a dozen different conceptual models of health literacy, which they reviewed and consolidated to propose two key competencies central to health literacy: 1) fundamental competencies, including basic knowledge, such as word knowledge and numeracy; and 2) critical competencies, including application of healthcare information.
While existing conceptual models have provided a theoretical foothold from which to examine health literacy in HIV, we know little about the multidimensional nature of the construct in PLWH. A literature search revealed only one study with a factor analytical design that included more than one measure of health literacy. In this study of 191 PLWH, an exploratory factor analysis (EFA) was utilized to investigate the contributions of a health-related reading comprehension measure (i.e., Test of Functional Health Literacy in Adults; TOFHLA), a basic numeracy task (Applied Problems subset of the Woodcock Johnson-III Test of Achievement), and scores from a comprehensive neurocognitive exam to predict the Columbia Medication Management Test (Waldrop-Velverde et al., 2010). Results showed that health-related reading comprehension and basic numeracy loaded onto the same factor, alongside neuropsychological tests of information processing speed and visuoconstructional memory. Scores derived from this factor were independently associated with medication management skills. However, the study was limited in its ability to explore the latent structure of health literacy because: 1) the battery included only one validated measure of health literacy (i.e., health-related reading comprehension); 2) the numeracy task assessed only basic math skills (i.e., unrelated to the context of health); 3) no seronegative persons were assessed (see Delis et al., 2003); and 4) neurocognitive scores were included in factor analysis, which limits the conclusions that could be drawn about health literacy specifically.
With this literature in mind, we first investigated the latent structure(s) of a comprehensive health literacy battery in a sample of HIV seronegative individuals using an EFA. Next, we aimed to confirm the exploratory factor structure of health literacy derived from the seronegative sample in group of PLWH using a confirmatory factor analysis (CFA). Since shared-variance procedures (e.g. factor analysis) can produce discrepant (and sometimes conflicting) results in healthy and clinical populations (e.g., Delis et al., 2003), we sought to evaluate the factor structure of health literacy in persons with and without HIV disease. In this case, our seronegative comparison group was not a “healthy control” group, per se, as it included persons with a variety of psychiatric (e.g., depression, substance use) and medical (e.g., hepatitis C) conditions that are also common in PLWH.
We hypothesized that a CFA would result in the same latent structure for health literacy in PLWH. Finally, we examined the associations between the health literacy factor(s) and HIV serostatus, as well as with measures of health motivation, self-efficacy for HIV management, and health-related decision-making in PLWH. We hypothesized that HIV infection would be associated with lower health literacy and that among PLWH, lower health literacy would be associated with lower motivation and poorer management and decision-making, independent of important co-factors (e.g., education).
Design
Participants
The human research protections programs at the University of California San Diego (UCSD) and University of Alabama at Birmingham (UAB) approved the parent studies. Participants with severe psychiatric (e.g., psychosis) and neurological (e.g., seizure disorder, traumatic brain injury) conditions were excluded. The study sample included 123 HIV seronegative community-dwelling adults enrolled in ongoing studies at UCSD (n=34) or UAB (n=89). The HIV− participants from UCSD were younger (F[1,121]=71.00, p<.001) and had a higher frequency of men (χ2[1]=3.84, p=.050) and Caucasians (χ2[1]=3.14, p=.077) than the UAB participants; the samples did not differ on level of education or household income (p=.634; see Table 1). We also included 220 HIV+ community-dwelling adults that were enrolled in the same ongoing studies at UCSD (n=89) or UAB (n=131) both of which recruited from local HIV clinics and community-based organizations. The parent study at UCSD was a cross-sectional study of internet navigation skills in PLWH, while the parent study at UAB was an investigation of a novel neurorehabilitation approach for PLWH (baseline only). The HIV− participants were recruited into both parent studies as a comparison, rather than a healthy control sample. Thus, they have higher rates of SUD, chronic medical conditions and mood disorders than would be expected from a typical healthy control sample. The HIV+ participants from UCSD were younger (F[1,218]=22.51, p<.001) and more highly educated (F[1,218]=5.24, p=.023), had a higher frequency of men (χ2[1]=52.54, p≤.001) and Caucasians (χ2[1]=29.73, p<.001), and had higher household incomes than the UAB participants (see Table 1).
Table 1.
Demographic and clinical information for HIV+ and HIV− adults
| Variable | HIV+(n = 220) | HIV−(n = 123) | p |
|---|---|---|---|
| Age (years) | 49.3 (9.0) | 55.9 (11.5) | < 0.001 |
| Gender (% men) | 62.3 | 50.4 | 0.033 |
| Education (years) | 13.2 (2.3) | 13.9 (2.4) | 0.010 |
| Site (% UC San Diego) | 40.5 | 27.6 | 0.018 |
| Race/Ethnicity (%) | 0.305 | ||
| African American | 55.6 | 48.8 | |
| Caucasian | 33.7 | 42.3 | |
| Hispanic | 7.4 | 6.5 | |
| Asian | 1.8 | -- | |
| Native American | 1.4 | .8 | |
| Other | .1 | 1.6 | |
| Current Depression (%)b | 41.8 | 20.4 | < 0.001 |
| Health Literacy (Total Scores) | |||
| 3-Briefa | 0 (0, 2) | 0 (0, 3) | 0.987 |
| REALMa | 64 (59, 66) | 64 (61, 66) | 0.358 |
| NVSa | 4 (2, 5) | 4 (3, 5) | 0.149 |
| TOFHLA Reading Comprehension (Raw)a | 48 (44, 49) | 48 (46, 49) | 0.092 |
| TOFHLA Numeracy (Weighted)a | 45 (39, 48) | 45 (42, 48) | 0.028 |
| ENSa | 4 (2, 6) | 5 (3, 6) | 0.031 |
| HIVKQa | 7 (5, 15) | 5 (4, 9) | < 0.001 |
| Medical | |||
| Estimated duration of infection (years) | 15.5 (9.0) | -- | |
| Plasma HIV RNA (% Detectable) | 0.24 | -- | |
| Current CD4 count (cells/μL)a | 641 (418, 857) | -- | |
| Nadir CD4 count (cells/μL)a | 195 (24, 390) | -- |
Note. Data represent M (SD) or valid population % values. HIV = Human Immunodeficiency Virus; CD4 = cluster of differentiation; REALM = The Rapid Estimate of Adult Literacy in Medicine; NVS = Newest Vital Sign; TOFHLA = Test of Functional Health Literacy in Adults; ENS = Expanded Numeracy Scale. HIV Neurobehavioral Research Program
Based on median and interquartile range (IQR) scores
Calculated based on established cut points for POMS (n=123) or CES-D (n=220)
Main Outcome Measures
Health Literacy
The Rapid Estimate of Adult Literacy in Medicine (REALM; Murphy et al., 1993) is a 66-item instrument that assesses capacity to recognize and pronounce health-related words (e.g., “anemia”). Total scores range from 0 to 66 (sample range 11–60), with scores 60 and below commonly used to indicate limited health literacy.
The Newest Vital Sign (NVS; Weiss et al., 2005) is a 6-item performance-based measure of health literacy on which participants answer questions about an ice cream nutrition label (e.g., “If you eat the entire container, how many calories will you eat?”). A total score was generated with a possible range from 0–6 (sample range 0 to 6) with higher scores indicated better health literacy (Cronbach’s alpha=0.70).
The 3-BRIEF is a three-item self-report measure of health literacy problems (Chew et al., 2008). The three items are, “How often do you have someone help you read hospital materials?”, “How often do you have problems learning about your medical condition because of difficulty understanding written information?”, and “How confident are you filling out forms by yourself?” Responses were scored on a scale from 0 (none of the time) to 4 (all of the time) for the first two items and from 0 (extremely) to 4 (not at all) for the third item for a total possible score range of 0 to 12 (sample range 0 to 11). In the current study sample, the Cronbach’s alpha was 0.73.
The Test of Functional Health Literacy in Adults (TOFHLA; Parker et al., 1995) is among the most widely used research instruments to assess health literacy. The measure consists of a 50-item reading comprehension and 17-item numerical ability test, which is weighted with higher scores indicating greater health literacy knowledge. The numeracy score is multiplied by 2.941 to create a score from 0 to 50, the same range as that for the reading comprehension scores. For the purposes of this study, a total score was generated for each section, with scores ranging from 5 to 50 on the weighted numeracy subscale and from 16 to 50 on the reading subscale in our sample.
The Expanded Numeracy Scale (ENS; Lipkus et al., 2001) is a seven-item task assessing the fundamental competency with mathematical concepts (e.g., basic probability) in the context of perceived health risks (e.g., “Which of the following numbers represents the biggest risk of getting a disease: 1 in 10, 1 in 100, or 1 in 1,000?”). A total score for correct items was created and ranged from 0 to 7 in the full sample.
The HIV Knowledge Questionnaire (HIV-KQ-18; Carey & Schroder, 2002) is an 18-item self-administered questionnaire, which measures an individual’s HIV-related knowledge. Each item is scored on three-choice options of true, false, or do not know. A total score ranging from 0 to 18 in the full sample was calculated, with higher scores reflecting greater HIV-related knowledge (sample Cronbach’s alpha=0.91).
Clinical Variables
All participants provided urine samples for toxicology. Current depression was assessed using the Profile of Mood States (POMS; Lorr et al., 1971) for participants recruited from UCSD and the Center for Epidemiological Studies Depression Scale (CES-D; Locke & Putman, 1971) for participants recruited from UAB. HIV disease and treatment characteristics were derived from a clinical interview, clinic records, and blood draw (UCSD only).
Health-Related Management and Decision-Making Measures
The Perceived HIV Self-Management Scale (PHIVMS; Wallston et al., 2011) assessed the participants’ perceived self-efficacy in managing their HIV disease. Participants rated each item statement (e.g., “I succeed in the projects I undertake to manage my HIV infection”) from 1 (“Strongly Disagree”) to 5 (“Strongly Agree”). Due to a transcription error, one item from the scale (“It is difficult for me to find effective solutions for problems managing my HIV infection”) was not included in the questionnaire form. Possible scores ranged from 7 to 35, with higher scores indicating higher levels of perceived ability to self-manage HIV disease. In the current study sample, scores ranged from 7 to 35 and the Cronbach’s alpha was .84.
The Beliefs Related to Medication Adherence (BERMA; Mcdonald-Miszczak et al., 2004) is a questionnaire with three subscales. For the purposes of the current study, the 23-item Dealing with Health Professionals (DWHP) subscale (e.g., “I am good at asking questions about my medical conditions”) and the 24-item Memory for Medications subscale (e.g., “I am poor at remembering the names of my medications”) were used. Participants rated each item on a five-point Likert scale ranging from 1 (“Strongly Disagree”) to 5 (”Strongly Agree”). The subscale range for this sample was from 49 to 115 for DWHP (Cronbach’s alpha=0.94) and 28 to 100 for Memory for Medications (Cronbach’s alpha=0.91).
UCSD Brief Assessment of Capacity to Consent (UBACC; Burton et al., 2012) is a ten-item performance-based test that assesses medical decisional capacity based on questions derived from a hypothetical treatment scenario (see Doyle et al., 2016). Each item is scored from 0 (inadequate) to 2 points (adequate) yielding a possible range of 0–20 (sample range 3 to 19).
The Decisional Conflict Scale (DCS; O’Connor, 1995; Légaré et al., 2010) is a 16-item measure of self-efficacy for health-related decision-making. Briefly, participants are presented with a hypothetical scenario about which they make a decision (Doyle et al., 2016). Participants then answered 16 questions assessing self-efficacy in relation to their decision (e.g., “I know which options are available to me,”) using a scale with a range of 0 to 4 (0=strongly agree, 4=strongly disagree) with higher total values indicating greater decisional conflict. Raw responses were transformed to be on a 0 to 100 scale (sample range 0 to 100), such that 0 indicates the lowest level of decisional conflict and 100 indicated the highest decisional conflict (sample Cronbach’s alpha=0.95).
Data Analyses
For the first set of analyses within the seronegatives, the latent structure of the seven variables of interest (i.e. 3-BRIEF, HIVKQ, REALM, TOFHLA Reading Comprehension, TOFHLA Numeracy (Weighted), NVS and ENS) was evaluated using EFA in SPSS Version 25 (SPSS, 2017). EFA allows for a parsimonious representation of observed correlations between variables by latent factors. We used principal axis factoring (PAF), which helps uncover the underlying structure of original variables by analyzing common/shared variance across variables. An Oblimin rotation, which allows for correlation across components, was applied to the PAF. Factor loadings ≥0.40 were considered significant for individual items (Floyd & Widaman, 1995) and eigenvalues ≥1.0 were considered significant for a factor (Kaiser, 1960). In order to help determine the best number of components, the scree plot and parallel analysis were used to compare the components to simulated chance values (O’Connor, 2000; Glorfeld, 1995). Data were inspected prior to the analysis to ensure that the following assumptions were met: (1) univariate normality within the data must be observed; (2) each factor should at least be comprised of three variables; (3) the ratio of respondents to variables should be at a minimum 5:1; (4) the correlation (r) between the variables should be 0.30 or greater; (5) if data are missing, it should be in a random pattern; and (6) there should be an absence of multicollinearity and singularity (Yong & Pearce, 2013; Field et al., 2012).
A CFA was used to corroborate the latent structure of the health literacy variables that emerged from the EFA conducted in the HIV− individuals to PLWH. The CFA was performed on Mplus Version 7.2 (Muthén & Muthén, 2010). The CFA was conducted to examine the theoretical relationships among our observed and unobserved (latent) variables; in this way, CFA attempts to minimize the difference between the estimated and observed covariance matrices in the data (Schreiber et al., 2006). When testing the predetermined model, several indices are used to identify adequate fit of the model to the data. For continuous data, in addition to the Γ2 goodness-of-fit index, which is limited due to its sensitivity to sample size, recommended indices include: root mean square error of approximation (RMSEA), Tucker-Lewis Index (TLI), and Comparative Fit Index (CFI) (Schreiber et al., 2006). Recommended cutoffs for these indices were used such that good fit would be indicated by RMSEA <0.06, TLI >0.95, and CFI >0.95 (Hu & Bentler, 1999). Maximum likelihood estimation was used with a free data format. For model comparison, three information criteria indices are typically reported: Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), and a sample-size adjusted BIC (sBIC). While no absolute thresholds exist for these indices – they are intended only for comparison of competing models – reduction of AIC, BIC, and sBIC suggests a better model.
Results
Factor Structure in Seronegatives
Examination of the data suggested all assumptions were met. Data were verified for normality (Assumption 1) and all components were comprised of at least three items (Assumption 2). Data were collected on a total of 167 items across the seven variables; our sample of 123 individuals satisfied the recommended minimum 5:1 ratio of respondents to variables (i.e., minimum of 35 respondents; Assumption 3). Correlations between response items were 0.3 and higher (Assumption 4). There were no cases of missing data (Assumption 5). Multicollinearity and singularity (Assumption 6) were assessed using The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett’s test of sphericity. KMO was 0.820, suggesting adequate sampling and utility of the PAF (Kaiser, 1974). Bartlett’s test of sphericity was significant, approximate Γ2(21)=227.53, p<.001, suggesting sufficient relation between variables to detect an underlying component structure (Snedecor & Cochran, 1989). Using an eigenvalue cutoff of 1.0, the PAF resulted in two factors accounting for 59.69% of the cumulative variance. Qualitative review of the unrotated factor matrix suggested all items except for HIVKQ and TOFHLA Numeracy loaded on factor 1. This was improved in the rotated pattern matrix, which suggested a first factor comprised of HIVKQ, TOFHLA Reading, NVS, and ENS and a second factor comprised of 3-BRIEF, REALM, and TOFHLA Numeracy.
Examination of the correlation matrix showed that HIVKQ and TOFHLA Numeracy were not correlated with each other (r=.094, p=.152) while all other comparison pairs were significant at the p≤.05 level. Given the two poor loadings on the unrotated matrix and the qualitative review of the two factors, we tested a solution without those two measures (i.e., HIVKQ and TOFHLA Numeracy). The resulting five variable solution also showed adequate sampling and utility of the PAF. Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy was 0.810. Bartlett’s test of sphericity was significant, approximate Γ2(10)=191.10, p<.001, suggesting sufficient relation between variables to detect an underlying component structure (Snedecor & Cochran, 1989). Using an eigenvalue cutoff of 1.0, the PAF resulted in a single factor accounting for 57.65% of the cumulative variance. The unrotated factor matrix showed the 3-BRIEF, REALM, TOFHLA Reading, NVS, and ENS adequately loaded onto this single factor (all loadings ≥0.40).
Factor Structure in PLWH
We tested the five-variable, single-factor model suggested by the EFA in Study 1. The Γ2 goodness-of-fit test was significant; Γ2(1)=39.35, p<.001. However, the model did not meet our recommended cutoffs for model fit; the RMSEA=0.117 (90% CI: 0.128, 0.230), CFI=0.92, and TLI=0.839. As additional confirmation, we tested a single-factor model with the original seven variables included in Study 1, which also showed poor model fit; Γ2(1)=65.47, p<.001, RMSEA=0.129 (90% CI: 0.099, 0.016), CFI=0.911 and TLI=0.866. Lastly, we tested a seven-variable, bi-factor model, which was consistent with the rotated matrix in the EFA and showed a similar fit to the single-factor seven-variable model; Γ2(1)=60.279, p<.001, RMSEA=0.129 (90% CI:0.097, 0.0162), CFI=0.918, and TLI=0.868. The results suggest a better model fit of the five-variable solution compared to the seven-variable solutions. However, none of the solutions tested above fully met our recommended cutoffs for model fit (see Table 2).
Table 2.
CFA Factor Models tested in HIV+ adults
| Model | Χ2 | Χ2 DF | RMSEA [90% CI] | CFI | TLI | AIC | BIC | sBIC |
|---|---|---|---|---|---|---|---|---|
| 7 Variables 2 Factor | 60.279 | 13 | 0.129 [0.097, 0.162] | 0.918 | 0.868 | 8229.215 | 8303.875 | 8234.156 |
| 7 Variables 1 Factor | 65.472 | 14 | 0.129 [0.099, 0.0162] | 0.911 | 0.866 | 8232.408 | 8303.674 | 8237.125 |
| 5 Variables 1 Factor | 39.346 | 5 | 0.177 [0.128, 0.230] | 0.920 | 0.839 | 5465.534 | 5516.438 | 5468.903 |
| 4 Variables 1 Factor | 0.246 | 1 | 0.000 [0.000, 0.141] | 1.000 | 1.000 | 4541.400 | 4585.517 | 4544.320 |
CFA with 4 Variables: Re-specification
Given the poor fit of the five-variable model, we examined the residual values of the variables, which demonstrated a low value for the 3-BRIEF (<0.40), the remaining variables had higher values (>0.60). Therefore, we explored the fit of a re-specified model using only four variables: REALM, TOHFLA Reading, NVS, and ENS (Table 2). Moreover, to account for the similar test administration in the two reading comprehension measures (REALM and TOHFLA Reading) and to improve model fit, we modeled the residual covariance of the two measures. This four-variable CFA estimation converged normally. The Γ2 goodness-of-fit test was significant; Γ2(1)=0.246, p<.001. Further, the RMSEA, CFI and TLI were all well within recommended cut off value ranges; RMSEA=0.000 (90% CI:0.000, 0.141), CFI=1.000, and TLI=1.000, suggesting that this model provided the best fit to the data in this sample of PLWH (see Figure 1).
Figure 1.
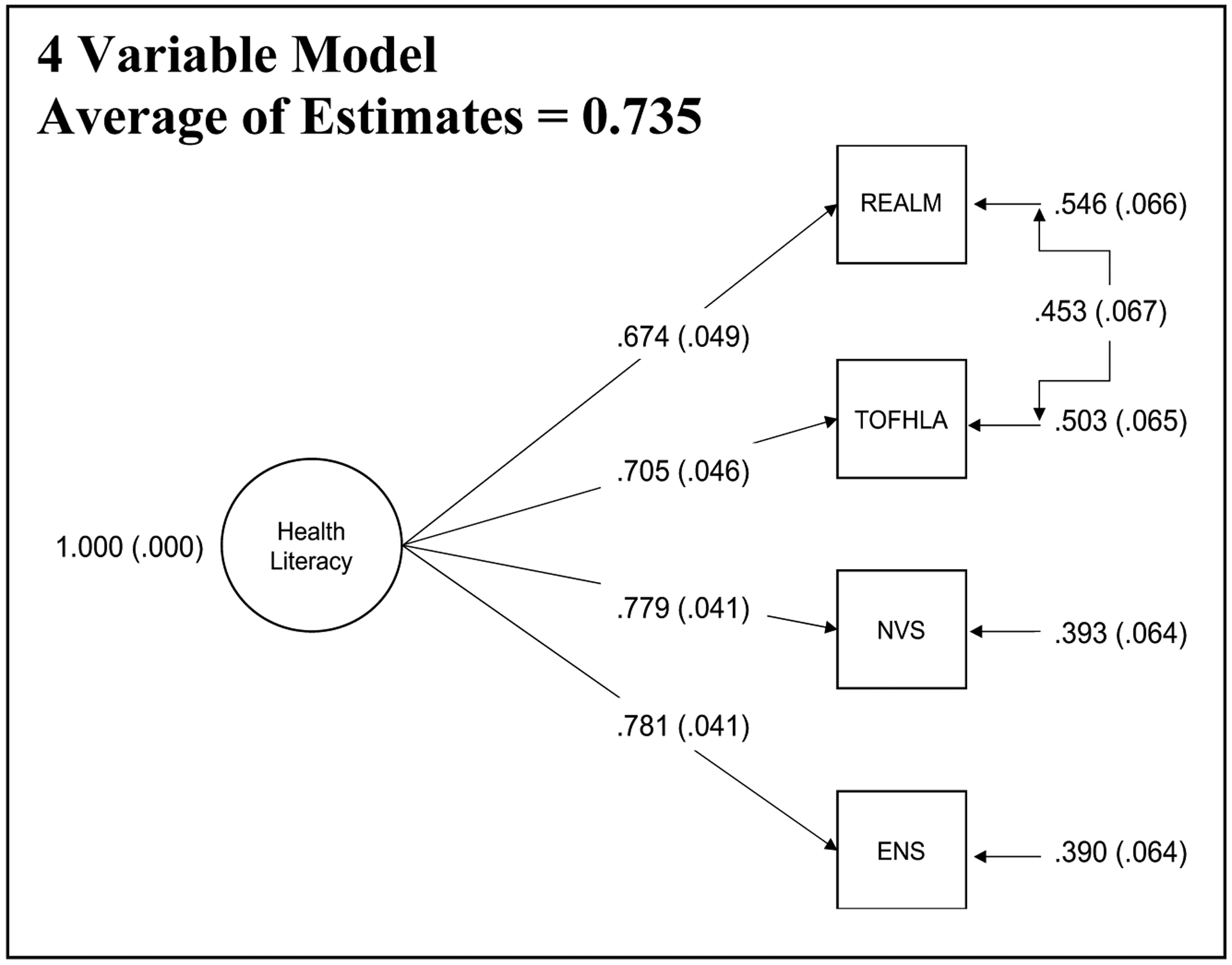
Four variable CFA model of health literacy
Note. Numbers represent loading values. REALM = The Rapid Estimate of Adult Literacy in Medicine; NVS = Newest Vital Sign; TOFHLA = Test of Functional Health Literacy in Adults; ENS = Expanded Numeracy Scale. HIV Neurobehavioral Research Program.
Health Literacy and HIV Serostatus.
Given the results of our CFA, a composite score was created using principal component analysis (PCA) from the four variables in the entire sample (N=343). In order to examine the association between HIV status and the four-measure health literacy composite (REALM, TOFHLA Reading, NVS, and ENS), we used a multiple linear regression model within the entire sample (N=343) with the health literacy composite as the outcome measure and HIV status as an independent variable. Covariates were selected in a data-driven approach by identifying any demographic, psychiatric, or medical variables listed in Table 1 that were associated with both HIV status and the health literacy composite variable (using a critical alpha of 0.05).
The HIV+ group was younger (χ2[1] = 34.9, p<.001), reported fewer years of education (χ2[1]=6.61, p=.010), had a higher proportion of men (χ2[1]=4.56, p=.033), demonstrated higher rates of current depression (χ2[1]=13.6, p<.001), and had more individuals enrolled at the UCSD site (χ2[1]=5.63, p=.018) than the HIV− comparison group. No other variables listed in Table 1 differed significantly by HIV status (all ps>.05). All of the clinicodemographic variables that differed by serostatus, except for current depression (p=.220), were also associated with the health literacy composite score in the full sample (ps<.05) and thus, were included as covariates. Therefore, the regression model included the health literacy composite score as the outcome and HIV status, age, gender, education, and visit site as predictors. The overall model was significant (F[5,337]=34.3, p<.001, adjusted R2=.33). Within this model, HIV status was independently associated with health literacy (95% CI=0.01, 0.20; p=.031), such that participants with HIV had lower scores on the health literacy composite (HIV+ M=.14, SE=.08; HIV− M=−.08, SE=.06). With regard to the covariates, higher levels of education (β=10.27, 95% CI=0.16, 0.24; p<.001), study site (β=−4.70, 95% CI=−0.37, −0.15; p<.001) and younger age (β=−2.06, 95% CI=−0.02, 0.00; p=.040) were all independently associated with higher scores on the health literacy composite, whereas gender (β=−0.02, 95% CI=−0.10, 0.10; p=.982) was not.
Health Literacy and Other Health-related Variables.
Next, in order to examine the downstream effects of the health literacy composite on aspects of critical health behaviors in PLWH, we ran five parallel hierarchical linear regression models only within HIV+ participants (n=220) with health literacy as a predictor variable and Perceived HIV Self-Management Scale (PHIVMS), The Beliefs Related to Medications Survey (BERMA) Dealing with Health Professionals (DWHP) subscale, BERMA Memory for Medications, UCSD Brief Assessment of Capacity to Consent (UBACC), and Decisional Conflict Scale (DCS) as the criterion variables, respectively.
For each hierarchical regression, a data-driven approach was used to select covariates that were related to the health literacy composite and the respective outcome measure within the HIV+ group. As five parallel models were conducted, a critical alpha level of <.01 was used to decrease the risk of Type I error. Age, gender, education, visit site, and ethnicity were all independently associated with the health literacy composite in the HIV+ sample (ps<.05) and were thus investigated as possible covariates for regression models examining the association between the health literacy composite and critical health attitudes and behaviors. None of these potential covariates were associated with PHIVMS or DCS (ps>.05). Education, but none of the other covariates, was associated with BERMA Memory for Medications (p<.001) and BERMA DWHP (p<.001), respectively. Education (p<.001) and ethnicity (p<.001), but none of the other covariates, were associated with UBACC.
The details of the individual regression models are provided in Table 3. The regression model for PHIVMS was significant (Adjusted R2=0.040, ΔR2=0.040, F(1,217)=9.40, p=.002) and health literacy was independently associated with PHIVMS (p=.002). In the BERMA Memory for Medications model, education entered in the first step accounted for a significant amount of variance (Adjusted R2 = 0.039, ΔR2=0.044, F(1,215)=9.84, p=.002). The entry of health literacy at step two accounted for significantly more variance in the outcome (Adjusted R2 = 0.076, ΔR2=0.041, F(2,214)=9.87, p<.001) and the effect of education was no longer significant in step two (p=.115). Correspondingly, in the BERMA DWHP model, education entered in the first step accounted for a significant amount of variance (Adjusted R2 = 0.047, ΔR2=0.051, F(1,215)=11.6, p=.001). The entry of health literacy at step two accounted for significantly more variance in the outcome (Adjusted R2 = 0.088, ΔR2=0.045, F(2,214)=11.4, p<.001) and the effect of education was no longer significant in step two (p=.080). In the UBACC model, the two covariates entered in the first step (i.e. race/ethnicity and education) accounted for a significant amount of variance (Adjusted R2 = 0.118, ΔR2=0.126, F(2,217)=15.7, p<.001) with education being the only significant contributor (p <.001). The entry of health literacy at step two accounted for significantly more variance in the outcome (Adjusted R2 = 0.401, ΔR2=0.283, F(3,216)=50.0, p<.001) and neither of the covariates were significant in step two (ps>.05). Lastly, the regression model for DCS was significant (Adjusted R2=0.030, ΔR2=0.032, F(1,217)=7.17, p=.008) and health literacy was independently associated with DCS (p=.008).
Table 3.
Hierarchical regression results for health literacy associations to self-efficacy for health management and health-related decision-making in HIV
| Model | B | B 95% CI [LL,UL] | β | t | p |
|---|---|---|---|---|---|
| PHIVMS | |||||
| Step 1 | |||||
| Health literacy composite | 0.94 | [0.33, 1.54] | 0.20 | 3.07 | .002 |
| BERMA (Memory for Medications) | |||||
| Step 1 | |||||
| Education (years) | 1.24 | [0.46, 2.02] | 0.21 | 3.14 | .002 |
| Step 2 | |||||
| Education (years) | 0.68 | [−0.17, 1.53] | 0.11 | 1.58 | .115 |
| Health literacy composite | 2.86 | [1.03, 4.69] | 0.22 | 3.08 | .002 |
| BERMA (DWHP) | |||||
| Step 1 | |||||
| Education (years) | 1.51 | [0.64, 2.38] | 0.23 | 3.41 | .001 |
| Step 2 | |||||
| Education (years) | 0.84 | [−0.10, 1.79] | 0.13 | 1.76 | .080 |
| Health literacy composite | 3.39 | [1.35, 5.43] | 0.24 | 3.28 | .001 |
| UBACC | |||||
| Step 1 | |||||
| Ethnicity (%) | 0.52 | [−0.00, 1.03] | 0.13 | 1.97 | .051 |
| Education (years) | 0.51 | [0.31, 0.71] | 0.32 | 4.97 | <.001 |
| Step 2 | |||||
| Ethnicity (%) | −0.18 | [−.624, .270] | −0.04 | −.780 | .437 |
| Education (years) | 0.12 | [−.062, .301] | 0.08 | 1.30 | .196 |
| Health literacy composite | 2.13 | [1.72, 2.55] | 0.62 | 10.2 | <.001 |
| DCS | |||||
| Step 1 | |||||
| Health literacy composite | −2.46 | [−4.27, −0.65] | −0.18 | −2.68 | .008 |
Note. B represents unstandardized regression weights. β represents standardized regression weights. LL and UL indicate the lower and upper limits of a confidence interval, respectively. Health literacy composite = 4 variable health literacy factor score derived using PCA based on the CFA health literacy factor structure. PHIVMS = Perceived HIV Self-Management Scale; BERMA = The Beliefs Related to Medications Survey; DWHP = Dealing with Health Professionals; UBACC = UCSD Brief Assessment of Capacity to Consent; DCS = The Decisional Conflict Scale.
Conclusion
This study sought to investigate the latent structure of health literacy and explore downstream associations between the health literacy composite and measures of self-efficacy for health management and health-related decision-making in HIV. Low health literacy is consistently associated with lower disease prevention and treatment knowledge, higher rates of non-adherence, and lower perceived self-efficacy for medication management and health behaviors in PLWH (see Reynolds et al., 2019 for review). Yet, the construct of health literacy in HIV and the association linking health literacy and health conditions of PLWH is still poorly understood. To our knowledge, this study is the first to use a large database using two representative cohorts of the epidemic with multiple well-validated measures of health literacy to implement a data-driven approach to investigate the latent structure of health literacy and its downstream associations.
We first used EFA to estimate the latent structure(s) of a comprehensive battery of health literacy measures among HIV seronegative individuals. In contrast to theoretical models conceptualizing health literacy as a multidimensional construct (e.g., Sorenson et al., 2012), results showed that the shared variance between a battery of measures of health word reading (i.e., REALM), verbal comprehension (i.e., NVS and TOFHLA Reading), numeracy (i.e., ENS and NVS), and self-reported problems (i.e., 3-BRIEF), was best explained by a single factor that explained over half the variance in the test scores. HIV-KQ-18 and TOFHLA Numeracy both loaded poorly on the unrotated matrix and were therefore removed from the final solution. Qualitative review suggested principal differences at the conceptual and psychometric levels in both of these measures, which may have contributed to their suboptimal loadings. For example, HIV-KQ-18 measures highly disease specific knowledge, while the TOFHLA Numeracy measures numeracy in an applied context. Thus, it is possible that these two aspects of health literacy were sufficiently specific as to preclude their loading with the more general aspects of health literacy measured by the remaining five tests in the battery. We originally included the TOFHLA numeracy measure because numeracy is a core component of health literacy in most conceptual models, including Sorenson et al (2012). However, this particular measure introduced a lot of noise into the CFA model, resulting in a substandard noise-to-signal ratio, and did not improve model fit in any meaningful way. Thus, it was removed in subsequent analyses. Given their content overlap, we were surprised that TOFHLA Numeracy did not load with the Expanded Numeracy Scale (or even Newest Vital Sign) on a numeracy factor or on the general factor. TOHFLA numeracy is a widely used and well-validated measure of health literacy, but in our seronegatives was only weakly correlated with the other health literacy measures whose content included auditory numeracy items (ENS) and aspects of nutritional numeracy (NVS; rs < .25). This is consistent with prior studies showing that TOFHLA numeracy shows fairly modest correlations with other measures of numeracy (e.g., Housten et al., 2018; Griffey et al., 2014). Of course, its poor fit in the current study should not be taken to mean that TOFHLA numeracy scale is not useful or would not show different loadings in other healthy or clinical samples (e.g., Lou et al., 2018). Indeed, studies focused on health specific numeracy would be well advised to consider the TOFHLA.
A one-factor solution of health literacy was also evident from the CFA analysis conducted in PLWH, which was encouraging considering prior research suggesting that the latent structures of various psychological constructs can vary across healthy populations and clinical samples (Delis et al., 2003). Although the original five-test factor solution observed in seronegatives was not a good fit for PLWH, a re-specified four-test solution based on the core performance-based measures of health literacy (i.e., REALM, TOHFLA Reading, NVS, and ENS) provided the best fit to the data in PLWH. Specifically, the removal of the 3-BRIEF–a measure of self-reported problems–greatly improved model fit in PLWH. This may reflect one or more important differences between this measure and the rest of the battery, including its relative brevity (i.e., only three items), format (i.e., self-report), and construct (i.e., self-reported problems rather than capacity). Taken together, the results from these factor analyses converge with those of Waldrop-Valverde et al. (2010) in suggesting a single factor structure of health literacy in PLWH. Our findings extend that earlier work by including a sample of HIV seronegatives, using an expanded battery of performance-based and self-report health literacy measures, and excluding measures of neurocognitive function from the factor analyses, thus giving a conceptually cleaner picture of the latent structure of health literacy.
The single factor structure of health literacy observed in both seronegatives and PLWH appears to reflect more of the “fundamental competencies” of this construct (Sorenson et al., 2012). For example, the majority of measures included assessed basic aspects of health literacy, including health word reading (REALM), numeracy (ENS and NVS), and health reading comprehension (TOFHLA Reading). Thus, these components of health literacy appear to represent a set of core competencies, with no meaningful distinction between numeric and verbal aspects of the construct as measured and analyzed here. It remains to be determined whether the inclusion of higher-level aspects of health literacy (e.g., application) would alter the observed factor structure. Moreover, the numeric and verbal aspects of health literacy may have separable value in other contexts (e.g., in the prediction of various health outcomes) and in different clinical populations. Moreover, the numeric and verbal aspects of health literacy may have separable value in other contexts (e.g., in the prediction of various health outcomes) and in different clinical populations. The single-factor solution in which a global score is used might be most parsimonious in studies for which data reduction is of premium value; for example, as use as a sole indicator of health literacy that is being used primarily as a covariate or is being evaluated in relation to multiple biomarkers or health outcomes. Additionally, future studies can utilize factor analytic approaches rooted in Item Response Theory (Crane et al., 2008; van der Linden & Hambleton, 2013), in order to examine how each of the items is related to the total ability score. As such, these approaches help identify the stronger items and can be used to shorten measures – either through standalone briefer tools or through computer-adapted testing. Another option to help shorten the battery would be Rasch modeling (Mair & Hatzinger, 2007), which applies a slightly different framework, but can be used for a similar purpose. These approaches differ in the aims of the current paper, which had more to do with identifying and operationalizing the underlying latent construct from the total scores rather than examining how the individual items that comprise each measure’s total score relate to the latent construct. In clinical settings, individual components of the current composite with adequate evidence of predictive power (e.g. NVS) can be used instead in shorter batteries and the current study may be used as evidence of its construct validity.
The derived factor of health literacy was lower in PLWH than it was in seronegatives (d=0.22). This finding was commensurate with existing literature suggesting that PLWH are at high risk for low health literacy, which may be partly related to various risk factors for HIV infection (e.g., lower socioeconomic status) and some symptoms of HIV disease (e.g., HIV− associated neurocognitive disorders; Morgan et al., 2015). The association between HIV and health literacy was not better explained by notable cofactors, including sociodemographics (e.g., age, gender, education), study variables (i.e., visit site) and depression. Thus, the single factor model, aside from demonstrating the best fit to the data, also appears to be sensitive to HIV disease independent of important comorbidities.
Notably, the health literacy composite was independently associated with self-efficacy for various aspects of health management and health-related decision-making among PLWH. Findings were independent of education, which dropped to non-significant in the models once health literacy was added. The R2 change values suggested that health literacy accounted for an additional 4–5% of variance in most of these outcomes. The exception was UBACC, for which an additional 12% of variance was explained, perhaps due to the fact that both the predictor and criterion were performance-based measures. Studies consistently show that suboptimal health literacy is associated with lower treatment knowledge, lower motivation for health behaviors and health-related decision-making, and lower perceived self-efficacy for medication management in PLWH (see Reynolds et al., 2019 for review). However, this is the first study to date to directly examine the association between a health literacy factor score, derived from basic tests of reading comprehension and numeracy skills, and aspects of critical health behaviors in PLWH, while excluding measures of neurocognitive function from the factor analyses. Thus, these data suggest that low levels of basic literacy and numeracy skills (i.e. fundamental competency of health literacy) is a major barrier for PLWH and shows significant downstream relevance to important health behaviors in this vulnerable population. Further, the findings from this study offer implications for assessing health literacy in future research and clinical practice that might help identify those at risk for poorer outcomes, which may allow for a more concise battery of measures.
The current study has several notable strengths, including the utilization of multiple diverse samples from two independent sites. Studies often mix samples of healthy participants with clinical populations or use one type of patient (e.g. a full sample of PLWH). This can be highly problematic in studies utilizing shared-variance procedures (Delis et al., 2003). Thus, in order to avoid mixing different types of clinical populations, the current sample utilized a sub-sample of PLWH and a sub-sample of persons with a variety of psychiatric conditions that are also common in PLWH. Another strength is the robustness of the association between the health literacy composite and the respective critical health attitudes (e.g., perceived self-efficacy for health behavior and dealing with health professionals), or health behaviors (e.g., remembering medication details and making health-related decisions) (ps<.01). Specifically, for the BERMA Memory for Medications and DWHP subscales, as well as for UBACC, the addition of education at step one of each model accounted for a significant amount of variance, but that association became null in each of the models after adding in the health literacy composite variable. This finding further highlights the importance of health literacy, over and above general years of education on health attitudes and behaviors.
There are multiple limitations of the current study that are important to consider. Despite including a comprehensive battery of health literacy measures in this study and attempting to capture multidimensionality of health literacy as a construct, our findings were limited by the data, with the majority of the measures capturing the fundamental competencies factor of health literacy. Thus, future studies should look to include more higher order measures of health literacy, which would capture the critical competencies factor using factor analytic designs to gain a better understanding of the construct and more fully explore the conceptual models empirically. Based on our results, we hypothesize that inclusion of these higher order measures would result in a two-factor solution consistent with the Sorenson model of health literacy. Another limitation of this study is the use of exploratory modifications for the CFA analysis in HIV to address poor fit of the tested models. Thus, future studies are needed to confirm the final solution in other samples. Notwithstanding these limitations, results of the current study extend the extant literature by providing preliminary evidence for health literacy as a multidimensional construct in HIV. Our single factor does not provide evidence for previously suggested numeracy versus literacy distinctions in health literacy (Parker et al., 1995), but rather supports lower versus higher order conceptualization of health literacy. Further, the four-variable one-factor solution significantly related to these higher-level functional outcomes which suggests that the composite may be helpful in identifying persons at risk for negative functional outcomes due to low health literacy.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Steven Paul Woods, upon reasonable request.
Footnotes
Disclosures
There are no conflicts of interest for the authors to disclose.
References
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, … & Peel J (2002). Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American journal of public health, 92(8), 1278–1283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, … & Peel J (2004). Health literacy and use of outpatient physician services by medicare managed care enrollees. Journal of general internal medicine, 19(3), 215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman ND, Davis TC, & McCormack L (2010). Health literacy: what is it?. Journal of health communication, 15(S2), 9–19. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, & Crotty K (2011). Low health literacy and health outcomes: an updated systematic review. Annals of internal medicine, 155(2), 97–107. [DOI] [PubMed] [Google Scholar]
- Burton CZ, Twamley EW, Lee LC, Palmer BW, Jeste DV, Dunn LB, & Irwin SA (2012). Undetected cognitive impairment and decision-making capacity in patients receiving hospice care. American Journal of Geriatric Psychiatry, 20, 306–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, & Schroder KE (2002). Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS education and prevention, 14(2), 172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2006. Vol. 18. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008 [Google Scholar]
- Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, … & VanRyn M (2008). Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of general internal medicine, 23(5), 561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho YI, Lee SYD, Arozullah AM, & Crittenden KS (2008). Effects of health literacy on health status and health service utilization amongst the elderly. Social science & medicine, 66(8), 1809–1816. [DOI] [PubMed] [Google Scholar]
- Crane PK, Narasimhalu K, Gibbons LE, Mungas DM, Haneuse S, Larson EB, et al. (2008). Item response theory facilitated cocalibrating cognitive tests and reduced bias in estimated rates of decline. Journal of Clinical Epidemiology, 61, 1018–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Jacobson M, Bondi MW, Hamilton JM, & Salmon DP (2003). The myth of testing construct validity using factor analysis or correlations with normal or mixed clinical populations: Lessons from memory assessment. Journal of the International Neuropsychological Society, 9(6), 936–946. [DOI] [PubMed] [Google Scholar]
- Doyle KL, Woods SP, Morgan EE, Iudicello JE, Cameron MV, Gilbert PE, … & HIV Neurobehavioral Research Program (HNRP) Group. (2016). Health-related decision-making in HIV disease. Journal of clinical psychology in medical settings, 23(2), 135–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A, Miles J, & Field Z (2012). Discovering statistics using R. Sage publications. [Google Scholar]
- Floyd FJ, & Widaman KF (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological assessment, 7(3), 286. [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, & Baker DW (2003). Health literacy and knowledge of chronic disease. Patient education and counseling, 51(3), 267–275. [DOI] [PubMed] [Google Scholar]
- Glorfeld LW (1995). An improvement on Horn’s parallel analysis methodology for selecting the correct number of factors to retain. Educational and psychological measurement, 55(3), 377–393. [Google Scholar]
- Griffey RT, Melson AT, Lin MJ, Carpenter CR, Goodman MS, & Kaphingst KA (2014). Does numeracy correlate with measures of health literacy in the emergency department?. Academic Emergency Medicine, 21(2), 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haun JN, Valerio MA, McCormack LA, Sørensen K, & Paasche-Orlow MK (2014). Health literacy measurement: an inventory and descriptive summary of 51 instruments. Journal of health communication, 19(sup2), 302–333. [DOI] [PubMed] [Google Scholar]
- Housten AJ, Lowenstein LM, Hoover DS, Leal VB, Kamath GR, & Volk RJ (2018). Limitations of the S-TOFHLA in measuring poor numeracy: a cross-sectional study. BMC public health, 18(1), 405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 6(1), 1–55. [Google Scholar]
- Kaiser HF (1960). The application of electronic computers to factor analysis. Educational and psychological measurement, 20(1), 141–151. [Google Scholar]
- Kaiser HF (1974). An index of factorial simplicity. Psychometrika, 39(1), 31–36. [Google Scholar]
- Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, & Rompa D (2000). Health literacy and health-related knowledge among persons living with HIV/AIDS. American journal of preventive medicine, 18(4), 325–331. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Gatti ME, & Jacobson TA (2010). Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient education and counseling, 81(2), 177–181. [DOI] [PubMed] [Google Scholar]
- Légaré F, Kearing S, Clay K, Gagnon S, D’Amours D, Rousseau M, & O’Connor A (2010). Are you SURE?: Assessing patient decisional conflict with a 4-item screening test. Canadian family physician, 56(8), e308–e314. [PMC free article] [PubMed] [Google Scholar]
- Lipkus IM, Samsa G, & Rimer BK (2001). General performance on a numeracy scale among highly educated samples. Medical decision making, 21(1), 37–44. [DOI] [PubMed] [Google Scholar]
- Locke BA, & Putman P (1971). Center for Epidemiological Studies Depression Scale (CES‐D).
- Lorr M, McNair DM, & Droppleman LF (1971). Manual: profile of mood states. San Diego, CA: Educational and Industrial Testing Service. [Google Scholar]
- Luo H, Patil SP, Wu Q, et al. Validation of a combined health literacy and numeracy instrument for patients with type 2 diabetes. Patient Educ Couns. 2018;101(10):1846–1851. doi: 10.1016/j.pec.2018.05.017 [DOI] [PubMed] [Google Scholar]
- Mayben JK, Kramer JR, Kallen MA, Franzini L, Lairson DR, & Giordano TP (2007). Predictors of delayed HIV diagnosis in a recently diagnosed cohort. AIDS patient care and STDs, 21(3), 195–204. [DOI] [PubMed] [Google Scholar]
- Mcdonald-Miszczak L, Maris P, Fitzgibbon T, & Ritchie G (2004). A pilot study examining older adults’ beliefs related to medication adherence: the BERMA survey. Journal of aging and health, 16(5), 591–614. [DOI] [PubMed] [Google Scholar]
- Morgan EE, Iudicello JE, Cattie JE, Blackstone K, Grant I, Woods SP, & HIV Neurobehavioral Research Program (HNRP) Group. (2015). Neurocognitive impairment is associated with lower health literacy among persons living with HIV infection. AIDS and Behavior, 19(1), 166–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy PW, Davis TC, Long SW, Jackson RH, & Decker BC (1993). Rapid estimate of adult literacy in medicine (REALM): a quick reading test for patients. Journal of Reading, 37(2), 124–130. [Google Scholar]
- Muthen LK, & Muthen BO (2010). Mplus user’s guide. 7th. Los Angeles, CA: Muthén & Muthén, 19982006. [Google Scholar]
- O’Connor AM (1995). Validation of a decisional conflict scale. Medical decision making, 15(1), 25–30. [DOI] [PubMed] [Google Scholar]
- O’Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behavior Research Methods, Instruments, & Computers 2000; 32: 396–402. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, Cheng DM, Palepu A, Meli S, Faber V, & Samet JH (2006). Health literacy, antiretroviral adherence, and HIV-RNA suppression. Journal of General Internal Medicine, 21(8), 835–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche‐Orlow MK, Parker RM, Gazmararian JA, Nielsen‐Bohlman LT, & Rudd RR (2005). The prevalence of limited health literacy. Journal of general internal medicine, 20(2), 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, & Nurss JR (1995). The test of functional health literacy in adults. Journal of general internal medicine, 10(10), 537–541. [DOI] [PubMed] [Google Scholar]
- Pellowski JA, & Kalichman SC (2016). Health behavior predictors of medication adherence among low health literacy people living with HIV/AIDS. Journal of health psychology, 21(9), 1981–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds R, Smoller S, Allen A, & Nicholas PK (2019). Health literacy and health outcomes in persons living with HIV disease: a systematic review. AIDS and Behavior, 23(11), 3024–3043. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, … & Bindman AB (2002). Association of health literacy with diabetes outcomes. Jama, 288(4), 475–482. [DOI] [PubMed] [Google Scholar]
- Schreiber JB, Nora A, Stage FK, Barlow EA, & King J (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of educational research, 99(6), 323–338. [Google Scholar]
- Snedecor GW, & Cochran WG (1989). Statistical methods, 8th edn.(Iowa State University Press: Ames, IA: ). [Google Scholar]
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, & Brand H (2012). Health literacy and public health: a systematic review and integration of definitions and models. BMC public health, 12(1), 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS I (2017). IBM SPSS Statistics for Windows, version 25. Armonk, NY: IBM SPSS Corp. [Google Scholar]
- van der Linden WJ, & Hambleton RK (Eds.). (2013). Handbook of modern item response theory. Springer Science & Business Media. [Google Scholar]
- Waldrop-Valverde D, Jones DL, Gould F, Kumar M, & Ownby RL (2010). Neurocognition, health-related reading literacy, and numeracy in medication management for HIV infection. AIDS patient care and STDs, 24(8), 477–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker RL, Hong JH, Talavera DC, Verduzco M, & Woods SP (2018). Health literacy and current CD4 cell count in a multiethnic US sample of adults living with HIV infection. International journal of STD & AIDS, 29(5), 498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Osborn CY, Wagner LJ, & Hilker KA (2011). The perceived medical condition self-management scale applied to persons with HIV/AIDS. Journal of health psychology, 16(1), 109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, … & Hale FA (2005). Quick assessment of literacy in primary care: the newest vital sign. The Annals of Family Medicine, 3(6), 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong AG, & Pearce S (2013). A beginner’s guide to factor analysis: Focusing on exploratory factor analysis. Tutorials in quantitative methods for psychology, 9(2), 79–94. [Google Scholar]


