Abstract
The question of whether rising life expectancy has led to additional life years spent in good health or poor health is of major public health relevance. We tested the theories of compression or expansion of morbidity for Germany with respect to the mental and physical component summary scales (MCS/PCS) of the health-related quality of life (HRQOL) questionnaire (SF-12). Data of 90,758 women and 81,400 men were obtained from the German Socio-Economic Panel between 2002 and 2018. Linear and logistic regression analyses were applied to estimate temporal changes in MCS and PCS in different life stages. The development of healthy life expectancy (H-LE) expressed by life years without severe functional limitations was calculated by applying the Sullivan method.
Overall, a significant increase of MCS and PCS was found in both genders. The rise was mainly due to declining proportions of severe limitations (norm values < 40 points) while the proportions of norm values > 60 points did not change substantially. Improvements were most apparent for the ‘young seniors’ (65–79 years) and at ‘old age’ (80 years +). In contrast, no improvements in PCS were found for ‘later working life’ (50–64 years) and decreasing levels were observed for persons of ‘middle working age’ (30–49 years). During the study period, H-LE at age 50 increased in women/men by 2.93/2.90 years (MCS) and 1.92/2.53 years (PCS), respectively. Our results support the hypothesis of absolute compression of morbidity. However, since consistent improvements were not found for ages below 65 years, it remains open to debate whether the positive health trend will also persist in the future. Our findings suggest that health promotion efforts should be strengthened for people of middle and later working age to support healthy aging.
Keywords: Population health, Trend, Life stages, Temporal change, Health-related quality of life, Morbidity compression, Morbidity expansion
Highlights
-
•
In Germany, mental and physical quality of life increased between 2002 and 2018 for both genders.
-
•
Overall, our findings pointing to absolute compression of morbidity.
-
•
Improvements in health-related quality of life were most pronounced among people aging 65 years or older.
-
•
Our results speak in favor of a life stage specific approach to the analysis of health trends.
Introduction
Increasing life expectancy together with declining fertility rates have contributed to a growing share of older persons in the German population as well as in other industrialized countries. At the same time, the main causes of death have undergone considerable changes. They shifted from infectious diseases and a relatively short period of illness to chronic non-communicable diseases often accompanied with a long survival time preceding death (Jakovljevic & Milovanovic, 2015). The question of whether the rise in life expectancy is providing people with additional years in good health or poor health is of major public health relevance since the outcome of this question has a decisive influence on how health care needs will develop in the future.
In principle, two opposing scenarios about the future development of health in populations have been proposed. The hypothesis of ‘morbidity compression’ postulated by Fries (Fries, 1980) assumes that due to improvements in the prevention of chronic conditions the onset of disability will be postponed leading to decreasing life years spend in morbidity and increasing lifetime in good health. In contrast, the ‘expansion of morbidity hypothesis’ posed by Gruenberg (Gruenberg, 2005) suggested that the decline in mortality is accompanied by an increase in lifetime spent in morbidity. Another assumption postulated by Manton (Manton, 1982), termed as ‘dynamic equilibrium’ suggests that while the number of people in poor health increases, the prevalence of more severe disorders will decline. This assumption refers mainly to people with chronic conditions claiming that their quality of life and functional health status will improve over time.
Bio-medically oriented measures like mortality and morbidity rates provide only a partial picture of the population's health. For this reason, perceived-health measures such as self-rated health (SRH) or health-related quality of life (HRQOL) have been established as elements of health monitoring systems worldwide. Combined with information on the length of life they are used to calculate healthy life expectancy and quality-adjusted life expectancy that give information on a country's burden of diseases (Nordic Burden of Disease, 2019). While SRH is usually assessed by means of a single item on a five-point Likert-scale (Macias, Gold, Öngür, Cohen, & Panch, 2015), HRQOL is a multidimensional construct composed of different health domains including physical functioning, psychological wellbeing and social and role functioning (Guyatt, Feeny, & Patrick, 1993). HRQOL measures provide information on the extent of dysfunction and disability associated with chronic diseases and other health problems. They are considered as appropriate indicators of service needs to inform health policy, planning, and practice (Hennessy, Moriarty, Zack, Scherr, & Brackbill, 1994).
Previous research on self-rated health trends revealed heterogeneous findings, suggesting temporal improvement in SRH (Hanibuchi, Nakaya, & Honjo, 2016; Põld, Pärna, & Ringmets, 2016; Sperlich, Tetzlaff, & Geyer, 2019; Trachte, Sperlich, & Geyer, 2015) as well as no change or even a deterioration of SRH (Galenkamp, Braam, Huisman, & Deeg, 2013; Mairey, Bjerregaard, & Brønnum-Hansen, 2014; Zack, Moriarty, Stroup, Ford, & Mokdad, 2004). Similarly, previous studies on trends in HRQOL are pointing towards health decline (Audureau, Rican, & Coste, 2013; Olfson, Wall, Liu, Schoenbaum, & Blanco, 2018) but also to health improvements (Beltrán-Sánchez, Soneji, & Crimmins, 2015; Gheorghe, Wubulihasimu, Peters, Nusselder, & Van Baal, 2016). So far, the few studies available for Germany are indicating either stability in HRQOL over time (Moor et al., 2018) or health improvements (Ellert & Kurth, 2013).
Recent studies have demonstrated that temporal trends in SRH and HRQOL may vary with age, pointing towards improvements in older ages but no change or even worsening trends in younger ages (Clause-Verdreau, Audureau, Leplège, & Coste, 2019; Greaney, Cohen, Blissmer, Earp, & Xu, 2019; Johansson, Midlöv, Sundquist, Sundquist, & Calling, 2015; Sperlich et al., 2019; Wolff, Nowossadeck, & Spuling, 2017). However, to our knowledge no study exists so far for Germany that analyzed temporal trends in HRQOL for people of different ages. In addition, we are not aware of German studies that provide information on healthy life expectancy with respect to HRQOL. Against this backdrop, we analyzed trends in HRQOL following a life stage approach and tested whether compression or expansion of morbidity applies with respect to severe functional limitations. In more detail, the study was guided by the following research questions:
-
1.
How does HRQOL evolve between 2002 and 2018 at a population level in Germany?
-
2.
Do the trends in HRQOL differ depending on the life stages considered, namely ‘middle working life’ (30–49 years), ‘later working life’ (50–64 years), ‘young seniors’ (65–79 years) and persons of ‘old age’ (80+ years)?
-
3.
Do the findings indicate compression or expansion of morbidity with respect to severe limitations in HRQOL?
Methods
Data source
The following analyses are based on data from the German Socio-Economic Panel (GSOEP V.31), conducted by the German Institute for Economic Research. The GSOEP is a representative annual survey of German individuals in private households that started in 1984. Data were collected by face-to-face interviews using different questionnaires for individuals, households or specific subgroups. The HRQOL-questionnaire as the core instrument of this study is applied bi-annually from 2002 on. Our analyses are based on a pooled dataset containing all even calendar years from 2002 to 2018, allowing for trend analysis on a population level. We used cross-sectional weights that are assumed to produce a nationally representative sample (Goebel et al., 2019). Further information on the GSOEP can be obtained from Frick et al. (Frick, Schupp, & Wagner, 2007). We included individuals aged 30 years and over and assigned the population to four different life stages, namely ‘middle working life’ (30–49 years) ‘later working life’ (50–64 years), ‘young seniors’ (65–79 years) and ‘old age’ (80+ years). Severe limitations in physical health (PCS) are rare in ages below 30 years. For example, in our data only 3.8% of individuals aged between 20 and 30 years show severe physical health limitations. Hence, we started our analysis from ages above 30 years.
Overall, 51,003 respondents (24,482 men/26,521 women) were observed 172,158 (81,400 men/90,758 women) times between 2002 and 2018, corresponding to an average participation in 3.3 and 3.4 waves for men and women, respectively. The weighted sample characteristics, separated by gender and time period, are presented in Table 1. The proportion of missing values varied between 0 and 5.0%. Respondents with missing information were excluded (Table 1).
Table 1.
Weighted sample characteristics in % by time period, GSOEP 2002–2018, n = 198,391.
| 2002/04 (n = 44,896) |
2006/08 (n = 44,749) |
2010/12 (n = 40,778) |
2014/16 (n = 45,041) |
2018 (n = 22,927) |
|
|---|---|---|---|---|---|
| % | % | % | % | % | |
| Sex | |||||
| women | 52.0 | 52.0 | 51.9 | 51.7 | 51.6 |
| men | 48.0 | 48.0 | 48.1 | 48.3 | 48.4 |
| missing | 0 | 0 | 0 | 0 | 0 |
| Age groups in years | |||||
| 30–49 | 43.6 | 42.8 | 40.2 | 37.4 | 36.0 |
| 50–64 | 28.2 | 27.3 | 29.4 | 31.6 | 32.7 |
| 65–79 | 22.4 | 23.3 | 23.5 | 23.7 | 22.9 |
| 80+ | 5.7 | 6.6 | 6.9 | 7.2 | 8.3 |
| missing | 0 | 0 | 0 | 0 | 0 |
| HRQOL | |||||
| PCS (Mean/SD) | 47.5/10.4 | 47.5/10.4 | 46.9/10.4 | 47.3/10.4 | 47.4/10.4 |
| MCS (Mean/SD) | 49.5/10.4 | 50.0/10.3 | 49.9/10.3 | 51.0/10.2 | 51.2/9.9 |
| missing MCS/PCS | 5.0 | 3.8 | 3.2 | 3.3 | 2.0 |
GSOEP: German Socio-Economic Panel; n = weighted number of observations, HRQOL = Health-related quality of life.
MCS = Mental Component Scale, PCS = Physical Component Scale, Mean/SD = Mean value/Standard deviation.
Measures
Health-related quality of life (HRQOL)
HRQOL was assessed using a slightly modified version of the second version of the 12-Item Short Form Health Survey (SF-12v.2) (Nübling, Andersen, Mühlbacher, Schupp, & Wagner, 2007). The SF-12v.2 includes 12 items making up eight scales: physical functioning, role limitations due to physical problems, bodily pain, general health, vitality, social functioning, role limitation due to emotional problems and perceived mental health. Based on these items a physical component summary (PCS) score and a mental component summary (MCS) score were calculated. Values are standardized to a national norm (GSOEP population in 2004) ranging from 0 to 100 points with a mean of 50 points and a standard deviation of 10 points (Nübling et al., 2007). A higher score corresponds to a better health status. Norm values below 40 (mean value minus 1 standard deviation: 50–10 = 40) are considered to be below average while norm values from 60 (mean plus 1 standard deviation: 50 + 10 = 60) are to be assessed as above-average performance. Building on this convention, proportions of norm values below 40 and above 60 in HRQOL were calculated, which means that HRQOL is significantly below and above the population average of the year 2004. In addition, mean values of HRQOL were considered.
Time trend
For graphical illustration, panel waves between the years 2002 and 2018 were classified into five consecutive time periods (2002/2004, 2006/2008, 2010/2012, 2014/2016 and 2018). In order to establish the effect of time on HRQOL, a continuous trend variable was created ranging from 0 to 1 for the entire study period. The first year of observation (2002) is coded as 0 and the last year (2018) as 1, with the years in between getting fractional values according to the following formula: [(year-2002)/(2018-2002)]. The coefficients obtained with this variable can be interpreted as the average change in MCS/PCS over the whole study period.
Statistical analysis
We performed logistic regression analyses for the dichotomous outcomes (MCS/PCS < 40 points and MCS/PCS > 60 points) and linear regression analyses for the interval-scaled outcomes (mean values of MCS/PCS). We tested the effect of time on MCS/PCS using cluster-robust standard errors to adjust for the panel structure of the data. In addition to unstandardized regression coefficients (coef) and odds ratios (OR) we reported predicted means and probabilities (margins at means) giving the trends a more substantial interpretation. All regression analyses were performed separately for men and women and each life stage. We controlled for age by including a continuous age-variable as a covariate, taking possible shifts in age composition within the life stages into account. We did not control for other background characteristics such as socioeconomic status since our aim was to analyze the real change unadjusted for social factors potentially contributing to temporal trends. For all analyses, population weights were employed to match the official population statistics.
In order to test whether compression or expansion of HRQOL applied, we calculated changes in healthy life expectancies (H-LE) by applying the method introduced by Sullivan (Sullivan, 1971). The method combines data issued from a regular period life table on the one hand and from cross-sectional survey providing prevalence of a given health dimension on the other hand. The main advantage of the Sullivan's method lies in the separate collection of mortality and disability data. In our case, disability data was obtained from the SOEP survey while mortality data was derived from period life tables of the Federal Statistical Office (Destatis, 2019). These life tables cover 3 years as standard. We used life tables from three time-periods (2002–2004, 2010–2012, and 2016–2018) for calculating H-LE. Since the HRQOL-questionnaire was assessed by a two-yearly rhythm, data was not available for the uneven years. We calculated H-LE by applying the age- and gender-specific prevalence of ‘no severe limitations in mental/physical health’ to further LE. This value can be interpreted as the number of remaining years, at a particular age, which an individual can expect to live without severe mental and physical limitations. We calculated this value by subtracting the value 1 from the proportion of severe limitations defined as a significant deviation below the average (norm values MCS/PCS < 40 points). Furthermore, we determined the health ratio as the proportion of remaining life expected to be spent without severe limitations to the total remaining life time. In our case, relative compression of morbidity is present if this ratio increases over time. For meeting the condition for absolute compression also the total number of life years expected to live with severe health limitations decreases over time (Howse, 2006). Therefore, we additionally calculated the expected LE with severe mental and physical limitations as the number of remaining years with norm values of PCS and MCS significantly below the average. Further information on the Sullivan Method and the calculation of H-LE can be found in the manual written by Jagger (Jagger, 2007). Microsoft Excel version 2010 was used for life table analysis, regression analyses were performed using STATA 11.1.
Results
The weighted sample characteristics, separated by time periods, are presented in Table 1. Over time the proportion of subjects aged 30–49 years decreased while in particular the number of those aged 50–64 years increased. The distribution of gender did not change substantially over time.
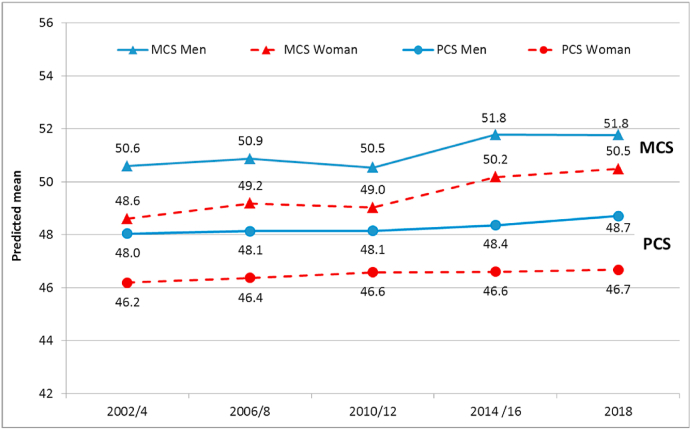
Temporal development in HRQOL between 2002 and 2018 – all ages
In both genders, mean scores of MCS were higher as compared to that of PCS. Women as compared to men reported consistently lower levels of MCS and PCS at each time period (Fig. 1). Over time, the mean scores of both subscales improved for both genders. For example, norm values of MCS increased for men and women of ‘all ages’ on average by 1.17 points (95%CI 0.68 to 1.67) and 1.77 points (95%CI 1.28 to 2.27), respectively (Table 2). The increase was mainly due to declining proportions of severe limitations in mental and physical health (norm values < 40 points) while the proportions of high levels of HRQOL (norm values > 60 points) did not improve substantially over time. The only exception was found in women where norm values > 60 points for PCS significantly increased (OR = 1.36, 95%CI 1.06 to 1.76).
Fig. 1.
Temporal development of mental and physical component scale (MCS/PCS) of HRQOL in men and women of all ages (30 yr and above).
Table 2.
Effect of time on MCS and PCS (mean norm values, norm values < 40 and >60 points) in men and women for all ages and according to different life stages, Germany, 2002–2018.
| Mean norm values |
Norm values < 40 pts |
Norm values > 60 pts |
||||
|---|---|---|---|---|---|---|
| Time-Trend | Coef | 95% CI | OR | 95% CI | OR | 95% CI |
| Men: MCS | ||||||
| all ages | 1.17*** | 0.68–1.67 | 0.74*** | 0.64–0.85 | 1.03 | 0.92–1.16 |
| 30–49 yr. | 1.69*** | 1.09–2.28 | 0.78** | 0.65–0.92 | 1.39** | 1.15–1.68 |
| 50–64 yr. | 0.92* | 0.22–1.61 | 0.83 | 0.69–1.01 | 0.93 | 0.78–1.11 |
| 65–79 yr. | 1.88*** | 1.06–2.70 | 0.60** | 0.46–0.77 | 1.27* | 1.06–1.53 |
| 80+ yr. | 2.38* | 0.47–4.23 | 0.48** | 0.31–0.75 | 1.08 | 0.72–1.64 |
| Men: PCS | ||||||
| all ages | 1.30*** | 0.81–1.78 | 0.78*** | 0.70–0.87 | 1.00 | 0.75–1.32 |
| 30–49 yr. | −0.34 | −0.83-0.14 | 1.31* | 1.06–1.62 | 1.00 | 0.84–1.20 |
| 50–64 yr. | 0.48 | −0.22-1.17 | 0.89 | 0.76–1.05 | 0.83 | 0.60–1.15 |
| 65–79 yr. | 2.33*** | 1.54–3.13 | 0.67*** | 0.56–0.79 | 2.18** | 1.29–3.70 |
| 80+ yr. | 2.23* | 0.63–3.84 | 0.71 | 0.51–1.00 | ||
| Women: MCS | ||||||
| all ages | 1.77*** | 1.28–2.27 | 0.73*** | 0.65–0.82 | 1.12 | 0.99–1.27 |
| 30–49 yr. | 2.31*** | 1.77–2.85 | 0.66*** | 0.58–0.75 | 1.20 | 0.98–1.45 |
| 50–64 yr. | 0.75* | 0.05–1.44 | 0.90 | 0.77–1.06 | 1.00 | 0.84–1.20 |
| 65–79 yr. | 2.60*** | 1.77–3.44 | 0.61*** | 0.50–0.74 | 1.29** | 1.07–1.57 |
| 80+ yr. | 3.96*** | 2.40–5.51 | 0.49*** | 0.36–0.67 | 1.15 | 0.81–1.63 |
| Women: PCS | ||||||
| all ages | 1.16*** | 0.71–1.62 | 0.82*** | 0.74–0.90 | 1.36* | 1.06–1.76 |
| 30–49 yr. | −0.50* | −0.98–−0.02 | 1.24* | 1.04–1.49 | 0.96 | 0.81–1.12 |
| 50–64 yr. | −0.09 | −0.73-0.55 | 1.05 | 0.91–1.21 | 1.20 | 0.90–1.60 |
| 65–79 yr. | 2.42*** | 1.63–3.22 | 0.67*** | 0.57–0.78 | 2.30** | 1.29–4.09 |
| 80+ yr. | 2.19** | 0.86–3.53 | 0.68* | 0.51–0.91 | ||
Notes: time trend adjusted for age, MCS = Mental Component Summary, PCS = Physical Component Summary, norm values < 40 points = a standard deviation (SD) of 10 points below the mean norm, norm values > 60 points = a SD of 10 points above the mean norm, the continuous time-trend variable is coded 0 for 2002 and 1 for 2018 (reference group: 2002). 95%CI = confidence interval of 95%, *p < 0.05, **p < 0.01, ***p < 0.001. Norm values > 60 points for PCS are not displayed for age 80+ due to small sample size (n < 20).
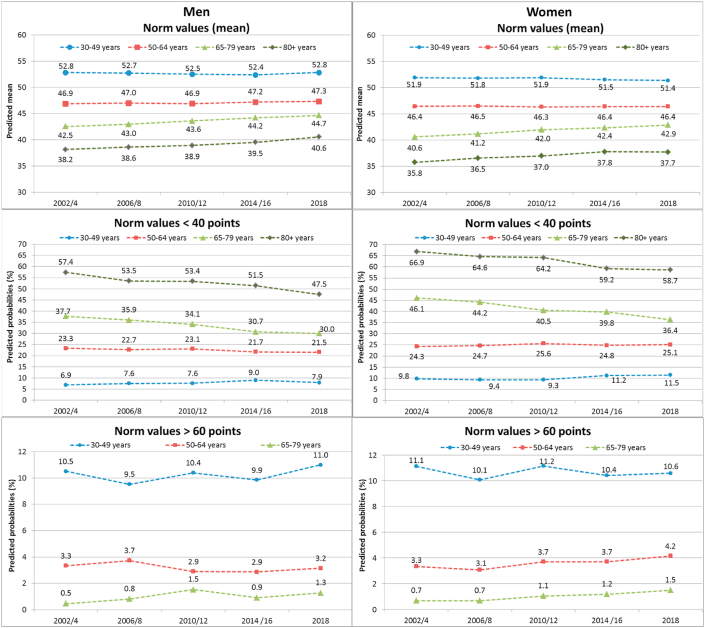
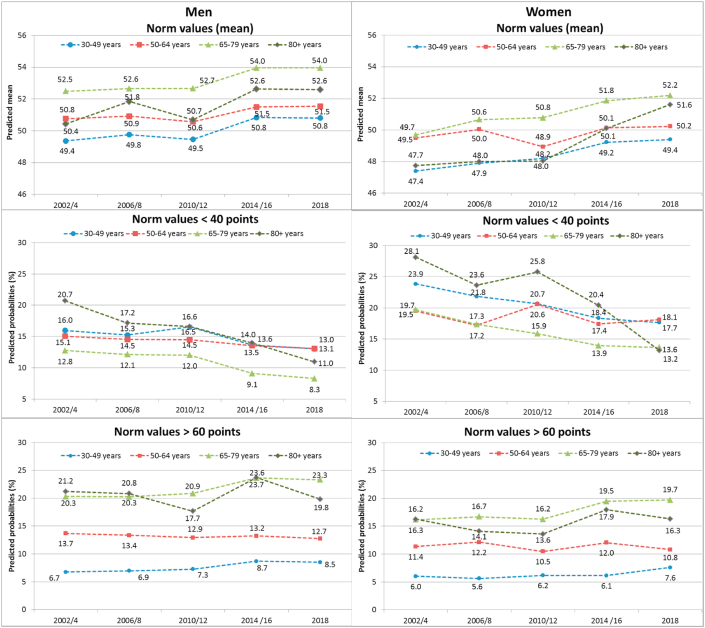
Temporal changes in HRQOL across life-stages
At each time point, levels of PCS were highest for persons aged 30–49 years and decreased steadily with age (Fig. 2). By contrast, levels of MCS were higher among young seniors (65–79 years) and people of old age (80 years or older) while younger individuals showed consistently lower levels of mental wellbeing (Fig. 3). In both genders, significant improvements in PCS were found only in young seniors and in people of old age (Table 2). In the latter age group predicted probabilities of severe limitations in PCS (norm values < 40 points) declined in women from 66.9% to 58.7% (OR = 0.68, 95%CI 0.51 to 0.91) and in men from 57.4% to 47.5% (OR = 0.71, 95%CI 0.51 to 1.00) (Fig. 2 and Table 2). Among women aged 65–79 years, severe limitations in PCS decreased from 46.1% to 36.4% (OR = 0.67, 95%CI 0.57 to 0.78) and in men of the same age from 37.7% to 30.0% (OR = 0.67, 95%CI 0.56 to 0.79). In addition, also norm values > 60 points significantly increased in that life stage for both women (OR = 2.30, 95%CI 1.29 to 4.09) and men (OR = 2.18, 95%CI 1.29 to 3.70). By contrast, PCS did not change or even tended to decline over time in women and men of working age. For example, among women of middle working age (30–49 years) the proportion of severe limitations increased from 9.8% to 11.5% (OR = 1.24, 95%CI 1.04 to 1.49) and in men of that age from 6.9% to 7.9% (OR = 1.31, 95%CI 1.06 to 1.62) while they remained largely the same for women and men of later working life (50–64 years) (Table 2). With respect to MCS (Fig. 3 and Table 2) significant improvements were found for all ages, but here too, the improvements were more pronounced for ages beyond working age.
Fig. 2.
Temporal development of the physical component scale (PCS) of HRQOL according to different life-stages in men (left) and women (right).
Fig. 3.
Temporal development of the mental component scale (MCS) of HRQOL according to different life-stages in men (left) and women (right).
Changes in healthy and unhealthy life expectancy
LE as well as H-LE increased over the study period. With the exception of ages above 84 years, this increase revealed to be statistically significant (Table 3). For example, in 2002–04, men aged 50 years could expect to live another 28.3 years of which 24.0 years (95%CI 23.4 to 24.6) are expected to be lived without severe mental limitations (H-LE: MCS) and 18.9 years (95%CI 18.4 to 19.4) without severe physical limitations (H-LE: PCS). In 2016-18, LE increased in men to 30.2 years while H-LE increased to 26.9 years (95%CI 26.4 to 27.5) (MCS) and 21.4 years (95%CI 20.9 to 21.9) (PCS), respectively. Women of that age could expect to live another 33.0 years at baseline, of which 26.0 years (95%CI 25.4 to 26.6) are expected to be lived without severe mental and 19.7 years (95%CI 19.1 to 22.2) without severe physical limitations. In 2016-18, LE increased to 34.4 years while H-LE for MCS and PCS increased to 28.9 (95%CI 28.3 to 29.5) and 21.6 years (95%CI 21.1 to 22.1), respectively.
Table 3.
Life expectancy (total) and without severe limitations in mental (MCS) and physical health (PCS) at different time-periods.
| MCS | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
|||||||||||||||||||||||||
| 2002/04 |
2010/12 |
2016/18 |
2002/04 |
2010/12 |
2016/18 |
|||||||||||||||||||||
| Age |
LE |
H-LE |
95%CI |
LE |
H-LE |
95%CI |
LE |
H-LE |
95%CI |
p |
LE |
H-LE |
95%CI |
LE |
H-LE |
95%CI |
LE |
H-LE |
95%CI |
p |
||||||
| lower | upper | lower | upper | lower | upper | lower | upper | lower | upper | lower | upper | |||||||||||||||
| 30 | 46.93 | 39.64 | 38.96 | 40.32 | 48.55 | 41.26 | 40.53 | 41.99 | 49.21 | 43.41 | 42.77 | 44.05 | *** | 52.23 | 40.59 | 39.88 | 41.30 | 53.36 | 42.59 | 41.85 | 43.34 | 53.78 | 44.88 | 44.19 | 45.57 | *** |
| 35 | 42.12 | 35.59 | 34.94 | 36.23 | 43.72 | 37.17 | 36.49 | 37.85 | 44.36 | 39.17 | 38.56 | 39.79 | *** | 47.32 | 36.87 | 36.18 | 37.55 | 48.44 | 38.74 | 38.04 | 39.45 | 48.87 | 40.79 | 40.12 | 41.45 | *** |
| 40 | 37.37 | 31.58 | 30.96 | 32.21 | 38.92 | 33.16 | 32.54 | 33.79 | 39.56 | 35.02 | 34.43 | 35.61 | *** | 42.46 | 33.25 | 32.59 | 33.92 | 43.57 | 34.82 | 34.16 | 35.49 | 43.99 | 36.70 | 36.05 | 37.34 | *** |
| 45 | 32.75 | 27.67 | 27.07 | 28.27 | 34.21 | 29.24 | 28.64 | 29.83 | 34.83 | 30.89 | 30.32 | 31.46 | *** | 37.69 | 29.64 | 28.99 | 30.28 | 38.75 | 30.98 | 30.34 | 31.62 | 39.16 | 32.83 | 32.20 | 33.47 | *** |
| 50 | 28.32 | 24.01 | 23.43 | 24.60 | 29.65 | 25.49 | 24.93 | 26.06 | 30.23 | 26.91 | 26.36 | 27.46 | *** | 33.04 | 25.99 | 25.36 | 26.62 | 34.04 | 27.26 | 26.65 | 27.88 | 34.42 | 28.92 | 28.31 | 29.54 | *** |
| 55 | 24.08 | 20.54 | 19.97 | 21.10 | 25.34 | 21.77 | 21.24 | 22.31 | 25.82 | 23.06 | 22.53 | 23.59 | *** | 28.50 | 22.38 | 21.77 | 22.98 | 29.46 | 23.88 | 23.28 | 24.47 | 29.80 | 25.17 | 24.57 | 25.78 | *** |
| 60 | 20.05 | 17.01 | 16.47 | 17.56 | 21.28 | 18.43 | 17.92 | 18.94 | 21.69 | 19.48 | 18.97 | 19.99 | *** | 24.08 | 18.76 | 18.18 | 19.33 | 25.03 | 20.27 | 19.70 | 20.84 | 25.34 | 21.50 | 20.92 | 22.09 | *** |
| 65 | 16.26 | 13.75 | 13.21 | 14.29 | 17.46 | 15.08 | 14.59 | 15.57 | 17.87 | 16.18 | 15.69 | 16.67 | *** | 19.77 | 15.24 | 14.68 | 15.80 | 20.74 | 16.70 | 16.15 | 17.24 | 21.06 | 17.93 | 17.37 | 18.50 | *** |
| 70 | 12.83 | 10.60 | 10.06 | 11.15 | 13.87 | 11.82 | 11.35 | 12.29 | 14.33 | 12.95 | 12.48 | 13.43 | *** | 15.67 | 11.76 | 11.22 | 12.29 | 16.61 | 13.19 | 12.67 | 13.71 | 16.98 | 14.35 | 13.80 | 14.90 | *** |
| 75 | 9.83 | 7.88 | 7.31 | 8.45 | 10.54 | 8.81 | 8.33 | 9.29 | 11.02 | 9.81 | 9.35 | 10.28 | *** | 11.93 | 8.71 | 8.19 | 9.22 | 12.67 | 9.81 | 9.30 | 10.33 | 13.11 | 10.89 | 10.36 | 11.41 | *** |
| 80 | 7.24 | 5.57 | 3.94 | 6.20 | 7.68 | 6.34 | 5.83 | 6.85 | 8.00 | 7.03 | 6.54 | 7.52 | * | 8.64 | 6.08 | 5.57 | 6.60 | 9.17 | 6.75 | 6.24 | 7.26 | 9.50 | 7.84 | 7.31 | 8.37 | *** |
| 85 | 5.19 | 3.57 | 2.82 | 4.33 | 5.38 | 4.23 | 3.63 | 4.83 | 5.51 | 4.80 | 4.24 | 5.35 | ns | 6.01 | 3.86 | 3.30 | 4.42 | 6.31 | 4.68 | 4.14 | 5.22 | 6.49 | 5.27 | 4.71 | 5.83 | * |
|
90+ |
3.64 |
2.23 |
1.26 |
3.19 |
3.66 |
3.04 |
2.25 |
3.84 |
3.71 |
3.20 |
2.45 |
3.95 |
ns |
4.02 |
2.29 |
1.68 |
2.90 |
4.21 |
2.93 |
2.25 |
3.62 |
4.27 |
3.49 |
2.85 |
4.14 |
ns |
| PCS | ||||||||||||||||||||||||||
| Men | Women | |||||||||||||||||||||||||
| 2002/04 | 2010/12 | 2016/18 | 2002/04 | 2010/12 | 2016/18 | |||||||||||||||||||||
| Age | LE | H-LE | 95%CI | LE | H-LE | 95%CI | LE | H-LE | 95%CI | p | LE | H-LE | 95%CI | LE | H-LE | 95%CI | LE | H-LE | 95%CI | p | ||||||
| lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
|||||||||||||||
| 30 | 46.93 | 36.43 | 35.80 | 37.06 | 48.55 | 37.71 | 37.01 | 38.40 | 49.21 | 38.83 | 38.24 | 39.42 | *** | 52.23 | 37.13 | 36.49 | 37.77 | 53.36 | 38.37 | 27.69 | 39.06 | 53.78 | 38.79 | 38.19 | 39.38 | ** |
| 35 | 42.12 | 31.80 | 31.22 | 32.39 | 43.72 | 33.06 | 32.43 | 33.69 | 44.36 | 34.18 | 33.63 | 34.74 | *** | 47.32 | 32.46 | 31.86 | 33.06 | 48.44 | 33.68 | 33.05 | 34.31 | 48.87 | 34.29 | 33.72 | 34.85 | ** |
| 40 | 37.37 | 27.24 | 26.69 | 27.80 | 38.92 | 28.45 | 27.89 | 29.02 | 39.56 | 29.65 | 29.12 | 30.17 | *** | 42.46 | 27.94 | 27.37 | 28.52 | 43.57 | 29.11 | 28.53 | 29.70 | 43.99 | 29.83 | 29.29 | 30.38 | *** |
| 45 | 32.75 | 22.88 | 22.36 | 23.41 | 34.21 | 24.15 | 23.62 | 24.67 | 34.83 | 25.36 | 24.86 | 25.86 | *** | 37.69 | 23.70 | 23.16 | 24.25 | 38.75 | 24.78 | 24.24 | 25.33 | 39.16 | 25.57 | 25.04 | 26.09 | *** |
| 50 | 28.32 | 18.85 | 18.35 | 19.35 | 29.65 | 20.06 | 19.58 | 20.55 | 30.23 | 21.38 | 20.90 | 21.85 | *** | 33.04 | 19.65 | 19.14 | 20.17 | 34.04 | 20.72 | 20.21 | 21.23 | 34.42 | 21.57 | 21.07 | 22.07 | *** |
| 55 | 24.08 | 15.24 | 14.77 | 15.71 | 25.34 | 16.33 | 15.88 | 16.78 | 25.82 | 17.64 | 17.19 | 18.09 | *** | 28.50 | 15.84 | 15.35 | 16.33 | 29.46 | 17.02 | 16.54 | 17.49 | 29.80 | 17.82 | 17.34 | 18.30 | *** |
| 60 | 20.05 | 11.99 | 11.55 | 12.42 | 21.28 | 13.16 | 12.74 | 13.57 | 21.69 | 14.23 | 13.80 | 14.66 | *** | 24.08 | 12.40 | 11.95 | 12.85 | 25.03 | 13.69 | 13.24 | 14.14 | 25.34 | 14.43 | 13.98 | 14.89 | *** |
| 65 | 16.26 | 9.27 | 8.84 | 9.70 | 17.46 | 10.42 | 10.03 | 10.81 | 17.87 | 11.52 | 11.11 | 11.93 | *** | 19.77 | 9.32 | 8.90 | 9.74 | 20.74 | 10.60 | 10.18 | 11.02 | 21.06 | 11.37 | 10.94 | 11.80 | *** |
| 70 | 12.83 | 6.71 | 6.29 | 7.13 | 13.87 | 7.63 | 7.27 | 7.99 | 14.33 | 8.90 | 8.52 | 9.29 | *** | 15.67 | 6.69 | 6.30 | 7.08 | 16.61 | 6.89 | 6.51 | 7.27 | 16.98 | 8.45 | 8.04 | 8.85 | *** |
| 75 | 9.83 | 4.80 | 4.36 | 5.23 | 10.54 | 5.24 | 4.88 | 5.59 | 11.02 | 6.25 | 5.89 | 6.61 | *** | 11.93 | 4.49 | 4.13 | 4.85 | 12.67 | 5.20 | 4.84 | 5.57 | 13.11 | 5.89 | 5.52 | 6.26 | *** |
| 80 | 7.24 | 3.02 | 2.56 | 3.48 | 7.68 | 3.37 | 3.01 | 3.73 | 8.00 | 4.00 | 3.63 | 4.36 | * | 8.64 | 2.80 | 2.45 | 3.15 | 9.17 | 3.22 | 2.87 | 3.56 | 9.50 | 3.75 | 3.39 | 4.11 | ** |
| 85 | 5.19 | 1.91 | 1.36 | 2.47 | 5.38 | 1.82 | 1.43 | 2.21 | 5.51 | 2.50 | 2.10 | 2.90 | ns | 6.01 | 1.72 | 1.34 | 2.09 | 6.31 | 1.98 | 1.63 | 2.34 | 6.49 | 2.40 | 2.03 | 2.78 | ns |
| 90+ | 3.64 | 1.26 | 0.53 | 1.98 | 3.66 | 0.82 | 0.41 | 1.23 | 3.71 | 1.59 | 1.06 | 2.12 | ns | 4.02 | 0.91 | 0.53 | 1.30 | 4.21 | 1.25 | 0.80 | 1.70 | 4.27 | 1.29 | 0.90 | 1.68 | ns |
Notes: LE = total life expectancy (Destatis, 2019), H-LE=Healthy life expectancy (without severe limitations in mental/physical health), 95%CI = confidence interval of 95%, p = significant change in H-LE between first (2002/4) and last time-point (2016/18): *p < 0.05, **p < 0.01, ***p < 0.001, ns = not significant (p > 0.05).
In addition, the proportion of life spent without severe health limitations (‘health-ratio’) rose over time, however not always reaching statistical significance (Table 4). For example, in 2002-04 women aged 50 years could expect to live 78.7% (95%CI 78.0 to 79.3) of their remaining lifetime without severe mental limitations. In 2016-18, this proportion increased to 84.0% (95%CI 83.4 to 84.6) while the proportion of life spent without severe physical limitations increased from 59.5% (95%CI 59.0 to 60.0) to 62.7% (95%CI 62.2 to 63.2). In men of the same age, the health-ratio increased for MCS from 84.8% (95%CI 84.2 to 85.4) to 89.0% (95%CI 88.5 to 89.6) and for PCS from 66.6% (95%CI 66.1 to 67.1) to 70.7% (95%CI 70.2 to 71.2).
Table 4.
Proportion of remaining life spent without severe limitations (H-Ratio) in mental (MCS) and physical health (PCS) at different time-periods.
| MCS | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
|||||||||||||||||||
| 2002/04 |
2010/12 |
2016/18 |
2002/04 |
2010/12 |
2016/18 |
|||||||||||||||
| Age |
H-Ratio |
95%CI |
H-Ratio |
95%CI |
H-Ratio |
95%CI |
p |
H-Ratio |
95%CI |
H-Ratio |
95%CI |
H-Ratio |
95%CI |
p |
||||||
| lower | upper | lower | upper | lower | upper | lower | upper | lower | upper | lower | upper | |||||||||
| 30 | 84.47 | 83.79 | 85.15 | 84.99 | 84.26 | 85.71 | 88.21 | 87.57 | 88.85 | ** | 77.72 | 77.01 | 78.43 | 79.82 | 79.07 | 80.57 | 83.45 | 82.76 | 84.14 | *** |
| 35 | 84.49 | 83.84 | 85.13 | 85.02 | 84.34 | 85.70 | 88.31 | 87.70 | 88.93 | * | 77.91 | 77.22 | 78.59 | 79.98 | 79.28 | 80.69 | 83.46 | 82.79 | 84.12 | *** |
| 40 | 84.52 | 83.89 | 85.14 | 85.21 | 84.58 | 85.83 | 88.53 | 87.94 | 89.12 | * | 78.31 | 77.65 | 78.98 | 79.93 | 79.26 | 80.59 | 83.42 | 82.77 | 84.07 | *** |
| 45 | 84.49 | 83.88 | 85.09 | 85.46 | 84.87 | 86.05 | 88.69 | 88.12 | 89.26 | * | 78.63 | 77.99 | 79.28 | 79.96 | 79.32 | 80.60 | 83.84 | 83.21 | 84.48 | ** |
| 50 | 84.79 | 84.21 | 85.37 | 85.98 | 85.42 | 86.55 | 89.02 | 88.47 | 89.57 | * | 78.66 | 78.03 | 79.29 | 80.09 | 79.47 | 80.70 | 84.03 | 83.42 | 84.65 | ** |
| 55 | 85.28 | 84.72 | 85.84 | 85.92 | 85.39 | 86.46 | 89.32 | 88.79 | 89.85 | ns | 78.51 | 77.90 | 79.12 | 81.05 | 80.46 | 81.65 | 84.48 | 83.88 | 85.08 | ** |
| 60 | 84.86 | 84.32 | 85.40 | 86.59 | 86.08 | 87.10 | 89.79 | 89.28 | 90.30 | ns | 77.90 | 77.33 | 78.48 | 80.99 | 80.42 | 81.56 | 84.87 | 84.28 | 85.45 | ** |
| 65 | 84.55 | 84.02 | 85.09 | 86.38 | 85.89 | 86.87 | 90.55 | 90.06 | 91.04 | ns | 77.08 | 76.53 | 77.64 | 80.51 | 79.96 | 81.05 | 85.15 | 84.58 | 85.72 | ** |
| 70 | 82.64 | 82.10 | 83.19 | 85.19 | 84.72 | 85.66 | 90.40 | 89.92 | 90.88 | * | 75.02 | 74.48 | 75.56 | 79.40 | 78.88 | 79.92 | 84.51 | 83.96 | 85.06 | ** |
| 75 | 80.12 | 79.55 | 80.69 | 83.56 | 83.08 | 84.04 | 89.03 | 88.57 | 89.50 | ns | 73.00 | 72.48 | 73.51 | 77.46 | 76.95 | 77.98 | 83.03 | 82.51 | 83.56 | * |
| 80 | 76.93 | 76.30 | 77.55 | 82.55 | 82.04 | 83.06 | 87.85 | 87.36 | 88.34 | ns | 70.42 | 69.91 | 70.94 | 73.63 | 73.12 | 74.14 | 82.55 | 82.02 | 83.07 | * |
| 85 | 68.87 | 68.11 | 69.63 | 78.62 | 78.02 | 79.22 | 87.10 | 86.54 | 87.65 | ns | 64.25 | 63.69 | 64.81 | 74.18 | 73.64 | 74.72 | 81.19 | 80.64 | 81.75 | ns |
| 90+ |
61.21 |
60.25 |
62.18 |
83.18 |
82.39 |
83.98 |
86.34 |
85.59 |
87.09 |
ns |
57.06 |
56.45 |
57.67 |
69.64 |
68.95 |
70.32 |
81.85 |
81.21 |
82.49 |
ns |
| PCS | ||||||||||||||||||||
| Men | Women | |||||||||||||||||||
| 2002/04 | 2010/12 | 2016/18 | 2002/04 | 2010/12 | 2016/18 | |||||||||||||||
| Age | H-Ratio | 95%CI | H-Ratio | 95%CI | H-Ratio | 95%CI | p | H-Ratio | 95%CI | H-Ratio | 95%CI | H-Ratio | 95%CI | p | ||||||
| lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
lower |
upper |
|||||||||
| 30 | 77.62 | 76.99 | 78.25 | 77.66 | 76.97 | 78.36 | 78.90 | 78.31 | 79.49 | ns | 71.09 | 70.45 | 71.73 | 71.91 | 71.23 | 72.60 | 72.12 | 71.52 | 72.72 | ns |
| 35 | 75.51 | 74.92 | 76.09 | 75.62 | 74.99 | 76.25 | 77.06 | 76.50 | 77.62 | ns | 68.60 | 68.00 | 69.20 | 69.53 | 68.90 | 70.16 | 70.16 | 69.59 | 70.73 | ns |
| 40 | 72.90 | 72.34 | 73.45 | 73.11 | 72.54 | 73.68 | 74.94 | 74.42 | 75.47 | ns | 65.81 | 65.24 | 66.39 | 66.82 | 66.24 | 67.40 | 67.82 | 67.27 | 68.37 | ns |
| 45 | 69.87 | 69.35 | 70.40 | 70.58 | 70.06 | 71.10 | 72.82 | 72.32 | 73.32 | ns | 62.89 | 62.35 | 63.44 | 63.96 | 63.41 | 64.50 | 65.29 | 64.77 | 65.81 | ns |
| 50 | 66.57 | 66.07 | 67.07 | 67.66 | 67.18 | 68.15 | 70.71 | 70.24 | 71.19 | * | 59.49 | 58.97 | 60.01 | 60.87 | 60.36 | 61.38 | 62.67 | 62.17 | 63.17 | * |
| 55 | 63.30 | 62.83 | 63.77 | 64.44 | 63.99 | 64.89 | 68.32 | 67.87 | 68.77 | ** | 55.58 | 55.09 | 56.07 | 57.76 | 57.28 | 58.24 | 59.78 | 59.30 | 60.26 | * |
| 60 | 59.78 | 59.34 | 60.22 | 61.84 | 61.42 | 62.25 | 65.60 | 65.17 | 66.02 | ** | 51.49 | 51.04 | 51.94 | 54.68 | 54.23 | 55.13 | 56.96 | 56.50 | 57.42 | ** |
| 65 | 57.02 | 56.59 | 57.45 | 59.66 | 59.27 | 60.05 | 64.46 | 64.06 | 64.87 | ** | 47.12 | 46.70 | 47.54 | 51.12 | 50.70 | 51.53 | 54.00 | 53.57 | 54.43 | ** |
| 70 | 52.31 | 51.89 | 52.74 | 55.03 | 54.67 | 55.39 | 62.14 | 61.75 | 62.53 | *** | 42.69 | 42.30 | 43.09 | 41.49 | 41.11 | 41.88 | 49.76 | 49.35 | 50.16 | ** |
| 75 | 48.78 | 48.35 | 49.22 | 49.68 | 49.33 | 50.04 | 56.69 | 56.33 | 57.05 | * | 37.66 | 37.29 | 38.02 | 41.07 | 40.71 | 41.44 | 44.90 | 44.53 | 45.28 | * |
| 80 | 41.72 | 41.26 | 42.18 | 43.90 | 43.54 | 44.26 | 49.95 | 49.59 | 50.31 | ns | 32.45 | 32.10 | 32.80 | 35.09 | 34.75 | 35.44 | 39.44 | 39.08 | 39.80 | ns |
| 85 | 36.82 | 36.27 | 37.38 | 33.81 | 33.43 | 34.20 | 45.46 | 45.06 | 45.86 | ns | 28.56 | 28.19 | 28.93 | 31.43 | 31.08 | 31.78 | 37.04 | 36.67 | 37.41 | ns |
| 90+ | 34.56 | 33.83 | 35.28 | 22.36 | 21.95 | 22.77 | 42.93 | 42.40 | 43.46 | ns | 22.67 | 22.28 | 23.05 | 29.73 | 29.28 | 30.18 | 30.13 | 29.74 | 30.52 | ns |
Notes: Health-Ratio = H-LE/LE = proportion of life spent without severe limitations in mental/physical health, 95%CI = confidence interval of 95%, p = significant change in H-Ratio between first (2002/4) and last time-point (2016/18): *p < 0.05, **p < 0.01, ***p < 0.001, ns = not significant (p > 0.05).
Thirdly, also life expectancy with severe limitation (UH-LE) decreased while predominantly failing to reach statistical significance (Supplementary Table 1). For instance, the absolute number of remaining years expected to be lived with severe mental limitations among men aged 50 years decreased from 4.3 years (95%CI 3.7 to 4.9) in 2002-04 to 3.3 years (95%CI 2.8 to 3.9) in 2016-18 while that of severe physical limitations decreased from 9.5 years (95%CI 9.0 to 10.0) to 8.8 years (95%CI 8.4 to 9.3). Among women of that age, severe mental and physical limitations decreased from 7.0 (95%CI 6.4 to 7.7) to 5.5 (95%CI 4.9 to 6.1) years and from 13.4 (95%CI 12.9 to 13.9) to 12.8 years (95%CI 12.3 to 13.3), respectively.
Discussion
Health trends are embedded in the socio-demographic and political context of a given country. Germany is one of the wealthiest countries in the world with a well-developed social security and pension system. At the same time, significant social disparities continue to exist in terms of a highly unequal distribution of income and wealth, poor prospects for low-skilled people in the labor market and growth in precarious employment (Lampert, Hoebel, & Kroll, 2019). In this study, we focused on life stage-specific trends in HRQOL in order to allow for the possibility that social and demographic change may have altered people's HRQOL differently depending on their stage in the life course and the specific living conditions associated therewith.
Previous studies revealed heterogeneous directions of self-rated health trends. For example, Audureau et al. reported evidence on worsening trends of HRQOL between 1995 and 2003 in France (Audureau et al., 2013). In a similar vein, Olfson et al. found a significant decline in average HRQOL ratings of US adults between 2001/2 and 2012/13 (Olfson et al., 2018) and for the same country Greaney et al. reported increasing trends in poor SRH between 2001 and 2016 (Greaney et al., 2019). In contrast, the results by Beltrán-Sánchez et al. indicate that not only the length of life but also the number of disability-free life years in older ages has the potential to increase in the US (Beltrán-Sánchez et al., 2015). Pointing into the same direction, Gheorghe et al. found for the Netherlands that quality-adjusted life expectancy increased for men and women between 2001 and 2011 while educational inequalities widened in that time (Gheorghe et al., 2016). Ambiguous health trends were also reported for Germany where Moor et al. reported stability of mental and physical HRQOL between 2002 and 2014 (Moor et al., 2018) whereas Ellert and Kurth observed increasing rates of HRQOL between 1998 and 2008/11 (Ellert & Kurth, 2013). In line with the latter finding, we found the physical as well as mental component of HRQOL to be improving between 2002 and 2018. As compared with men, the increase in MCS was somewhat stronger among women, leading to a moderate decrease in the gender health gap with respect to mental quality of life. The improvements in MCS and PCS were most visible after the years 2010/12 while before that, there were largely stable trends in HRQOL. It might be that the economic and financial crisis which peaked in 2008 meant that the positive trend did not start earlier.
Behind this overall health trend we found different temporal evolvements according to life stages. Since previous studies used different study designs including varying age composition of participants, this finding might partly explain the mixed results on health trends obtained so far. Our results indicate that improvements in HRQOL were more pronounced for ages beyond working age. The greatest improvements were seen in the life stage of young seniors aged 65–79 years where not only severe limitations in PCS decreased but also the norm values above average significantly increased. In contrast, the number of severe limitations in PCS was on the rise for both genders for the life-stage of ‘middle working age’ (30–49 years) while they largely remained constant for women and men of later working life (50–64 years). With respect to MCS significant improvements were found for all ages but here, too, the improvements were stronger for ages beyond working age.
This key finding of health improvements in older ages but stable or even worsening trends in younger ages has already been reported before. For example, in a recent study (Sperlich et al., 2019), the largest increase in rates of good SRH was found just before and after official retirement age. This finding is consistent with another German study conducted by Wolff et al. indicating that the rise in functional health between 2008 and 2014 was restricted to ages above 65 years while in younger individuals the contrary pattern of a functional health decline was observed (Wolff et al., 2017). A recent study from France came to similar results, demonstrating that between 1995 and 2016 HRQOL substantially decreased among men aged 45–54 years while an overall improvement for both genders was noted in the age group 65–84 years (Clause-Verdreau et al., 2019). Finally, increasing trends of poor SRH among young adults (21–39 years) but decreasing rates among older adults (65+ years) were also reported in a recent US study (Greaney et al., 2019).
Explanatory approaches for different health trends according to life stage
The pattern of health improvement foremostly for adults over 64 years of age might be open to different explanations. First, working conditions might act as a barrier against positive health trends among the working population. In Germany, the official retirement age for men and women today is 65 years and most people under that age are still working (Destatis, 2020). Evidence suggests that working conditions in Germany became harder in the last decades due to increasing mental and physical stress placed on employees (Franke & Wetzel, 2017). This development might be one reason for the less beneficial health trends observed in the life stages of middle and later working life. In addition, it could be that the economic and financial crisis in 2008 had a more harmful effect on HRQOL among the working population as compared to those who are retired. It could be assumed that the crisis and the related risk of unemployment and economic uncertainty had a stronger impact on those still working. Supporting this assumption, we found among young seniors no inflection point with significant increases in HRQOL only after 2010/12 as this was the case for the working population. Instead, we found a gradual increase in HRQOL over the entire observation period that might partly explain why young seniors overall benefited the most. Similar results were obtained in a previous study where predicted probabilities of good self-rated health declined between the periods 2000/04 and 2005/09 for the working population while they increased among those who are retired (Sperlich et al., 2019).
In addition, significant health improvements among the elderly could be attributed to medical progress in the prevention and treatment of diseases that might be particularly relevant for advanced age where chronic conditions become more important. One might assume that similar health benefits will occur for the current working population when they reach retirement age. However, this assumption is based on the premise that all conditions related to health remained stable over time. There are good reasons to doubt this assumption. Not only psychosocial strain like work-related burden (Franke & Wetzel, 2017) but also health-related behaviors have changed considerably over the past decades. In this context, the rise in obesity might be particularly troubling given its strong impact on a wide range of morbidities such as diabetes and coronary heart disease that are associated with high rates of disability (Nordic Burden of Disease, 2019). Sturm et al. have already predicted that rising obesity rates could wipe out the progress in health that has been made before (Sturm, Ringel, & Andreyeva, 2004). In order to establish the causes of health trends and to estimate future developments, attention should be likewise directed to other material, psychosocial and behavioral factors determining health (Moor, Spallek, & Richter, 2017). Particular attention should be paid to the further development of social inequality and spatial disparities, e.g. between East and West Germany. As our findings indicate diverging health trends according to age, a life stage specific approach should guide further research in this field.
Changes in healthy life expectancy (H-LE)
We found LE as well as H-LE improving for both genders while at the same time LE with severe limitation (UH-LE) decreased. Although the decrease in UH-LE were not statistically significant for most ages, these findings are speaking in favor of absolute compression of morbidity (Howse, 2006). Hence, our findings add evidence for a positive health scenario indicating that not only quantity of life but also quality of life improved over time. However, the estimates obtained by the Sullivan method are based on period life tables using synthetic cohorts instead of real cohorts. In this approach, H-LE at a given age is defined as the average number of years a person would live under the condition that he or she experienced the age-specific morbidity and mortality rates for that time period. For instance, it is assumed that a today 30 year old person would experience the same mortality and morbidity rates at age 70 as a today 70 year old person. Such predictions are subject to many uncertainties, in particular given the less favorable health trends that were found in younger age-groups.
Limitations
This study has some limitations worth noting. Although sampling weights were used, the existence of sampling bias cannot be completely ruled out since a full match of the official population statistics cannot be taken for granted. Selection bias might also be due to the exclusion of the institutionalized population as well as persons who could not participate in the survey for health reasons. Therefore, we cannot exclude that H-LE is overestimated in our study. However, there is no reason to assume that the proportion of these people substantially changed over time. Hence, the time trends reported should not be affected by this source of bias.
Conclusions
We found evidence for decreasing rates of severe limitations in mental and physical HRQOL between 2002 and 2018 when considering the entire study population. Healthy life expectancy increased while lifetime in severe morbidity decreased, supporting the hypothesis of absolute compression of morbidity. However, health trends were not consistent across life stages, pointing to less improvements or even worsening trends in younger ages. Given these findings, it remains open whether the positive health trend will persist in the future.
Author statement
Marie Kristin Klar: Conceptualization, Methodology, Formal analysis, Writing-Original draft preparation, Stefanie Sperlich: Conceptualization, Methodology, Formal analysis, Writing-Original draft preparation, Writing- Reviewing and Editing, Supervision. Batoul Safieddine: Writing- Reviewing and Editing, Fabian Tetzlaff: Writing- Reviewing and Editing, Juliane Tetzlaff: Writing- Reviewing and Editing, Siegfried Geyer: Writing- Reviewing and Editing, Funding acquisition.
Declaration of competing interest
All authors declared that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100758.
Contributor Information
Marie Kristin Klar, Email: marie-k.klar@gmx.de.
Siegfried Geyer, Email: Geyer.Siegfried@mh-hannover.de.
Batoul Safieddine, Email: Safieddine.Batoul@mh-hannover.de.
Fabian Tetzlaff, Email: Tetzlaff.Fabian@mh-hannover.de.
Juliane Tetzlaff, Email: Tetzlaff.Juliane@mh-hannover.de.
Stefanie Sperlich, Email: Sperlich.Stefanie@mh-hannover.de.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Audureau E., Rican S., Coste J. Worsening trends and increasing disparities in health-related quality of life: Evidence from two French population-based cross-sectional surveys, 1995–2003. Quality of Life Research. 2013;22(1):13–26. doi: 10.1007/s11136-012-0117-7. [DOI] [PubMed] [Google Scholar]
- Beltrán-Sánchez H., Soneji S., Crimmins E.M. Past, present, and future of healthy life expectancy. Cold Spring Harb Perspect Med. 2015;5(11) doi: 10.1101/cshperspect.a025957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clause-Verdreau A.C., Audureau É., Leplège A., Coste J. Contrasted trends in health-related quality of life across gender, age categories and work status in France, 1995-2016: Repeated population-based cross-sectional surveys using the SF-36. Journal of Epidemiology & Community Health. 2019;73(1):65–72. doi: 10.1136/jech-2018-210941. [DOI] [PubMed] [Google Scholar]
- Destatis . 2019. Sterbetafeln 2016/2018. Ergebnisse aus der laufenden Berechnung von Periodensterbetafeln für Deutschland und die Bundesländer. [Google Scholar]
- Destatis Erwerbstätige und Erwerbstätigenquote1 nach Geschlecht und Alter 2009 und 2019. Ergebnis des Mikrozensus. 2020;2020 25.10.2020. [Google Scholar]
- Ellert U., Kurth B.-M. Vol. 56. Robert Koch-Institut; 2013. (Gesundheitsbezogene Lebensqualität bei Erwachsenen in Deutschland). [DOI] [PubMed] [Google Scholar]
- Franke J., Wetzel M. Länger zufrieden arbeiten? Qualität und ausgestaltung von Erwerbstätigkeit in der zweiten lebenshälfte. In: Mahne K., Wolff J.K., Simonson J., Tesch-Römer C., editors. Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS) Springer Fachmedien Wiesbaden; Wiesbaden: 2017. pp. 47–63. [Google Scholar]
- Frick J., Schupp J., Wagner G. The German socio-economic panel study (SOEP)—scope, evolution and enhancements. Schmollers Jahrbuch : Journal of Applied Social Science Studies/Zeitschrift für Wirtschafts- und Sozialwissenschaften. 2007;127:139–169. doi: 10.2139/ssrn.1028709. [DOI] [Google Scholar]
- Fries J.F. Aging, natural death, and the compression of morbidity. New England Journal of Medicine. 1980;303(3):130–135. doi: 10.1056/nejm198007173030304. [DOI] [PubMed] [Google Scholar]
- Galenkamp H., Braam A.W., Huisman M., Deeg D.J. Seventeen-year time trend in poor self-rated health in older adults: Changing contributions of chronic diseases and disability. The European Journal of Public Health. 2013;23(3):511–517. doi: 10.1093/eurpub/cks031. [DOI] [PubMed] [Google Scholar]
- Gheorghe M., Wubulihasimu P., Peters F., Nusselder W., Van Baal P.H. Health inequalities in The Netherlands: Trends in quality-adjusted life expectancy (QALE) by educational level. The European Journal of Public Health. 2016;26(5):794–799. doi: 10.1093/eurpub/ckw043. [DOI] [PubMed] [Google Scholar]
- Goebel J., Grabka M.M., Liebig S., Kroh M., Richter D., Schröder C. The German socio-economic panel (SOEP) 2019. 239(2), 345. [DOI]
- Greaney M.L., Cohen S.A., Blissmer B.J., Earp J.E., Xu F. Age-specific trends in health-related quality of life among US adults: Findings from national health and nutrition examination survey, 2001-2016. Quality of Life Research. 2019;28(12):3249–3257. doi: 10.1007/s11136-019-02280-z. [DOI] [PubMed] [Google Scholar]
- Gruenberg E.M. The failures of success. The Milbank Quarterly. 2005;83(4):779–800. doi: 10.1111/j.1468-0009.2005.00400.x. 1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G.H., Feeny D.H., Patrick D.L. Measuring health-related quality of life. Annals of Internal Medicine. 1993;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- Hanibuchi T., Nakaya T., Honjo K. Trends in socioeconomic inequalities in self-rated health, smoking, and physical activity of Japanese adults from 2000 to 2010. SSM Popul Health. 2016;2:662–673. doi: 10.1016/j.ssmph.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy C.H., Moriarty D.G., Zack M.M., Scherr P.A., Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Reports. 1994;109(5):665–672. [PMC free article] [PubMed] [Google Scholar]
- Howse K. 2006. Increasing life expectancy and the compression of morbidity: A critical review of the debate. [Google Scholar]
- Jagger C. 3rd ed. 2007. Health expectancy calculation by the sullivan method: A practical guide.https://webgate.ec.europa.eu/chafea_pdb/assets/files/pdb/2006109/2006109_d5sullivan_guide_final_jun2007.pdf Retrieved from. [Google Scholar]
- Jakovljevic M.B., Milovanovic O. Growing burden of non-communicable diseases in the emerging health markets: The case of BRICS. Frontiers in Public Health. 2015;3(65) doi: 10.3389/fpubh.2015.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson S.E., Midlöv P., Sundquist J., Sundquist K., Calling S. Longitudinal trends in good self-rated health: Effects of age and birth cohort in a 25-year follow-up study in Sweden. International Journal of Public Health. 2015;60(3):363–373. doi: 10.1007/s00038-015-0658-y. [DOI] [PubMed] [Google Scholar]
- Lampert T., Hoebel J., Kroll L.E. Vol. 4. 2019. pp. 3–14. (Social differences in mortality and life expectancy in Germany: Current situation and trends). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macias C., Gold P.B., Öngür D., Cohen B.M., Panch T. Are single-item global ratings useful for assessing health status? Journal of Clinical Psychology in Medical Settings. 2015;22(4):251–264. doi: 10.1007/s10880-015-9436-5. [DOI] [PubMed] [Google Scholar]
- Mairey I., Bjerregaard P., Brønnum-Hansen H. Gender difference in health expectancy trends in Greenland. Scandinavian Journal of Public Health. 2014;42(8):751–758. doi: 10.1177/1403494814550174. [DOI] [PubMed] [Google Scholar]
- Manton K.G. Changing concepts of morbidity and mortality in the elderly population. Milbank Memorial Fund Quarterly - Health & Society. 1982;60(2):183–244. [PubMed] [Google Scholar]
- Moor I., Günther S., Knöchelmann A., Hoebel J., Pförtner T.K., Lampert T. Educational inequalities in subjective health in Germany from 1994 to 2014: A trend analysis using the German socio-economic panel study (GSOEP) BMJ Open. 2018;8(6) doi: 10.1136/bmjopen-2017-019755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor I., Spallek J., Richter M. Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioural factors. Journal of Epidemiology & Community Health. 2017;71(6):565–575. doi: 10.1136/jech-2016-207589. [DOI] [PubMed] [Google Scholar]
- Nordic Burden of Disease C. Life expectancy and disease burden in the nordic countries: Results from the global burden of diseases, injuries, and risk factors study 2017. The lancet. Public Health. 2019;4(12):e658–e669. doi: 10.1016/s2468-2667(19)30224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nübling M., Andersen H., Mühlbacher A., Schupp J., Wagner G. Computation of standard values for physical and mental health scale scores using the SOEP version of SF12v2. Schmollers Jahrbuch : Journal of Applied Social Science Studies/Zeitschrift für Wirtschafts- und Sozialwissenschaften. 2007;127(1):171–182. [Google Scholar]
- Olfson M., Wall M., Liu S.M., Schoenbaum M., Blanco C. Declining health-related quality of life in the U.S. American Journal of Preventive Medicine. 2018;54(3):325–333. doi: 10.1016/j.amepre.2017.11.012. [DOI] [PubMed] [Google Scholar]
- Põld M., Pärna K., Ringmets I. Trends in self-rated health and association with socioeconomic position in Estonia: Data from cross-sectional studies in 1996-2014. International Journal for Equity in Health. 2016;15(1):200. doi: 10.1186/s12939-016-0491-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperlich S., Tetzlaff J., Geyer S. Trends in good self-rated health in Germany between 1995 and 2014: Do age and gender matter? International Journal of Public Health. 2019;64(6):921–933. doi: 10.1007/s00038-019-01235-y. [DOI] [PubMed] [Google Scholar]
- Sturm R., Ringel J.S., Andreyeva T. Increasing obesity rates and disability trends. Health Affairs. 2004;23(2):199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- Sullivan D.F. A single index of mortality and morbidity. HSMHA Health Reports. 1971;86(4):347–354. doi: 10.2307/4594169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachte F., Sperlich S., Geyer S. [Compression or expansion of morbidity? Development of health among the older population] Zeitschrift für Gerontologie und Geriatrie. 2015;48(3):255–262. doi: 10.1007/s00391-014-0644-7. [DOI] [PubMed] [Google Scholar]
- Wolff J.K., Nowossadeck S., Spuling S.M. Altern nachfolgende Kohorten gesünder? Selbstberichtete Erkrankungen und funktionale Gesundheit im Kohortenvergleich. In: Mahne K., Wolff J.K., Simonson J., Tesch-Römer C., editors. Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS) Springer Fachmedien Wiesbaden; Wiesbaden: 2017. pp. 125–138. [Google Scholar]
- Zack M.M., Moriarty D.G., Stroup D.F., Ford E.S., Mokdad A.H. Worsening trends in adult health-related quality of life and self-rated health-United States, 1993-2001. Public Health Reports. 2004;119(5):493–505. doi: 10.1016/j.phr.2004.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.