ABSTRACT
Phase angle has been suggested as a useful, noninvasive, and objective index to evaluate the nutritional status of older people. However, there are no studies analyzing the relationship between nutritional status and phase angle in older patients, according to sex. The aim of this study was to clarify the relationship between phase angle and malnutrition, and to calculate cut-off points of malnutrition with phase angle in older inpatients, according to sex. This study was a retrospective cross-sectional study. Participants were older inpatients of a rehabilitation unit, and data within 1 week of hospitalization were collected from the medical records. We collected data of demographics, phase angle, and the Geriatric Nutritional Risk Index. Phase angle was measured with InBody S10. To confirm whether phase angle is an important factor in predicting malnutrition, we conducted binary logistic regression analysis. In addition, to determine the cut-off points of malnutrition in older inpatients, we used the receiver operator characteristic (ROC) curve. Participants included 59 men (mean age 76.5 years) and 101 women (mean age 78.8 years). As a result of statistical analysis, phase angle was an important factor related to malnutrition in both male and female inpatients. Our findings showed that cut-off points of 4.03 degrees (sensitivity; 87.0%, specificity; 75.9%) in male patients and 3.65 degrees (sensitivity; 78.6%, specificity; 60.5%) in female patients could be used to predict malnutrition. The results of this study suggest that phase angle may be useful as an indicator to predict the nutritional status of older inpatients.
Key Words: older adults, inpatients, malnutrition, nutrition assessment
INTRODUCTION
Malnutrition in older adults is associated with a decline in activities of daily living1 and quality of life2 and an increased mortality rate.3 In addition, malnutrition affects the length of hospitalization of older patients.4 Therefore, it is particularly important to evaluate the nutritional status of older inpatients.
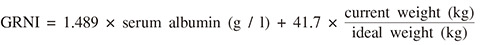
The Geriatric Nutritional Risk Index (GNRI) is a useful objective method to evaluate the nutritional status of older people.5 The GNRI is calculated from height, weight, and serum albumin, and malnutrition is suspected with a value 98 or less. However, blood tests to investigate serum albumin are invasive, which may place a burden on older patients. In addition, the GNRI is sometimes difficult to promptly assess unless the facility is equipped with an analyzer. Therefore, calculation of the GNRI is considered to be less versatile when it is used to investigate daily changes.
Noninvasive evaluation methods of nutrition status include the Malnutrition Screening Tool,6 Malnutrition Universal Screening Tool,7 and Nutritional Risk Screening – 2002.8 Although these tools are more versatile than more invasive evaluation methods, there is a possibility of subjectivity in patients’ responses; furthermore, it may be difficult for patients with declining cognitive function to provide quick and accurate responses so as to calculate index values.
As a noninvasive evaluation method and index of objective nutritional status, phase angle (PA) measured via bioelectrical impedance analysis has recently attracted attention.9-11 The PA is the arctangent value calculated from resistance and reactance obtained in bioelectrical impedance analysis and represents cellularity, integrity of cell membranes, and cell function.12 Generally, the larger the PA value, the better the patient’s condition.
PA is associated with muscle strength,13-15 muscle quality,16 functional capacity,16 inflammatory and oxidative stress biomarkers,17 severity of musculoskeletal and respiratory diseases18 and quality of life19 in older adults. It has also been suggested to be useful in the diagnosis of sarcopenia,20 osteoporosis,21 and prediction of mortality.19,22-24 Among these, Lukaski et al22 reported that PA is useful for evaluating the nutritional status of older adults.
As a noninvasive and objective method of evaluation, PA is considered a highly versatile and objective indicator for evaluating the nutritional status of older adults. However, few studies to date have been conducted to evaluate nutritional status using PA. One study calculated cut-off points for use of PA as a screening tool for nutritional disorders in older inpatients,10 that study did not use objective methods, such as the GNRI, to assess malnutrition. In addition, PA has been suggested to show sex differences,25 but no analyses according to sex have been carried out. Kyle et al9 investigated the relationship between PA and serum albumin and calculated the cut-off of malnutrition for PA. The PA is reported to be affected by age, but that study was not limited to older participants. Therefore, the aim of the present study was to clarify the effectiveness of malnutrition assessed using PA and the GNRI, and to calculate cut-off points of malnutrition for PA in older inpatients, according to sex.
MATERIALS AND METHODS
Setting, Study Design and Participants
This study was conducted at a 50-bed rehabilitation unit in Kasugai City, Aichi Prefecture, Japan. This was a retrospective cross-sectional study. Using the medical records, we collected inpatient data evaluated within 1 week of hospitalization in the rehabilitation unit.
Study participants were inpatients hospitalized between August 2017 and March 2019. Included patients were those age 65 years or older who were admitted to the rehabilitation unit and had no missing data. Because PA is affected by age,25 we excluded inpatients over 85 years of age.26 We also excluded inpatients in whom it was impossible to obtain measurements using bioelectrical impedance analysis.
Measurements
We collected data of demographics, PA, and the GNRI. Demographic data included age, sex, diagnosis at admission, period from onset to admission, and the motor Functional Independence Measure score. In addition, we recorded the Skeletal Muscle Index. The Skeletal Muscle Index was calculated by dividing upper and lower limb muscle mass (obtained with the InBody S10 [In Body, Koto-ku, Tokyo, Japan]), by the square of height. Based on the resistance and reactance obtained when measuring muscle mass with the InBody S10, PA was calculated using the following formula27:
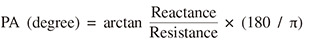
PA was calculated from measurement values taken from the right upper limb, right lower limbs, and trunk. To eliminate the effects of paralysis and surgical operation when measuring PA in patients with stroke and hip fractures, the PA was calculated using measurement values from the upper and lower limbs of the unaffected side, and from the trunk. The measurement using InBody S10 were taken with the patient in the supine position before rehabilitation exercises. It has been reported that the InBody S10 has high accuracy in measuring the SMI and PA, according to studies including older adults.28,29 In addition, it has been shown that PA obtained by bioelectrical impedance analysis has low within-day and between-day fluctuation.27
The GNRI was calculated using participants’ height, weight, and serum albumin.5 Based on previous research, in this study, we defined a GNRI of 98 or less as malnutrition.5 The GNRI was calculated using the following formula5:
Ideal weight for men = height (cm) – 100 – [(height (cm) – 150) / 4]
Ideal weight for women = height (cm) – 100 – [(height (cm) – 150) / 2.5]
Statistical Analysis
We performed the analysis based on sex. Participants characteristics are shown using descriptive statistics. To confirm whether PA is an important factor that can predict malnutrition, we conducted binary logistic regression analysis using a crude model and an adjusted model, in the presence or absence of malnutrition (as defined by the GNRI) as a dependent variable. Prior to performing binary logistic regression in the adjustment model, we conducted a correlation analysis between the collected data and GNRI; variables that had significant correlation with PA were used in the analysis. The Hosmer-Lemeshow test was performed to assess goodness of fit in logistic regression analysis, and the model was considered a good fit with p > 0.05.
To determine the PA cut-off points of malnutrition, defined as GNRI 98 or less in older inpatients, we used the receiver operator characteristic curve and calculated the area under curve. The cut-off was defined as the point where the sensitivity and specificity were highest. We used IPM SPSS Statistics Version 24.0 (IBM Japan, Tokyo, Japan) for all analyses. A p-value of < 0.05 was considered statistically significant.
Ethical Considerations
We began the study after receiving approval of the Research Ethics Committee of the Tokai Memorial Hospital (Approval number: 30–10) and Seijoh University (Approval number: 2018C0051). Information on the use of medical record information was posted on the Tokai Memorial Hospital website, and all participants were offered the opportunity to refuse the use of their information. It was determined that informed consent was not necessary as deidentified secondary data were used in this study.
RESULTS
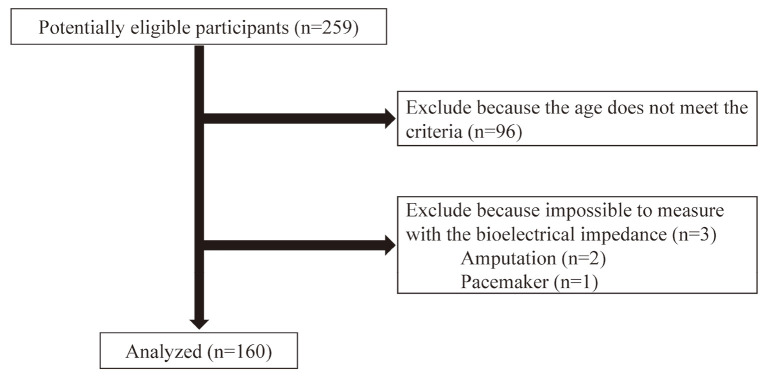
During the study period, 259 patients were admitted to the hospital, among which 160 patients were included in the present analysis (59 male and 101 female patients) (Figure 1). Participants characteristics are shown in Table 1. The average age of participants was 78.0 ± 5.3 years, range 65–84 years (male 76.5 ± 5.4 years, range 65–84 years; female 78.8 ± 5.2 years, range 65–84 years). The average PA was 3.9 ± 0.9 degrees, range 2.0–8.3 (male 4.1 ± 1.0, range 2.2–8.3, female 3.8 ± 0.9, range 2.0–7.0), and the average GNRI was 95.4 ± 10.2, range 67.2–119.7 (male 95.3 ± 10.3, range 76.2–119.0, female 95.5 ± 10.1, range 67.2–119.7). The prevalence of malnutrition was 55.9% for male inpatients and 60.4% for female ones. Among the collected data, the items that had significant correlation with GNRI were the motor Functional Independence Measure score (males; r = 0.46, p = 0.001, females; r = 0.29, p = 0.006) and the Skeletal Muscle Index (males; r = 0.61, p < 0.001, females; r = 0.48, p < 0.001) in both sexes. Therefore, these variables were used in the adjusted logistic regression analysis model.
Fig. 1.
Study flow chart
Table 1.
Participant characteristics
| All (160) | Male (59) | Female (101) | ||
| Age (years) | mean (SD) range | 78.0 (5.3)
65–84 |
76.5 (5.4)
65–84 |
78.8 (5.2)
65–84 |
| Period from onset to admission (days) | mean (SD) range | 33.1 (14.1)
2–61 |
33.9 (14.6)
2–61 |
32.6 (13.8)
5–61 |
| Phase angle (°) | mean (SD) range | 3.9 (0.9)
2.0–8.3 |
4.1 (1.0)
2.2–8.3 |
3.8 (0.9)
2.0–7.0 |
| Geriatric Nutritional Risk Index | mean (SD) range | 95.4 (10.2)
67.2–119.7 |
95.3 (10.3)
76.2–119.0 |
95.5 (10.1)
67.2–119.7 |
| mFIM score | mean (SD) range | 49.9 (19.7)
13–87 |
47.4 (21.3)
13–87 |
52.2 (18.1)
13–82 |
| SMI (kg/m2) | mean (SD) range | 5.7 (1.3)
2.2–10.2 |
6.5 (1.3)
4.3–10.2 |
5.2 (1.0)
2.2–7.8 |
| Admission diagnosis, n (%) | ||||
| Hemorrhagic stroke | 16 (10.0) | 12 (20.3) | 4 (4.0) | |
| Ischemic stroke | 22 (13.8) | 13 (22.0) | 9 (8.9) | |
| Hip fracture | 57 (35.6) | 16 (27.1) | 41 (40.6) | |
| Vertebral compression fracture | 32 (20.0) | 8 (13.6) | 24 (23.8) | |
| Pelvic fracture | 5 (3.1) | 1 (1.7) | 4 (4.0) | |
| Spinal canal stenosis | 6 (3.8) | 2 (3.4) | 4 (4.0) | |
| Spinal cord injury | 6 (3.8) | 3 (5.1) | 3 (3.0) | |
| Other | 16 (10.0) | 4 (6.8) | 12 (11.9) | |
| Prevalence of malnutrition*, n (%) | 94 (58.8) | 33 (55.9) | 61 (60.4) | |
mFIM: motor Functional Independence Measure
SD: Standard Deviation
SMI: Skeletal Muscle Index.
* Malnutrition was defined as Geriatric Nutritional Risk Index 98 or less.
No multicollinearity between independent variables was observed for either sex. PA was found to be an important factor in predicting malnutrition in both male inpatients (crude model: B = 2.42, odds ratio (OR) = 11.20, 95% confidence interval (CI) = 2.99–41.95, p < 0.001, Hosmer-Lemeshow test p = 0.78; adjusted model: B = 2.51, OR = 12.31, 95% CI = 2.36–64.07, p = 0.003, Hosmer-Lemeshow test p = 0.95) and female inpatients (crude model: B = 1.34, OR = 3.80, 95% CI = 1.79–8.08, p = 0.001, Hosmer-Lemeshow test p = 0.31; adjusted model: B = 1.02, OR = 2.79, 95% CI = 1.23–6.29, p = 0.014, Hosmer-Lemeshow test p = 0.61) (Table 2).
Table 2.
Binary logistic regression analysis for malnutrition with phase angle as an independent variable
| Male | Female | |||||
| Model | B | OR (95% CI) | p-value | B | OR (95% CI) | p-value |
| Crude model | 2.42 | 11.20 (2.99–41.95) | <0.001 | 1.34 | 3.80 (1.79–8.08) | 0.001 |
| Adjusted model | 2.51 | 12.31 (2.36–64.07) | 0.003 | 1.02 | 2.79 (1.23–6.29) | 0.014 |
Crude model: males: p < 0.001, females: p < 0.001.
Hosmer-Lemeshow test; males: p = 0.783, females: p = 0.315.
Adjusted model: males: p < 0.001, females: p < 0.001.
Hosmer-Lemeshow test; males: p = 0.950, females: p = 0.613.
Adjusted model adjusted for motor Functional Independence Measure score and Skeletal Muscle Index in both male and female inpatients.
OR: odds ratio
CI: confidence interval
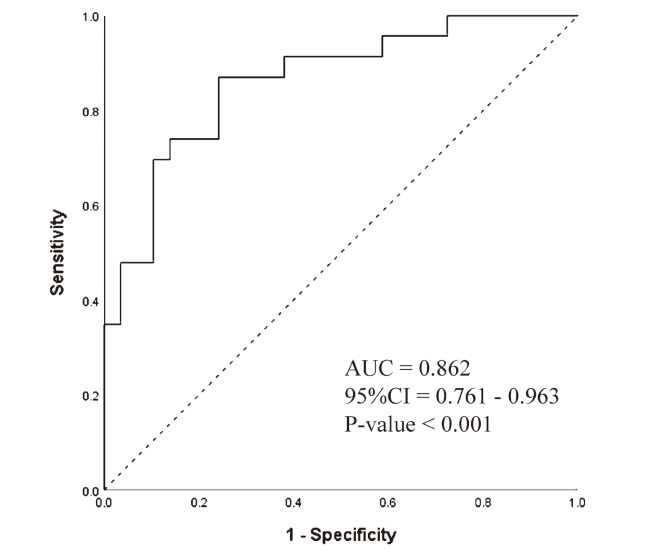
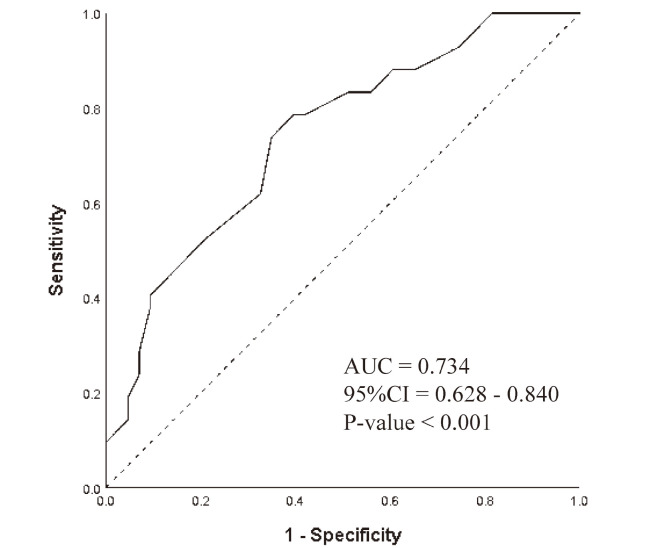
In the ROC analysis, male inpatients showed values of the area under curve = 0.86, 95% CI = 0.76–0.96, p < 0.001; for female inpatients, these values were the area under curve = 0.74, 95% CI = 0.64–0.85, p < 0.001. The cut-off points for suspected malnutrition using PA were 4.03 degrees (sensitivity; 87.0%, specificity; 75.9%) for male inpatients and 3.65 degrees (sensitivity; 78.6%, specificity; 60.5%) for female ones (Figures 2 and 3).
Fig. 2.
Receiver operator characteristic (ROC) curve of phase angle for malnutrition among male inpatients
AUC: Area under the ROC curve
CI: confidence interval.
Fig. 3.
Receiver operator characteristic (ROC) curve of phase angle for malnutrition among female inpatients
AUC: Area under the ROC curve
CI: confidence interval.
DISCUSSION
In this study, PA was found to be an important factor related to malnutrition in both male and female inpatients. In addition, our results showed cut-off points to predict malnutrition of 4.03 degrees in male inpatients and 3.65 degrees in female ones. Previous studies have reported that PA can predict nutritional status.9,10 However, PA has not previously been targeted for use in older patients and has not been analyzed according to sex. Therefore, in our study, we first examined the relationship between PA and nutritional status in older inpatients, according to sex. We found significant correlation between PA and malnutrition in both male and female inpatients. Although PA has been reported to show sex differences,25 the results of our study suggested that PA is associated with malnutrition in both male and female patients. As PA has been reported to be useful as an independent indicator for predicting malnutrition,10 even in older patients, PA may be an important factor that reflects malnutrition in both male and female inpatients. After confirming the association between PA and nutritional status in older inpatients, we determined the cut-off of PA to predict malnutrition among older inpatients according to sex. To our knowledge, this is the first verification of this cut-point.
Kyle et al9 reported that the cut-off value for malnutrition using PA is 5.0 degrees for male patients and 4.6 degrees for female ones. Varan et al10 reported a cut-off value of 4.7 degrees. In this study, the cut-point for malnutrition was 4.03 degrees for male inpatients and 3.65 degrees for female ones. Our study participants were limited to older inpatients, except for oldest-old patients, and were analyzed according to sex; these factors may account for our results, which differed from previously reported results. In addition, PA has been suggested to differ by ethnicity.30 There is a possibility that our results differed from those of previous studies because we included participants of different ethnicities.
Bioelectrical impedance analysis is a promising evaluation tool that is safe, does not burden the patient, and does not require specialized skills or experience in the examiner.31 As malnutrition affects various health-related outcomes, the results of our study demonstrated a method to easily assess malnutrition that would be useful to assist in the recovery of older hospitalized patients. Furthermore, the reliability of our results among older inpatients can be considered to be high because we compared the PA with the GNRI, which was developed to evaluate malnutrition in older people. In the future, bioelectrical impedance analysis should be confirmed as a useful method by longitudinally examining changes in malnutrition and PA.
The present study has several limitations. It has been suggested that PA decreases with severity of osteoporosis21 and musculoskeletal diseases.18 Many participants in this study were patients with fractures. Therefore, the study population may have included many patients with decreased bone density, which may affect the results. In addition, PA is associated with inflammation17: however, we had insufficient control regarding the period from onset, which may affect inflammation. It is recommended that some conditions, such as fasting, be met when conducting measurement using bioelectrical impedance analysis; in this study, the conditions before measurement could not be strictly controlled.32 By controlling these factors, malnutrition may be more accurately predicted.
CONCLUSION
The results of this study indicate that PA is an important factor for predicting malnutrition in older inpatients of both sexes, and that an appropriate cut-off for malnutrition is 4.03 degrees for male inpatients and 3.65 degrees for female ones.
ACKNOWLEDGMENTS
We thank Analisa Avila, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Abbreviations
- GNRI
Geriatric Nutritional Risk Index
- PA
phase angle
REFERENCES
- 1.Nishioka S, Wakabayashi H, Momosaki R. Nutritional status changes and activities of daily living after hip fracture in convalescent rehabilitation units: a retrospective observational cohort study from the Japan Rehabilitation Nutrition Database. J Acad Nutr Diet. 2018;118(7):1270–1276. doi: 10.1016/j.jand.2018.02.012. [DOI] [PubMed]
- 2.Damião R, Meneguci J, da Silva Santos Á, Matijasevich A, Menezes PR. Nutritional risk and quality of life in community-dwelling elderly: a cross-sectional study. J Nutr Health Aging. 2018;22(1):111–116. doi: 10.1007/s12603-017-0935-y. [DOI] [PubMed]
- 3.Naseer M, Forssell H, Fagerström C. Malnutrition, functional ability and mortality among older people aged ≥60 years: a 7-year longitudinal study. Eur J Clin Nutr. 2016;70(3):399–404. doi: 10.1038/ejcn.2015.196. [DOI] [PubMed]
- 4.Gärtner S, Kraft M, Krüger J, et al. Geriatric nutritional risk index correlates with length of hospital stay and inflammatory markers in older inpatients. Clin Nutr. 2017;36(4):1048–1053. doi: 10.1016/j.clnu.2016.06.019. [DOI] [PubMed]
- 5.Bouillanne O, Morineau G, Dupont C, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–783. doi: 10.1093/ajcn/82.4.777. [DOI] [PubMed]
- 6.Ferguson M, Capra S, Bauer J, Banks M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition. 1999;15(6):458–464. doi: 10.1016/s0899-9007(99)00084-2. [DOI] [PubMed]
- 7.Elia M. Screening for malnutrition: a multidisciplinary responsibility. Development and use of the ‘Malnutrition Universal Screening Tool’(‘MUST’) for adults. Redditch: Malnutrition Advisory Group, a Standing Committee of BAPEN. https://www.bapen.org.uk/pdfs/must/must-report.pdf.Published October 2012. Accessed January, 2020.
- 8.Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–421. doi: 10.1016/s0261-5614(03)00098-0. [DOI] [PubMed]
- 9.Kyle UG, Soundar EP, Genton L, Pichard C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Clin Nutr. 2012;31(6):875–881. doi: 10.1016/j.clnu.2012.04.002. [DOI] [PubMed]
- 10.Varan HD, Bolayir B, Kara O, et al. Phase angle assessment by bioelectrical impedance analysis and its predictive value for malnutrition risk in hospitalized geriatric patients. Aging Clin Exp Res. 2016;28(6):1121–1126. doi: 10.1007/s40520-015-0528-8. [DOI] [PubMed]
- 11.Slee A, Birch D, Stokoe D. Bioelectrical impedance vector analysis, phase-angle assessment and relationship with malnutrition risk in a cohort of frail older hospital patients in the United Kingdom. Nutrition. 2015;31(1):132–137. doi: 10.1016/j.nut.2014.06.002. [DOI] [PubMed]
- 12.Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin Nutr. 2012;31(6):854–861. doi: 10.1016/j.clnu.2012.05.008. [DOI] [PubMed]
- 13.Campa F. Silva AM, Toselli S. Changes in phase angle and handgrip strength induced by suspension training in older women. Int J Sports Med. 2018;39(6):442–449. doi: 10.1055/a-0574-3166. [DOI] [PubMed]
- 14.Ribeiro AS, Schoenfeld BJ, Souza MF, et al. Resistance training prescription with different load-management methods improves phase angle in older women. Eur J Sport Sci. 2017;17(7):913–921. doi: 10.1080/17461391.2017.1310932. [DOI] [PubMed]
- 15.Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB. Changes in phase angle and body composition induced by resistance training in older women. Eur J Clin Nutr. 2016;70(12):1408–1413. doi: 10.1038/ejcn.2016.124. [DOI] [PubMed]
- 16.Tomeleri CM, Cavalcante EF, Antunes M, et al. Phase angle is moderately associated with muscle quality and functional capacity, independent of age and body composition in older women. J Geriatr Phys Ther. 2017;42(4):281–286. doi: 10.1519/JPT.0000000000000161. [DOI] [PubMed]
- 17.Tomeleri CM, Cavaglieri CR, de Souza MF, et al. Phase angle is related with inflammatory and oxidative stress biomarkers in older women. Exp Gerontol. 2018;102:12–18. doi: 10.1016/j.exger.2017.11.019. [DOI] [PubMed]
- 18.Graf CE, Herrmann FR, Genton L. Relation of disease with standardized phase angle among older patients. J Nutr Health Aging. 2018;22(5):601–607. doi: 10.1007/s12603-018-1034-4. [DOI] [PubMed]
- 19.Norman K, Wirth R, Neubauer M, Eckardt R, Stobäus N. The bioimpedance phase angle predicts low muscle strength, impaired quality of life, and increased mortality in old patients with cancer. J Am Med Dir Assoc. 2015;16(2):173.e17–e22. doi: 10.1016/j.jamda.2014.10.024. [DOI] [PubMed]
- 20.Kilic MK, Kizilarslanoglu MC, Arik G, et al. Association of bioelectrical impedance analysis–derived phase angle and sarcopenia in older adults. Nutr Clin Pract. 2017;32(1):103–109. doi: 10.1177/0884533616664503. [DOI] [PubMed]
- 21.Tanaka S, Ando K, Kobayashi K, et al. A low phase angle measured with bioelectrical impedance analysis is associated with osteoporosis and is a risk factor for osteoporosis in community-dwelling people: the Yakumo study. Arch Osteoporos. 2018;13(1):39. doi: 10.1007/s11657-018-0450-8. [DOI] [PubMed]
- 22.Lukaski HC, Kyle UG, Kondrup J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: phase angle and impedance ratio. Curr Opin Clin Nutr Metab Care. 2017;20(5):330–339. doi: 10.1097/MCO.0000000000000387. [DOI] [PubMed]
- 23.Genton L, Norman K, Spoerri A, et al. Bioimpedance-derived phase angle and mortality among older people. Rejuvenation Res. 2017;20(2):118–124. doi: 10.1089/rej.2016.1879. [DOI] [PubMed]
- 24.Genton L, Herrmann FR, Spörri A, Graf CE. Association of mortality and phase angle measured by different bioelectrical impedance analysis (BIA) devices. Clin Nutr. 2018;37(3):1066–1069. doi: 10.1016/j.clnu.2017.03.023. [DOI] [PubMed]
- 25.Gonzalez MC, Barbosa-Silva TG, Bielemann RM, Gallagher D, Heymsfield SB. Phase angle and its determinants in healthy subjects: influence of body composition. Am J Clin Nutr. 2016;103(3):712–716. doi: 10.3945/ajcn.115.116772. [DOI] [PMC free article] [PubMed]
- 26.Hajek A, Brettschneider C, van den Bussche H, et al. Impact of falls on depressive symptoms among the oldest old: Results from the AgeQualiDe study. Int J Geriatr Psychiatry. 2018;33(10):1383–1388. doi: 10.1002/gps.4949. [DOI] [PubMed]
- 27.Bosy-Westphal A, Danielzik S, Dörhöfer RP, Later W, Wiese S, Müller MJ. Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN J Parenter Enteral Nutr. 2006;30(4):309–316. doi: 10.1177/0148607106030004309. [DOI] [PubMed]
- 28.Jayanama K, Putadechakun S, Srisuwarn P, et al. Evaluation of body composition in hemodialysis Thai patients: comparison between two models of bioelectrical impedance analyzer and dual-energy X-ray absorptiometry. J Nutr Metab. 2018;4537623. doi: 10.1155/2018/4537623. [DOI] [PMC free article] [PubMed]
- 29.Kim D, Sun JS, Lee YH, Lee JH, Hong J, Lee JM. Comparative assessment of skeletal muscle mass using computerized tomography and bioelectrical impedance analysis in critically ill patients. Clin Nutr. 2019;38(6):2747–2755. doi: 10.1016/j.clnu.2018.12.002. [DOI] [PubMed]
- 30.Piccoli A, Pillon L, Dumler F. Impedance vector distribution by sex, race, body mass index, and age in the United States: standard reference intervals as bivariate Z scores. Nutrition. 2002;18(2):153–167. doi: 10.1016/s0899-9007(01)00665-7. [DOI] [PubMed]
- 31.Player EL, Morris P, Thomas T, et al. Bioelectrical impedance analysis (BIA)-derived phase angle (PA) is a practical aid to nutritional assessment in hospital in-patients. Clin Nutr. 2019;38(4):1700–1706. doi: 10.1016/j.clnu.2018.08.003. [DOI] [PubMed]
- 32.Kyle UG, Bosaeus I, De Lorenzo AD, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430–1453. doi: 10.1016/j.clnu.2004.09.012. [DOI] [PubMed]