Abstract
Background
The role of glaucoma virtual clinics has developed to help meet demand for capacity within busy glaucoma services. There is limited research of patient and clinician experiences and perceptions of these clinics and the aim of this study is to provide further information to help improve patient experience and guide service delivery.
Methods
A mixed methods research design was employed comprising of a patient satisfaction survey, and patient and clinician interviews. Consultant ophthalmologists were recruited from throughout the UK, and patients and data gathering clinical staff recruited from the Manchester Royal Eye Hospital and Bristol Eye Hospital.
Results
We received a total of 148 patient satisfaction questionnaires with an overall response rate of 55.4%. Most respondents were diagnosed with primary open angle glaucoma (33.9%) at Manchester and glaucoma suspect status at Bristol (50.6%). Patients had high levels of confidence in the person conducting the tests (94.8% Manchester, 98.8% Bristol), and most were likely to recommend the service to family or friends (94.8% Manchester, 92.6% Bristol). We interviewed 10 consultant ophthalmologists, 10 data gathering staff and 20 patients. A number of key themes emerged from the transcribed interviews including: patient experience, clinician perception of patient experience, service delivery, staffing and staff experience, and patient safety.
Conclusions
Glaucoma virtual clinics can be acceptable to both clinicians and patients, including those with a varied complexity of glaucoma and glaucoma-related disease. Dissatisfaction seemed to relate to poor communication or processes and systems within the service rather than complexity of disease.
Subject terms: Health services, Health occupations
Introduction
Approximately 2% of those over 40 years old in the UK have chronic open angle glaucoma, rising to nearly 10% for those over 75 [1]. As patients live longer and the population steadily rises, so too does the clinical demand of those with, or at risk of developing, glaucoma. Both the NHS England elective care transformation programme [2] and Getting It Right First Time (GIRFT) ophthalmology report [3] made recommendations in 2019 to meet demand in glaucoma care. In March 2020, the Coronavirus (COVID-19) pandemic led to NHS trusts suspending routine hospital outpatient appointments during lockdown, highlighting the urgent need for change in ophthalmic practice [4].
To meet this significant demand for clinical review, innovations have developed in glaucoma service delivery, most notably the presence of “shared care” or co-management. Within this healthcare professionals (HCP) work under the supervision of a consultant ophthalmologist, or with appropriate qualifications independently, with roles ranging from data gathering through to decision-making and independent management [1, 5–7].
A “virtual clinic” describes clinics where face-to-face aspects of doctor-patient interactions are removed [8] by separation into two components: (i) clinical measurements (data collection); and (ii) clinical decision-making (review). Virtual clinics have developed throughout the world for a broad range of medical conditions including diabetes [9], cancer [10], bowel disease [11], orthopaedics [12] and more. In a glaucoma virtual clinic (GVC) patients attend a hospital outpatient’s appointment, a community clinic or mobile unit for clinical measurements. Patient data are collected through a series of tests performed by technicians, non-specialist nurses, orthoptists or optometrists. Following the appointment results are reviewed by consultant ophthalmologists or other appropriately trained HCPs, with outcomes sent to the patient via letter [13].
These clinics are intended to reduce time spent in clinic, provide a ‘one-stop-shop’ with all tests being performed on the day, and maximise appointment capacity [14]. A national survey of 42 clinical leads in the UK found half of all ophthalmology units were operating a GVC, and for those not, 42.9% were planning to establish one [15]. GVC are also being established for glaucoma throughout the world [16, 17]. Yet, despite this rise in use, little is known about the experiences of patients and clinicians within this care model, something of even greater relevance after the emergence of COVID-19.
The aims of this study were to determine how satisfied patients were with their glaucoma care across different GVC models, and to qualitatively evaluate both patient and clinician views and experiences of GVC.
Methods
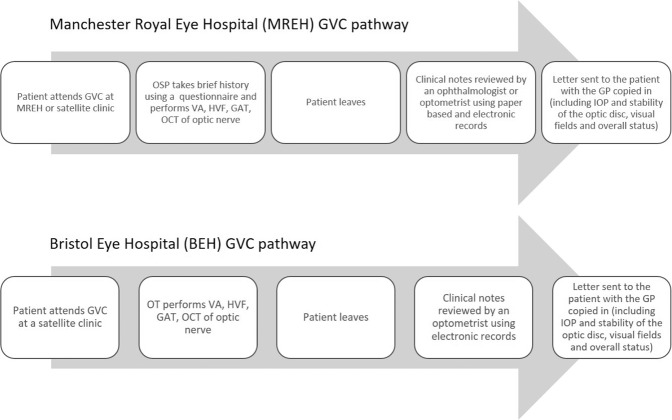
A mixed methods research design was employed comprising of (i) a patient satisfaction survey, and (ii) patient/staff interviews. Lead or glaucoma specialist consultant ophthalmologists were recruited from around the UK, and patients and data gathering clinicians were recruited from the Manchester Royal Eye Hospital (MREH) and the Bristol Eye Hospital (BEH). The usual pathway for GVCs from these hospitals is detailed in Fig. 1. Ethical approval was granted for this project (IRAS project ID 188595).
Fig. 1. Patient pathway through the GVC at the MREH and BEH.
This figures summarises the similarities and differences between the GVC pathways at the two study centres (summary of abbreviations: OSP ophthalmic science practitioner, VA visual acuity, HVF Humphrey visual fields, GAT Goldmann applanation tonometry, OCT optical coherence tomography, OT ophthalmic technician).
Patient satisfaction survey
A Patient Satisfaction Questionnaire (PSQ) was sent to patients of MREH and BEH. The PSQ was adapted from a well-validated General Practice survey [18] to suit patients attending a GVC that has previously been used in eye care [19]. Patients were asked to respond to a range of statements surrounding patient experience.
Method of recruitment and sampling
Patient clinic lists were identified by collaborating clinicians from databases incorporating those seen in a GVC within the previous three weeks, May to July 2018. A random sample of patients were invited to complete a postal PSQ and return their responses.
Inclusion and exclusion criteria
Adult patients (≥18 years of age) with glaucoma or suspect glaucoma status attending a GVC in one of the two services around three weeks prior to receipt of the PSQ. Exclusion criteria were being aged under 18 years old or having not recently attended a GVC.
Patient interviews
Method of recruitment and sampling
A sample of patients with a range of glaucoma-related diagnoses were invited to undertake face-to-face interviews when attending a GVC in the two centres. Patients were provided with a patient information sheet and informed consent obtained. A range of open-ended questions regarding the GVC were employed to allow for an exploration of issues pertinent to each patient. Interviewed patients were contacted 4 to 6 weeks later to complete a short telephone interview establishing how satisfied they were with their feedback letter and any subsequent reflections on the GVC.
Inclusion and exclusion criteria
Adult patients with glaucoma, ocular hypertension (OHT) or suspect glaucoma seen in a virtual clinic at one of the two participating centres. Exclusion criteria were being aged under 18 years; not attending a GVC; and those unable to speak fluent English without translators or interpreters.
Clinicians’ interviews
Lead or glaucoma specialist consultant ophthalmologists were interviewed face-to-face or by telephone. Data gathering clinical staff, including ophthalmic science practitioners (OSP) and ophthalmic technicians (OT), were interviewed face-to-face about their views and experiences of GVCs.
Method of recruitment and sampling
Interviewed consultant ophthalmologists were recruited from a national survey, distributed to 92 lead ophthalmologists from the Royal College of Ophthalmologists’ database, with 42 respondents (response rate 45.7%) about their views and opinions of the use of GVC [15]. As part of the survey, participants were asked if they would be happy to participate in an interview to provide further information. This convenience sample included a range of ophthalmologists from units who were delivering GVCs from all 4 nations of the UK, as well as those who were not. Data gathering clinical staff were recruited from the 2 collaborating sites via a written participant invitation letter, including a participant information sheet and consent form.
Patient and clinician interviews and data analysis
Semi-structured interviews were used to ensure that, whilst the primary topic areas would be covered, respondents were given flexibility in how they answered, guiding the interview and allowing for unanticipated areas raised by participants. The interviews were recorded digitally and transcribed anonymously. Data was analysed using the framework method, a systematic and widely recognised tool for qualitative data analysis [20]. Interviews from clinicians and patients were initially analysed separately within the same underlying framework, before relationships and interlinked themes between cohorts were identified using NVIVO 12 (QSR International, Cambridge, Massachusetts, USA).
Results
Patient satisfaction questionnaire results
Patient background
We received 148 PSQs comprised of 67 patients from the MREH (response rate 48.9%) and 81 from the BEH (response rate 62.3%); an overall response rate of 55.4%. Nine patients were excluded from the MREH and we were unable to access notes for 2 patients to determine their background. The female-to-male ratio was 52:48% at MREH and 61:39% at BEH. Most respondents described their ethnicity as White British (83% - MREH; 89% - BEH) followed by “not stated” (7% - MREH; 4% - BEH) then Black Caribbean (2% - MREH; 3% - BEH).
Glaucoma-related diagnosis
The patients’ glaucoma-related diagnoses (worst eye) are illustrated in Table 1. At MREH most patients who responded were diagnosed with primary open angle glaucoma (POAG) (33.9%), whereas at BEH most patients who responded were glaucoma suspects (50.6%) and only 4.9% had POAG.
Table 1.
Glaucoma-related diagnosis in eye with worst disease.
| Diagnosis (worst eye) | Manchester | Bristol | Total | |||
|---|---|---|---|---|---|---|
| Not stated / unknown | 0 | 0.0% | 4 | 4.9% | 4 | 2.9% |
| Glaucoma Suspect | 16 | 28.6% | 41 | 50.6% | 57 | 41.6% |
| Ocular Hypertension | 9 | 16.1% | 28 | 34.6% | 37 | 27.0% |
| Normal Tension Glaucoma | 6 | 10.7% | 0 | 0.0% | 6 | 4.4% |
| Primary Open Angle Glaucoma | 19 | 33.9% | 4 | 4.9% | 23 | 16.8% |
| Secondary Glaucoma | 3 | 5.4% | 2 | 2.5% | 5 | 3.6% |
| Narrow Angle Glaucoma | 3 | 5.4% | 2 | 2.5% | 5 | 3.6% |
| Total | 56 | 100.0% | 81 | 100.0% | 137 | 100.0% |
Previous glaucoma laser or surgery
Ten patients from the MREH (17.9%) had undergone surgery (5 patients with trabeculectomy, 1 patient with bilateral Xen implants) or laser treatment (3 patients with YAG peripheral iridotomy and 1 selective laser trabeculoplasty). There were no patients who had previously undergone glaucoma-related surgery or laser from the BEH cohort.
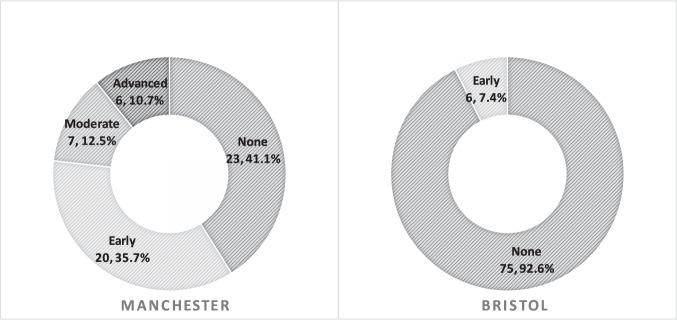
Visual field status
The extent of visual field loss in the eye with the best field of vision was classified using the mean deviation (MD) of the Humphrey 24-2 visual field assessment. The comparison results between MREH and BEH are detailed in Fig. 2. Patients from the BEH had less visual field loss (mean MD −0.42 dB, range +2.40 to −6.13 dB) than those from the MREH (mean MD −1.90 dB, range +2.36 to −22.18 dB) and this difference was statistically significant (two-tailed t test t(138) = −2.510, p = 0.013).
Fig. 2. Stage of glaucoma-related visual field loss.
This figure shows the stage of glaucoma related visual field loss in the eye with the best visual field (N, %) using a simplified Hoddap-Parrish-Anderson criteria (where early is mean deviation < −6 dB, moderate is mean deviation ≥ −6 and < −12 dB and severe is mean deviation ≥ −12 dB).
Topical treatment
Patients from BEH were on fewer medications (mean 0.54, range 0–3) than those from MREH (mean 0.88, range 0 to 4 medications). Whilst there was no statistically significant difference (chi-square) when comparing those on medications versus those on ≥1 medication between BEH and MREH, the value (X2 (1, N = 137) = 3.272) did approach significance (p = 0.070).
Questionnaire responses
Responses to the PSQ are summarised in Table 2. All patients felt they received adequate information from both sites prior to attending the GVC and both units scored highly on waiting times and staff interaction. Patients attending both GVCs had high levels of confidence in staff conducting tests (94.8% MREH, 98.8% BEH) and would recommend the service to family or friends (94.8% MREH, 92.6% BEH). There was a slightly higher reported preference from the MREH patients compared to BEH patients for attending a GVC over a traditional face-to-face clinic (81.0% MREH, 71.8% BEH). Feedback letters were received by a minority of patients at the point of responding to the PSQ (27.6% MREH, 22.2% BEH). However, 100% of patients who did receive a letter felt it was clear and helped them understand their condition.
Table 2.
Summary of the PSQ responses from patients attending the GVC at the MREH and BEH (N, %).
| Agree | Disagree | Unsure | No response | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MREH | BEH | Overall | MREH | BEH | Overall | MREH | BEH | Overall | MREH | BEH | Overall | |||||||||||||
| Q1: I received adequate information about my appointment prior to attending | 58 | 100.00% | 81 | 100.00% | 139 | 100.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0% | 0 | 0.00% | 0 | 0.00% | 0 | 0% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q2: The length of time that I had to wait to be seen was reasonable | 56 | 96.60% | 79 | 97.50% | 135 | 97.10% | 2 | 3.40% | 1 | 1.20% | 3 | 2.20% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q3: The health care person introduced themselves to me | 58 | 100.00% | 79 | 97.50% | 137 | 98.60% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q4: The health care person listened to me | 57 | 98.30% | 81 | 100.00% | 138 | 99.30% | 0 | 0.00% | 0 | 0.00% | 0 | 0% | 1 | 1.70% | 0 | 0.00% | 1 | 0.70% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q5: The health care person explained the tests and procedures fully in a way that I could understand | 57 | 98.30% | 80 | 98.80% | 137 | 98.60% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 1 | 1.70% | 0 | 0.00% | 1 | 0.70% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q6: I was given enough privacy when tested or advised | 58 | 100.00% | 78 | 96.30% | 136 | 97.80% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
| Q7: I was seen in a clean and safe environment | 58 | 100.00% | 80 | 98.80% | 138 | 99.30% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
| Q8: I hadconfidence and trust in the health care person who was carrying out the tests/ advising me | 55 | 94.80% | 80 | 98.80% | 135 | 97.10% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 3 | 5.20% | 0 | 0.00% | 3 | 2.20% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
| Q9: I was treated with dignity at all times | 57 | 98.30% | 80 | 98.80% | 137 | 98.60% | 0 | 0.00% | 0 | 0.00% | 0 | 0% | 1 | 1.70% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 0 | 0.00% | 1 | 0.70% |
| Q10: was made aware I would not see a doctor or optometrist during my visit, but would receive the results of my assessment with a letter after my appointment | 55 | 94.80% | 75 | 92.60% | 130 | 93.50% | 3 | 5.20% | 4 | 4.90% | 7 | 5.00% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
| Q11: I was happy to receive my results later and not to see a doctor or optometrist on the day | 51 | 87.90% | 69 | 85.20% | 120 | 86.30% | 6 | 10.30% | 9 | 11.10% | 15 | 10.80% | 1 | 1.70% | 2 | 2.50% | 3 | 2.20% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
| Q12a: Have you received a letter giving you feedback and an outcome from your appointment? | 16 | 27.60% | 18 | 22.20% | 34 | 24.50% | 42 | 72.40% | 59 | 72.80% | 101 | 72.70% | 0 | 0.00% | 0 | 0.00% | 0 | 0 | 0 | 0.00% | 4 | 4.90% | 4 | 2.90% |
| Q12b: The letter I received after the appointment was clear and helped me to understand my condition | 16 | 100.00% | 18 | 100.00% | 34 | 100.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% |
| Q13: I prefer to be seen in this type of clinic where I receive my results by post rather than previous clinics where I have waited to see a doctor or optometrist | 47 | 81.00% | 59 | 72.80% | 106 | 76.30% | 5 | 8.60% | 12 | 14.80% | 17 | 12.20% | 4 | 6.90% | 5 | 6.20% | 9 | 6.50% | 2 | 3.40% | 5 | 6.20% | 7 | 5.00% |
| Q14: I would recommend the service to my family and friends | 55 | 94.80% | 75 | 92.60% | 130 | 93.50% | 2 | 3.40% | 4 | 4.90% | 6 | 4.30% | 1 | 1.70% | 1 | 1.20% | 2 | 1.40% | 0 | 0.00% | 1 | 1.20% | 1 | 0.70% |
Patient, consultant and ophthalmic science practitioner/technician interviews
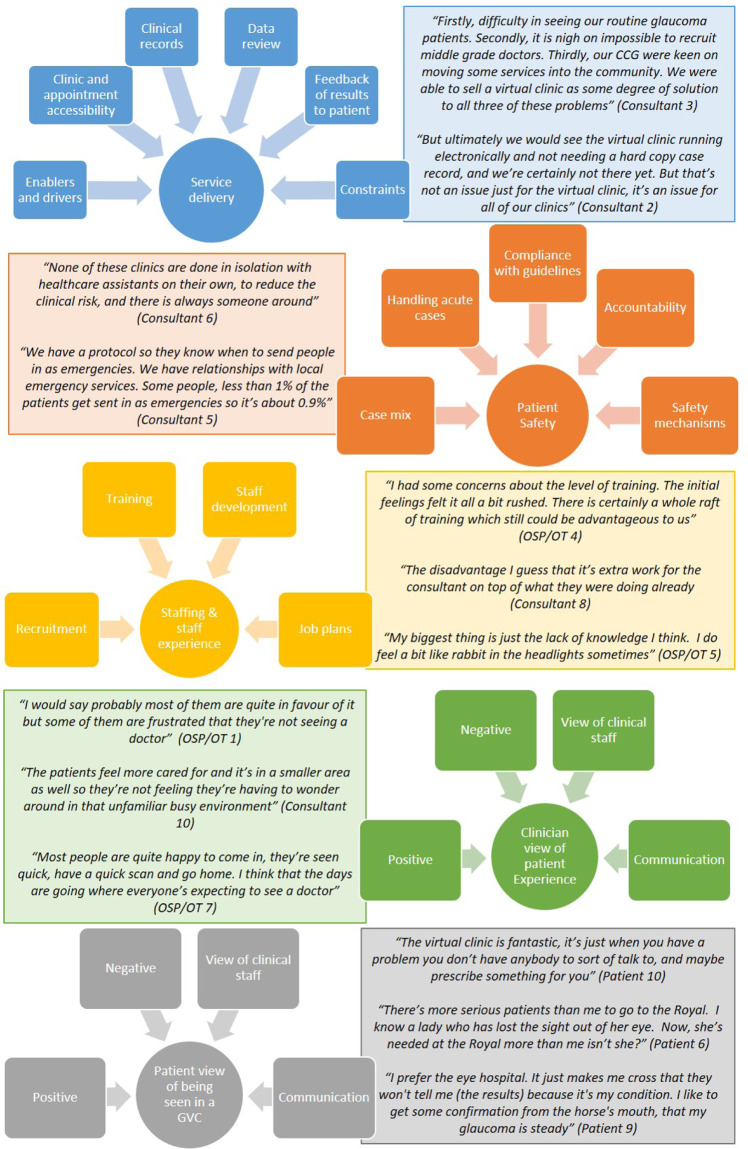
We interviewed 10 consultant ophthalmologists from 10 different departments about their views and opinions of GVCs. There were 7 OSPs and 13 patients interviewed from MREH and 3 OTs and 7 patients interviewed from BEH. A number of key themes emerged including patient experience, clinician perception of patient experience, service delivery, staffing and staff experience, and patient safety. These are outlined below with further supporting evidence in Fig. 3.
Fig. 3.
Summary of themes and sub-themes, as well as anonymised quotes from patient, OSP/OT and consultant interviews.
Patient experience and clinician perception of patient experience
All cohorts offered perspectives on how the GVC influence patient experience, with the main sub-themes relating to waiting times, communication, accessibility, and patient-clinician interactions. Waiting times were reported by all participants as a key aspect of positive experiences, reporting GVCs to provide quicker care delivery:
“That benefits the staff and the patient, because you know we are in and out. So whereas you are always told to allow for 2 h…under an hour and I am finished” (Patient 10).
“Once they’ve gone through it once and realise that they’re in and out in less than an hour and they get a letter from their own consultant a week later they’re converts. Most of them don’t want to go back into a regular clinic” (Consultant 5).
Some HCPs felt patients were sometimes unaware they were not seeing a doctor or optometrist on the day or receive the clinical outcome of their appointment, sometimes leading to OSP/OTs handling patient concerns:
“Patients who are already in the system, who like it, it’s fantastic, but it’s the patients who first time, come along and they just don’t understand why they’re there and they’ve had absolutely no literature at all” (OSP/OT 6).
Many Consultants made use of patient information sheets and specific clinic letters to advise their patients of differences between a GVC and more conventional clinic appointments:
“We’ve actually designed a specific letter for them that goes out with the appointment to explain that we’re aware that their appointment is overdue, and so this is a way of getting all the information that we require on them, and to reassure them that they will still remain under the care of a consultant” (Consultant 2).
For those attending GVCs outside of the main hospital sites, both patients and OSP/OT staff reported positive improvements to the clinical environment:
“The patients feel more cared for and it’s in a smaller area as well so they’re not feeling they’re having to wonder around in that unfamiliar busy environment” (OSP/OT 8).
“It’s certainly a much better environment here. Because it’s a bit like a cattle market there, lots of people dashing around” (Patient 17).
That said, some consultants were concerned about taking away the patient-clinician interaction:
“I think the biggest disadvantage is not picking up on the nuances of a conversation about someone’s quality of life issues” (Consultant 6).
One OSP stated they highlighted to patients that being referred to a GVC could be seen as an assurance about the stability of their condition:
“We try to be positive and say you’re a very well managed patient, you’re obviously low risk, the consultant has reviewed your status and you’re so low risk you don’t need to see a doctor every single time” (OSP/OT 4).
Service delivery
GVCs were running mainly from Trust sites, although many were using satellite clinics or community centres. Some had part electronic records and software to view visual fields. However, most units did not have a fully electronic patient record and felt this was a limiting factor for service efficiency:
“I can see a patient virtually in about 5 min. If I had a full electronic patient record, I could see a patient virtually in about 3 min. If I see a patient face-to-face it’s 10 min. So I influence far more patients under my care by seeing a lot of them virtually” (Consultant 9).
Use of paper records, poorly linked electronic records and unavailability of visual field progression analyses were often reported as constraints of running a GVC by Consultants. In addition, staffing to provide data collection and virtual review were reported as challenges. Creating capacity was the driving force for service organisers to establish GVCs, alongside concerns about sustainability of the traditional clinic model due to lack of staff and clinic space.
Staffing & staff experience
Consultants reported their GVCs were staffed by a mixture of OTs, OSPs, orthoptists, ophthalmic nurses and optometrists gathering data for review, alongside consultant ophthalmologists, specialist trainee ophthalmologists and optometrists reviewing cases. One consultant felt it was important to select the right personality to work in a GVC:
“It’s very important to pick the appropriate personalities rather than just assume that a particular professional group can take a role on. The requirements for that role do demand a very good ability to interact well with patients, rather than just all the ability to do the tests” (Consultant 2).
Relatedly, some OSP/OTs felt they would benefit from further training:
“I would welcome a lot more training and a lot more understanding of the conditions of glaucoma. We’re not given as much information as is available and it would help us to know whether or not the tests we’re performing are of sufficient quality” (OSP/OT 9).
An OSP reported satisfaction that their role helped support the overall glaucoma structure:
“What I like best is knowing you’re making the entire glaucoma structure work better, you’re taking up a group of patients to allow everything else to fall into place, the more complicated cases to be seen by a consultant” (OSP/OT 2).
Patient safety
Patient safety was described by consultants as both an incentive for GVCs and a cause for concern. Some consultants were worried about missed pathology in a GVC, whereas others reported greater concerns over appropriate follow-up times in standard care:
“It’s much better to actually have some information on those backlog patients rather than no information at all, so we’ve used the virtual model to actually see some of those, which are far more complex” (Consultant 2).
“Patient safety is the primary concern isn’t it, so we were extremely cautious in rolling out the project and we had very strict inclusion criteria and now we are slowly increasing our numbers” (Consultant 7).
There was a concern from one consultant that GVCs were creating a paradox where lower risk patients were getting timelier follow-up, and more frequent imaging and visual field testing:
“We have this paradox that the patients who are less at risk of visual loss are now getting a whole raft of tests in a timely manner. Whereas the more complex patients who come to our clinic and are very much at risk of losing their vision maybe don’t get a visual field test as often as we would like” (Consultant 2).
The additional capacity in GVC and availability of imaging and visual fields at each visit has led some units to use GVC for interim appointments to increase the timeliness of follow-ups as well as the frequency of diagnostic tests.
Discussion
The results of this study demonstrate a broad spectrum of opinion amongst patients and clinicians about the role of GVCs in delivering safe and effective care for glaucoma and glaucoma-related diagnoses. Patients responding to the PSQ were satisfied with clinic waiting times and demonstrated high levels of trust in the staff performing tests in the GVC. All patients felt they had been given prior advice of the type of clinic they were due to attend, highlighted by one OSP/OT as a potential cause for complaint with patients. Almost all patients responding to the PSQ would recommend a GVC to family or friends (93.5%), although 10.8% of patients were not happy to receive clinic results by post, and 12.2% of patients would have been happier to wait longer to see a doctor or optometrist on the day.
The qualitative interviews showed some patients preferred to hear their results directly from clinicians and some clinicians were also concerned about missing quality of life nuances that may be identified during conversations conducted in traditional clinics. Whilst 100% of those who received feedback letters from the GVC agreed they helped them understand their condition, just 24.5% of patients had received their letter following their clinic attendance, at the time of interviewing, suggesting delays in receipt of appointment outcomes. This limits the qualitative evidence we have from patients who completed the full patient journey within the GVC and is in contrast from Consultant 5 working at another unit, quoted in the results to say patients receive their letter within a week. Addressing such delays and adding further quality of life questions in clinical questionnaires may aid acceptance. As some patients may have difficulties in reading letters due to visual impairment, disability or language barriers a letter may not be suitable for communicating clinic outcomes for all patients. With increased use of telephone and video consultations during COVID-19 [21], further research to which methods patients preferred for communicating GVC outcomes would be useful.
Despite having a more complex case mix in MREH than BEH, MREH patients reported a slightly higher preference on being seen in the GVC over a traditional glaucoma clinic. At the time this survey was conducted, a questionnaire was being used within the GVC in MREH, but not in BEH, potentially influencing responses. Some patients did report dissatisfaction with not having the opportunity to ask questions about their condition and the MREH GVC model accommodates patient questions through the OSP completed questionnaire, thereby allowing clinicians to respond accordingly. Interviewed patients reported satisfaction with how calm and efficient the GVC environment was compared to the traditional clinics, suggesting those with more complex glaucoma may have experienced longer waits historically.
As well as overall satisfaction with GVC, patients often reported an understanding that GVC helped hospitals to prioritise traditional clinics for more complex cases. One respondent highlighted a case of someone that had lost sight in one eye and felt such patients were greater priority (Fig. 3). It was also noted by all cohorts that providing better patient information about the purpose of a GVC nurtures acceptance of this care model.
Staff working as OSP/OTs reported satisfaction in working within the glaucoma service. However, OSP/OTs commonly felt they would benefit from more detailed training, particularly around knowledge of the condition and medications. As some patients also highlighted concerns about GVC staff ability to answer condition-related questions, providing better education for OSP/OTs may enable them to respond to some queries, improving staff and patient experience.
This study is the first qualitative-based research to examine the experiences and perceptions of GVC from both patients and clinicians, including data gathering staff from two centres. Court and Austin undertook some early work on patient experience in GVCs [22], looking at both patient acceptance of GVCs as well as comparing patient education in the GVC to standard clinics. Whilst Court and Austin’s study showed a similar overall mean satisfaction score between clinics, as a questionnaire was used there was no opportunity to probe patient views and this work was focussed more towards patient education, rather than patient experience attending this clinic.
In turn, Kotecha et al. used a semi-structured qualitative approach, interviewing patients before and after attending standard glaucoma clinics at Moorfields Eye Hospital and the GVC [23]. This study usefully considers the views of both follow-up patients and those first seen in an NHS hospital-based glaucoma service. However, it only considers patients being seen for the first time in GVCs, whereas our study seeks the views of those who may have attended a GVC multiple times. As no patient surveyed had attended the GVC for more than three visits, further analysis of whether there is a fatigue effect in patient experience after multiple GVC visits would be beneficial. Our study also offers perspectives from the North and South West of England, complementing work by Kotecha et al in London, although both studies may not be representative of patient views across the UK given consultants interviewed reported different approaches to the GVC model. Like previous studies, a mainly Caucasian patient population was recruited, and the views may not reflect the wider glaucoma population. Further qualitative work on experiences of patients from different ethnic groups or where English is not their first language and different GVC models is needed. A limitation of this study is the response rate of the PSQ and it is possible patient satisfaction may have differed in those who did not respond.
The present study was undertaken prior to the COVID-19 pandemic and much may change in how clinics are likely to be delivered. As further delays to routine outpatient appointments will increase the capacity burden, the role of GVC will become more important. The UK and Eire Glaucoma Society and the Royal College of Ophthalmologists’ have recently released recommendations for glaucoma services in the recovery phase of COVID-19, including the role of GVCs [24]. The Royal College of Ophthalmologists’ also recently highlighted the role of telemedicine and remote consultation in increasing capacity [25]. Potentially GVCs could also include remote consultations for those requesting them, which may further increase patient acceptance.
This study shows GVCs can be acceptable to both clinicians and patients, including those with varied complexity of glaucoma and glaucoma-related disease. Whilst pressures on services may mean service planners expand GVCs to create capacity, our results indicate that ensuring services are set up to run safely and effectively across different risk profiles, rather than developing services just for those at lowest risk, may be key to successful GVCs.
Summary
What was known before
Virtual clinics for glaucoma care are being increasingly used to meet demands for capacity.
However, little was known about patient and clinicians’ experiences and perceptions.
What this study adds
This study shows GVCs can be acceptable to both clinicians and patients, including those with varied complexity of glaucoma and glaucoma-related disease.
Acknowledgements
The team would like to acknowledge Glaucoma UK for funding this study.
Funding
This project was funded by Glaucoma UK.
Author contributions
PJGG is first author, who planned the study, collected the data and prepared this paper JRM planned the study, collected and analysed the data LA planned the study, reviewed and contributed to the content of this paper SR reviewed and contributed to the content of this paper HW planned the study, reviewed and contributed to the content of this paper PGDS planned the study, collected the data, reviewed and contributed to the content of this paper RAH planned the study, collected the data, reviewed and contributed to the content of this paper.
Compliance with ethical standards
Conflict of interest
PJGG – no relevant conflict of interest declarations. JRM – no relevant conflict of interest declarations. LA – no relevant conflict of interest declarations. SR– no relevant conflict of interest declarations. HW – no relevant conflict of interest declarations. PGDS – provides independent consultancy service to Newmedica. RAH – no relevant conflict of interest declarations.
Footnotes
The authors would like to dedicate this paper to the memory of their friend, colleague and co-author Joanne R Marks.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Institute for Health and Care Excellence. Glaucoma: diagnosis and management. NICE guideline NG81. https://www.nice.org.uk/guidance/ng812017. [PubMed]
- 2.NHSE. Transforming elective care services ophthalmology. https://www.england.nhs.uk/wp-content/uploads/2019/01/ophthalmology-elective-care-handbook-v1.1.pdf; 2019.
- 3.MacEwen C, Davis A, Chang L GIRFT Programme National Specialty Report Ophthalmology. https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/12/OphthalmologyReportGIRFT19P-FINAL.pdf; 2019.
- 4.Oliver D, David Oliver. Covid-19 will make us stop some activities for good. BMJ. 2020;369:m1148. doi: 10.1136/bmj.m1148. [DOI] [PubMed] [Google Scholar]
- 5.RNIB. Models of glaucoma care: ensuring patients are at the centre. www.rnib.org.uk2017.
- 6.Spencer IC, Spry PGD, Gray SF, Baker IA, Menage MJ, Easty DL, et al. THE BRISTOL SHARED CARE GLAUCOMA STUDY - STUDY DESIGN. Ophthalmic Physiol Opt. 1995;15:391–4. doi: 10.1046/j.1475-1313.1995.9500065l.x. [DOI] [PubMed] [Google Scholar]
- 7.Roberts HW, Rughani K, Syam P, Dhingra S, Ramirez-Florez S. The Peterborough scheme for community specialist optometrists in glaucoma: results of 4 years of a two-tiered community-based assessment and follow-up service. Curr Eye Res. 2015;40:690–6. doi: 10.3109/02713683.2014.957326. [DOI] [PubMed] [Google Scholar]
- 8.McGrail KM, Ahuja MA, Leaver CA. Virtual visits and patient-centered care: results of a patient survey and observational study. J Med Internet Res. 2017;19:e177. doi: 10.2196/jmir.7374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cox PRN, Maric T, Naik A, Northover E, Greg M, Alcayde D, et al. A pilot study assessing the safety of a virtual clinic for diabetes in pregnancy. Diabet Med. 2018;35:188. [Google Scholar]
- 10.McIver A, Maddock N, Dunbar J, Hughes J, Ledson MJ, Smyth C, et al. The use of a virtual clinic to speed up and improve the cancer diagnostic pathway-2 year experience. Thorax. 2016;71:A131–A. doi: 10.1136/thoraxjnl-2016-209333.230. [DOI] [Google Scholar]
- 11.Yarrow H, Irving P, Williams A, Hibberts F, Koumoutsos I, Darakhshan A, et al. Improving care for patients with perianal Crohn’s disease; review of a perianal virtual clinic. J Crohns Colitis. 2017;11:S492–S. doi: 10.1093/ecco-jcc/jjx002.926. [DOI] [Google Scholar]
- 12.Gupta S, Jones G, Shah S. Optimising orthopaedic follow-up care through a virtual clinic. Int J Orthop Trauma Nurs. 2018;28:37–9. doi: 10.1016/j.ijotn.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Wright H, Diamond J Service innovation in glaucoma management: using a web-based electronic patient record to facilitate virtual specialist supervision of a shared care glaucoma programme. Br J Ophthalmol.; 2015. p. 313–9. [DOI] [PMC free article] [PubMed]
- 14.Royal College of Ophthalmologists. Standards for Virtual Clinics in Glaucoma Care in the NHS Hospital Eye Service. www.rcophth.ac.uk/wp-content/uploads/2017/03/Virtual-Glaucoma-Clinics.pdf2016.
- 15.Gunn PJG, Marks JR, An L, Waterman H, Spry PGD, Harper RA. Acceptability and use of glaucoma virtual clinics in the UK: a national survey of clinical leads. BMJ Open Ophthalmol. 2018;3:7. doi: 10.1136/bmjophth-2017-000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kassam F, Yogesan K, Sogbesan E, Pasquale LR, Damji KF. Teleglaucoma: improving access and efficiency for glaucoma care. Middle East Afr J Ophthalmol. 2013;20:142–9. doi: 10.4103/0974-9233.110619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The Current State of Teleophthalmology in the United States. Ophthalmology. 2017;124:1729–34. doi: 10.1016/j.ophtha.2017.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paddison CAM, Saunders CL, Abel GA, Payne RA, Campbell JL, Roland M. Why do patients with multimorbidity in England report worse experiences in primary care? Evidence from the General Practice Patient Survey. BMJ Open. 2015;5:e006172. doi: 10.1136/bmjopen-2014-006172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baker H, Harper RA, Edgar DF, Lawrenson JG. Multi-stakeholder perspectives of locally commissioned enhanced optometric services. BMJ Open. 2016;6:e011934. doi: 10.1136/bmjopen-2016-011934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ritchie J, Spencer L Qualitative data analysis for applied policy research Analysing qualitative data by A Bryman and R G Burgess. London: Routledge 1994. p. 173–94.
- 21.Safadi K, Kruger JM, Chowers I, Solomon A, Amer R, Aweidah H, et al. Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol. 2020;5:e000487. doi: 10.1136/bmjophth-2020-000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Court JH, Austin MW. Virtual glaucoma clinics: patient acceptance and quality of patient education compared to standard clinics. Clin Ophthalmol. 2015;9:745–9. doi: 10.2147/OPTH.S75000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotecha A, Bonstein K, Cable R, Cammack J, Clipston J, Foster P. Qualitative investigation of patients’ experience of a glaucoma virtual clinic in a specialist ophthalmic hospital in London, UK. BMJ Open. 2015;5:9. doi: 10.1136/bmjopen-2015-009463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UKEGS TRCoOa. Glaucoma Management Plans during Recovery Phase of COVID-19. 2020.
- 25.Royal College of Ophthalmologists. Overview of Digital Transformation and Telemedicine during COVID19. 2020.