Abstract
Background:
Most patellar dislocations occur in a lateral direction because of a summed lateral force vector and predisposing anatomic risk factors. Medial patellar instability is rare and is a well-recognized iatrogenic complication of an overly aggressive lateral retinacular release. Noniatrogenic medial patellar dislocations are rare. The management of these injuries is not well described.
Purpose:
To describe the experience of the International Patellofemoral Study Group with patients with noniatrogenic medial patellar dislocation.
Study Design:
Case series; Level of evidence, 4.
Methods:
Members of the International Patellofemoral Study Group (N = 64) were surveyed between October 2018 and April 2019. This group was chosen because of its wide referral base and interest in patellar instability. Specialists who had encountered a patient with medial patellar instability were sent a questionnaire inquiring about details of the case, including patient demographics, medical history, level of athletic competition, injury characteristics, and treatment. Cases were confirmed by physical examination records and, in some cases, with findings on advanced radiographic imaging.
Results:
The survey response rate was 73% (47/64). Three of the 47 specialists (6.4%) reported they had seen a case of noniatrogenic medial patellar dislocation, for a total of 6 cases. Four cases were described as recurrent medial dislocations in the setting of hypermobile Ehlers-Danlos syndrome; 2 were treated nonoperatively, 1 underwent lateral patellofemoral ligament reconstruction, and 1 underwent derotational osteotomies. Two medial-sided patellar dislocations in collegiate athletes were sports-related injuries that required surgical debridement but no ligamentous reconstruction. None of the patients had persistent or recurrent instability at the time of their most recent follow-up.
Conclusion:
Noniatrogenic medial patellar dislocations are extremely rare. This case review suggests that the treatment of first-time medial patellar instability in patients without known risk factors should follow the same principles as the treatment of lateral instability with no known risk factors, which is nonoperative management. For patients with documented risk factors and recurrence, surgery to address the risk factors may be appropriate.
Keywords: collegiate athlete, lateral patellar dislocation, medial patellar dislocation, noniatrogenic
Acute patellar dislocation is a common knee injury in adolescents and young adults, with primary patellar dislocations occurring at a rate of 42 per 100,000 person-years.4 Most primary and recurrent dislocations are lateral because of the summed lateral force vector on the patella at the time of injury. Additionally, a subset of patients have predisposing anatomic risk factors of lateralized tibial tuberosity, dysplastic trochlea, and medial soft tissue insufficiency.24 Rarely, patients may present with medial patellar instability. Although medial patellar instability is a recognized complication of lateral retinacular release, it sometimes occurs without previous lateral-sided surgery.1,9,10,16,25,26
Given the perceived rarity of noniatrogenic medial patellar dislocations, we sought to characterize them further. In this study, we examined the experience of a large group of academic patellofemoral surgeons with the diagnosis and treatment of noniatrogenic medial patellar dislocations. We present in detail 2 cases of posttraumatic medial patellar dislocation in athletes with no history of knee surgery.
Methods
International Patellofemoral Study Group Experience
All members of the International Patellofemoral Study Group (IPSG) (N = 64) were surveyed via email between October 2018 and April 2019. This group was chosen because of its wide referral base, extensive experience, and multidisciplinary scholarly work on the patellofemoral joint. IPSG members were asked whether they had ever treated a patient with a medial patellar dislocation with no known history of previous ipsilateral knee injury or surgery. Members who had encountered a patient with medial patellar instability were sent a questionnaire inquiring about details of the case(s). Cases were included if the member could identify the patient and provide sufficient history to ensure a correct diagnosis. All included cases were confirmed by records of the specialist’s physical examination; some cases had findings on advanced radiographic imaging indicating dislocation. This study was deemed exempt from institutional review board approval.
Results
The survey response rate was 73% (47/64). Of the 47 respondents, 44 (94%) had encountered no patients with medial patellar dislocation in the absence of previous ipsilateral knee surgery. Several respondents recalled cases but were unable to identify the patients, provide sufficient details, or confirm that the patients had not undergone previous knee surgery. The 3 surgeons (6.4%) who had seen at least 1 case of noniatrogenic medial patellar dislocation reported 6 cases in total (Table 1). Four of these cases were in patients with hypermobile Ehlers-Danlos syndrome who had experienced recurrent medial patellar dislocations without radiographic confirmation of complete dislocation. None of these patients had previous injury or surgery on the ipsilateral knee. Three of these 4 patients had bilateral instability, 2 of whom had previous surgery on the contralateral knee for recurrent medial instability symptoms. One patient had rotational malalignment of bilateral lower extremities including increased femoral anteversion of 22º and increased tibial torsion of 46º. All 4 patients underwent physical therapy and bracing. Surgical intervention was considered after an adequate trial of nonoperative treatment was unsuccessful.
Table 1.
Characteristics of 6 Patients With Noniatrogenic Medial Patellar Dislocationa
| Patient | Age, y | Sex | Acuity | Bilateral Dislocation | Hypermobile EDS | Sports-Related Injury | Radiographic Confirmation of Dislocation | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1 | 19 | Male | Acute | No | No | Yes | Yes | Arthroscopic chondroplasty |
| 2 | 21 | Female | Acute | No | No | Yes | Yes | Arthroscopic chondroplasty |
| 3 | 16 | Female | Recurrent | Yes | Yes | No | No | Femoral and tibial derotation osteotomies |
| 4 | 15 | Female | Recurrent | Yes | Yes | No | No | Physical therapy |
| 5 | 13 | Male | Recurrent | No | Yes | No | No | LPFL reconstruction |
| 6 | 23 | Female | Recurrent | Yes | Yes | No | No | Physical therapy |
aEDS, Ehlers-Danlos syndrome; LPFL, lateral patellofemoral ligament.
Two of the 6 cases occurred in otherwise healthy patients, both as primary dislocations in collegiate athletes. Because of their distinct features, these cases are described in detail.
Patient 1
A 19-year-old male National Collegiate Athletic Association Division I collegiate basketball player was referred to the orthopaedic surgery clinic for a fourth opinion. Three months before presentation, he had experienced a sharp, sudden pain in the left knee when he landed awkwardly from a jump during basketball practice. The injury had been managed via rest, icing, bracing, physical therapy, nonsteroidal anti-inflammatory drugs, and a corticosteroid injection. The patient noted a history of lateral patellar dislocation of the contralateral knee, which required reduction, and a family history of patellar instability. On physical examination, the patient was 213 cm tall, weighed 88 kg, and had upper extremity hyperlaxity. He had neutral tibiofemoral alignment, normal cruciate and collateral ligament examinations, tenderness over the medial femoral condyle, and apprehension with both medial and lateral patellar translation.
Radiographs showed patella alta with an Insall-Salvati ratio of 1.4 and a shallow trochlear groove but without a crossing sign (Figure 1). Magnetic resonance imaging (MRI) scans showed bone contusions of the anterior medial femoral condyle and inferolateral patella (Figure 2). He was treated using reverse J-shaped patellar bracing, nonsteroidal anti-inflammatory drugs, and physical therapy. He underwent arthroscopic chondroplasty, recovered fully, and successfully completed the following collegiate basketball season, with no recurrence during 1.5-year follow-up.
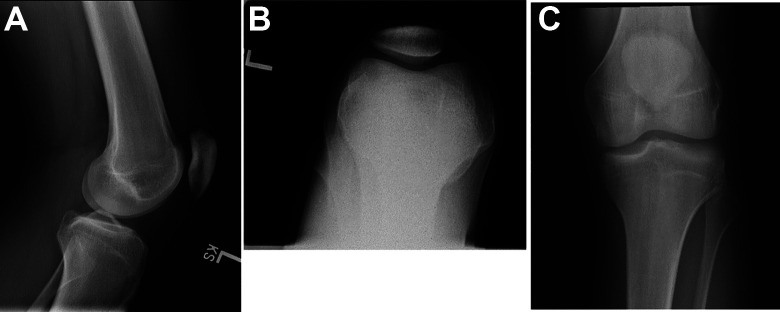
Figure 1.
(A) Lateral, (B) axial, and (C) anteroposterior radiographs of the left knee of a 19-year-old man showing patella alta and a shallow trochlear groove.
Figure 2.
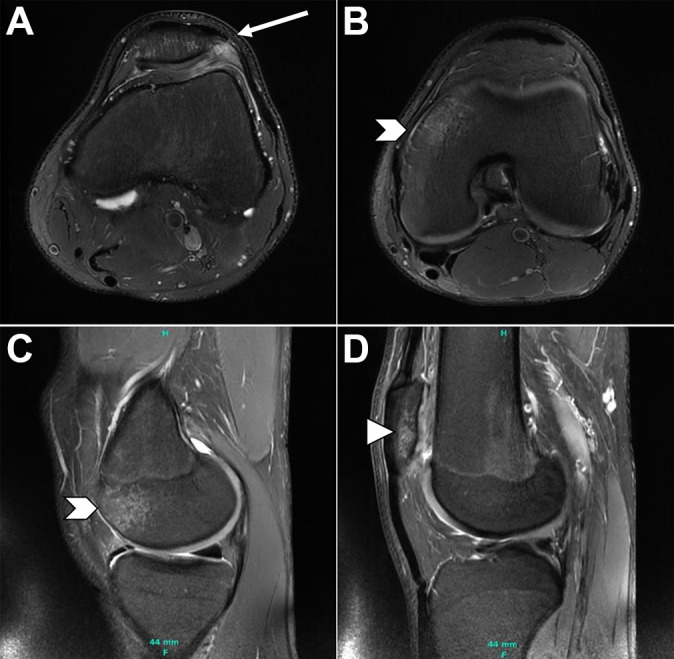
Fat-saturated T2-weighted axial (A, B) and sagittal (C, D) magnetic resonance imaging scans of the left knee of a 19-year-old man showing lateral retinacular disruption at the (A) patellar insertion (arrow) and (B, C) edema within the anterior medial femoral condyle (chevrons) and (D) lateral patella (arrowhead).
Patient 2
A 21-year-old female National Collegiate Athletic Association Division I center back on the soccer team was referred for an acute patellar cartilage injury during her junior year. She had been a starting player since her freshman year. She injured her right knee while playing spring soccer. An opposing player was dribbling across and in front of her when she lunged to make a tackle. She missed the ball, and the other player hit the lateral aspect of her right knee, causing both players to fall. She felt the patella dislocate medially with spontaneous reduction. She was able to walk off the field but noted new grinding and catching. Her knee swelled within several hours. She underwent MRI and was referred for consultation; 2 weeks after injury, she underwent an examination. She was 170 cm tall and weighed 137 lb (61.65 kg). She had mild varus in limb alignment with normal hip rotation. She had no generalized ligamentous laxity. She had mild-to-moderate knee effusion and patellofemoral pain without focal tenderness of the medial or lateral soft tissues. Patellar tilt was positive. She had guarding with displacement of the patella by 1 quadrant laterally and half a quadrant medially without classic apprehension.
Radiographs showed no fracture or dislocation, normal trochlear morphology, and normal patellar height. MRI scans obtained 1 week after injury showed a large, partially displaced chondral flap of the medial aspect of the patellar apex measuring 10 × 15 mm, separated from the underlying bone by as much as 5 mm. Displaced free chondral fragments were observed (Figure 3). She underwent arthroscopic chondroplasty and began a core strength rehabilitation program. Four months after injury, she received a series of 3 injections for viscosupplementation. She recovered fully and completed the last season of her collegiate soccer career with minimal pain and no instability episodes. At 14 months after injury, she continued to have mild patellofemoral discomfort and was offered patellar cartilage restoration if symptoms progressed.
Figure 3.
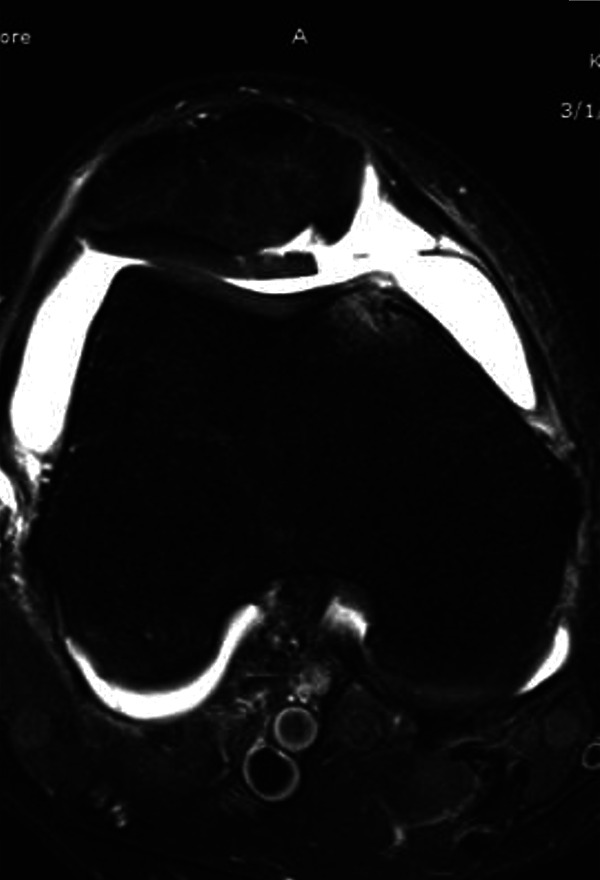
T2-Weighted axial magnetic resonance imaging scan of the right knee of a 21-year-old woman showing medial femoral condyle edema, high-grade chondral lesion, and joint effusion.
Discussion
Overly aggressive lateral retinacular release has been identified as the primary contributing factor to iatrogenic medial patellar instability.6,17 Risk factors for iatrogenic medial patellar instability are lateral retinacular release in the absence of an excessively tight lateral retinaculum preoperatively and release of the vastus lateralis tendon, although vastus lateralis tendon release usually results in subluxation rather than dislocation.20 Miller et al11 highlighted 3 cases of medial patellar dislocation after excessive lateral releases. All 3 cases involved releases extending into the vastus lateralis tendon and subsequent loss of the lateralizing vector during knee extension. Figure 4 shows computed tomography images in a patient who developed medial instability after undergoing 2 stabilization surgeries, including lateral release for recurrent lateral instability.11
Figure 4.
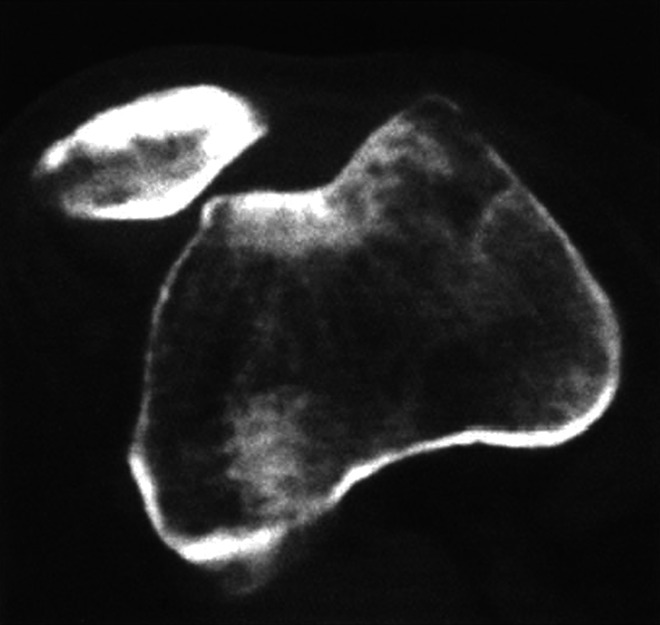
Axial computed tomography image showing medial dislocation of the patella in a 26-year-old woman. Reprinted with permission from Springer Nature: Miller et al.11
However, noniatrogenic medial patellar dislocations are exceedingly rare. We obtained an excellent survey response rate of 73% from the IPSG. Individuals qualify for IPSG membership if substantial portions of their practice and academic focus are dedicated to patellofemoral disorders.22 Of these respondents, 94% had never encountered a patient with noniatrogenic medial patellar dislocation, showing the rarity of this entity. Respondents indicated several additional cases of medial patellar dislocation for which history and examination could not be confirmed. A higher proportion of confirmed cases were in patients with connective tissue disorders that cause ligamentous laxity and malalignment, which may be identifiable risk factors. The 2 confirmed nonsyndromic cases were both in athletes; however, 1 patient had a noncontact injury, and the other had a traumatic injury.
Reports of acute medial patellar dislocation not associated with lateral retinacular release or congenital conditions are rare. The earliest reported case was described by Ratton15 in 1869 in a man with traumatic medial patellar dislocation after being thrown from a cart. The patella was locked medially with the leg flexed; after reduction, the patient was treated via a splint. Memminger10 described a 14-year-old girl with a shallow trochlea, patella alta, and genu recurvatum of 20° who sustained an osteochondral fracture of the lateral patellar facet after internally rotating her tibia in a wide stance. Le Corroller et al9 reported the case of a 19-year-old woman with a shallow trochlea who fell from a horse and sustained a presumed direct trauma to the patella resulting in a transient medial patellar dislocation. On ultrasonography, acute injury to the lateral retinaculum with avulsion at the patellar insertion was noted. The diagnosis was confirmed on MRI scans, which showed a contused anteromedial medial femoral condyle and lateral patellar facet. She was treated using physical therapy and experienced no recurrent symptoms during 15 months of follow-up.
Other cases of noniatrogenic medial patellar instability in the literature typically present as chronic subluxations. These cases display medial patellofemoral tracking and have been treated using various methods, including nonoperative treatments (eg, physical therapy) and operative treatments (eg, quadricepsplasty with lateral retinacular imbrication,16 lateral retinacular and lateral patellofemoral ligament reconstruction,2,18 and medial retinacular release19). Additionally, there is a subset of patients with noniatrogenic medial patellar instability with syndromic features that contribute to instability. These patients typically exhibit muscle paresis or imbalance, severe femoral or tibial torsion, coronal plane malalignment, hyperlaxity, and/or joint contractures.1,25,26 The surgical treatment of these patients addresses these factors directly.
Because medial patellar instability is rare, a thorough history and physical examination are crucial to making the diagnosis. Noting a history of previous knee procedures, especially lateral retinacular release, is important. Whereas patients with lateral instability typically have tenderness over the medial patella, medial patellofemoral ligament, and lateral trochlear ridge, patients with medial instability present with tenderness over the lateral patella and medial femoral condyle. Tests such as the medial patellar apprehension test, Fulkerson relocation test, and Nonweiler and DeLee gravity subluxation test may be positive in patients with medial instability.3,12 Assessing and quantifying lower limb alignment using a rotational profile examination is essential to rule out torsion as a contributing factor.
On MRI scans, lateral patellar dislocations typically display a bone contusion pattern involving the lateral femoral condyle and medial patella, along with joint effusion and disruption of the medial patellofemoral ligament.7,8,13,23 In contrast, the 2 acute cases presented in this study showed the corresponding opposite findings on imaging. The bone contusion pattern instead involved the anterior medial femoral condyle and the lateral patella, indicating a medial patellofemoral dislocation. Additionally, in 1 of the 2 cases, MRI scans showed lateral retinacular failure at the conjoint attachment of the transverse band to the patella, similar to the case described by Le Corroller et al.9 Both patients also had cartilage damage, which was treated using chondral debridement without formal stabilization procedures. Neither patient had experienced a recurrent instability episode at the time of most recent follow-up.
Given the paucity of information in the literature to guide treatment of noniatrogenic medial patellar instability, it makes intuitive sense to follow the same recommendations for treating lateral instability. Patients with first-time dislocations and without major osteochondral fracture should initially be treated nonoperatively using functional bracing, quadriceps strengthening, and progressive return to activity.5,24 Patients with osteochondral injuries after first-time dislocations may require surgery to address these lesions, as noted in 2 of our patients. Patients with recurrent instability that is unresponsive to nonoperative treatment should be considered for stabilization surgery. Contributing factors, such as trochlear dysplasia, patella alta, muscle imbalance, and abnormal tibiofemoral coronal and rotational alignment, should be evaluated and may require concomitant treatment.
Repair or reconstruction of the lateral retinaculum should be considered in patients who have undergone lateral release or who experience recurrent symptoms. Nonweiler and DeLee12 reported a technique of pants-over-vest imbrication of the lateral retinaculum for a series of patients with medial instability after lateral release. This procedure was performed with patients under sensory epidural anesthesia to more accurately assess the tracking of the patella intraoperatively. Teitge and Torga Spak21 described a reconstruction technique that uses a slip of quadriceps tendon with patellar bone block. The tendon is passed through the patella and sutured anteriorly, while the bone block is countersunk into the femur. The femoral starting point was evaluated and selected using an isometer, and the graft was fixed with the knee in 60° to 90° of flexion. Notably, this technique was associated with a 5% rate of patellar fracture.21 A slip of iliotibial band or a free hamstring autograft or allograft14 can also been used for reconstruction of the lateral retinaculum.1,25
Conclusion
Noniatrogenic medial patellar dislocations are extremely rare. This case review suggests that the treatment of first-time medial patellar instability in patients without known risk factors should follow the same principles as the treatment of lateral instability in patients with no known risk factors (ie, nonoperative management).5,24 For patients with documented risk factors and recurrence, surgery to address the risk factors may be appropriate. However, it is difficult to make broad generalizations when overall experience with this specific injury is so limited.
Footnotes
Final revision submitted September 3, 2020; accepted September 25, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.E.L. has received hospitality payments from Zimmer Biomet. J.F. has received research support from Active Implants, Arthrex, Episurf, Fidia Pharma, JRF Ortho, Moximed, Novartis, Organogenesis, Samumed, Vericel, and Zimmer Biomet; consulting fees from Aastrom Biosciences, Aesculap/B.Braun, Arthrex, Cartiheal, Ceterix, Cook Biotech, DePuy Synthes, Exactech, ISTO Technologies, MedShape, Moximed, Organogenesis, Osiris, Regentis, RTI Surgical, Samumed, Vericel, Zimmer Biomet, and ZKR Orthopedics; speaking fees from Aastrom Biosciences, Arthrex, Moximed, Organogenesis, Vericel, and Zimmer Biomet; and royalties from Arthrex, Biopoly, DePuy Synthes, Organogenesis, Springer, and Thieme Medical Publishers and has stock/stock options in MedShape and Ortho Regenerative Tech. S.N.P. has received education payments from CDC Medical and speaking fees from Synthes. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by The Johns Hopkins University.
References
- 1. Ahmad CS, Sinicropi SM, Su B, Puffinbarger WR. Congenital medial dislocation of the patella. Orthopedics. 2003;26(2):189–190. [DOI] [PubMed] [Google Scholar]
- 2. Aksahin E, Yumrukcal F, Yuksel HY, Dogruyol D, Celebi L. Role of pathophysiology of patellofemoral instability in the treatment of spontaneous medial patellofemoral subluxation: a case report. J Med Case Rep. 2010;4:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fulkerson JP. A clinical test for medial patella tracking (medial subluxation). Tech Orthop. 1997;12:144. [Google Scholar]
- 4. Gravesen KS, Kallemose T, Blond L, Troelsen A, Barfod KW. High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1204–1209. [DOI] [PubMed] [Google Scholar]
- 5. Hevesi M, Heidenreich MJ, Camp CL, et al. The recurrent instability of the patella score: a statistically based model for prediction of long-term recurrence risk after first-time dislocation. Arthroscopy. 2019;35(2):537–543. [DOI] [PubMed] [Google Scholar]
- 6. Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383–388. [DOI] [PubMed] [Google Scholar]
- 7. Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109–113. [DOI] [PubMed] [Google Scholar]
- 8. Lance E, Deutsch AL, Mink JH. Prior lateral patellar dislocation: MR imaging findings. Radiology. 1993;189(3):905–907. [DOI] [PubMed] [Google Scholar]
- 9. Le Corroller T, Dediu M, Champsaur P. Transient medial patellar dislocation: injury patterns at US and MR imaging. Skeletal Radiol. 2009;38(5):519–523. [DOI] [PubMed] [Google Scholar]
- 10. Memminger M. Medial patella dislocation. Article in German. Unfallchirurg. 2001;104(10):1011–1013. [DOI] [PubMed] [Google Scholar]
- 11. Miller PR, Klein RM, Teitge RA. Medial dislocation of the patella. Skeletal Radiol. 1991;20(6):429–431. [DOI] [PubMed] [Google Scholar]
- 12. Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994;22(5):680–686. [DOI] [PubMed] [Google Scholar]
- 13. O’Reilly MA, O’Reilly PM, Bell J. Sonographic appearances of medial retinacular complex injury in transient patellar dislocation. Clin Radiol. 2003;58(8):636–641. [DOI] [PubMed] [Google Scholar]
- 14. Parikh SN, Saper MG. Lateral patellofemoral ligament reconstruction for medial patellar instability. In: Parikh SN, ed. Patellar Instability: Management Principles and Operative Techniques. Wolters Kluwer Health; 2019:94–110. [Google Scholar]
- 15. Ratton JJL. Case of dislocation of the patella, inwards. Ind Med Gaz. 1869;4(8):164. [PMC free article] [PubMed] [Google Scholar]
- 16. Richman NM, Scheller AD, Jr. Medial subluxation of the patella without previous lateral retinacular release. Orthopedics. 1998;21(7):810–813. [DOI] [PubMed] [Google Scholar]
- 17. Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC, Merchant AC. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31(3):422–427. [DOI] [PubMed] [Google Scholar]
- 18. Saper MG, Shneider DA. Medial patellar subluxation without previous lateral release: a case report. J Pediatr Orthop B. 2014;23(4):350–353. [DOI] [PubMed] [Google Scholar]
- 19. Shannon BD, Keene JS. Results of arthroscopic medial retinacular release for treatment of medial subluxation of the patella. Am J Sports Med. 2007;35(7):1180–1187. [DOI] [PubMed] [Google Scholar]
- 20. Song GY, Hong L, Zhang H, et al. Iatrogenic medial patellar instability following lateral retinacular release of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2825–2830. [DOI] [PubMed] [Google Scholar]
- 21. Teitge RA, Torga Spak R. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20(9):998–1002. [DOI] [PubMed] [Google Scholar]
- 22. The International Patellofemoral Study Group. IPSG Home. Accessed on April 2, 2020. https://ipsg.org /
- 23. Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189(1):243–246. [DOI] [PubMed] [Google Scholar]
- 24. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 25. Yazdi H, Monshizadeh S, Bozorgi Z. Congenital medial dislocation of the patella with multiple congenital anomalies: case report and method of treatment. J Pediatr Orthop B. 2014;23(2):126–129. [DOI] [PubMed] [Google Scholar]
- 26. Zadek I. Recurrent medial dislocation of the patella: report of a case. Bull Hosp Jt Dis. 1947;8(1):30–32. [PubMed] [Google Scholar]