Abstract
Background
Several studies have established the prognostic value of vasodilator stress cardiovascular magnetic resonance (CMR) in broad population of patients with suspected or known coronary artery disease (CAD), but this specific population of asymptomatic patients with known CAD have never been formally evaluated. To assess the long-term prognostic value of vasodilator stress perfusion CMR in asymptomatic patients with obstructive CAD.
Methods
Between 2009 and 2011, consecutive asymptomatic patients with obstructive CAD referred for vasodilator stress CMR were followed for the occurrence of major adverse cardiovascular events (MACE), defined by cardiovascular mortality or recurrent non-fatal myocardial infarction (MI). Uni- and multivariable Cox regressions were performed to determine the prognostic value of myocardial ischemia and myocardial infarction defined by late gadolinium enhancement (LGE) with ischemic pattern.
Results
Among 1529 asymptomatic patients with obstructive CAD, 1342 (87.8%; 67.7 ± 10.5 years, 82.0% males) completed the follow-up (median 8.3 years), and 195 had MACE (14.5%). Patients without stress-induced myocardial ischemia had a low annualized rate of MACE (2.4%), whereas the annualized rate of MACE was higher for patients with mild, moderate, or severe ischemia (7.3%, 16.8%, and 42.2%, respectively; ptrend < 0.001). Using Kaplan–Meier analysis, myocardial ischemia and LGE were associated with MACE (hazard ratio, HR 2.52; 95% CI 1.90–3.34 and HR 2.04; 95% CI 1.38–3.03, respectively; both p < 0.001). In multivariable stepwise Cox regression, myocardial ischemia and LGE were independent predictors of MACE (HR 2.80 95% CI 2.10–3.73, p < 0.001 and HR 1.51; 95% CI 1.01–2.27, p = 0.045; respectively). The addition of myocardial ischemia and LGE led to improved model discrimination for MACE (change in C statistic from 0.61 to 0.68; NRI = 0.207; IDI = 0.021).
Conclusions
Vasodilator stress CMR-induced myocardial ischemia and LGE are good long-term predictors for the incidence of MACE in asymptomatic patients with obstructive CAD.
Keywords: Cardiovascular magnetic resonance, Stress testing, Ischemia, Asymptomatic, Coronary artery disease, Secondary prevention
Introduction
Despite the decline in the rate of recurrent cardiovascular events over the past decades, recurrence remains a major cause of mortality and morbidity among patients with known obstructive coronary artery disease (CAD) [1, 2]. Risk stratifying patients for recurrent cardiovascular events could be helpful to manage therapeutic strategy for secondary prevention in this population. Whereas the interest of coronary revascularization has been very recently debated in patients with stable CAD [3], secondary prevention therapy is therefore key to decrease the rate of recurrent cardiovascular events in this population. The intensification of secondary prevention therapy is possible, justifying the careful selection of patients with a high residual risk and low therapeutic risk.
In patients with known CAD, the prevalence of myocardial ischemia is estimated around 20% [4]. Furthermore, several studies have shown that asymptomatic patients with myocardial ischemia have at least similar risk for adverse cardiovascular events and mortality as symptomatic patients with typical angina [5, 6]. While risk stratification of asymptomatic patients can be useful in managing secondary prevention, the European and American guidelines do not recommend systematic stress testing in the follow-up of patients with CAD [7, 8], because they are mainly based on studies of symptomatic patients.
Cardiovascular magnetic resonance (CMR) imaging has emerged as an accurate technique to assess ventricular function, the presence of myocardial scar and viability, and myocardial ischemia without ionizing radiation [9–11]. Vasodilator stress CMR has been reported in several studies to be effective to stratify the risk of recurrent cardiac events in secondary prevention [9, 10, 12]. Although several large stress CMR prognostic studies have included asymptomatic patients, targeted prognostic data in those patients with known CAD are very scarce, and dedicated subgroup analysis has not been separately performed [9, 13].
This study aimed to assess the long-term prognostic value of vasodilator stress perfusion CMR in asymptomatic patients with prior obstructive CAD and to evaluate the incremental impact of stress CMR compared to traditional CAD risk factors.
Methods
Study population
Between December 2009 and December 2011, we conducted a single-centre longitudinal study with retrospective enrollment of consecutive asymptomatic patients with known obstructive CAD, referred for vasodilator stress perfusion CMR. Known obstructive CAD was defined by a history of percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) or myocardial infarction (MI), defined by a history of MI on the medical records or presence of significant Q wave on 12-lead electrocardiogram (ECG) in a coronary territory [14]. Exclusion criteria were: (1) any reported cardiovascular-related symptoms such as chest pain or shortness of breath at rest or on exertion 6 months prior to enrollment; (2) contraindication to CMR (e.g., cerebral clips, metallic eye implant); (3) contraindication to dipyridamole; (4) known allergy to gadolinium-based contrast medium; and (5) estimated glomerular filtration rate < 30 ml/min/1.73 m2. Clinical data were collected according to medical history and clinical examination on the day of stress CMR. All patients provided informed written consent. The study was approved by the local ethic committee of our institutions and conducted in accordance with the 1964 Declaration of Helsinki. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
Patients follow-up and clinical outcome
The follow-up consisted of a clinical visit as part of usual care (62%) or by direct contact with the patient or the referring cardiologist (38%). A clinical questionnaire with a detailed description of clinical study endpoints was filled out by three senior cardiologists. Data collection was ended on January 2020. The primary endpoint was the occurrence of at least one of the combined major adverse cardiovascular events (MACE) defined as cardiovascular mortality or non-fatal MI. The secondary endpoint was cardiovascular mortality. Clinical event adjudication was based on the follow-up clinical visit or contact, with a consensus reached by two senior cardiologists. Non-fatal MI was defined by typical angina of ≥ 20 min duration, ECG changes, and a rise in troponin or creatine kinase level above the 99 percentile of the upper reference limit [14]. Cardiovascular mortality was defined as sudden cardiac death with documented fatal arrhythmias or any death immediately preceded by acute MI, acute or exacerbation of heart failure, or stroke. All clinical events were defined according to the published standardized definitions [15]. In patients with multiple events, only the first event was considered for event-free survival analysis. Late coronary artery revascularization was defined by a revascularization occurring > 90 days after CMR. For patients who underwent PCI < 90 days after the index examination, peri-procedural events (MI or cardiovascular mortality) [16] were not included in the analysis.
CMR protocol
The detailed CMR protocol has been published in previous studies [17, 18]. CMR was performed with a 1.5 T CMR system (MAGNETOM Espree, Siemens Healthineers, Erlangen, Germany) with an 18-channel anterior body coil. Long-axis (2-, 3-, and 4-chamber) and short-axis cine images encompassing the left ventricle (LV) from base to apex. Vasodilatation was induced with dipyridamole injected at 0.84 mg/kg over 3 min. At the end of dipyridamole infusion, a 0.1 mmol/kg bolus of gadolinium-based contrast (Dotarem, Guerbet, Paris, France,) was injected at a rate of 5.0 ml/s with an injector (Mallinckrodt Optistar Elite). Stress perfusion imaging was performed using an ECG-triggered saturation-prepared balanced steady state free precession (bSSFP) sequence with the following typical parameters: repetition time/echo time (TR/TE) = 287/1.2 ms, acceleration factor = 2, field of view = 370 × 314 mm, matrix = 224 × 180, reconstructed pixel size = 1.7 × 1.7 × 8 mm. A series of six slices (four short-axis views, a 2-chamber, and a 4-chamber view) were acquired every other heartbeat. Then, theophylline was injected intravenously to null the effect of dipyridamole. Ten minutes after contrast injection, breath-hold contrast-enhanced 3D T1-weighted inversion-recovery gradient-echo sequence was acquired with the same prescriptions to detect late gadolinium enhancement (LGE). Safety was studied with clinical monitoring 1 h after CMR.
CMR image analysis
The syngo.via software (Siemens Healthineers) was used for image display and processing, and Hemolia (Clinigrid Inc., Paris, FR) was used for reporting. LV volumes and function were quantified on the short-axis cine stack. Stress perfusion and LGE images were evaluated according to the 17-segment model of the American Heart Association [19]. The analysis of perfusion images was done visually by two experienced cardiologists (JG and FS) blinded to clinical and follow-up data. Myocardial ischemia was defined as a subendocardial perfusion defect that (1) occurred in at least one myocardial segment, (2) persisted for at least three phases beyond peak contrast enhancement, (3) followed a coronary distribution, and (4) occurred in the absence of LGE in the same segment [13, 20]. The diagnosis of peri-infarction myocardial ischemia surrounding prior MI was confirmed when the perfusion deficit exceeded the limits of LGE by ≥ 1 segment. A transmural perfusion defect in the same area than a subendocardial LGE was not considered as myocardial ischemia. The long-axis perfusion images were used to confirm perfusion defects visualized on the short-axis slices and to assess the apical segment. A myocardial scar was defined by LGE with ischemic patterns defined by subendocardial or transmural LGE [21]. A scar was considered viable if the LGE thickness was < 50% of the total myocardial wall, and nonviable if ≥ 50% [22]. The total number of ischemic segments was calculated for each patient. Mild, moderate, and severe myocardial ischemia were defined as the involvement of 1–2, 3–5, and ≥ 6 myocardial segments, respectively, as already described [10]. LGE was semi-quantitatively assessed using the number of LGE segments.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as frequency with percentage. Follow-up was presented as median and interquartile range (IQR). Differences between patients with and without myocardial ischemia in terms of baseline clinical and CMR characteristics were compared using the Student’s t-test or the Wilcoxon rank-sum test for continuous variables and the chi-square or Fisher’s exact test for categorical variables, as appropriate. Normal distribution was assessed using the Shapiro–Wilk test. Cumulative incidence rates of individual and composite outcomes were estimated using the Kaplan–Meier method and compared with the log-rank test. Data on patients who were lost to follow-up were censored at the time of the last contact. Cox proportional hazards methods were used to identify the predictors of MACE among patients with and without myocardial ischemia. The assumption of proportional hazards ratio (HR) was verified.
The different multivariable models used for adjustment were as follows:
- Model 1
used a stepwise forward Cox regression strategy to select the strongest parsimonious set of clinical covariates for MACE and cardiovascular mortality, considering all clinical covariates with a p-value ≤ 0.2 on univariable screening (without the presence of myocardial ischemia and LGE).
- Model 2
model 1 + presence of myocardial ischemia and LGE.
- Model 3
included the following traditional cardiovascular risk factors: age, male, body mass index (BMI), hypertension, diabetes mellitus, current or previous smoking, dyslipidemia and LV ejection fraction (LVEF).
- Model 4
model 3 + presence of myocardial ischemia and LGE.
The discriminative capacity of each model for predicting MACE was determined according to the Harrell’s C-statistic at baseline and after addition of CMR-induced myocardial ischemia and LGE. The additional predictive value of the presence of myocardial ischemia and LGE was calculated by the Harrell’s C-statistic increment, the categorical net reclassification improvement (NRI), and the integrative discrimination index (IDI). NRI and IDI were computed at the end of follow-up using the R package “survIDINRI” [23].
In competitive risk analysis, cumulative incidence functions (CIFs) were used to display the proportion of patients with the event of interest or the competing event (non-fatal MI or cardiovascular mortality) as time progressed. To analyze the effect of baseline predictors on the CIF, we used the Fine and Gray regression model for the subdistribution hazard.
In addition, the prognostic value of stress CMR in different subsamples of clinical interest were investigated by a Forest Plot. A two-tailed p-value < 0.05 was considered statistically significant. Statistical analysis was performed using R software, version 3.3.1 (R Project for Statistical Computing, R Foundation for Statistical Computing, Vienna, Austria).
Results
Patients characteristics
Among the 6,095 individuals referred for dipyridamole vasodilator stress CMR during the inclusion period, 1,529 (25.1%) patients were asymptomatic with prior obstructive CAD. The flowchart of study participants is depicted in Additional file 1. A total of 1342 asymptomatic patients with prior obstructive CAD completed the clinical follow-up and constituted our study cohort. Baseline patient characteristics and baseline CMR data are shown in Table 1. Among these 1342 patients (82.0% males, 67.7 ± 10.5 years), 55.6% had prior MI, 54.8% previous PCI and 32.1% previous CABG. Most subjects were in sinus rhythm (99.6%). The overall study cohort had a mean LVEF of 45.8 ± 12.5%. A MI was diagnosed by LGE with ischemic patterns in 689 (51.3%) patients, and the presence of myocardial ischemia was detected in 376 (28.0%) patients (Fig. 1). Among the 409 diabetics, 151 (36.9%) had myocardial ischemia.
Table 1.
Baseline and CMR Characteristics of Patients with and without Myocardial Ischemia (N = 1342)
| All patients (N = 1342) |
No ischemia (N = 966) |
Ischemia (N = 376) |
p value | |
|---|---|---|---|---|
| Age (years) | 67.7 ± 10.5 | 67.2 ± 10.7 | 69.0 ± 9.3 | 0.003 |
| Males, n (%) | 1101 (82.0) | 781 (80.8) | 320 (85.1) | 0.024 |
| Body mass index (kg/m2) | 27.2 ± 4.0 | 27.1 ± 3.9 | 27.5 ± 4.0 | 0.135 |
| Coronary risk factors, n (%) | ||||
| Diabetes mellitus | 409 (30.5) | 258 (26.7) | 151 (40.2) | < 0.001 |
| Hypertension | 691 (51.5) | 468 (48.4) | 223 (59.3) | < 0.001 |
| Dyslipidemia | 849 (63.3) | 589 (61.0) | 260 (69.1) | 0.006 |
| Current or previous smoking | 324 (24.1) | 244 (25.3) | 80 (21.3) | 0.144 |
| Family history of CAD | 431 (32.1) | 309 (32.0) | 122 (32.4) | 0.923 |
| Obesitya | 310 (23.1) | 220 (22.8) | 90 (23.9) | 0.703 |
| Medical history of CV disease, n (%) | ||||
| Prior PCI | 735 (54.8) | 552 (57.1) | 183 (48.7) | 0.006 |
| Prior CABG | 431 (32.1) | 309 (32.0) | 122 (32.4) | 0.923 |
| Prior MI | 746 (55.6) | 570 (59.0) | 176 (46.8) | < 0.001 |
| Peripheral atheroma | 115 (8.6) | 64 (6.6) | 51 (13.6) | < 0.001 |
| Ischemic stroke | 35 (2.6) | 28 (2.9) | 7 (1.9) | 0.379 |
| Pacemaker | 2 (0.1) | 1 (0.1) | 1 (0.3) | 0.482 |
| Renal failureb | 16 (1.2) | 12 (1.2) | 4 (1.1) | 1.000 |
| Heart failure hospitalization | 31 (2.3) | 24 (2.5) | 7 (1.9) | 0.631 |
| Indications to stress CMR (multiple possible), n (%) | ||||
| PCI or CABG follow-upc | 1184 (88.2) | 830 (85.9) | 354 (94.1) | < 0.001 |
| Inconclusive stress test | 107 (8.0) | 65 (6.7) | 42 (11.2) | 0.01 |
| Inconclusive CCTAd | 110 (8.2) | 60 (6.2) | 50 (13.3) | < 0.001 |
| Cardiac rhythm, n (%) | ||||
| Sinus rhythm | 1151 (85.8) | 818 (84.7) | 333 (88.6) | |
| Sinus rhythm with extrasystoles | 185 (13.8) | 145 (15.0) | 40 (10.6) | 0.039 |
| Atrial fibrillation/supraventricular arrhythmias | 6 (0.4) | 3 (0.3) | 3 (0.8) | |
| LV ejection fraction, % | 45.8 ± 12.5 | 45.1 ± 12.5 | 47.7 ± 12.5 | < 0.001 |
| LV end-diastolic volume index, ml/m2 | 100.2 ± 31.3 | 102.2 ± 32.1 | 95.1 ± 28.4 | < 0.001 |
| LV end-systolic volume index, ml/m2 | 57.1 ± 27.4 | 58.9 ± 27.7 | 52.2 ± 25.8 | < 0.001 |
| LV mass, g/m2 | 73.8 ± 7.1 | 73.6 ± 7.2 | 73.5 ± 7.1 | 0.319 |
| RV ejection fraction, % | 57.2 ± 11.2 | 57.1 ± 11.3 | 57.3 ± 12.9 | 0.429 |
| Presence of LGE, n (%) | 689 (51.3) | 502 (52.0) | 187 (49.7) | 0.018 |
| Presence of viabilitye, n (%) | 280 (20.9) | 175 (18.1) | 105 (27.9) | < 0.001 |
| Number of segments of LGE | 2.3 ± 1.9 | 2.4 ± 1.9 | 2.2 ± 2.0 | 0.268 |
| Number of segments of myocardial ischemia | 0.7 ± 1.5 | 0.0 ± 0.0 | 2.5 ± 1.7 | < 0.001 |
| HR at baseline, beats/min | 67 ± 12 | 67 ± 12 | 71 ± 13 | 0.512 |
| HR at stress, beats/min | 91 ± 9 | 90 ± 9 | 96 ± 11 | 0.069 |
| RPP at baseline (k), mmHg-beats/min | 9.1 (7.5–10.6) | 9.0 (7.5–10.6) | 9.2 (7.5–11.0) | 0.621 |
| RPP at stress (k), mmHg-beats/min | 10.6 (9.0–12.4) | 10.4 (9.0–12.4) | 10.9 (9.5–12.8) | 0.193 |
Values are n (%), mean ± SD, or median (interquartile range)
BMI body mass index, CABG coronary artery bypass grafting, CAD coronary artery disease, CCTA coronary computed tomography angiography, CMR cardiovascular magnetic resonance, CV cardiovascular disease, GFR glomerular filtration rate, HF heart failure, HR heart rate, LGE late gadolinium enhancement, LV left ventricle, MI myocardial infarction, PCI percutaneous coronary intervention, RPP rate-pressure product (pressure mmHg x Heart rate bpm)/1000, RV right ventricle, SD standard deviation
aBMI ≥ 30 kg/m2
bGlomerular filtration rate < 60 ml/min/1.73 m2
cTo detect myocardial ischemia in asymptomatic patient every 3 to 5 years in accordance with ESC guidelines. (REF)
dCoronary stenosis of unknown significance on CCTA
ePresence of LGE with < 50% transmurality
Fig. 1.
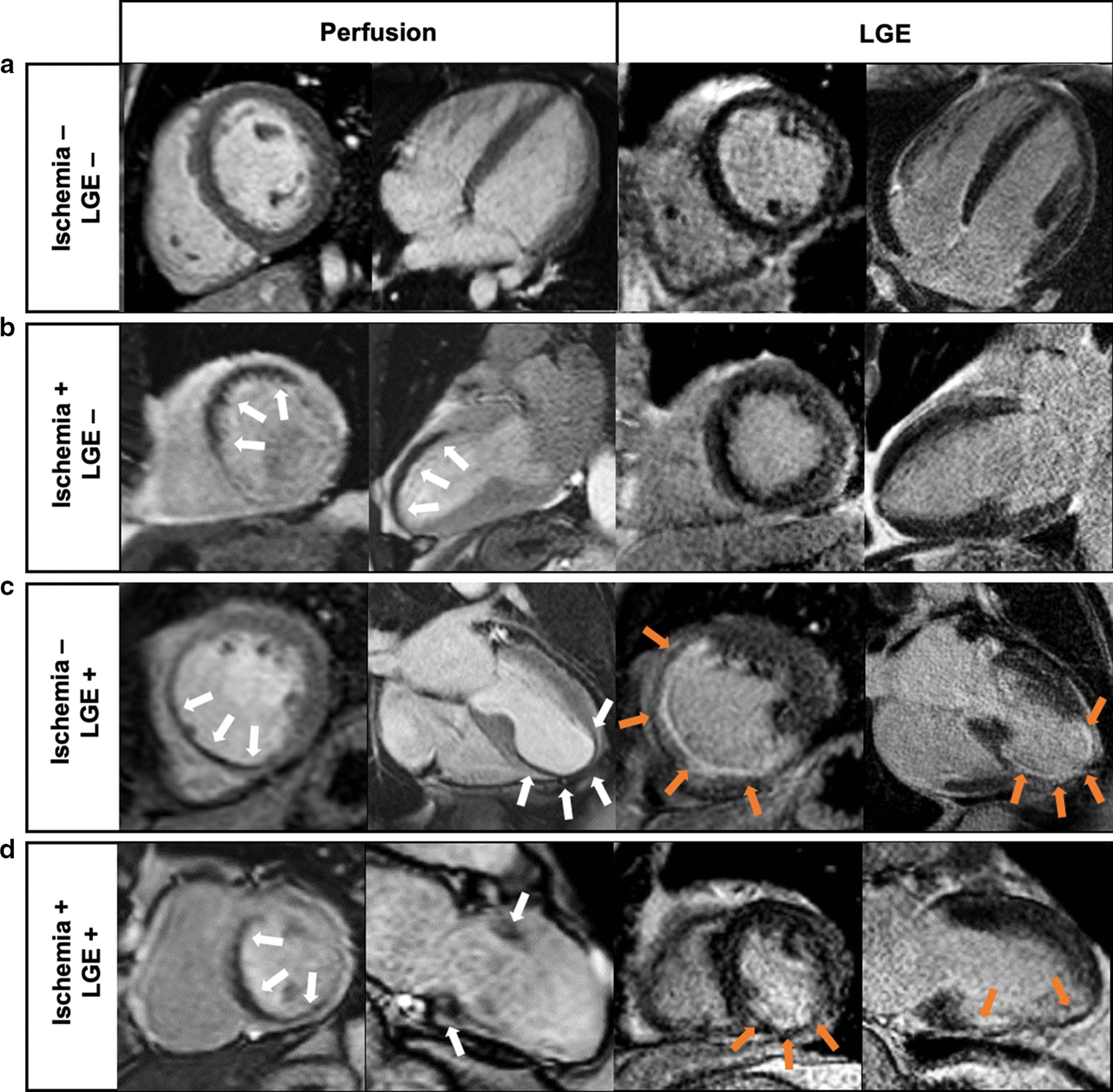
Examples of inducible myocardial ischemia on stress CMR in asymptomatic patients. a Normal. 58-year old male with hypertension and history of non-ST elevation myocardial infarctino (NSTEMI) treated by percutaneous coronary intervention (PCI) of the left anterior descending coreonary artery (LAD). Stress CMR revealed no perfusion defect and late gadolinium enhancement (LGE) was negative, ruling out the diagnosis of myocardial ischemia. b inducible ischemia. 62-year old female with a history of inferior NSTEMI treated by PCI of the right coronary artery (RCA). First-pass myocardial stress perfusion images revealed a reversible perfusion defect of the anteroseptal wall (white arrows) without LGE, indicative of myocardial ischemia suggestive of significant LAD stenosis, confirmed by coronary angiography. c myocardial scar without ischemia. 73-year old male with prior anterior STEMI treated by PCI of the LAD. Stress CMR showed a subendocardial antero-septo-apical scar on LGE (orange arrows), with a colocalization of the perfusion defect (white arrows) and, therefore, no inducible ischemia. Coronary angiography confirmed the absence of significant stenosis. d myocardial scar with ischemia. 66-year old male with a history of inferior STEMI treated by PCI of the RCA. Stress CMR showed a subendocardial scar on the inferior wall on LGE sequences (orange arrows), and a perfusion defect of the antero-septo-basal wall (white arrows) on first-pass perfusion images, indicative of inducible myocardial ischemia. Coronary angiography revealed high-grade stenoses of the LAD
Patients with myocardial ischemia were older (69.0 ± 9.3 vs. 67.7 ± 10.7 years, p = 0.003) and more frequently male (85.1% vs. 80.8%, p = 0.024). Of the 376 patients with myocardial ischemia, 267 (71.0%) had a coronary angiography with early revascularization < 90 days after CMR. Among those, 11 patients were censored due to the recurrence of MI or cardiovascular mortality within 90 days after CMR.
CMR study
Of 1529 asymptomatic patients with prior obstructive CAD, 1,466 (95.9%) completed the stress CMR protocol. Reasons for failure to complete CMR were claustrophobia (1.4%), intolerance to stress agent (0.7%), renal failure (0.7%), poor gating (0.7%) and declining participation (0.6%) (Additional file 1). No patient died during or shortly after CMR in relation with the study. There were two cases of unstable angina, one case of acute pulmonary edema and one patient with persistent atrial fibrillation. Detailed safety results are presented in Additional file 1.
Prognostic value
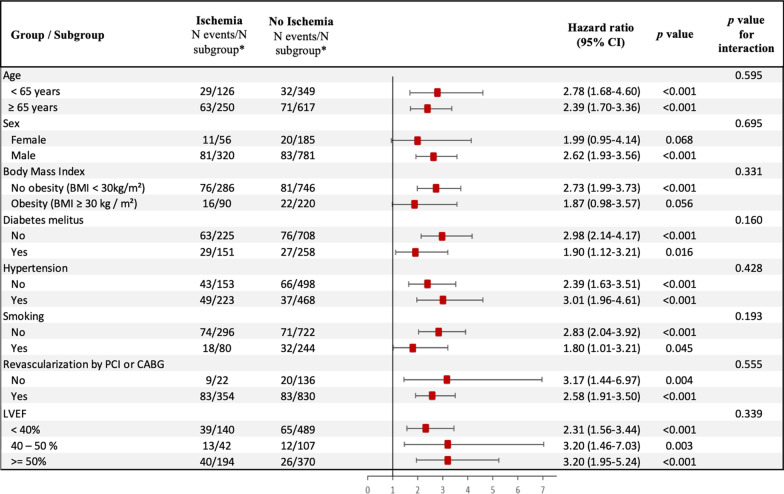
Median (IQR) follow-up was 8.3 (7.0–9.4) years. There were 195 MACE (13.3%), including 102 cardiovascular mortality (7.6%) and 93 non-fatal MI (6.9%). Furthermore, 190 all-cause mortality (14.2%), 172 late coronary revascularizations without emergency (12.8%) (6 CABG), 78 hospitalizations for heart failure (5.8%), and 23 sustained documented ventricular tachycardia (1.6%) were recorded. Annualized event rates were 6.7% for MACE, 2.3% for cardiovascular mortality, and 6.6% for all-cause mortality. The annualized event rates for MACE according to the presence or absence of myocardial ischemia and LGE are presented in Fig. 2. Patients without myocardial ischemia or LGE had a lower annualized rate of MACE (2.4%), whereas the annualized rate of MACE was greater for patients with both myocardial ischemia and LGE (14.6%) (p < 0.001). The annualized rates of MACE and cardiovascular mortality are depicted in Additional file 1 based on the presence and extent of myocardial ischemia. The annualized rate of MACE was higher for patients with moderate or severe ischemia than patients with mild ischemia (16.8%, 42.2% and 7.3%, respectively; ptrend < 0.001). The univariable analysis of baseline individuals and CMR characteristics for the prediction of MACE and cardiovascular mortality is shown in Table 2. Age, hypertension, the presence of myocardial ischemia, the number of ischemic segments, the presence of LGE, LVEF and both LV end-diastolic and end-systolic volumes indexed were all significantly associated with MACE. Using Kaplan–Meier analysis, myocardial ischemia and LGE were associated with the occurrence of MACE (HR 2.52; 95% CI 1.90–3.34 and HR 2.04; 95% CI 1.38–3.03, respectively; both p < 0.001) (Fig. 3). In addition, myocardial ischemia was associated with cardiovascular mortality (HR 2.52; 95% CI 1.90–3.34), non-fatal MI (HR 3.09; 95% CI 2.06–4.64), late coronary revascularization (HR 2.30; 95% CI 1.45–3.66) (all p < 0.001) and all-cause mortality (HR 1.55; 95% CI 1.15–2.08, p = 0.004; Additional file 1). The prognostic value of myocardial ischemia or LGE to predict MACE was not significantly different in men and women (p = 0.695, Fig. 4).
Fig. 2.
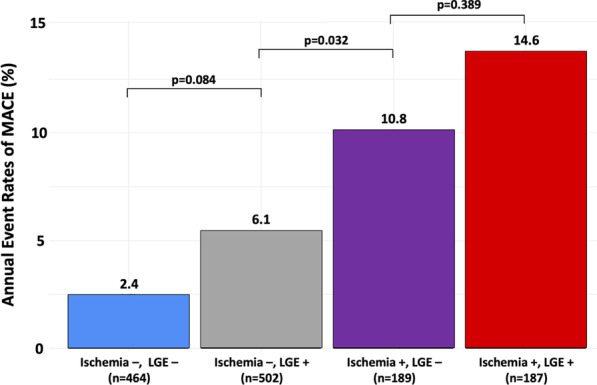
Annualized rates of MACE stratified by the presence of myocardial ischemia and LGE. Annual event rates (N = 1342) of MACE (cardiovascular mortality and non-fatal MI) for the entire study cohort
Table 2.
Univariable analysis of clinical and CMR characteristics for prediction of adverse events (N = 1342)
| MACE | Cardiovascular Mortality | |||
|---|---|---|---|---|
| Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | |
| Age | 1.02 (1.01–1.03) | 0.007 | 1.05 (1.03–1.07) | < 0.001 |
| Male | 1.18 (0.80–1.73) | 0.400 | 1.28 (0.74–2.22) | 0.374 |
| Body mass index | 0.96 (0.93–1.00) | 0.123 | 0.98 (0.93–1.01) | 0.382 |
| Hypertension | 0.73 (0.55–0.97) | 0.031 | 0.74 (0.50–1.09) | 0.127 |
| Diabetes mellitus | 0.91 (0.67–1.25) | 0.575 | 1.14 (0.75–1.71) | 0.546 |
| Dyslipidemia | 0.89 (0.66–1.18) | 0.408 | 0.76 (0.51–1.12) | 0.168 |
| Current or previous smoking | 1.09 (0.79–1.51) | 0.594 | 0.96 (0.61–1.52) | 0.861 |
| Family history of CAD | 0.88 (0.64–1.19) | 0.401 | 1.04 (0.69–1.57) | 0.846 |
| Prior PCI | 0.85 (0.64–1.13) | 0.263 | 0.56 (0.38–0.83) | 0.003 |
| Prior CABG | 0.88 (0.64–1.19) | 0.401 | 1.04 (0.69–1.57) | 0.846 |
| Stroke | 0.76 (0.28–2.05) | 0.592 | 0.74 (0.18–2.99) | 0.669 |
| Renal Failure | 0.42 (0.06–3.00) | 0.387 | 0.00 (0.00– + ∞) | 0.993 |
| Peripheral atheroma | 0.81 (0.47–1.39) | 0.442 | 1.01 (0.51–2.00) | 0.975 |
| Heart failure hospitalization | 1.40 (0.62–3.15) | 0.422 | 1.84 (0.68–5.01) | 0.231 |
| Presence of myocardial ischemia | 2.52 (1.90–3.34) | < 0.001 | 2.04 (1.38–3.03) | < 0.001 |
| Number of segments of myocardial ischemia | 1.47 (1.39–1.56) | < 0.001 | 1.40 (1.29–1.53) | < 0.001 |
| Presence of LGE | 1.66 (1.13–2.42) | 0.009 | 1.87 (1.08–3.24) | 0.025 |
| Number of segments of LGE | 1.35 (1.26–1.45) | < 0.001 | 1.38 (1.25–1.53) | < 0.001 |
| LVEF, per 10% | 0.84 (0.75–0.94) | 0.003 | 0.88 (0.75–1.03) | 0.101 |
| LV end-diastolic volume index, per 10 ml/m2 | 1.06 (1.02–1.11) | 0.006 | 1.05 (0.98–1.11) | 0.150 |
| LV end-systolic volume index, per 10 ml/m2 | 1.09 (1.03–1.14) | 0.001 | 1.07 (1.00–1.15) | 0.052 |
| RV ejection fraction, % | 0.92 (0.75–1.15) | 0.490 | 1.05 (0.78–1.48) | 0.980 |
CABG coronary artery bypass grafting, CAD coronary artery disease, CI confidence interval, CMR cardiovascular magnetic resonance, HF heart failure, LGE late gadolinium enhancement, LV left ventricle, LVEF left ventricular ejection fraction, MACE major adverse cardiac events, MI myocardial infarction, PCI percutaneous intervention, RV right ventricle
Fig. 3.
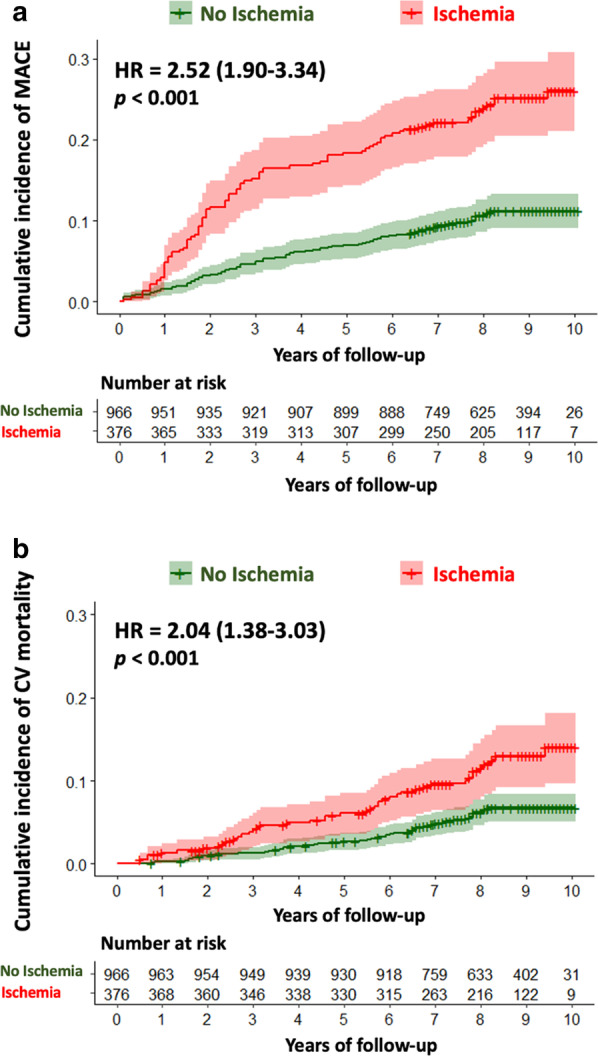
Kaplan–Meier curves for MACE and cardiovascular mortality. Kaplan Meier curves of MACE (cardiovascular mortality or non-fatal MI) (a) and cardiovascular mortality (b) as a function of length of follow-up in patients with and without myocardial ischemia
Fig. 4.
Subgroup analysis. Forest-plot of incidence of MACE based on the presence of myocardial ischemia in prespecified subgroups. *N events/N subgroup: number of patients had a major adverse clinical events (MACE)/number of patients in the subgroup
In multivariable stepwise Cox regression (model 2), the presence of myocardial ischemia and LGE were independent predictors of a higher incidence of MACE (HR 2.80 95% CI 2.10–3.73, p < 0.001 and HR 1.51; 95% CI 1.01–2.27, p = 0.045; respectively) and cardiovascular mortality (HR 2.20 95% CI 1.47–3.28, p < 0.001 and HR 2.07; 95% CI 1.13–3.78, p = 0.018; respectively) (Table 3). In competitive risk analysis, the presence of myocardial ischemia was independently associated with non-fatal MI and cardiovascular mortality (both p < 0.001) (Additional file 1). The prognostic value of myocardial ischemia remained consistent in different subsamples of clinical interest such as diabetics and non-diabetics (Fig. 4). The presence and extent of myocardial ischemia remained associated with MACE in each age category (Fig. 5).
Table 3.
Multivariable cox regression analysis for the prediction of adverse events (N = 1342)
| MACE | Cardiovascular Mortality | |||
|---|---|---|---|---|
| Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | |
| Model 1a | ||||
| Age | 1.03 (1.01–1.04) | < 0.001 | 1.06 (1.04–1.08) | < 0.001 |
| Hypertension | 0.72 (0.54–0.96) | 0.026 | 0.70 (0.47–1.04) | 0.073 |
| Dyslipidemia | – | – | 0.76 (0.51–1.12) | 0.168 |
| Prior PCI | – | – | 0.51 (0.34–0.76) | 0.001 |
| LVEF, per 10% | 0.87 (0.78–0.97) | 0.028 | 0.89 (0.76–1.05) | 0.211 |
| LV end-systolic volume index, per 10 ml/m2 | 1.10 (1.05–1.16) | < 0.001 | 1.13 (1.05–1.21) | < 0.001 |
| Model 2b | ||||
| Presence of myocardial ischemia | 2.80 (2.10–3.73) | < 0.001 | 2.20 (1.47–3.28) | < 0.001 |
| Presence of LGE | 1.51 (1.01–2.27) | 0.045 | 2.07 (1.13–3.78) | 0.018 |
| Model 3c | ||||
| Age | 1.03 (1.01–1.04) | < 0.001 | 1.06 (1.03–1.08) | < 0.001 |
| Male | 1.17 (0.79–1.72) | 0.424 | 1.25 (0.72–2.17) | 0.424 |
| Body mass index | 0.98 (0.94–1.00) | 0.233 | 0.95 (0.63–1.52) | 0.851 |
| Hypertension | 0.72 (0.53–0.98) | 0.037 | 0.68 (0.44–1.03) | 0.068 |
| Diabetes mellitus | 0.95 (0.69–1.31) | 0.748 | 1.23 (0.80–1.88) | 0.344 |
| Dyslipidemia | 0.97 (0.72–1.31) | 0.831 | 0.78 (0.52–1.19) | 0.251 |
| Current or previous smoking | 1.13 (0.81–1.58) | 0.477 | 1.17 (0.72–1.88) | 0.523 |
| LVEF, per 10% | 0.81 (0.72–0.92) | < 0.001 | 0.83 (0.70–0.98) | 0.024 |
| Model 4d | ||||
| Presence of myocardial ischemia | 2.85 (2.13–3.81) | < 0.001 | 2.16 (1.44–3.24) | < 0.001 |
| Presence of LGE | 0.98 (0.97–0.99) | 0.005 | 1.89 (1.05–3.41) | 0.034 |
aCovariates in the model 1 by stepwise variable selection with entry and exit criteria set at the p ≤ 0.2 level:
for MACE: age, hypertension, LVEF per 10% and LV end-systolic volume index, per 10 ml/m2.
for CV mortality: age, hypertension, dyslipidemia, previous PCI, LVEF per 10% and LV end-systolic volume index, per 10 ml/m2.
bCovariates in the model 2: model 1 + presence of myocardial ischemia and LGE
cCovariates in the model 3 were traditional cardiovascular risk factors: age, male, BMI, hypertension, diabetes mellitus, current or previous smoking, dyslipidemia and LVEF per 10%
dCovariates in the model 4: model 3 + presence of myocardial ischemia and LGE
CI confidence interval, EDVi end-diastolic volume index, ESVi end-systolic volume index, HR hazard ratio, LGE late gadolinium enhancement, MACE major adverse cardiac events, LV left ventricle, LVEF left ventricular ejection fraction
Fig. 5.
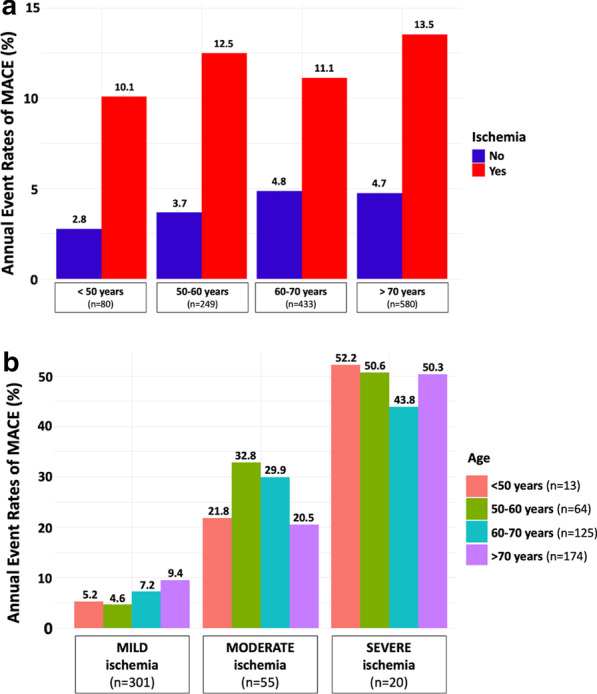
Annualized event rates of MACE stratified by age, presence/absence and the amount of myocardial ischemia. Annualized event rates of MACE are stratified by presence/absence of myocardial ischemia (a) and the amount of myocardial ischemia (b) in different age categories: < 50 years; 50–60 years; 60–70 years and > 70 years. Mild, moderate, and severe myocardial ischemia were defined as the involvement of 1–2, 3–5, and ≥ 6 myocardial segments, respectively
Incremental prognostic value of CMR
Model 1 with stepwise variable selection had a baseline C statistic value of 0.61 (95% CI 0.57–0.64) for predicting MACE, whereas model 3 including traditional cardiovascular risk factors had a C statistic value of 0.68 (95% CI 0.61–0.71). The addition of CMR–induced myocardial ischemia and LGE significantly improved the C statistic of model 1 to 0.68 (95% CI 0.62–0.71; C statistic improvement for model 1: 0.07; NRI = 0.207; IDI = 0.021) and of model 3 to 0.72 (95% CI 0.67–0.78; C statistic improvement for model 2: 0.04; NRI = 0.359; IDI = 0.065) (Additional file 1).
Discussion
In asymptomatic patients with known CAD referred for stress CMR, the presence of myocardial ischemia and LGE were independent long-term predictors of MACE and cardiovascular mortality. Furthermore, the presence of myocardial ischemia and LGE improved model discrimination in predicting MACE, after adjusting for covariates or traditional cardiovascular risk factors.
The prevalence of myocardial ischemia and LGE was 28.0% and 51.3%, respectively, which is consistent with previous studies in patients with known CAD [4, 13]. In agreement with others, the prevalence of myocardial ischemia was higher in diabetics (36.9%) [24, 25]. Of note, myocardial ischemia and LGE remained good prognosticators in different clinical subgroups, including diabetic and non-diabetic patients, obese and nonobese patients, with or without prior revascularization, and regardless of sex or LVEF, thereby extending the aggregate data on the prognostic value of stress CMR [9, 10, 17, 18]. Besides the presence of myocardial ischemia, the current report shows the prognostic value of the extent of myocardial ischemia in these patients, which concur with previous reports [13]. Similar to other studies, the presence of LGE was an independent predictor of MACE in the current study [26]. Moreover, the safety profile of stress CMR was excellent, as described in a registry of > 11,000 patients with a significant proportion of asymptomatic patients with prior CAD [27].
Whereas the interest of coronary revascularization has been recently debated in patients with stable CAD [3], some studies have suggested potential clinical interest of coronary revascularization in asymptomatic patients with documented myocardial ischemia [28]. A large study of 1,473 patients with objective myocardial ischemia showed a significant reduction in cardiovascular mortality at > 5 years in the revascularization group as compared with the medical therapy group (25 vs. 34%) [29]. Interestingly, patients who received initial revascularization for myocardial ischemia and who had documented residual ischemia on follow-up stress testing had a higher cardiovascular mortality rate [30]. Although the current guidelines do not recommend systematic stress testing in asymptomatic patients with prior CAD, the current data show the incremental prognostic value of stress perfusion CMR over traditional risk factors in these patients. Recent studies have shown promizing new therapy strategies targeting inflammation and coagulation to decrease the risk of recurrent CV events in patients with CAD [30, 31]. An improved risk stratification using stress CMR could allow to identify high-risk patients who could benefit from treatment intensification, new therapy and/or revascularization.
Study limitations
Our study has several limitations. First, 124 (8.5%) patients were lost to follow-up, which can be explained by a relatively long follow-up and the design of the study. However, the French National Registry of Death was carefully reviewed, which strengthens the mortality data. The analysis of the CMR perfusion scans was visual but it represents the most widely accepted clinical method with optimal diagnostic accuracy. Although adenosine is commonly used for stress perfusion CMR, dipyridamole was used in our center between 2009 and 2011 mainly because of medico-economic reasons and similar or very close efficacy/safety profile compared to adenosine.
Conclusions
In this large monocenter study, vasodilator stress perfusion CMR has accurate discriminative long-term prognostic value in asymptomatic patients with known CAD. Myocardial ischemia and LGE are independently associated with cardiovascular mortality or non-fatal MI over a long-term follow-up and offer incremental prognostic value over traditional CAD risk factors. The clinical implications of improved risk stratification on diagnostic and therapeutic decision making remain to be evaluated in this population.
Supplementary Information
Additional file 1: Supplement 1: Study flowchart. Supplement 2: Safety results. Supplement 3: Annualized event rates of MACE (A) and Cardiovascular mortality (B) stratified by the extent of myocardial ischemia (N = 1342). Supplement 4: Table. Univariable analysis of myocardial ischemia for prediction of adverse events (N = 1342). Supplement 5: Competitive risk analysis. Supplement 6: Table. Univariable and Multivariable Competing Risk Regression Analysis (N = 1342). Supplement 7: Table. Discrimination and reclassification associated with myocardial ischemia and LGE for prediction of MACE (N = 1342).
Acknowledgements
We thank the medical, paramedical and research staff of Hôpital Privé J. CARTIER.
Abbreviations
- BMI
Body mass index
- bSSFP
Balanced steady state free precession
- CABG
Coronary artery bypass grafting
- CAD
Coronary artery disease
- CI
Confidence interval
- CIF
Cumulative incidence function
- CMR
Cardiovascular magnetic resonance
- ECG
Electrocardiogram
- HR
Hazard ratio
- IDI
Integrative discrimination index
- LGE
Late gadolinium enhancement
- LV
Left ventricle/left ventricular
- LVEF
Left ventricular ejection fraction
- MACE
Major adverse cardiovascular event
- MI
Myocardial infarction
- NRI
Net reclassification index
- PCI
Percutaneous coronary intervention.
- RPP
Rate pressure product
- SD
Standard deviation
Authors’ contributions
All authors participated in the discussion of the concept of the study. TP and JG conceived the study design. TP, FS, MK, TH, SC, TU, PG and JG, obtained CMR images and analyzed CMR scans. TP and JG analyzed data and drafted the manuscript with critical revision. JG and ST have technically defined the CMR protocol. As authors, we attest to each of our substantial contributions to the manuscript and revision. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
The study was evaluated and approved by the local ethic committee of our institutions and conducted in accordance with the 1964 Declaration of Helsinki. All patients enrolled in this study were required to understand and give their consent for participation.
Consent for publication
Not applicable.
Competing interests
Solenn Toupin is an employee of Siemens Healthcare. The authors declare no conflict of interest and no financial disclosure in relation to this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12968-021-00721-8.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz HM, Normand S-LT, Wang Y. Twenty-year trends in outcomes for older adults with acute myocardial infarction in the United States. JAMA Netw Open. 2019;2(3):e191938. doi: 10.1001/jamanetworkopen.2019.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–1407. doi: 10.1056/NEJMoa1915922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anand DV, Lim E, Raval U, Lipkin D, Lahiri A. Prevalence of silent myocardial ischemia in asymptomatic individuals with subclinical atherosclerosis detected by electron beam tomography. J Nucl. 2004;11(4):450–457. doi: 10.1016/j.nuclcard.2004.06.125. [DOI] [PubMed] [Google Scholar]
- 5.Biagini E, Schinkel AFL, Bax JJ, Rizzello V, van Domburg RT, Krenning BJ, et al. Long term outcome in patients with silent versus symptomatic ischaemia during dobutamine stress echocardiography. Heart Br Card Soc. 2005;91(6):737–742. doi: 10.1136/hrt.2004.041087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deedwania PC, Carbajal EV. Silent ischemia during daily life is an independent predictor of mortality in stable angina. Circulation. 1990;81(3):748–756. doi: 10.1161/01.CIR.81.3.748. [DOI] [PubMed] [Google Scholar]
- 7.Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina–summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina) Circulation. 2003;107(1):149–158. doi: 10.1161/01.CIR.0000047041.66447.29. [DOI] [PubMed] [Google Scholar]
- 8.Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 9.Heitner JF, Kim RJ, Kim HW, Klem I, Shah DJ, Debs D, et al. Prognostic value of vasodilator stress cardiac magnetic resonance imaging: a multicenter study with 48,000 patient-years of follow-up. JAMA Cardiol. 2019;4(3):256–264. doi: 10.1001/jamacardio.2019.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwong RY, Ge Y, Steel K, Bingham S, Abdullah S, Fujikura K, et al. Cardiac magnetic resonance stress perfusion imaging for evaluation of patients with chest pain. J Am Coll Cardiol. 2019;74(14):1741–1755. doi: 10.1016/j.jacc.2019.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nagel E, Greenwood JP, McCann GP, Bettencourt N, Shah AM, Hussain ST, et al. Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med. 2019;380(25):2418–2428. doi: 10.1056/NEJMoa1716734. [DOI] [PubMed] [Google Scholar]
- 12.Bodi V, Sanchis J, Lopez-Lereu MP, Nunez J, Mainar L, Monmeneu JV, et al. Prognostic and therapeutic implications of dipyridamole stress cardiovascular magnetic resonance on the basis of the ischaemic cascade. Heart Br Card Soc. 2009;95(1):49–55. doi: 10.1136/hrt.2007.139683. [DOI] [PubMed] [Google Scholar]
- 13.Vincenti G, Masci PG, Monney P, Rutz T, Hugelshofer S, Gaxherri M, et al. Stress perfusion CMR in patients with known and suspected CAD. JACC Cardiovasc Imaging. 2017;10(5):526–537. doi: 10.1016/j.jcmg.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72(18):2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 15.Hicks KA, Tcheng JE, Bozkurt B, Chaitman BR, Cutlip DE, Farb A, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials. J Am Coll Cardiol. 2015;66(4):403–469. doi: 10.1016/j.jacc.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 16.Stone GW, Ben-Yehuda O, Sabik JF, Kappetein AP, Serruys PW. Considerations for an optimal definition of procedural myocardial infarction. Eur Heart J. 2020;41(17):1704–1705. doi: 10.1093/eurheartj/ehaa185. [DOI] [PubMed] [Google Scholar]
- 17.Pezel T, Sanguineti F, Kinnel M, Hovasse T, Garot P, Unterseeh T, et al. Prognostic value of dipyridamole stress perfusion cardiovascular magnetic resonance in elderly patients >75 years with suspected coronary artery disease. Eur Heart J Cardiovasc Imaging. 2020;5:193. doi: 10.1093/ehjci/jeaa193. [DOI] [PubMed] [Google Scholar]
- 18.Kinnel M, Garot J, Pezel T, Hovasse T, Unterseeh T, Champagne S, et al. Prognostic value of vasodilator stress perfusion CMR in morbidly obese patients (BMI ≥40 kg/m2) without known CAD. JACC Cardiovasc Imaging. 2020;13(5):1276–1277. doi: 10.1016/j.jcmg.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–542. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 20.Schwitter J, Wacker CM, Wilke N, Al-Saadi N, Sauer E, Huettle K, et al. MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J. 2013;34(10):775–781. doi: 10.1093/eurheartj/ehs022. [DOI] [PubMed] [Google Scholar]
- 21.Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005;26(15):1461–1474. doi: 10.1093/eurheartj/ehi258. [DOI] [PubMed] [Google Scholar]
- 22.Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343(20):1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 23.Uno H, Tian L, Cai T, Kohane IS, Wei LJ. A unified inference procedure for a class of measures to assess improvement in risk prediction systems with survival data. Stat Med. 2013;32(14):2430–2442. doi: 10.1002/sim.5647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zellweger MJ, Haaf P, Maraun M, Osterhues HH, Keller U, Müller-Brand J, et al. Predictors and prognostic impact of silent coronary artery disease in asymptomatic high-risk patients with diabetes mellitus. Int J Cardiol. 2017;244:37–42. doi: 10.1016/j.ijcard.2017.05.069. [DOI] [PubMed] [Google Scholar]
- 25.Zellweger MJ. Prognostic significance of silent coronary artery disease in type 2 diabetes. Herz. 2006;31(3):240–245. doi: 10.1007/s00059-006-2790-1. [DOI] [PubMed] [Google Scholar]
- 26.Nordenskjöld AM, Hammar P, Ahlström H, Bjerner T, Duvernoy O, Lindahl B. Unrecognized myocardial infarction assessed by cardiac magnetic resonance imaging is associated with adverse long-term prognosis. PLoS ONE. 2018;13(7):e0200381. doi: 10.1371/journal.pone.0200381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Monmeneu Menadas JV, Lopez-Lereu MP, Estornell Erill J, Garcia Gonzalez P, Igual Muñoz B, Maceira GA. Pharmacological stress cardiovascular magnetic resonance: feasibility and safety in a large multicentre prospective registry. Eur Heart J Cardiovasc Imaging. 2016;17(3):308–315. doi: 10.1093/ehjci/jev153. [DOI] [PubMed] [Google Scholar]
- 28.Gada H, Kirtane AJ, Kereiakes DJ, Bangalore S, Moses JW, Généreux P, et al. Meta-analysis of trials on mortality after percutaneous coronary intervention compared with medical therapy in patients with stable coronary heart disease and objective evidence of myocardial ischemia. Am J Cardiol. 2015;115(9):1194–1199. doi: 10.1016/j.amjcard.2015.01.556. [DOI] [PubMed] [Google Scholar]
- 29.Choi KH, Lee JM, Park I, Kim J, Rhee T-M, Hwang D, et al. Comparison of long-term clinical outcomes between revascularization versus medical treatment in patients with silent myocardial ischemia. Int J Cardiol. 2019;277:47–53. doi: 10.1016/j.ijcard.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 31.Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319–1330. doi: 10.1056/NEJMoa1709118. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplement 1: Study flowchart. Supplement 2: Safety results. Supplement 3: Annualized event rates of MACE (A) and Cardiovascular mortality (B) stratified by the extent of myocardial ischemia (N = 1342). Supplement 4: Table. Univariable analysis of myocardial ischemia for prediction of adverse events (N = 1342). Supplement 5: Competitive risk analysis. Supplement 6: Table. Univariable and Multivariable Competing Risk Regression Analysis (N = 1342). Supplement 7: Table. Discrimination and reclassification associated with myocardial ischemia and LGE for prediction of MACE (N = 1342).
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].