Abstract
Background
Coronavirus disease 2019 (COVID‐19) is associated with high rates of thromboembolic events in hospitalized patients. It remains to be determined if this risk persists following hospital discharge.
Methods
We conducted a retrospective cohort study of outpatients recently hospitalized for COVID‐19 to determine the incidence of vascular thromboembolic events within 30 days of discharge. We investigated the risk factors associated with these events, including intensive care admission, age, and anticoagulation.
Results
Among 447 patients hospitalized for COVID‐19, 2.0% experienced a vascular thromboembolic event within 30 days of discharge. No risk factor variable was significantly associated with an increased risk for these events.
Conclusions
The incidence of vascular thromboembolic events following hospital discharge for COVID‐19 is low. These findings suggest against the routine use of postdischarge thromboprophylaxis in patients with COVID‐19.
Keywords: anticoagulant, COVID‐19, discharge, outpatients, thromboembolism
Essentials.
Coronavirus disease 2019 is associated with increased risk of thrombosis in hospitalized patients.
There are limited data on whether this risk persists after discharge.
The incidence of vascular thromboembolic events in recently hospitalized outpatients is low.
The role of routine postdischarge thromboprophylaxis is unsupported.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is associated with a high incidence of vascular thromboembolic events (VaTEs) in hospitalized patients; 1 however, there are currently limited data on the incidence of VaTEs following hospital discharge. 2 , 3 , 4 The National Institutes of Health has issued guidelines recommending that postdischarge thromboprophylaxis be considered in certain high‐risk patients, such as the elderly and patients with active malignancy or prior history of venous thromboembolism (VTE). 5 It remains uncertain whether the severity of COVID‐19 is an independent risk factor for these events. We report the incidence of postdischarge venous and arterial thromboembolism after hospital admission for COVID‐19 at our institution and investigated the risk factors associated with outpatient VaTEs.
2. METHODS
Our study population consisted of patients hospitalized for COVID‐19 at 1 of 11 hospitals in the University of North Carolina Health system and discharged between March 15 and July 4, 2020. COVID‐19 was confirmed by the presence of a positive qualitative polymerase chain reaction test for severe acute respiratory distress syndrome coronavirus 2 obtained from nasopharyngeal or oropharyngeal swab samples. We excluded patients who died, were discharged to hospice or comfort care, screened positive when hospitalized for an unrelated condition, or were discharged on therapeutic anticoagulation for another indication.
The study outcome was the diagnosis of a VaTE within 30 days of hospital discharge. This included deep vein thrombosis, pulmonary embolism, superficial thrombophlebitis, myocardial infarction, ischemic stroke, and systemic arterial thromboembolism. VaTEs were identified through documentation of an associated International Classification of Diseases, Tenth Revision code within the electronic medical record and were subsequently validated by manual chart review of all records. We report outcomes as incidence rates for the entire study population. Logistic regression was used to evaluate the association of risk factors with the development of a VaTE within 30 days of hospital discharge. The risk factors included in the final model were age, intensive care unit (ICU) admission during hospitalization, and anticoagulation at discharge.
3. RESULTS
A total of 447 patients met the inclusion criteria. Background characteristics for the cohort are outlined in Table 1. One hundred seventy‐six (39.4%) patients required treatment in the ICU during hospitalization for COVID‐19. One hundred ninety (42.5%) patients were discharged on prophylactic anticoagulation. Of these patients, 171 (90%) received a direct oral anticoagulant.
TABLE 1.
Background characteristics
| Required ICU | Did not require ICU | Overall cohort | |
|---|---|---|---|
| Total number | 176 | 271 | 447 |
| Average age, y | 53.5 ± 18.2 | 55 ± 17.6 | 54.4 ± 17.9 |
| Female, n (%) | 75 (42.6) | 142 (52.4) | 217 (48.5) |
| Anticoagulated at discharge, n (%) | 62 (35.2) | 128 (47.2) | 190 (42.5) |
| Duration of initial hospitalization, d | 11.7 ± 11.6 | 5.5 ± 5.0 | 8.0 ± 8.8 |
| Venous thromboembolic events | 2 | 1 | 3 |
| Arterial thromboembolic events | 4 | 2 | 6 |
| Total VaTEs, n (%) | 6 (3.4) | 3 (1.1) | 9 (2.0) |
| 30‐day postdischarge VaTE incidence in patients discharged on vs off anticoagulation, n (%) | 1/62 (1.6) vs | 1/128 (0.8) vs | 2/190 (1.1) vs |
| 5/114 (4.4) | 2/143 (1.4) | 7/257 (2.7) |
Abbreviations: ICU, intensive care unit; VaTE, vascular thromboembolic event.
Nine individuals (2.0%) experienced a VaTE within 30 days of hospital discharge. Events sustained included four non–ST‐segment myocardial infarctions, three pulmonary emboli, one ischemic stroke, and one splenic infarct. Although the difference was not statistically significant, the incidence of postdischarge VaTE was higher in patients who required intensive care during their initial hospitalization for COVID‐19 compared to those who did not (3.4% vs 1.1%, respectively; adjusted odds ratio [aOR], 3.08; 95% confidence interval [CI], 0.78‐15.02). The incidence of VaTE was 1.1% in those discharged on anticoagulation and 2.7% in those discharged without anticoagulation (aOR, 0.52; 95% CI, 0.08‐2.26). Unadjusted and adjusted odds ratios for the logistic regression model can be found in Table 2.
TABLE 2.
Logistic regression outcomes
| Variable | 30‐day incidence of postdischarge VaTE, n (%) | Unadjusted OR | Adjusted OR | |
|---|---|---|---|---|
| (95% CI) | (95% CI) | |||
| ICU during admission | No ICU | 3/271 (1.1) | ‐ | ‐ |
| ICU | 6/176 (3.4) | 3.15 (0.82‐15.10) P = .11 | 3.08 (0.78‐15.02) P = .12 | |
| Anticoagulation at discharge | No anticoagulation | 7/257 (2.7) | ‐ | ‐ |
| Anticoagulation | 2/190 (1.1) | 0.38 (0.06‐1.59) P = .23 | 0.52 (0.08‐2.26) P = .42 | |
| Age (per 10‐y increment) | ‐ | ‐ | 1.47 (0.98‐2.32) P = .08 | 1.47 (0.97‐2.38) P = .09 |
Abbreviations: CI, confidence interval; ICU, intensive care unit; OR, odds ratio; VaTE, vascular thromboembolic event.
4. DISCUSSION
We found that the incidence of postdischarge VaTE following admission for COVID‐19 is low but not negligible. Our findings are in line with published literature reporting a cumulative VaTE incidence of 2.5%, with VTE rates ranging from 0.14% to 0.6% following COVID‐19 hospital discharge. 2 , 3 , 4 Although we did not compare COVID to non‐COVID discharges, other studies have also reported low 30‐day postdischarge VTE incidence rates that do not significantly differ between medical patients with and without COVID‐19. 2 The incidence of VaTEs in our study was higher following ICU admission, but this increase was not statistically significant. Confirmation in larger studies is needed to determine if ICU admission has an effect on outpatient VaTEs.
This study has important limitations. Patients were not routinely screened for VaTEs and may have sought treatment for thrombotic complications outside the hospital system. These events may not have been captured by review of the electronic health record, leading to an underestimate of the true incidence. The designation of “symptomatic COVID‐19” was left to individual providers, which may have led to the inclusion of patients with symptoms attributable to another medical condition and incidentally COVID positive. Guidelines for prescribing outpatient thromboprophylaxis evolved over the course of the pandemic, which may have led to inconsistent application of our institutional protocol (Figure 1). It is possible that patients thought to be at higher risk for VaTEs were discharged on prophylactic anticoagulation and that this may have led to a low incidence of VaTEs in this group. While we attempted to adjust for significant confounders in our logistic regression model (age and ICU admission), it is possible that there were other unmeasured risk factors that contributed to differences in use of postdischarge anticoagulation. In addition, we considered whether higher inpatient anticoagulation dosing may have contributed to the low incidence of outpatient events, but we found a comparable rate of outpatient VaTEs as studies that used standard dose prophylaxis in inpatients. 2 , 3 , 4 Finally, the low number of VaTEs in our patient cohort, as well as the confounding influence of postdischarge anticoagulation, limited our ability to investigate the impact of other risk factors on the outcome. Future analyses are needed to study the role of risk stratification and postdischarge anticoagulation in patients hospitalized for COVID‐19.
FIGURE 1.
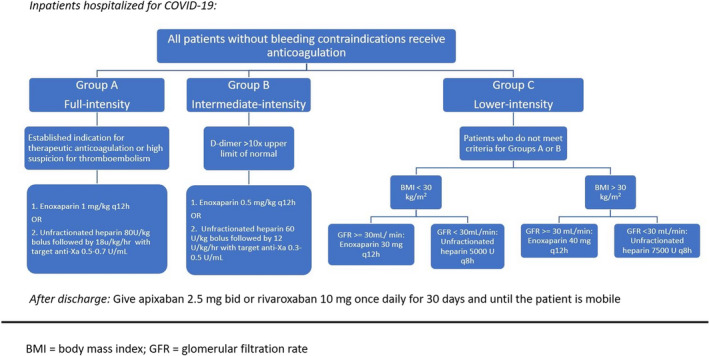
Institutional protocol for COVID‐19 thromboprophylaxis
In summary, post–hospital discharge occurrence of venous or arterial thrombosis in patients hospitalized for COVID‐19 infection is low, whether discharged with or without prophylactic anticoagulation. A randomized, controlled trial is needed to determine if the routine use of post–hospital discharge thromboprophylaxis is beneficial.
RELATIONSHIP DISCLOSURE
HE, JJ, AS, DM, TL, and DS declare no conflicts of interest. SM has been a consultant for Bristol‐Myers‐Squibb.
AUTHOR CONTRIBUTIONS
HE, JJ, AS, and SM designed the research and wrote the manuscript. HE, JJ, DM, TL, and DS obtained data and analyzed the results.
ACKNOWLEDGEMENTS
We thank the members of the UNC Health Alliance Population Health Services team for their support.
Eswaran H, Jarmul JA, Shaheen AW, et al. Vascular thromboembolic events following COVID‐19 hospital discharge: Incidence and risk factors. Res Pract Thromb Haemost. 2021;5:292–295. 10.1002/rth2.12485
Handling Editor: Dr Mary Cushman.
Contributor Information
Harish Eswaran, Email: harish.eswaran@unchealth.unc.edu.
Stephan Moll, @StephanHDMoll.
REFERENCES
- 1. Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID‐19. J Thromb Haemost. 2020;18:1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roberts LN, Whyte MB, Georgiou L, et al. Postdischarge venous thromboembolism following hospital admission with COVID‐19. Blood. 2020;136(11):1347–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patell R, Bogue T, Koshy A, et al. Postdischarge thrombosis and hemorrhage in patients with COVID‐19. Blood. 2020;136(11):1342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hill JB, Garcia D, Crowther M, et al. Frequency of venous thromboembolism in 6513 patients with COVID‐19: a retrospective study. Blood Adv. 2020;4(21):5373–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Institutes of Health . COVID‐19 treatment guidelines: Antithrombotic therapy in patients with COVID‐19. https://www.covid19treatmentguidelines.nih.gov/. Updated November 3, 2020. Accessed November 11, 2020


