Abstract
Objectives
To compare physical activity (PA) and sedentary behavior (SB) levels during work time between those who work from home (WFH) and at workplaces (no WFH), and by WFH subgroups.
Methods
This cross‐sectional internet‐based survey included 1239 workers (mean age [standard deviation], 44.7 [13.7] years; 59.2% men) living in the Tokyo Metropolitan Area. Time spent sitting (SB), standing (light‐intensity PA; LPA), walking, and engaging in heavy labor (moderate‐to‐vigorous PA; MVPA) during work time was measured using the Work‐related Physical Activity Questionnaire. Workers reported weekly WFH percentages (eg, 0% implies no WFH and 100% implies full WFH), and WFH percentages were categorized into no WFH (0% WFH) and WFH (1%‐100% WFH) groups. The WFH group was further subcategorized into 1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100% subgroups.
Results
Overall, 494 workers (39.9%) worked from home. During working hours, SB time was longer in the WFH group than in the no WFH group (mean minutes [% working‐time SB]: 335.7 vs 224.7 min [74% vs 50%]). Significantly shorter LPA and MVPA times (%) were reported in the WFH group than in the no WFH group (LPA, 59.6 vs 122.9 min [14% vs 29%]; MVPA, 55.3 vs 91.9 min [13% vs 22%], all P < .001). Among the WFH subgroups, longer SB time and shorter LPA and MVPA times were observed in the highest WFH group (WFH 76%‐100%) than in the WFH 1%‐25% and 26%‐50% subgroups.
Conclusions
Workers who telecommuted were less physically active and had longer sedentary during work time than those who worked at the workplaces.
Keywords: COVID‐19, physical activity, sedentary behavior, telework
1. INTRODUCTION
As of December 2020, the coronavirus disease 2019 (COVID‐19) pandemic remains one of the most major public health concerns worldwide. 1 Keeping one's physical distance in places where people gather, such as workplaces and public spaces, to mitigate person‐to‐person transmission is one of the pragmatic protective measures in the absence of an effective vaccine or treatment against the infectious disease. 2 , 3 In Japan, the Ministry of Internal Affairs and Communications has been promoting teleworking, including work from home (WFH) and mobile working. 4 During the current COVID‐19 pandemic, working from home is rapidly becoming the “new normal” working style for many workers. 4 , 5 , 6 Different workplaces have different office environments, and occupational physical activity (PA) and sedentary behavior (SB) levels differ across different workplaces. 7 Different office environments are associated with PA and SB levels among workers. 7 , 8 Therefore, PA/SB levels at work would be affected by the rapid change in the office environment from people's familiar workplaces to their own homes in the COVID‐19 pandemic. Because low levels of PA and high levels of SB are associated with increased mortality, 9 , 10 , 11 poor mental health, 12 and work‐related outcomes, such as presenteeism 13 and work productivity, 12 it is important to know how workers with WFH spend their working time in terms of PA and SB. To date, little is known about PA/SB levels among workers with WFH. To the best of our knowledge, only one study has examined the association between WFH and PA/SB, and reported that WFH is associated with greater sitting and screen time, but not PA time. 14 However, this previous study measured the total daily PA/SB levels; hence, the association of WFH with occupational PA/SB during work time remains unclear.
Therefore, we examined associations of WFH with occupational sitting time and intensity‐specific PA during work time.
2. METHODS
2.1. Participants and data collection
This was a cross‐sectional internet‐based survey that was conducted between July 28 and August 2, 2020, by a Japanese internet research company called MyVoice Communication, Inc Detailed sampling procedures have been described elsewhere. 15 Briefly, approximately 1.12 million individuals registered themselves in the company's database, which included their sociodemographic data. Data of 2400 men and women aged 20‐79 years were originally collected on February 25, 2020, according to gender and 10‐yearly age brackets (12 groups, n = 200 in each group). Subsequently, these fixed participants were followed up to the present survey wave. A series of these surveys were repeated every 5‐6 weeks to monitor the lifestyle of ordinary Japanese citizens during the COVID‐19 pandemic. The present data were obtained from the fifth wave of the series of these surveys. Participants were living in seven prefectures in the Tokyo Metropolitan Area (ie, Tokyo, Kanagawa, Saitama, Chiba, Ibaraki, Tochigi, and Gunma). During the first survey wave, there was a rapid increase in the number of laboratory‐confirmed COVID‐19 cases in the urban areas, especially in Tokyo. 16 Hence, the participants were sampled from the Tokyo Metropolitan Area. Information regarding occupational PA and SB was initially assessed in this fifth survey wave. Occupational PA and SB times were measured using the Work‐related Physical Activity Questionnaire (WPAQ). 17 WPAQ was only displayed for participants who had stated their latest job characteristics as full‐time jobs (eg, company employee, government worker), part‐time job, and self‐employed on the website. To examine the association between working from home and occupational PA with SB, self‐employed workers were excluded from the analyses. Rewards valued at 50 Yen (approximately 0.5 US Dollars as of July 2020) were provided as an incentive for participation. This study was approved by the Ethics Committee of Tokyo Medical University, Tokyo, Japan (No: T2019‐0234). Informed consent was obtained from all the respondents.
2.2. Assessment of the work from home status
Participants were asked: “What percentage of your work entails working from home? (0%, if all the work is done at the workplace; 100%, if all the work is done from home)?” These percentages were considered as continuous variables. Participants who reported 0% work were categorized into the “no WFH group,” and those who engaged in any amount (range 1%‐100%) of work from home into the “WFH group.” The no WFH group would potentially include essential workers (workers who are unable to work from home, eg, cleaners and helpers); hence, further analyses to examine the dose‐response manners of the amount of WFH for workers who could work from home were performed. Thus, those in the WFH group were further subdivided into four subcategories (1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100% reported WFH percentage).
2.3. Measures of occupational PA, SB, and SB bout length
We assessed time spent in PA, SB, and SB bout during work using the WPAQ, which has acceptable reliability and validity. 17 The WPAQ inquired about the usual working time and the proportion of sitting, standing, walking, and engaging in heavy labor during work. In calculating the time spent on each category, the proportion of each occupational activity was multiplied by the total minutes at work. With these questions, sitting time was regarded as being equivalent to SB; standing, for light‐intensity PA (LPA); walking, for moderate PA (MPA); and engaging in heavy labor, for vigorous PA (VPA). Time spent in MVPA was calculated by summing up the time spent in MPA and VPA. The duration of uninterrupted sitting time, which is associated with adverse health outcomes, 18 , 19 , 20 was also measured as sedentary bout length by the WPAQ. The WPAQ surveys the duration of SB bouts rather than the number of breaks per hour. 17 Previous studies usually asked for the number of breaks per hour 21 , 22 ; however, those questionnaires cannot provide sufficient information regarding the duration of each bout (ie, even if there are two breaks per hour, it is unclear whether the duration of the SB bouts are 10, 10, and 40 minutes, or whether they are all 20 minutes each). Specifically, in the WPAQ, participants were asked “At what minute intervals do you stand up when you sit down for work (eg, to get up for a photocopy, do another errand, stretch, or go to the restroom, etc)?” Participants selected their responses from “0, 10, 20, 30, 40, 50, 60, 70, 80, and ≥90 minutes.” The responses were treated as a quantitative variable (the response in the ≥90‐minute category was treated as 90) in the analysis.
2.4. Covariates
Demographic variables information, such as age, gender, current smoking (yes/no), regular drinking (every day or not), height, and weight, was obtained in the first survey wave. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Self‐rated health was measured using the question “How do you feel about your current health status?” and a response was selected from “excellent,” “good,” “fair,” or “very poor.” Self‐rated health was dichotomized into “excellent/good” or “fair/very poor” in the analyses. The internet research company also provided information regarding educational attainment (more than high school or less), residential area, job characteristics (full‐time or part‐time job). The Japan Standard Industrial Classification was also provided by the research company as categorized data, 23 and was reclassified as the first, second, and tertiary industries according to the Statistic Bureau, Ministry of Internal Affairs, and Communications classification. 23
2.5. Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Tokyo, Japan). For large studies (eg, >1000 participants), according to Fagerland, “t tests and their corresponding confidence intervals can and should be used even for heavily skewed data.” 24 Therefore, comparisons between the no WFH and WFH groups were conducted using Student's t test, while comparisons among WFH subgroups used analysis of variance and chi‐squared for continuous and categorical variables, respectively. The mean time spent in SB, LPA, MVPA, and SB bout length was compared not only between the no WFH and WFH groups but also among WHF subcategories using analysis of covariance, adjusted for age, gender, smoking status, drinking frequency, BMI, residential area (Tokyo/others), educational attainment, self‐rated health (good/bad), job characteristics, industrial classification (first, second, and tertiary industries), and working time (hours/day). For all analyses, P < .05 were considered as statistically significant.
3. RESULTS
Of the 2400 original participants in the first survey, 2362 participants remained registered for the fifth survey wave with the internet research company and 2155 were valid responses. Of the 2155 participants, 1365, including company employees and part‐time workers, had WPAQ displayed on the website to which they responded. Of the 1365 participants, 126 self‐employed participants were excluded. Finally, 1239 participants were included in the analyses.
Demographic characteristics are shown in Table 1. Four hundred and ninety‐four workers (39.9%) worked from home. Compared with the no WFH group, workers in the WFH group did not significantly differ in terms of age, smoking and alcohol consumption habit, BMI, and self‐rated health status. Compared with the no WFH group, men living in the Tokyo Metropolitan Area, with higher educational attainment, who were engaged in full‐time jobs were more frequently observed in the WHF group. Eight participants were engaged in the primary industry. Working hours and all sociodemographic variables were similar between the no WFH and the WFH groups.
TABLE 1.
Participant characteristics
| No WFH (n = 745) | WFH (n = 494) | p value a | Subgroups by the percentage of WFH (n = 494) | p value b | ||||
|---|---|---|---|---|---|---|---|---|
| 1%‐25% (n = 112) | 26%‐50% (n = 105) | 51%‐75% (n = 48) | 76%‐100% (n = 229) | |||||
| Age (years) | 44.7 (13.9) | 44.6 (13.5) | 0.83 | 43.0 (13.5) | 44.3 (13.8) | 44.0 (13.2) | 45.6 (13.5) | 0.42 |
| Gender | ||||||||
| Men | 396 (53.2%) | 338 (68.4%) | <0.001 | 78 (69.9%) | 73 (69.5%) | 36 (75.0%) | 151 (65.9%) | 0.63 |
| Women | 349 (46.8%) | 156 (31.6%) | 34 (30.4%) | 32 (30.5%) | 12 (25.0%) | 78 (34.1%) | ||
| Current Smoker | 118 (15.8%) | 93 (18.8%) | 0.17 | 21 (18.8%) | 22 (21.0%) | 13 (27.1%) | 37 (16.2%) | 0.32 |
| Regular drinker (every day) | 102 (13.7%) | 81 (16.4%) | 0.19 | 23 (20.5%) | 15 (14.3%) | 7 (14.6%) | 36 (15.7%) | 0.59 |
| BMI | 22.4 (3.5) | 22.2 (3.7) | 0.33 | 22.2 (4.0%) | 22.6 (3.5) | 21.5(2.9) | 22.2 (3.8) | 0.37 |
| Residential area | ||||||||
| Tokyo | 275 (36.9%) | 242 (49.0%) | <0.001 | 55 (49.1%) | 52 (49.5%) | 23 (47.9%) | 112 (48.9%) | >0.99 |
| Others | 470 (63.1%) | 252 (51.0%) | 57(50.9%) | 53 (50.5%) | 25 (52.1%) | 117 (51.1%) | ||
| Educational attainment | ||||||||
| More than high school | 519 (72.4%) | 430 (88.7%) | <0.001 | 97 (86.6%) | 91 (88.3%) | 44 (91.7%) | 198 (89.2%) | 0.81 |
| Up to high school | 198 (27.6%) | 55 (11.3%) | 15 (13.4%) | 12 (11.7%) | 4 (8.3%) | 24 (10.8%) | ||
| Self‐rated Health | ||||||||
| Excellent/good | 625 (83.9%) | 424 (85.8%) | 0.38 | 96 (85.7%) | 94 (89.5%) | 42 (87.5%) | 192 (83.8%) | 0.57 |
| Fair/very poor | 120 (16.1%) | 70 (14.2%) | 16 (14.3%) | 11 (10.5%) | 6 (12.5%) | 37 (16.2%) | ||
| Job characteristic | ||||||||
| Full‐time job | 490 (65.8%) | 455 (92.1%) | <0.001 | 104 (92.9%) | 96 (91.4%) | 46 (95.8%) | 209 (91.3%) | 0.73 |
| Part‐time job | 255 (34.2%) | 39 (7.9%) | 8 (7.1%) | 9 (8.6%) | 2 (4.2%) | 20 (8.7%) | ||
| Industrial classification | ||||||||
| Primary industry | 7 (1.0%) | 1 (0.2%) | 0.004 | 0 (0.0%) | 0 (0.0%) | 0 (0.0) | 1 (0.4) | 0.55 |
| Secondary industry | 129 (18.0%) | 122 (25.2%) | 25 (22.3%) | 26 (25.2%) | 17(35.4) | 54 (24.3) | ||
| Tertiary industry | 581 (81.0%) | 362 (74.6%) | 87 (77.7%) | 77 (74.8%) | 31 (64.6) | 167 (75.2) | ||
| Working time (hours) | 7.3 (2.1) | 7.5 (2.2) | 0.14 | 7.8 (2.2) | 7.3 (1.9) | 8.1 (1.7) | 7.4 (2.5) | 0.06 |
Values are presented as means (standard deviations) or n (%). Total number of participants is not always same because of missing values.
Abbreviations: WFH, work from home; BMI, body mass index.
p for Student's t test.
p for analysis of variance (ANOVA).
Descriptive statistics for occupational SB (sitting time), LPA (standing), and MVPA (walking and heavy labor) are shown as a crude model in Table 2. Times spent in SB during work time in the WFH group were significantly longer than those in the no WFH group (mean [standard deviation]: 224.7 [173.6] vs 335.7 [152.7] min, P <.001). Times spent in LPA and MVPA in the WFH group were significantly shorter than those in the no WFH group (LPA: 122.9 [118.2], vs 59.6 [69.4], MVPA: 91.9 [92.4] vs 55.3 [62.6] min, respectively). Similar patterns were observed in the proportions of SB, LPA, and MVPA. In the crude model, there was no significant difference in SB bout length between the no WFH and WFH groups. After adjusting for covariates (ie, the adjusted model in Table 2), the significant difference in SB bout length between the no WFH and WFH groups was confirmed, and the differences in SB, LPA, and MVPA time remained significant.
TABLE 2.
R1 Comparison of time and proportion of each behavior during working time between the no WFH and WFH groups
| Crude model | Adjusted model | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time spent in each behavior during working time (min) | Proportion of each behavior per working time (%) | Time spent in each behavior during working time (min) | Proportion of each behavior per working time (%) | |||||||||
| No WFH (n = 745) | WFH (n = 494) | p value | No WFH (n = 745) | WFH (n = 494) | p value | No WFH (n = 676) | WFH (n = 477) | p value | No WFH (n = 676) | WFH (n = 477) | p value | |
| SB | 224.7 (173.6) | 335.7 (152.7) | <0.001 | 49.5 (34.7) | 73.7 (23.9) | <0.001 | 179.7 (17.4) | 256.2 (18.7) | <0.001 | 37.1 (3.8) | 53.3 (4.0) | <0.001 |
| LPA | 122.9 (118.2) | 59.6 (69.4) | <0.001 | 29.0 (26.4) | 13.6 (15.5) | <0.001 | 146.5 (12.8) | 97.3 (13.7) | <0.001 | 34.6 (2.9) | 24.0 (3.1) | <0.001 |
| MVPA | 91.9 (92.4) | 55.3 (62.6) | <0.001 | 21.5 (20.3) | 12.7 (13.7) | <0.001 | 118.0 (10.3) | 90.7 (11) | <0.001 | 27.8 (2.3) | 21.8 (2.5) | <0.001 |
| SB bout length | 30.5 (25.4) | 42.8 (24.3) | 0.354 | ‐ | ‐ | 24.0 (3.2) | 33.6 (3.5) | <0.001 | ‐ | ‐ | ||
Values are presented as the means (standard deviations) in the crude (unadjusted) model according to Student's t test or the estimated mean (standard error) in the adjusted model according to analysis of covariance (ANCOVA). The ANCOVA was performed by adjusting for age, gender, smoking status, drinking frequency, body mass index, residential area (Tokyo/others), educational attainment, self‐rated health (good/bad), job characteristics, industrial classification (first, second, and tertiary industries), and working time (hours/day). WFH, work from home; SB, sedentary behavior; LPA, light‐intensity physical activity; MVPA, moderate‐to‐vigorous physical activity.
Figure 1 shows the comparisons of adjusted means of SB, LPA, MVPA, and sitting bout length among the subgroups categorized according to the degree of WFH. Compared with the less WFH groups, there were significant trends (all P for trend were <.05) for longer SB time and sitting bout length, and shorter LPA and MVPA time in the higher WFH groups. Post‐hoc analyses showed that SB time in the highest WFH group (76%‐100%) was the longest compared with the other groups (WFH 1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100%: 235.2 [38.4], 243.5 [38.8], 258.5 [40.2], and 3005.0 [37.5] min, respectively). Furthermore, LPA and MVPA were significantly shorter in the WFH 76%‐100% subgroup than in the WFH 1%‐25% and 26%‐50% subgroups, but not the WFH 51%‐75% subgroup (LPA; WFH 1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100%: 123.6 [24.1], 115.3 [24.4], 103.6 [25.3], and 82.8 [23.6] min, MVPA; WFH 1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100%: 95.3 [22.1], 95.2 [22.3], 91.9 [23.1], and 66.2 [21.6] min, respectively). Moreover, SB bout lengths in both the WFH 51%‐75% and 76%‐100% subgroups were significantly longer than those in the WFH 1%‐25% subgroup (WFH 1%‐25%, 26%‐50%, 51%‐75%, and 76%‐100%: 32.7 [8.6], 39.0 [8.7], 44.5 [9.0], and 42.2 [8.4] min, respectively).
FIGURE 1.
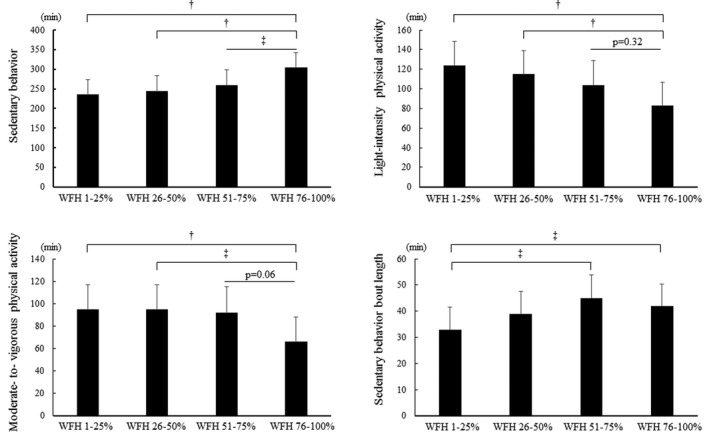
Comparisons of SB, intensity‐specific PA, and SB bout length during work among the different degree of WFH groups. SB, sedentary behavior; PA, physical activity; WFH, work from home. Values are presented as estimated means and standard error by analysis of covariance (ANCOVA), adjusted for age, gender, smoking, drinking frequency, body mass index (BMI), residential area, educational attainment, self‐rated health, job characteristics, industrial classification, and working time. Post hoc comparisons were examined using the Bonferroni method. †<.001, ‡<.05
4. DISCUSSION
Our results indicated that workers who worked from home spent less PA time and longer uninterrupted SB time during work time than those who never worked at home. To clarify the dose responses of WFH to PA/SB by excluding workers who were unable to work from home (eg, essential workers), we revealed that longer SB time and shorter LPA and MVPA times were more significantly observed in the highest WFH subgroup (WFH 76%‐100%) than in the WFH 1%‐25% and 26%‐50% subgroups. In addition, workers who reported >50% of WFH had significantly more prolonged, uninterrupted SB bouts during work in comparison with those in the lowest WFH subgroup (WFH 1%‐25%). Our findings suggest important concerns regarding the health risks of workers with less PA and longer SB times caused by WFH.
In this study, approximately 40% of workers worked from home. The telework implementation rate that was reported as 13.2% in March 2020 had doubled to 27.9% by April 2020. 5 , 25 In particular, the telework implementation rate in the Tokyo Metropolitan Area that was 18.5% in March 2020 had rapidly increased to 41.0%, suggesting similar telework implementation rates in our study sample compared with those of a previously reported study. 25 This was a very timely and important study that examined the association of WFH with PA and SB during the current rapid increase in telecommunication. 25
MVPA time during work in the WFH group was significantly shorter than that in the no WFH group. Reduced MVPA would usually be considered to be due to the absence of commuting from home to the office. However, the WPAQ was developed to assess the time spent in MVPA during work time. Hence, MVPA during commuting was not included in this reported MVPA time. Herein, we could suggest that the finding that WFH would decrease MVPA time during work time, apart from the reduction in MVPA time by commuting, is a remarkable result. Although the reasons are still unclear, it may be speculated that this could be due to the differences in environmental factors between the workplace and home, such as differences in the size of the office area and layout of the workplace (eg, perceived distance to a printer or coffee machine). 26 Additionally, the lunch time as well as commuting time to work were reported to be useful in accumulating (increasing) the total daily steps on workdays (ie, MVPA). 27 Workers with WFH may not need to go out for their lunch, particularly because of the present COVID‐19 pandemic.
The unadjusted SB time during work time in the no WFH group was 3.7 hours in this study. This result is similar to those of previous studies, which reported descriptive sitting times at worksite, measured by a questionnaire among full‐ and part‐time workers, of 2.0‐3.3 hours per working day. 28 , 29 , 30 The crude SB time in workers with WFH was >100 minutes (or >77 minutes using analysis of covariance to determine the estimated mean difference), longer than that in those who never worked from home. In addition, longer SB bout length was observed in the WFH groups compared to the no WFH group, and a dose‐response increase in SB bout length was also observed in the higher WFH groups. These findings suggest that workers with WFH may sit for prolonged SB time without interruption during work time. Teleworking has been reported to improve motivation and increase concentration, 31 and teleworkers would then achieve better performance without interruptions. 31 These might potentially explain the longer SB bout length in teleworkers with high percentage of WFH. SB bouts lasting >30 minutes are associated with adverse health outcomes, independently of the total time spent being sedentary. 18 , 19 , 20 In this study, the mean SB bout length was >30 minutes, regardless of the degree of WFH. It has been reported that alternating between uninterrupted sitting lasting for 30 minutes and standing could improve glucose metabolism and postprandial glucose responses in overweight/obese office workers. 20 This further suggests that intervention to break uninterrupted SB bouts would be needed for all workers, especially those in the high WFH group.
To increase PA and decrease SB, the working environment has been a practical target for health promotion programs. The longest SB time is observed during work time rather than during leisure time among white‐collar workers. 32 A survey reported that the proportion of workers who implemented telework for the first time was 47.8% in March 2020, and this increased to 68.7% in April 2020. 25 These findings suggest that many of the workers, newly and suddenly began telecommuting; therefore, the home office environments of workers may not be well developed in terms of workplace health promotion of better PA and SB levels. The use of active workstations is a powerful intervention 33 ; hence, the use of height‐adjustable desks (sit‐stand workstations) would be a useful interventional strategy for telecommuting workers to reduce SB and interrupt prolonged SB bouts, not only at their offices but also at home. In addition, a natural experimental study showed that office renovation by the introduction of activity‐based working and installation of height‐adjustable desks has a favorable effect on increasing PA as well as decreasing SB. 34 In addition to the above environmental interventions, other interventions for SB at the individual, social, and organizational levels have been suggested from the viewpoint of the ecological model. 35 Office workers habitually feel a barrier to interruption of their SB bout during work time once they are seated, since they fear being seen as unproductive by their manager and colleagues when they are not sitting at their desks. 36 In this regard, workers with WFH are more likely to interrupt sitting without worrying about their managers’ and colleagues’ perceptions. For instance, using the pop‐up prompt (computer prompt reminder) to inform workers of the need to interrupt SB bouts every 45 minutes has been shown to be an effective intervention at the individual level. 36 , 37 Moreover, online meetings would need computers or documents, and would make telecommuting workers sit uninterruptedly behind their computers. Managers and colleagues should encourage telecommuting workers to interrupt prolonged SB bouts during online meetings as a form of social and organizational‐level intervention. A recent consensus statement suggested that employees who engage in 2 hours of daily standing or LPA at work would progressively increase to 4 hours daily. 38 In a recent study, more than half of the workers expressed that they wanted to continue teleworking by the end of the COVID‐19 pandemic, 25 suggesting the need for further improvement of the home office environment.
A strength of our study was that we conducted this survey during a rapidly increasing telecommuting rate, during the COVID‐19 pandemic. Hence, our results provide initial results of PA and SB when the telecommuting home environment was not yet in place. The other strength was the use of a validated questionnaire (WPAQ) to assess occupational PA and SB during work time. Additionally, the WPAQ could be used to measure not only MVPA and SB but also LPA time and SB bout length, which are all associated with health outcomes. 19 , 20 , 39
There were some limitations to this study. First, the cross‐sectional design hampers causal inference. Second, we did not enquire about the pa limitation status. Workers with disabilities, especially those with mobility impairments, are more likely to work from home, and workers with disability have less pa and more SB. 40 Third, our web‐based study participants were limited to those who were registered with the research company involved in this study, which may lead to selection bias. Fourth, our internet survey participants would be familiar with using computers and they might spend more screen time during both work and leisure times, which might result in misclassification. Finally, our sample was collected from the Tokyo metropolitan area and is not entirely reflective of Japanese workers. WFH is more popular in the Tokyo metropolitan area than in the rural area. 6
5. CONCLUSIONS
Engaging in WFH was associated with less PA and longer SB time during work time, compared with working at worksites. Among workers who can work from home, the more they telecommute, the less they would be physically active and the more they would be sedentary during work time. Additionally, workers with WFH would be more exposed to having less MVPA time during work time, apart from the loss of MVPA by commuting to work. Our findings suggest the substantial need to promote better PA/SB levels for workers with WFH under the current situation where teleworking is rapidly increasing due to the COVID‐19 pandemic.
DISCLOSURE
Approval of the research protocol: This study was approved by the Ethics Committee of Tokyo Medical University, Tokyo, Japan (No: T2019‐0234). Informed consent: Informed consent was obtained from all respondents. Registry and the registration no. of the study/trial: N/A. Animal studies: N/A. Conflict of interest: The authors declare no conflict of interests for this article.
AUTHOR CONTRIBUTIONS
NF, MM, HK, and SI conceived the ideas; MM and HK collected the data; NF analyzed the data; NF led the writing; and all the authors revised the manuscript and approved the final version of the manuscript.
ACKNOWLEDGMENTS
This work was supported by a grant from the Meiji Yasuda Life Foundation of Health and Welfare. The authors wish to thank all the workers who participated in the survey.
Fukushima N, Machida M, Kikuchi H, et al. Associations of working from home with occupational physical activity and sedentary behavior under the COVID‐19 pandemic. J Occup Health. 2021;63:e12212. 10.1002/1348-9585.12212
REFERENCES
- 1. World Health Organization . Coronavirus disease (COVID‐19) pandemic, situation reports. 2020. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports. Accessed February 9, 2021.
- 2. Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Medicine. 2008;5:e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Qualls N, Levitt A, Kanade N, et al. Community mitigation guidelines to prevent pandemic influenza – United States. MMWR Recomm Rep. 2017;66(1):1‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Japanese Ministry of Internal Affairs and Communications . Information and communications policy. 2020. https://www.soumu.go.jp/main_sosiki/joho_tsusin/eng/index.html. Accessed February 9, 2021
- 5. Japanese Ministry of Internal Affairs and Communications . The 2020 White Paper on Information and Communications in Japan. 2020. https://www.soumu.go.jp/johotsusintokei/whitepaper/eng/WP2020/2020‐index.html. Accessed February 9, 2021
- 6. Japanese Ministry of Land, Infrastructure, Transport and Tourism . Telework population survey. 2019. 2020. https://www.mlit.go.jp/toshi/daisei/content/001338545.pdf. Accessed February 9, 2021. Japanese.
- 7. Hadgraft NT, Healy GN, Owen N, et al. Office workers' objectively assessed total and prolonged sitting time: individual‐level correlates and worksite variations. Prev Med Rep. 2016;4:184‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hipp JA, Reeds DN, van Bakergem MA, et al. Review of measures of worksite environmental and policy supports for physical activity and healthy eating. Prev Chronic Dis. 2015;12:E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ekelund U, Tarp J, Steene‐Johannessen J, et al. Dose‐response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta‐analysis. BMJ. 2019;366:l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;73:2062‐2072. [DOI] [PubMed] [Google Scholar]
- 11. Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all‐cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta‐analysis. Eur J Epidemiol. 2018;33:811‐829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Puig‐Ribera A, Martínez‐Lemos I, Giné‐Garriga M, et al. Self‐reported sitting time and physical activity: interactive associations with mental well‐being and productivity in office employees. BMC Public Health. 2015;15:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown HE, Gilson ND, Burton NW, Brown WJ. Does physical activity impact on presenteeism and other indicators of workplace well‐being? Sports Med. 2011;41:249‐262. [DOI] [PubMed] [Google Scholar]
- 14. McDowell CP, Herring MP, Lansing J, Brower C, Meyer JD. Working from home and job loss due to the COVID‐19 pandemic are associated with greater time in sedentary behaviors. Front Public Health. 2020;8:597619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Machida M, Nakamura I, Saito R, et al. Adoption of personal protective measures by ordinary citizens during the COVID‐19 outbreak in Japan. Int J Infect Dis. 2020;94:139‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Japanese Ministry of Health Labor, and Works . About coronavirus disease 2019 (COVID‐19). 2020. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000164708_00001.html. Accessed February 9, 2021. Japanese
- 17. Fukushima N, Amagasa S, Kikuchi H, et al. Validity and reliability of the Work‐related Physical Activity Questionnaire for assessing intensity‐specific physical activity and sedentary behavior in the workplace. Sangyo Eiseigaku Zasshi. 2020;62:61‐71. [DOI] [PubMed] [Google Scholar]
- 18. Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661‐666. [DOI] [PubMed] [Google Scholar]
- 19. Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio‐metabolic biomarkers in US adults: NHANES 2003–06. Euro Heart J. 2011;32:590‐597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thorp AA, Kingwell BA, Sethi P, Hammond L, Owen N, Dunstan DW. Alternating bouts of sitting and standing attenuate postprandial glucose responses. Med Sci Sports Exerc. 2014;46:2053‐2061. [DOI] [PubMed] [Google Scholar]
- 21. Clark BK, Thorp AA, Winkler EA, et al. Validity of self‐reported measures of workplace sitting time and breaks in sitting time. Med Sci Sports Exerc. 2011;43:1907‐1912. [DOI] [PubMed] [Google Scholar]
- 22. Pedisic Z, Bennie JA, Timperio AF, et al. Workplace Sitting Breaks Questionnaire (SITBRQ): an assessment of concurrent validity and test‐retest reliability. BMC Public Health. 2014;14:1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Japanese Ministry of Internal Affairs and Communications . 2014. https://www.soumu.go.jp/toukei_toukatsu/index/seido/sangyo/02toukatsu01_03000023.html. Accessed February 9, 2021. Japanese.
- 24. Fagerland MW. t‐tests, non‐parametric tests, and large studies–a paradox of statistical practice? BMC Med Res Methodol. 2012;12:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Persol Research and Consulting . Urgent survey on the impact of new coronavirus measures on telework. 2020. https://rc.persol‐group.co.jp/research/activity/files/telework.pdf. Accessed February 9, 2021. Japanese.
- 26. Zimring C, Joseph A, Nicoll GL, Tsepas S. Influences of building design and site design on physical activity: research and intervention opportunities. Am J Prev Med. 2005;28(2 Suppl 2):186‐193. [DOI] [PubMed] [Google Scholar]
- 27. Smith L, Hamer M, Ucci M, et al. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office‐based workers: the active buildings study. BMC Public Health. 2015;15:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mummery WK, Schofield GM, Steele R, Eakin EG, Brown WJ. Occupational sitting time and overweight and obesity in Australian workers. Am J Prev Med. 2005;29:91‐97. [DOI] [PubMed] [Google Scholar]
- 29. Jans MP, Proper KI, Hildebrandt VH. Sedentary behavior in Dutch workers: differences between occupations and business sectors. Am J Prev Med. 2007;33:450‐454. [DOI] [PubMed] [Google Scholar]
- 30. Vandelanotte C, Duncan MJ, Short C, et al. Associations between occupational indicators and total, work‐based and leisure‐time sitting: a cross‐sectional study. BMC Public Health. 2013;13:1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Macêdo TAM, Cabral ELDS, Silva Castro WR, et al. Ergonomics and telework: a systematic review. Work. 2020;66:777‐788. [DOI] [PubMed] [Google Scholar]
- 32. Fukushima N, Kitabayashi M, Kikuchi H, et al. Comparison of accelerometer‐measured sedentary behavior, and light‐ and moderate‐to‐vigorous‐intensity physical activity in white‐ and blue‐collar workers in a Japanese manufacturing plant. J Occup Health. 2018;60:246‐253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shrestha N, Kukkonen‐Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. 2018;12:CD010912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jindo T, Kai Y, Kitano N, et al. Impact of activity‐based working and height‐adjustable desks on physical activity, sedentary behavior, and space utilization among office workers: a natural experiment. Int J Environ Res Public Health. 2019;17:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults' sedentary behavior determinants and interventions. Am J Prev Med. 2011;41:189‐196. [DOI] [PubMed] [Google Scholar]
- 36. De Cocker K, Veldeman C, De Bacquer D, et al. Acceptability and feasibility of potential intervention strategies for influencing sedentary time at work: focus group interviews in executives and employees. Int J Behav Nutr Phys Act. 2015;12:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pedersen SJ, Cooley PD, Mainsbridge C. An e‐health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work. 2014;49:289‐295. [DOI] [PubMed] [Google Scholar]
- 38. Buckley JP, Hedge A, Yates T, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med. 2015;49:1357‐1362. [DOI] [PubMed] [Google Scholar]
- 39. Amagasa S, Machida M, Fukushima N, et al. Is objectively measured light‐intensity physical activity associated with health outcomes after adjustment for moderate‐to‐vigorous physical activity in adults? A systematic review. Int J Behav Nutr Phys Act. 2018;15:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schur LA, Ameri M, Kruse D. Telework after COVID: a “silver lining” for workers with disabilities? J Occup Rehabil. 2020;30:521‐536. [DOI] [PMC free article] [PubMed] [Google Scholar]


