Abstract
Background
A reduction of admission for MI has been reported in most countries affected by COVID-19. No clear explanation has been provided.
Methods
To report the incidence of myocardial infarction (MI) admission during COVID-19 pandemic and in particular during national lockdown in two unequally affected French provinces (10-million inhabitants) with a different media strategy, and to describe the magnitude of MI incidence changes relative to the incidence of COVID-19-related deaths. A longitudinal study to collect all MIs from January 1 until May 17, 2020 (study period) and from the identical time period in 2019 (control period) was conducted in all centers with PCI-facilities in northern “Hauts-de-France” province and western “Pays-de-la-Loire” Province. The incidence of COVID-19 fatalities was also collected.
Findings
In “Hauts-de-France”, during lockdown (March 18–May 10), 1500 COVID-19-related deaths were observed. A 23% decrease in MI-IR (IRR=0.77;95%CI:0.71–0.84, p<0.001) was observed for a loss of 272 MIs (95%CI:−363,−181), representing 18% of COVID-19-related deaths. In “Pays-de-la-Loire”, 382 COVID-19-related deaths were observed. A 19% decrease in MI-IR (IRR=0.81; 95%CI=0.73–0.90, p<0.001) was observed for a loss of 138 MIs (95%CI:−210,−66), representing 36% of COVID-19-related deaths. While in “Hauts-de-France” the MI decline started before lockdown and recovered 3 weeks before its end, in “Pays-de-la-Loire”, it started after lockdown and recovered only by its end. In-hospital mortality of MI patients was increased during lockdown in both provinces (5.0% vs 3.4%, p=0.02).
Interpretation
It highlights one of the potential collateral damages of COVID-19 outbreak on cardiovascular health with a dramatic reduction of MI incidence. It advocates for a careful and weighted communication strategy in pandemic crises.
Funding
The study was conducted without external funding.
Keywords: COVID-19 outbreak, Myocardial Infarction, Clinical outcome, Mortality
Abbreviations: COVID-19, Coronavirus disease 2019; MI, Myocardial Infarction; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non ST-segment elevation myocardial infarction
Research in context.
Evidence before this study
Studies have reported a reduction in admissions for acute myocardial infarction (MI) in various areas worldwide hit by the COVID-19 pandemic. Most studies, including one conducted in France and reporting a drop of MI as high as 30%, were collecting data from large cities. Population migration from large cities to countryside areas could have artificially exaggerated the magnitude of MI drop. In addition, the impact of media campaign in such context is unknown.
Added value of this study
It is the first to report the MI incidence in two provinces representing 1/7 of French population, unevenly affected by COVID-19 and with a different medical campaign policy. It is also the first to include all centers with PCI facilities of a territory and to match information on the absolute incidence of MI admission and of COVID-19 death.
A reduction of MI admission of ≈20% was observed throughout the national lockdown in the 2 provinces, which is much lower than the 30% drop recently reported from centers located in large cities disseminated on the French territory. Reduction of MI admission was not related to the intensity of the COIVD-19 outbreak, As such, in the province the least affected by the pandemic, the number of missing MIs was disproportionately higher compared to COVID-19-related fatalities (36% vs 18%). A faster normalization of MI incidence was observed in the province (Hauts-de-France) in which a large local media campaign was conducted.
Implications of all the available evidence
When conducting observational studies on the impact of COVID-19 outbreak on the incidence of MI admission, it advocates for the inclusion of all “contiguous” centers of the territory in order to have a more accurate estimation of the true rate of (missing) MIs. It also advocates for a careful and weighted communication strategy during pandemic crises to prevent exacerbation of an unreasonable fear of seeking medical care and keep providing optimal medical care for all high acuity patients.
Alt-text: Unlabelled box
1. Introduction
The coronavirus disease 2019 (COVID-19) outbreak has strained the healthcare system in France like in the rest of the world.
The first fatality for COVID in France was reported in Hauts-de-France province on February 25, 2020. To decrease the peak of the epidemic and avoid swamping the healthcare system, French government announced a countrywide lockdown from March 17 to May 10 without distinction between provinces with high or low incidence in COVID-19.
Several studies have reported that hospitals performing primary percutaneous coronary intervention (PCI) for acute myocardial infarction (MI) worldwide in various areas severely hit by the pandemic experienced a reduction in admissions for MI [1], [2], [3], [4], [5], [6], [7], [8] without clear explanation of this phenomenon. Among them, a study conducted in 22 centers in France, all located in major cities, reported a drop of MI as high as 30% [9].
Similar to the French registry, most studies conducted in Europe did not included all “contiguous” centers covering the territory to be studied but rather a sample of centers, mainly from large cities [[1], [2], [3], [4], [5], [6], [7], [8], [9]]. The usually small number of centers included (e.g. only 10% of all French centers with PCI facilities were involved in the French registry [9]), and the almost exclusive location in the largest cities could be a concern. In most countries, once the decision to lock the population was announced, a migration of populations from the large cities to the countryside areas was observed [10]. By decreasing the number of patients exposed to the risk of MI in those large cities, it could have artificially exaggerated the true magnitude of the drop of MIs supposedly occurring in the populations the “study samples” are representing [9].
The only way to prevent this issue, is to include all “contiguous centers” covering the territory of interest. In that case when a patient moves from one location to another and suffers an MI managed by a center which is not its original center, the event is still captured. While such methodology may be difficult to implement at a countrywide level, it can be done at the level of a province.
In addition, the impact of media campaign to remind the population about MI symptoms and the importance of early management of MIs in such context is unknown.
The objectives of this study were: i) to report the incidence of MI during COVID-19 pandemic and in particular during national lockdown in two French provinces by involving all “contiguous centers” delivering primary-PCI service, ii) to report the incidence of MI in two provinces unevenly affected by COVID-19 and with a different media campaign policy, iii) to describe the magnitude of MI incidence changes relative to the incidence of COVID-19-related deaths.
2. Methods
A nationwide lockdown was decided by the French government to start on March 17 12 am and end on May 10 12 am. As a drop in MI hospital admission was reported in some areas of the national territory, the French Cardiology Society issued a press release to recall the symptoms of MI [11] and the government broadcasted on April 7 a message that healthcare services remained operational and safe for use [12]. In “Hauts-de-France”, it was further carried through a province-wide media campaign was conducted for 2 weeks (April 6–April 18: TV, radio, newspapers, social media) [13,14]. In “Pays-de-la-Loire”, no dedicated local media campaign was conducted.
We carried out a longitudinal study in all PCI-capable hospitals (n=19) in northern “Hauts-de-France” province and in all PCI-capable hospitals (n=8) of western “Pays-de-la-Loire” Province from January 1, 2020 until May 17, 2020 (study period, (5,962,662 inhabitants in “Hauts-de-France” and 3,801,797 in “Pays-de-la-Loire”, as estimated by the French National Institute for Economical and Statistical Studies (INSEE)) and from the identical time period in 2019 (control period, 5,977,437 inhabitants in “Hauts-de-France” and 3,787,400 in “Pays-de-la-Loire”, INSEE).
The number of patients admitted with MIs and subtype (ST-segment elevation myocardial infarction [STEMI] and Non-STEMI [NSTEMI]) and in-hospital mortality were obtained by extraction of anonymous data from the hospitals’ databases. Patients in whom a coronary angiography was not performed and patients in whom the diagnosis of acute myocardial infarction (STEMI or NSTEMI) was invalidated by coronary angiography (+/− ventricular angiography) in favor of non-ischemic myocardial injury (e.g., myocarditis or stress cardiomyopathy) were not included in the analysis. Patients with a diagnosis of acute myocardial infarction (STEMI/NSTEMI) occurring in-hospital (e.g. post-angiography, post-PCI or post-surgery, …) were also not included in the analysis.
The distinction between STEMI and NSTEMI was performed by local physicians based on clinical presentation. Briefly, STEMI were identified as new ischemic symptoms lasting for >= 20 min and persistent ST-elevation of >= 1 mm in greater than 2 contiguous leads (or new left bundle-branch block) followed by dynamic changes in cardiac biomarkers (high-sensitive I or T troponin above the upper limit of normal at each study site). NSTEMI were identified as new ischemic symptoms and dynamic changes in cardiac biomarkers with or without associated electrocardiographic changes (ST-depression, transient ST-elevation and T-wave inversion).
Overall, the number of MIs are reported by specific time interval of exposure and the number of all the patients with final diagnosis of MI after coronary angiogram and do not take into account patients medically managed or without final diagnosis of MI.
The primary endpoint was the MI incidence rate (IR; expressed as cases per day reported to 100,000 persons). Results are reported in weekly periods. The demographic data and the incidence of COVID-19-related deaths for each province were obtained from “Santé Publique France” (https://geodes.santepubliquefrance.fr).
The ethical committee exempted the study from individual patient approval as no individual patient data was analyzed nor collected.
2.1. Statistical analysis
IRs of MIs (overall, STEMI and NSTEMI) were calculated, for a giving interval time of exposure within a period (2020 vs. 2019), by dividing the number of cumulative events by the number of person-time at risk (population size*interval time of exposure expressed in days). Within each province separately, we firstly compared the IRs (calculated for overall interval time of exposure) between 2020 (defined as study period) and 2019 (defined as control period) by using a Poisson regression model with number of cumulative events (all MIs, STEMI or NSTEMI) as dependent variable, period (study vs. control) as independent variable, and the log of person-time at risk as offset variable. Incidence-rate ratios (IRRs) for 2020 versus 2019 (and theirs 95% confidence intervals (CIs)) were derived from the Poisson regression model as effect size. We secondly examined if the difference in IRs between 2020 and 2019 differed according to interval time of exposure by including an interaction term between period (2020 vs. 2019) and interval time of exposure in multivariable Poisson regression model; effect sizes within each interval time of exposure were estimated from model by using linear contrasts. Statistical analyses were conducted with a two-tailed α level of 0.05. Data were analyzed using SAS software version 9.4 (SAS Institute, Cary, NC).
2.2. Role of the funding source
The study was conducted by the investigators without external funding. All authors had full access to all the data in the study and accept responsibility to submit for publication.
3. Results
3.1. Study population
8931 patients were admitted for acute MI confirmed by angiography (Table 2), including 3357 with STEMI (2120 in “Hauts-de-France” and 1237 in “Pays-de-la-Loire”, Suppl Table 2) and 5574 with NSTEMI (3367 in “Hauts-de-France” and 2207 in “Pays-de-la-Loire”, Suppl Table 4).
Table 2.
Comparison of number of Myocardial infarction between study period and control period in « Hauts-de-France » and in « Pays de la Loire » Provinces.
| « Hauts-de-France » province |
« Pays de la Loire » Province |
|||||||
|---|---|---|---|---|---|---|---|---|
| Time interval of exposure | Control period (2019) | Study period (2020) | Control period (2019) | Study period (2020) | ||||
| MI (n) | MI (n) | Difference | 95%CI | MI (n) | MI (n) | Difference | 95%CI | |
| Jan 1–Feb 17 | 898 | 967 | 69 | [−16; 154] | 581 | 608 | 27 | [−41; 95] |
| Feb 18–Feb 24 | 139 | 147 | 8 | [−26; 42] | 98 | 94 | −4 | [−32; 24] |
| Feb 25–Mar 3 | 160 | 179 | 19 | [−18; 56] | 105 | 101 | −4 | [−33; 25] |
| Mar 4–Mar 10 | 158 | 146 | −12 | [−47; 23] | 80 | 88 | 8 | [−18; 34] |
| Mar 11–Mar 17 | 148 | 111 | −37 | [−69; −5] | 91 | 84 | −7 | [−33; 19] |
| Mar 18–Mar 22 | 123 | 54 | −69 | [−96; −42] | 86 | 72 | −14 | [−39; 11] |
| Mar 23–Mar 29 | 186 | 85 | −101 | [−134; −68] | 96 | 72 | −24 | [−50; 2] |
| Mar 30–Apr 5 | 138 | 101 | −37 | [−68; −6] | 91 | 68 | −23 | [−48; 2] |
| Apr 6–Apr 12 | 153 | 128 | −25 | [−58; 8] | 98 | 75 | −23 | [−49; 3] |
| Apr 13–Apr 19 | 163 | 132 | −31 | [−65; 3] | 94 | 59 | −35 | [−60; −10] |
| Apr 20–Apr 26 | 162 | 154 | −8 | [−43; 27] | 85 | 95 | 10 | [−17; 37] |
| Apr 27–May 3 | 134 | 140 | 6 | [−27; 39] | 97 | 73 | −24 | [−50; 2] |
| May 4–May 10 | 137 | 130 | −7 | [−40; 26] | 92 | 87 | −5 | [−32; 22] |
| May 11–May 17 | 160 | 154 | −6 | [−41; 29] | 87 | 87 | 0 | [−26; 26] |
| Jan 1–May 17 (overall) | 2859 | 2628 | −231 | [−377; −85] | 1781 | 1663 | −118 | [−234; −2] |
| Mar 11–May 17 | 1504 | 1189 | −315 | [−417; −213] | 917 | 772 | −145 | [−226; −64] |
| Mar 18–May 10 (lockdown) | 1196 | 924 | −272 | [−363; −181] | 739 | 601 | −138 | [−210; −66] |
Apr: April, CI: confidence interval, Feb: February, IRR: incidence rate ratio, Jan: January, Mar: March, MI: myocardial infarction.
After exclusion of patients in whom angiography did not confirm the diagnosis of MI, the patients with angiography represented (96.5%) of patients admitted with the diagnosis of MI. This proportion was stable over time in the 2 provinces. In particular, it did not decreased during national lockdown (March 18–May 10 2020), as compared to the same period of the previous year both in "Hauts-de-France" (STEMI 98.1% vs 97.9%, p=0.87 and NSTEMI 95.3% vs 95.2%, p=0.91) and in “Pays-de-la-Loire” (STEMI 98.5% vs 98.5%, p=0.99 and NSTEMI 96.9% vs 96.6%, p=0.79).
3.2. In Hauts-de-France province
The first case of COVID-related death was identified on February 25, 2020 and was followed by a total of 1625 COVID-19 related-death by May 17 corresponding to the 3rd most hit province of the country (Supplemental Fig. 1).
During the national lockdown (March 18–May 10), a 23% decrease in MI IR (IRR=0.77;95%CI:0.71–0.84, p<0.001, Table 1) was observed for an overall loss of 272 MIs (95%CI:−363, −181, Table 2) including 111 STEMIs (95%CI:−168, −54, Suppl. Tables 1 and 2) and 161 NSTEMIs (95%CI:−232, −90, Suppl. Tables 3 and 4). During the same time period, “Hauts-de-France” experienced 1500 COVID-19-related deaths.
Table 1.
Comparison of Incidences of Myocardial Infarction between study period and control period in « Hauts-de-France » and in « Pays de la Loire » Provinces.
| « Hauts-de-France » province |
« Pays de la Loire » Province |
|||||||
|---|---|---|---|---|---|---|---|---|
| Time-interval of exposure | Control period (2019) | Study period (2020) | Control period (2019) | Study period (2020) | ||||
| MI incidencea | MI incidencea | IRR (95% CI) | P-value | MI incidencea | MI incidencea | IRR (95% CI) | P-value | |
| Jan 1–Feb 17 | 0.31 | 0.34 | 1.08 (0.99–1.18) | 0.099 | 0.32 | 0.33 | 1.04 (0.93–1.17) | 0.47 |
| Feb 18–Feb 24 | 0.33 | 0.35 | 1.06 (0.84–1.34) | 0.62 | 0.37 | 0.35 | 0.96 (0.72–1.27) | 0.75 |
| Feb 25–Mar 3 | 0.33 | 0.38 | 1.12 (0.91–1.39) | 0.29 | 0.35 | 0.33 | 0.96 (0.73–1.26) | 0.76 |
| Mar 4–Mar 10 | 0.38 | 0.35 | 0.93 (0.74–1.16) | 0.51 | 0.30 | 0.33 | 1.10 (0.81–1.48) | 0.55 |
| Mar 11–Mar 17 | 0.35 | 0.27 | 0.75 (0.59–0.96) | 0.023 | 0.34 | 0.32 | 0.92 (0.68–1.24) | 0.58 |
| Mar 18–Mar 22 | 0.41 | 0.18 | 0.44 (0.32–0.61) | <0.001 | 0.45 | 0.38 | 0.83 (0.61–1.14) | 0.26 |
| Mar 23–Mar 29 | 0.44 | 0.20 | 0.46 (0.35–0.59) | <0.001 | 0.36 | 0.27 | 0.75 (0.55–1.01) | 0.061 |
| Mar 30–Apr 5 | 0.38 | 0.28 | 0.73 (0.57–0.95) | 0.018 | 0.40 | 0.30 | 0.74 (0.54–1.02) | 0.066 |
| Apr 6–Apr 12 | 0.43 | 0.36 | 0.84 (0.66–1.06) | 0.14 | 0.43 | 0.33 | 0.76 (0.56–1.03) | 0.077 |
| Apr 13–Apr 19 | 0.45 | 0.37 | 0.81 (0.65–1.02) | 0.075 | 0.41 | 0.26 | 0.63 (0.45–0.87) | 0.005 |
| Apr 20–Apr 26 | 0.45 | 0.43 | 0.95 (0.76–1.19) | 0.67 | 0.37 | 0.42 | 1.11 (0.83–1.49) | 0.47 |
| Apr 27–May 3 | 0.37 | 0.39 | 1.05 (0.83–1.33) | 0.70 | 0.43 | 0.32 | 0.75 (0.55–1.02) | 0.063 |
| May 4–May 10 | 0.38 | 0.36 | 0.95 (0.75–1.21) | 0.68 | 0.40 | 0.38 | 0.94 (0.70–1.26) | 0.69 |
| May 11–May 17 | 0.45 | 0.43 | 0.96 (0.77–1.20) | 0.75 | 0.38 | 0.38 | 1.00 (0.74–1.34) | 0.98 |
| Jan 1–May 17 (overall) | 0.37 | 0.34 | 0.92 (0.87–0.97) | 0.002¤ | 0.36 | 0.33 | 0.93 (0.87–0.99) | 0.034# |
| Mar 11–May 17 | 0.41 | 0.33 | 0.79 (0.73–0.86) | <0.001 | 0.40 | 0.33 | 0.84 (0.76–0.92) | <0.001 |
| Mar 18–May 10 (lockdown) | 0.42 | 0.32 | 0.77 (0.71–0.84) | <0.001 | 0.41 | 0.33 | 0.81 (0.73–0.90) | <0.001 |
Incidence per 100,000 persons/day.
Apr: April, CI: confidence interval, Feb: February, IRR: incidence rate ratio, Jan: January, Mar: March, MI: myocardial infarction
Heterogeneity across time intervals: ¤P <0.001/ #P=0.085.
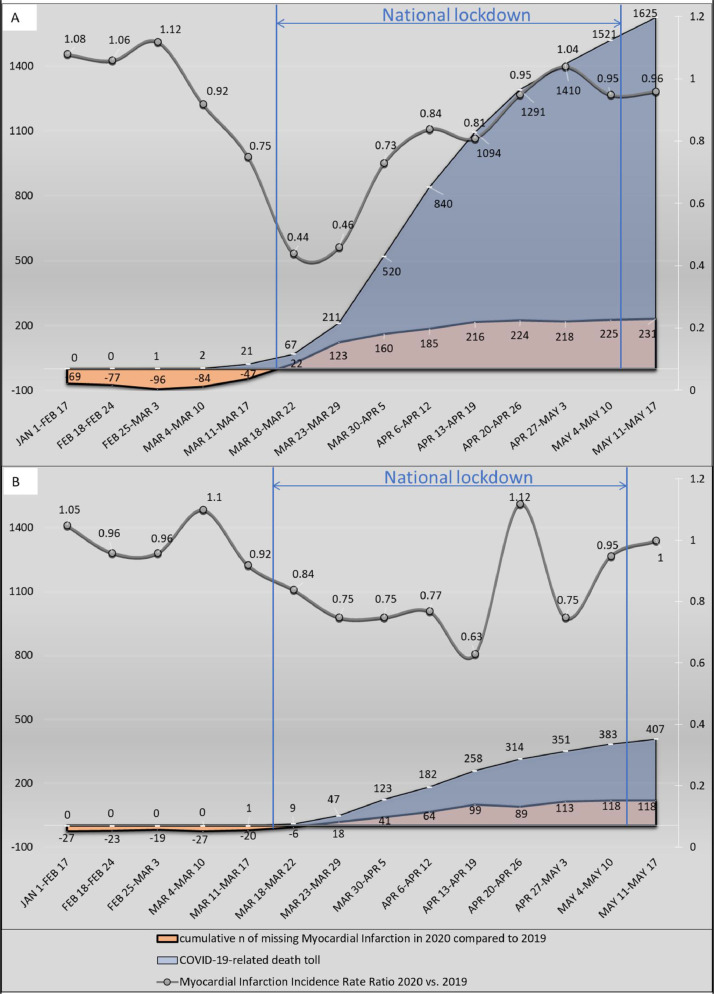
More specifically, from January1-to-May-17, a total of 2628 patients were referred for MI versus 2859 patients in 2019 (control period), corresponding to a 8% decline of IR (IRR=0.92; 95%CI:0.87–0.97, p=0.002, Table 1). Until March 11 the rate of MI was similar to 2019. The week before lockdown (March 11–17), it dropped by 25% (IRR=0.75; 95%CI:0.59–0.96, p=0.023). The decline was further amplified the first week of lockdown (March 18–March 22) with a decline of 56% compared to 2019 and returned to normal within 6 weeks (by April 19) and 3 weeks before the end of lockdown (Table 1 and Fig. 1). The incidence of both subtypes of MIs (STEMI and NSTEMI) followed roughly the same pattern and declined transitory during COVID outbreak (Supplemental Tables 1–4).
Fig. 1.
Myocardial infarction incidence rate ratio, COVID-19-related death toll and cumulative number of Myocardial Infarction missing compared to same period in 2019.
A): Haut-de-France province B): Pays-de-Loire province.
COVID-19: coronavirus disease 2019; n=number.
3.3. In “Pays-de-la-Loire” province
The first case of COVID-related death was identified on March 17, 2020 and was followed by a mild intensity epidemic for a total of 407 COVID-19 related-death by May 17 (Supplemental figure).
During the national lockdown (March 18–May 10), a 19% decrease in MI IR (IRR=0.81; 95%CI=0.73–0.90, p<0.001, Table 1) was observed for an overall loss of 138 MIs (95%CI:−210, −66, Table 2) including 63 STEMIs (95%CI:−105, −21, Suppl. Tables 1 and 2) and 75 NSTEMIs (95%CI:−134, −16, Suppl. Tables 3 and 4). During the same time period, “Pays-de-la-Loire” experienced 382 COVID-19-related deaths.
More specifically, from January1-to-May-17, a total of 1663 patients were referred for MIs compared to 1781 in 2019 corresponding to a 7% decline of IR (IRR=0.93; 95%CI:0.87–0.99, p=0.034, Table 1). It declined slowly after the beginning of the lockdown (March 10), to peak at the 4th week (IRR=0.63; CI:0.45–0.87, p=0.005) and recovered gradually by the end of the lockdown (Table 1 and Fig. 1).
3.4. In-hospital mortality
Overall, combining data of the 2 provinces, in-hospital mortality of patients admitted with acute MI increased during the national lockdown (March 18–May 10), as compared to the same period of the previous year (77/1525, 5.0% vs 67/1935, 3.4%, p=0.02, Suppl Table 5). A similar trend was observed in patients admitted with STEMI (50/548, 9.1% vs 45/722, 6.2%, p=0.05, Suppl Table 5) or NSTEMI (27/977, 2.8%, vs 22/1213, 1.8%, p=0.13, Suppl Table 5), and in each of the 2 provinces individually (Suppl. Table 5).
4. Discussion
The present study is the first to report the MI admission incidence in two provinces unevenly affected by COVID-19 and representing 1/7 of French population. It is also the first to include all centers with PCI facilities of a territory and to match information on the absolute incidence of MI and of COVID-19 death.
The main results are the following: i) a significant decline of admission for MIs (including STEMI and NSTEMI) was observed during COVID-19 outbreak and particularly during national lockdown; ii) This reduction was similar in magnitude (−23% and −19%) but with a different temporal pattern in the 2 provinces, iii) In the province the least affected, the number of missing MIs was disproportionately higher compared to COVID-19-related fatalities (138/382=36% in “Pays-de-la-Loire” vs 272/1500=18% in “Hauts-de-France” ); iv) This reduction was not sustained over the full duration of the national lockdown; v) Percent in-hospital mortality of admitted MIs was increased during the national lockdown period.
A reduction of MI admission of approximately 20% was observed in both provinces throughout the national lockdown. It affected both MI subtypes (STEMI and NSTEMI) with a similar magnitude. In “Hauts-de-France” , the reduction started suddenly 1 week before the official lockdown and was reversed after 6 weeks, still within the lockdown period. In “Pays-de-la-Loire”, the decrease started with the lockdown. It was also more progressive and more prolonged with a nadir at the 6th week of the lockdown.
The present report provides the best effort to date to collect all MIs occurring during lockdown in a large territory hit by COVID-19. The drop of MIs (−20%) observed in “Hauts-de-France” and “Pays-de-la-Loire”, and obtained by collecting information of all centers with PCI facilities in the two regions, is much lower than the 30% drop recently reported in a sample of 22 centers disseminated on the French territory, but all located in very large cities [9]. Interestingly, the drop of MIs observed in the largest city of each Province that we studied (Lille, in “Hauts-de-France” and Nantes, in “Pays-de-la-Loire”) was also ≈−30%. Altogether, this may suggest that studies involving only centers located in large cities may overestimate the true drop of MIs by counting as missing MIs those occurring in subjects who have moved to the countryside at the time of the lockdown [10] and have been managed by a center located in a different city.
Several studies have already reported a decrease of admission for MI during COVID outbreak. Four mains hypotheses have been generated so far to explain this phenomenon [1,3]: i) environmental improvement: reduction of air pollution, home rest, reduction of daily stressful commute, better medication adherence; ii) disorganization of the overloaded emergent healthcare system: inability to make an effective triage of the patients with MI amid the surge of COVID-19 patients; iii) Changes in MI management: more frequent medical management or fibrinolytic therapy administration; iv) combination of rigorous health public policy promoting social isolation, stay-at-home order, and the fear to contract virus in hospitals would have made patients reluctant to seek for medical care.
The hypothesis of an environmental improvement is not supported by our study since the recovery of the MI rate occurred way before the end of the lockdown in the “Hauts-de-France” province. Healthcare system disorganization or management changes are also unlikely as the drop in MIs was very similar (−23% and −19%) in 2 provinces with a very different prevalence of the COVID-19 outbreak.
The main cause of MI reduction was probably the patients’ fear of seeking care. This behavior seems driven by the progression of the pandemic and worsened by the national health policy decisions of rigorous lockdown in which social distancing was mandatory, all non-essential trips from home were banned and people were unable to leave their homes without a signed and dated permission form. The importance of such behavior changes is also supported by the observation that a faster normalization of MI incidence was observed in the province (Hauts-de-France) in which, in addition to national communications, a large local media campaign was conducted by healthcare workers. A potential positive impact of wide media campaign has also been suggested in the United States to explain regional differences in the "recovery" of STEMI admissions [7].
The higher percent in-hospitality mortality of MIs admitted during national lockdown is an interesting observation. As the proportion of patients referred to coronary angiography was not decreased during that period, it could reflect an overall a higher proportion of patients being at “high risk” among those admitted and/or further time delay in management leading to reperfusion [15].
Finally, our observation of a disproportion between the number of “missing” MIs and the magnitude of the COVID-19 outbreak raises concerns about the impact of indirect fatalities due to untreated MIs versus direct COVID-19-related fatalities. Since the mortality of untreated MI approximates 30–40% [16] and as 70% of the French territory was, similar to “Pays-de-la-Loire” province, relatively spared by COVID-19 (Supplemental figure), the observation that the number of missing MIs represented nearly 40% of the COVID-related deaths in that province may raise fears of a very heavy nationwide MI-related death toll. Further studies will be needed to detect a potential resurgence of mechanical complications or heart failure [17,18] and increase of cardio-vascular mortality as a consequence of COVID-19 outbreak-related lockdown.
4.1. Limitations
Our observational longitudinal study has several limitations and remains hypothesis-generating. No definite causal inference can be established through the temporality correlation between COVID-19 outbreak and MI reduction. We cannot rule out some degree of disorganization of healthcare system to partially explain the phenomenon, in particular, by saturation of the single emergency phone number “15”. However, none of these 2 provinces has been flooded by COVID-19 outbreak and the acute-care bed capacity was preserved (“Hauts-de-France” has been able to receive patients transferred from Paris or Eastern provinces). We were also unable to report the rate of fibrinolytic administration and therefore we cannot rule out the possibility of practice changes during this period. However, all the centers maintained 24/7 PCI-capabilities without modification of the MI management strategy as recommended by the French interventional cardiology scientific society still prioritizing primary percutaneous coronary interventions [12].
5. Conclusion
This study highlights one of the potential collateral damages of COVID-19 outbreak on cardiovascular health with a dramatic reduction of MI incidence, probably mainly driven by a self-limitation of access to care from patients that has been worsened by a countrywide lockdown. When conducting observational studies on the impact of COVID-19 outbreak on the incidence of MI admission, this report advocates for inclusion of all “contiguous” centers of the studied territory to be studied in order to have a more accurate estimation of the true rate of (missing) MIs. It also advocates for a careful and weighted communication strategy in pandemic crises to prevent exacerbation of an unreasonable fear of seeking medical care and keep providing optimal medical care for all high acuity patients.
Author Contributions
EVB, TM, AF; ND, ALB, JJB; ON, FH, MB; FV, MD; SS; AF; ED; UM; JC, AM; TL; AC, JJ; PH; MB; MDM, AT, DM; FA; AP; FP; CD; GL; GS; AC; HS; BV; SP; TP, DJ, TD, DA, VG and FV collected the data and made critical revision of the document.
EVB and FV designed the study, made literature search, drafted the manuscript and the figures.
EVB, FV, AP, and JL verified the underlying data and performed the analysis.
EVB, FV, AP, JL, GB and GC interpreted the data and made critical revision of the manuscript.
Declaration of Interests
Dr. Lemesle reports personal fees from Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, BMS, Daiichi Sankyo, Lilly, MSD, Mylan, Novartis, Novonordisk, Pfizer, Sanofi Aventis, Servier, outside the submitted work. Dr Delhaye reports personal fees from Medtronic outside the submitted work. Dr. Cayla reports personal fees from Amgen, personal fees from Astra Zeneca, personal fees from Bayer, personal fees from Biotronik, personal fees from Bristol Myers Squibb, grants and personal fees from Medtronic, personal fees from MSD, personal fees from Pfizer, personal fees from Sanofi, outside the submitted work. The other authors do not report any conflict of interest.
Data sharing statement
Request of the data set from qualified researchers trained in human subject confidentiality protocols with a specific research objective may be sent by email to the corresponding authors. Following mutual approval and singed data access agreement, deidentified data set will be made available following publication.
Acknowledgments
The study was conducted by the investigators without external funding. All authors had full access to all the data in the study and accept responsibility to submit for publication.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100030.
Contributor Information
Eric Van Belle, Email: ericvanbelle@aol.com.
Flavien Vincent, Email: flavienvincent@yahoo.fr.
Appendix. Supplementary materials
References
- 1.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. Epub 2020 Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rangé G, Hakim R, Motreff P. Where have the ST-segment elevation myocardial infarctions gone during COVID-19 lockdown? Eur Heart J – Qual Care Clin Outcomes. 2020;6(3):223–224. doi: 10.1093/ehjqcco/qcaa034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. Epub 2020 Apr 28. NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. Epub 2020 May 19. NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 5.Enache B, Claessens Y-E, Boulay F, Dor V, Eker A, Civaia F. Reduction in cardiovascular emergency admissions in Monaco during the COVID-19 pandemic. Clin Res Cardiol. 2020;109(12):1577–1578. doi: 10.1007/s00392-020-01687. http://link.springer.com/10.1007/s00392-020-01687-w Epub 2020 Jun 12. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184486/ ;Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia S, Stanberry L, Schmidt C, Sharkey S, Megaly M, Albaghdadi MS, Meraj PM, Garberich R, Jaffer FA, Stefanescu Schmidt AC, Dixon SR, Rade JJ, Smith T, Tannenbaum M, Chambers J, Aguirre F, Huang PP, Kumbhani DJ, Koshy T, Feldman DN, Giri J, Kaul P, Thompson C, Khalili H, Maini B, Nayak KR, Cohen MG, Bangalore S, Shah B, Henry TD. Impact of COVID-19 pandemic on STEMI care: an expanded analysis from the United States. Catheter Cardiovasc Interv. 2020 doi: 10.1002/ccd.29154. 10.1002/ccd.29154Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. The Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. Epub 2020 Jul 14, S0140673620313568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, Thuaire C, Angoulvant D, Cayla G, Bouleti C, Gallet de Saint Aurin R, Goube P, Lhermusier T, Dillinger JG, Paganelli F, Saib A, Prunier F, Vanzetto G, Dubreuil O, Puymirat E, Boccara F, Eltchaninoff H, Cachanado M, Rousseau A, Drouet E, Steg PG, Simon T, Danchin N. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Publ Health. 2020;5(10):e536–e542. doi: 10.1016/S2468-2667(20)30188-2. Epub 2020 Sep 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.SONDAGE - Les Français et le confinement: quatre millions de personnes ont quitté leur résidence principale. 2020. https://www.francebleu.fr/infos/societe/sondage-les-francais-et-le-confinement-quatre-millions-de-personnes-ont-quitte-leur-residence-1586183971.
- 11.Société française de Cardiologie, Société française neuro-vasculaire. Communiqué de presse: Le traitement des urgences cardiovaculaires et neurovasculaires reste une périorité en période épidémique [Internet]. 2020;Available from: https://sfcardio.fr/actualite/le-traitement-des-urgences-cardiovasculaires-reste-une-priorite-en-periode-epidemique<https://nam03.safelinks.protection.outlook.com/?url=https%3A%2F%2Fsfcardio.fr%2Factualite%2Fle-traitement-des-urgences-cardiovasculaires-reste-une-priorite-en-periode-epidemique&data=04%7C01%7CR.Verma1%40elsevier.com%7C012234514f9c4fa8488a08d8bb9ad4e8%7C9274ee3f94254109a27f9fb15c10675d%7C0%7C0%7C637465621423619756%7CUnknown%7CTWFpbGZsb3d8eyJWIjoiMC4wLjAwMDAiLCJQIjoiV2luMzIiLCJBTiI6Ik1haWwiLCJXVCI6Mn0%3D%7C2000&sdata=bjO3Kuj2x1mdORVP4k7039Gvckg17tCQFOpW%2FMR8IqU%3D&reserved=0>
- 12.Salomon Jérome. Point de situation du avril 2020, Directeur général de la santé, ministère de la solidarité et de la santé [Internet]. 2020;Available from: https://solidarites-sante.gouv.fr/IMG/pdf/point_de_situation_du_7_avril_2020-2.pdf
- 13.Patrick Seghi. Urgences cardiaques du CHU de Lille en décrue: «Aussi anormal qu'inquiétant» [Internet]. La Voix du Nord. 2020;Available from:https://www.lavoixdunord.fr/736259/article/2020-04-04/le-covid-19-attaque-aussi-les-urgences-cardiaques-du-chu-de-lille-en-pleine
- 14.Fabrice Julien. Baisse du nombre d'infarctus pris en charge: les cardiologues tirent la sonnette d'alarme. Les cardiologues de la région s'inquiètent de la baisse du nombre de patients pris en charge pour des infarctus. De nombreux malades renoncent en effet à se rendre à l'hôpital par peur du coronavirus.https://premium.courrier-picard.fr/id81696/article/2020-04-18/baisse-du-nombre-dinfarctus-pris-en-charge-les-cardiologues-tirent-la-sonnette
- 15.De Luca G, Verdoia M, Cercek M, Jensen LO, Vavlukis M, Calmac L, Johnson T, Ferrer GR, Ganyukov V, Wojakowski W, Kinnaird T, van Birgelen C, Cottin Y, IJsselmuiden A, Tuccillo B, Versaci F, Royaards KJ, Berg JT, Laine M, Dirksen M, Siviglia M, Casella G, Kala P, Díez Gil JL, Banning A, Becerra V, De Simone C, Santucci A, Carrillo X, Scoccia A, Amoroso G, Lux A, Kovarnik T, Davlouros P, Mehilli J, Gabrielli G, Rios XF, Bakraceski N, Levesque S, Cirrincione G, Guiducci V, Kidawa M, Spedicato L, Marinucci L, Ludman P, Zilio F, Galasso G, Fabris E, Menichelli M, Garcia-Touchard A, Manzo S, Caiazzo G, Moreu J, Forés JS, Donazzan L, Vignali L, Teles R, Benit E, Agostoni P, Bosa Ojeda F, Lehtola H, Camacho-Freiere S, Kraaijeveld A, Antti Y, Boccalatte M, Deharo P, Martínez-Luengas IL, Scheller B, Alexopoulos D, Moreno R, Kedhi E, Uccello G, Faurie B, Gutierrez Barrios A, Di Uccio FS, Wilbert B, Smits P, Cortese G, Parodi G, Dudek D. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76(20):2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biorck G, Blomqvist G, Sievers J. Studies on myocardial infarction in Malmö 1935 to 1954. I. Morbidity and mortality in a hospital material. Acta Med Scand. 1957;159:253–274. doi: 10.1111/j.0954-6820.1957.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 17.Riley RF, Kereiakes DJ, Mahmud E, Smith TD, Grines C, Henry TD. Back to the future" for STEMI?: The COVID-19 experience. JACC Case Rep. 2020;2(10):1651–1653. doi: 10.1016/j.jaccas.2020.07.011. Epub 2020 Aug 19. PMID: 32839761; PMCID: PMC7438036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson SJ, Connolly MJ, Elghamry Z, Cosgrove C, Firoozi S, Lim P. Effect of the COVID-19 pandemic on ST-segment–elevation myocardial infarction presentations and in-hospital outcomes. Circ: Cardiovasc Interv. 2020;13(7):e009438. doi: 10.1161/CIRCINTERVENTIONS.120.009438. https://www.ahajournals.org/doi/ [Internet][cited 2020 Jul 14];13. Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.