Abstract
A woman in her 70s presented to the emergency department with fever, fluctuating cognition and headache. A detailed examination revealed neurological weakness to the lower limbs with atonia and areflexia, leading to a diagnosis of bacterial meningitis, alongside a concurrent COVID-19 infection. The patient required critical care escalation for respiratory support. After stepdown to a rehabilitation ward, she had difficulties communicating due to new aphonia, hearing loss and left third nerve palsy. The team used written communication with the patient, and with this the patient was able to signal neurological deterioration. Another neurological examination noted a different pattern of weakness to the lower limbs, along with new urinary retention, and spinal arachnoiditis was identified. After more than 10 weeks in the hospital, the patient was discharged. Throughout this case, there were multiple handovers between teams and specialties, all of which were underpinned by good communication and examination to achieve the best care.
Keywords: infectious diseases, meningitis, TB and other respiratory infections, medical management
Background
This is a rare case which demonstrates the importance of good clinical examinations and investigations. The patient initially presented with fluctuating consciousness levels, headache and fever. Her COVID-19 swab was positive and therefore it would have been easy to dismiss her illness as delirium secondary to COVID-19. However, with thorough examinations during the initial clerking, focal neurological deficits were highlighted, leading to the eventual diagnosis of Escherichia coli bacterial meningitis, which by itself is also rare in adults.
The patient was transferred across multiple hospitals, and it was good documentation of previous examinations and ongoing clinical assessments that helped to identify changes to her condition. This demonstrates that repeated good examination techniques are a vital tool in the face of a complex patient or in the midst of a pandemic.
Case presentation
A woman in her 70s presented to the emergency department with fluctuating cognition, headache and chills. Initially, she had a low consciousness level as demonstrated on the Glasgow Coma Scale and was unable to provide any history, and therefore her family provided some collateral history. She woke up feeling unwell, with headache and chills, which progressed to generalised muscle pain and tiredness. Her family were concerned that she may become more confused throughout the day. Their main concern was that she may have contracted COVID-19 as they had been in contact with someone who was self-isolating. She was noted to have complete third and eighth nerve involvement, with ptosis of her left eye and new significant hearing loss.
The patient’s medical history included hypertension. She was previously independent and was living alone in her own home with no carers. This level of illness was a marked departure from her baseline. She was an ex-smoker, which alongside her history of hypertension suggested an increased risk of stroke.
Due to the non-specific nature of her symptoms, the initial examination was a thorough examination of all important body systems. Clinical examination highlighted that the patient had reduced power, reduced tone and absent reflexes in her lower limbs. Initially this led the team to believe she may have an acute central nervous system infection. Investigations revealed that she was COVID-19-positive and a Cerebrospinal Fluid PCR revealed E. coli meningitis. This was treated with intravenous antibiotics.
Soon after her admission the patient deteriorated significantly and required assistance with her breathing. She became acutely short of breath and showed a decline in her oxygen saturations, requiring oxygen supplementation. An arterial blood gas showed hypoxia and there was reduced air entry in the bases.
As this was an acute case and the patient had previously been independent, a decision was made to intubate her and admit her to the intensive care unit. While admitted to intensive care she was catheterised and ventilated for 5 days. She remained in the unit for 9 days before being stepped down to a medical ward.
During her inpatient stay she acquired a number of hospital-acquired infections. She was found to have Enterobacter cloacae in her sputum while in the intensive therapy unit. Following this, she was found to have Pseudomonas species in her urine while on the medical ward. After several weeks of antibiotic therapy on the medical ward, she was then stepped down again to a rehabilitation ward. Power in her lower limbs returned to near normal. Both her tone and reflexes had returned to normal at this point.
During rehabilitation she went into urinary retention, and an examination noted that she had worsening lower limb weakness in a pattern different from the previous one. The examination also noted an up-going plantar reflex on the left with altered sensation in L4–S1 dermatomes. While on admission there was equal bilateral weakness, this examination showed worsening left-sided weakness. Repeat investigations revealed raised inflammatory markers, and MRI of the spine showed arachnoiditis. This was discussed with the local neurosurgical team, who felt that the patient was not suitable for surgical intervention. She was treated with a further course of intravenous antibiotics and was discharged home with social support.
Investigations
Initially the blood results showed raised inflammatory markers with a C reactive protein (CRP) of 92 and white cell count of 12.5 x 109/L. White cell count showed raised neutrophils (11.8 x 109/L) and low lymphocytes (0.5 x 109/L). She had good renal and liver function on initial blood tests.
These results indicated a few things. First, the elevated CRP suggested inflammation, but ultimately was unhelpful in the diagnosis. Both the raised neutrophils and low lymphocytes suggested to the clinical team that there was more than just a bacterial infection or COVID-19; they were suggestive of a mixed picture. Additionally, the patient had a chest X-ray which showed lower zone consolidation, which was not typical of COVID-19 infection, as shown in figure 1. Additionally, a later CT of the thorax showed the same left lower zone consolidation, again showing pleural effusion and again not typical of COVID-19 infection1 (figure 2).
Figure 1.
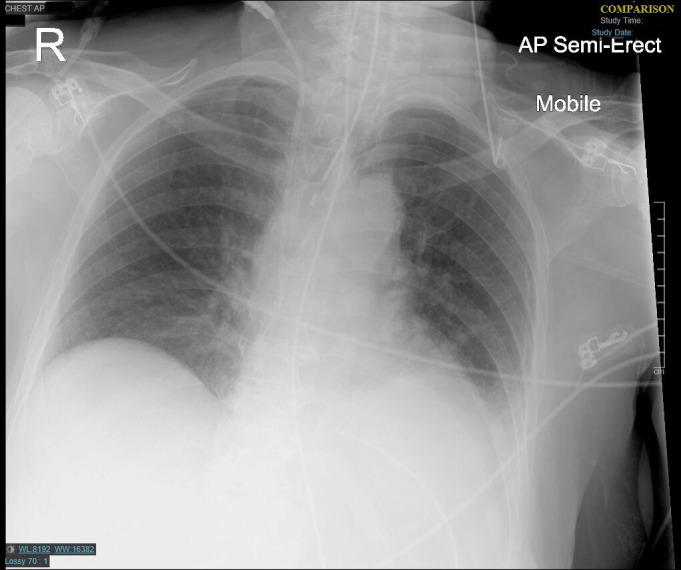
Initial chest X-ray showing non-specific left lower zone opacification. AP, anteroposterior.
Figure 2.

Later CT scan showing left lower zone consolidation and pleural effusion.
On presentation to the emergency department, she underwent a CT of the head due to concerns regarding her consciousness level and confusion. This ruled out the potential for haemorrhagic stroke or space-occupying lesion as the cause of her symptoms; however, the symptoms and examination findings did not point directly to this being the cause of her deterioration.
A lumbar puncture was performed which demonstrated high levels of polymorphic lymphocytes, reduced glucose and increased protein, but no organisms. This sample was further tested using 16S rDNA PCR, which identified E. coli rDNA.
Additionally, a COVID-19 reverse transcription-PCR screening swab was found to be positive. The COVID-19 swab is known to have adequate sensitivity to help diagnose early infection with SARS-CoV-2. The main issue with the COVID-19 swab currently is the interpretation and the significance of a false negative or false positive result.1 In many cases a negative result does not exclude the presence of a COVID-19 infection. In our case the patient had a positive result and therefore this required the clinicians to decide whether this was a false positive or not. A false positive may be due to contamination at any point from sampling to running the swab. As this swab is so new, the percentage of false positives is unknown. As our patient later required respiratory support and elicited symptoms of COVID-19, it is unlikely that this was a spurious result.
SARS-CoV-2 PCR was not performed on the cerebrospinal fluid sample. The initial test was carried out using two gene targets, the E gene and the N2 gene. Both genes were positive (the E gene was positive in 36.4 cycles and the N2 gene was positive in 38.6 cycles). The patient was positive on similar swabs on day 15, day 21 and day 26, and tested negative on day 33.
The swab was valuable as it allowed an alternative potential diagnosis which explained her respiratory symptoms. This allowed us to move forward with treatment as we had determined the cause of her respiratory distress. Additionally, this was taken into account in the decision for her to go to the intensive treatment unit. Blood and urine cultures were negative.
When she deteriorated while in rehabilitation, the team felt that the new changes suggested a spinal pathology, rather than a cranial one. As such, an MRI of the spine was performed in order to identify an evidence of cauda equina syndrome, a lesion or a collection. The MRI showed multilevel degenerative changes, but also an overall appearance of arachnoiditis, affecting the cauda equina, and focal adhesive arachnoiditis at the T10–T11 level. These findings are demonstrated in figures 3–6 in multiple views with different T weighting.
Figure 3.

T1-weighted precontrast MRI sagittal section showing arachnoiditis. HAR, Head Anterior Right; AFR, Anterior Feet Right; FPL, Feet Posterior Left; PHL, Posterior Head Left.
Figure 4.

T1-weighted postcontrast phase on the same location as figure 3.
Figure 5.

T2-weighted sagittal section on the same location as figure 3.
Figure 6.
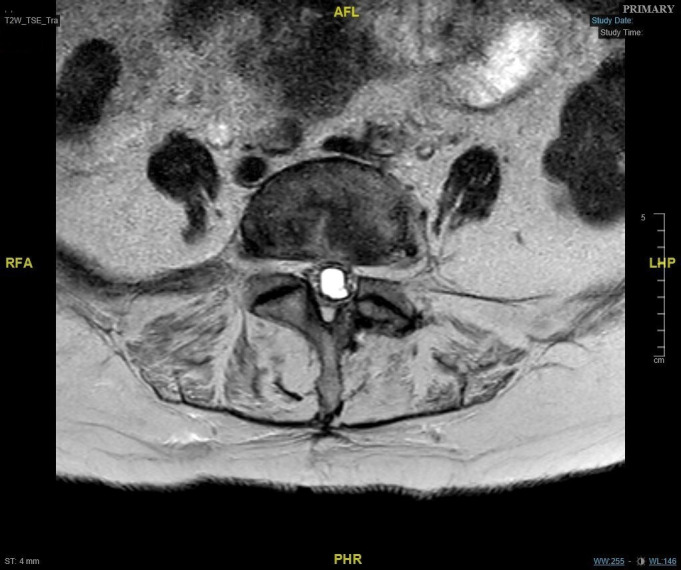
T2-weighted (T2W) MRI axial section demonstrating empty canal sign of arachnoiditis. AFL, Anterior Feet Left; RFA, Right Feet Anterior; LHP, Left Head Posterior; PHR, Posterior Head Right.
Differential diagnosis
The medical team took an inverted pyramid approach to the diagnosis, that is to say they started with a wide base of diagnoses and narrowed it down throughout the initial presentation. The fever, raised inflammatory markers and fluctuating consciousness level in a patient who was otherwise well led the team to believe they were dealing with an acute delirium secondary to an infection.
The first concern was COVID-19, as at the time the country was in the midst of a pandemic. This was also supported by the screening swab result.
The team was unable to conclude that the neurological signs could be explained by COVID-19, which is why they investigated for an acute central nervous system infection. The examination showing focal neurology in a lower limb distribution rather than a left-sided or right-sided distribution led them to feel that this was unlikely to be a stroke disease. The examination picture suggested a possible lower motor neuron picture with flaccid paralysis, areflexia and atonia, which the medical team thought could be consistent with Guillain-Barré syndrome. However, the cognitive changes, fluctuating consciousness level and cranial nerve involvement directed them away from these diagnoses.
The team investigated possible infective causes of neurological deficit from haematological, urinary and central nervous sources through the use of appropriate cultures. This confirmed E. coli meningitis.
When the patient deteriorated on the rehabilitation ward, the medical team had to decide whether this was an extension of her previous illness or a new illness. Here again examinations were helpful as they showed exclusively lower limb and sphincter changes, without the cognitive changes from the patient’s earlier presentation. As such, a spinal cause of the disease was investigated. A spinal MRI was performed which demonstrated arachnoiditis involving the cauda equine.
Throughout, there were concerns that the patient may be having an ischaemic stroke. While this did not fully align with the examination findings, for example there were no upper neuron patterns as there was no increase in tone/spasticity, this was deemed high enough risk to merit investigation. As such, she was investigated with a CT of the head on arrival and again when she deteriorated during rehabilitation.
Treatment
Her initial pharmacological management was with intravenous amoxicillin and intravenous ceftriaxone to treat the bacterial meningitis, as per local trust policy for bacterial meningitis. She underwent a full 14-day course of this intravenously. During this time she required ventilatory support on the intensive care unit, alongside intravenous fluids. She also received some positive inotropic support in the form of a norepinephrine infusion.
Following resolution of this illness she received two further courses of intravenous antibiotics, as intravenous piperacillin with tazobactam. Each course lasted 7 days. These were used to treat a catheter-acquired urinary tract infection and arachnoiditis.
The mainstay of non-pharmacological treatment in this patient was intensive physiotherapy during the final 3 weeks of her admission on a specialist neurorehabilitation ward. The physiotherapy team put emphasis on improving lower limb strength and function.
The speech and language therapists had significant input into the patient due to her suffering with aphonia and swallowing difficulties. It was felt she was at high risk of silent aspiration. She was provided with exercises in order to improve her aphonia and she was initially placed on a level 5 diet; however this was gradually stepped down as her swallowing issues improved.
An interesting aspect of the patient’s care involved the difficulty in communicating with her following discharge from the intensive care unit. Here, she had both hearing loss and aphonia as sequelae of her illness and intubation, respectively. As such, the team emphasised good communication by using a handheld whiteboard with an eraser to write out important communication. She was reviewed by audiology in the clinic and provided with a hearing aid. These measures were maintained on a daily basis until the patient’s hearing and speech improved.
For her discharge, we involved the local social service teams in order to ensure she had the appropriate support she needs in the community.
Outcome and follow-up
The patient improved with each course of antibiotics and her symptoms from meningitis and arachnoiditis have been slowly resolving. Her hearing has now returned, although she is partially deaf and uses hearing aids. Her aphonia from a laryngeal injury while being intubated has resolved completely. She is now able to partially move her legs; however mobility remained an ongoing issue.
She was in high spirits at discharge and was looking forward to seeing her family. Additionally, she was pleased to be out of hospital following her prolonged stay. However, she has since been readmitted for management of an infected sacral sore.
Discussion
A rapid review of COVID-19 cases1 suggests that bacterial or fungal coinfection in COVID-19 is in fact limited, with only 8% of patients identified as having a coinfection. The emphasis of the paper is respiratory infection, and interestingly it highlighted E. cloacae coinfection being identified (although at a low rate), something which this patient also had. However, the belief that there are low levels of coinfection may in fact be incorrect as there is a high amount of use of antibiotics without culture proof of infection, which may well eliminate any possible growth of pathogen in culture.2 3
Additionally, while the team initially dismissed COVID-19 as the sole cause of her symptoms, there are in fact case reports of SARS-CoV-2 causing meningitis and encephalitis in itself. Ahmed et al4 noted that COVID-19 can have a variety of neurological manifestations ranging in severity. They identified cases with meningitis, encephalitis and Guillain-Barré syndrome—all of which could potentially have caused her symptoms and indeed were all considered as differential diagnoses. Additionally, we have identified one report by Tadolini et al5 which identifies tuberculosis meningitis in patients with COVID-19; they felt that the tuberculosis meningitis pre-existed the COVID-19 infection.
In this case, we assumed that the cranial nerve involvement was due to her bacterial meningitis, something which is not unheard of in adults (despite being less common than in children).6 However, as previously mentioned, COVID-19 is known to have a variety of neurological manifestations, and focal cranial nerve involvement has been reported in other viral illnesses (eg, influenza A).7 Ultimately, we do not yet have enough information about this condition to be able to definitively say which will have caused the focal cranial nerve manifestations.
The British Infection Association guidelines for treatment of bacterial meningitis and meningitis in adults8 advise rapid identification of meningitis in adults. In our patient, this was done through identification of the red flag symptoms of headache, fever and altered consciousness. Initial intervention was performed following the guidelines, with rapid assessment and senior clinical review. On initial assessment the patient was not suffering from evolving sepsis but did have suspected meningitis. As mentioned previously, while it is possible that any such disease is caused directly by SARS-CoV-2, the clinical team correctly investigated for other causes, following the British Infection Association guidelines.
As there were no indications to delay lumbar puncture (ie, no evolving rash or severe sepsis, no severe respiratory/cardiac compromise, no significant risk of bleeding and no signs suggestive of shifts in brain compartments) on presentation, the lumbar puncture was performed. The patient was started on an appropriate antibiotic combination; the British Infection Association guidelines advise any penicillin/cephalosporin in a patient over 60 years old, which is what was given along with dexamethasone 6.6 mg intravenously four times a day. The dexamethasone was given 1 week after treatment with antibiotics had been initiated, during which time she had already required ventilator support due to pulmonary COVID-19 infection.
The next stage in the guidelines advises careful monitoring and review. This was performed and allowed the team to identify deterioration in the patient requiring critical care escalation.
Interestingly, there is a very low incidence of E. coli meningitis in the community, with the majority of the acquisition being secondary to neurosurgical intervention or occurring in neonates.9 10 Acquisition of Gram-negative bacterial meningitis in the community is usually linked to a range of pre-existing risk factors, including chronic alcoholism with cirrhosis, diabetes mellitus, disseminated strongyloidiasis with HIV, chronic obstructive pulmonary disease and chronic organ failure. There are a range of other, less common, associated risk factors.11 12 Importantly, our patient did not have any of these risk factors.
By being previously fit and well, our patient is in the minority of patients who had E. coli meningitis, making it quite a surprising final diagnosis. Additionally, by being discharged with good outcome, she is again in the minority of patients with this condition.12 Alongside this, her coinfection with COVID-19 appears to be the first such case in the literature.
Learning points.
When a patient presents with non-specific symptoms, particularly with confusion, it is important not to forget to carry out a thorough examination of relevant body systems.
Examination also allows monitoring of the patient’s condition and identification of any changes early on, which may lead to alternative differential diagnoses or investigations if required.
Even if the patient is complex, something as simple as good quality history and examination can point to the right direction.
It is worth identifying how to ensure the patient can communicate, even if it seems difficult to, as this will allow for a better patient journey and better care.
It may be interesting to review future cases to see if COVID-19 infection is an independent risk factor for Escherichia coli meningitis in adults.
Acknowledgments
Many thanks to Dr Hirak Mukherjee for providing the patient with an updated copy of the case report and providing her with a correctly dated consent form for signature. Many thanks to Victoria Blakey for her clarification regarding the patient’s PCR testing.
Footnotes
Twitter: @EliotMBHurn
Correction notice: This article has been corrected since it has been published online. The author name has been corrected from "Jijie Annie Abraham" to "Jijee Annie Abraham".
Contributors: EH contributed to writing of the main body and case note analysis, including external research and formatting. He explained the concept of consent, went through the case report with the patient and obtained initial consent from the patient. After edits to the case report were made, he contacted Dr Mukherjee to provide the patient with an updated draft of the report and to sign a newly dated consent form. LD contributed to the writing of this piece through drafting and manuscript revisions as well as research for the article. The patient was under the clinical care of JAA. The patient had E. coli meningitis, which is not a common cause of meningitis in adults. She also had concomitant COVID-19 and this was something not yet reported in journals. The patient's complications, namely complete third nerve palsy, eighth nerve palsy and arachnoiditis, were all equally interesting as was her progressive improvement. For these reasons, JAA chose to pick this case for write-up. JAA has been actively involved in literature search, discussion with the radiologist, patient’s progress and editing and referencing this case presentation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Long C, Xu H, Shen Q, et al. Diagnosis of the coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol 2020;126:108961. 10.1016/j.ejrad.2020.108961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis 2020;71:2459–68. 10.1093/cid/ciaa530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang C-Y, Chan K-G. Underestimation of co-infections in COVID-19 due to non-discriminatory use of antibiotics. J Infect 2020;81:e29–30. 10.1016/j.jinf.2020.06.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmed MU, Hanif M, Ali MJ, et al. Neurological manifestations of COVID-19 (SARS-CoV-2): a review. Front Neurol 2020;11. 10.3389/fneur.2020.00518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tadolini M, Codecasa LR, García-García J-M, et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J 2020;56:2001398. 10.1183/13993003.01398-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Senda J, Adachi T, Tago M, et al. Acute bilateral oculomotor nerve palsy in an adult patient with Neisseria meningitidis. Intern Med 2019;58:1639–42. 10.2169/internalmedicine.2098-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Senda J, Araki K, Tachi Y, et al. Acute unilateral isolated oculomotor nerve palsy in an adult patient with influenza A. Intern Med 2019;58:433–6. 10.2169/internalmedicine.0850-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.British Infection Association . Early management of suspected meningitis and meningococcal sepsis in immunocompetent adults, 2020. Available: https://www.britishinfection.org/application/files/5414/5674/3289/algorithm.pdf [Accessed 20 Jul 2020].
- 9.Tunkel A, Hasbun R, Bhimraj A. Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis*. Clinical Infectious Diseases 2017;2017:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Unhanand M, Mustafa MM, McCracken GH, et al. Gram-Negative enteric bacillary meningitis: a twenty-one-year experience. J Pediatr 1993;122:15–21. 10.1016/S0022-3476(05)83480-8 [DOI] [PubMed] [Google Scholar]
- 11.Bichon A, Aubry C, Dubourg G, et al. Escherichia coli spontaneous community-acquired meningitis in adults: a case report and literature review. Int J Infect Dis 2018;67:70–4. 10.1016/j.ijid.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 12.Bodilsen J, Brouwer MC, Kjærgaard N, et al. Community-Acquired meningitis in adults caused by Escherichia coli in Denmark and the Netherlands. J Infect 2018;77:25–9. 10.1016/j.jinf.2018.05.009 [DOI] [PubMed] [Google Scholar]


