Abstract
Introduction
Parenting interventions during early childhood are known to improve various child development outcomes immediately following programme implementation. However, less is known about whether these initial benefits are sustained over time.
Methods
We conducted a systematic literature review of parenting interventions in low- and middle-income countries (LMICs) that were delivered during the first 3 years of life and had completed a follow-up evaluation of the intervention cohort at least 1 year after the primary postintervention endpoint. We summarized intervention effects over time by child-level and parent-level outcomes as well as by timing of follow-up rounds in the short-term (1–3 years after programme completion), medium-term (4–9 years), and long-term (10+ years). We also conducted exploratory meta-analyses to compare effects on children’s cognitive and behavioral development by these subgroups of follow-up rounds.
Results
We identified 24 articles reporting on seven randomised controlled trials of parenting interventions delivered during early childhood that had at least one follow-up study in seven LMICs. The majority of follow-up studies were in the short-term. Three trials conducted a medium-term follow-up evaluation, and only two trials conducted a long-term follow-up evaluation. Although trials consistently supported wide-ranging benefits on early child development outcomes immediately after programme completion, results revealed a general fading of effects on children’s outcomes over time. Short-term effects were mixed, and medium-term and long-term effects were largely inconclusive. The exploratory meta-analysis on cognitive development found that pooled effects were significant at postintervention and in the short-term (albeit smaller in magnitude), but the effects were not significant in the medium-term and long-term. For behavioural development, the effects were consistently null over time.
Conclusions
There have been few longer-term follow-up studies of early parenting interventions in LMICs. Greater investments in longitudinal intervention cohorts are needed in order to gain a more comprehensive understanding of the effectiveness of parenting interventions over the life course and to improve the design of future interventions so they can have greater potential for achieving and sustaining programme benefits over time.
Keywords: prevention strategies, child health
Key questions.
What is already known?
Parenting interventions during early childhood are effective for improving early child development outcomes immediately following programme implementation.
Although a few individual parenting interventions have demonstrated longer-term benefits on certain child development outcomes, a systematic review of this literature has not previously been conducted.
What are the new findings?
Our review identified seven randomised controlled trials of parenting interventions that were delivered during early childhood and conducted at least one follow-up of the intervention trial cohort in a low- and middle-income country.
We found a general fading of intervention impacts on children’s development outcomes over time, with mixed results for short-term effects and largely inconclusive results for medium-term and long-term effects.
What do the new findings imply?
Additional follow-up evaluations are needed to gain a fuller understanding of the short-term, medium-term and long-term effects of early childhood parenting intervention and to inform the design of improved interventions that can maximize and sustain gains in child development outcomes over the life course.
Introduction
Globally 43% of children under 5 years are failing to attain their developmental potential due to poverty, poor health and inadequate stimulation.1 The first 3 years of life are a particularly sensitive period of brain and social development, during which parents are the primary providers of care for young children.2 Parenting interventions during the earliest years of life are effective for improving a wide range of outcomes.3 For example, reviews of common parenting interventions during early childhood—such as psychosocial stimulation,4 5 dialogical reading6 and attachment interventions7—have consistently revealed positive effects on children’s cognitive, language, motor and behavioural development outcomes, as well as parenting knowledge, practices and parent–child interactions immediately after the completion of the intervention.8
Parenting interventions during early childhood have received increasing policy attention globally.9 Policymakers and researchers have argued that if interventions can positively affect children’s cognitive and socioemotional development in the short run during the formative years of early childhood, then such effects may place children on more positive lifelong trajectories to offset the adverse effects of poverty and promote child development over the life course. In addition to the potential for reducing life course inequalities, it has been argued that early life interventions are worth scaling up because they can greatly reduce governmental support needs in the long run.10 Yet, experimental evidence to support longer-term effectiveness is in fact scarce.
Much of the limited literature on follow-up effects of early parenting interventions, and early interventions more broadly, comes from high-income countries (HICs).11 The majority of these follow-up studies have been small efficacy trials, targeted to vulnerable or at-risk populations (eg, families facing psychosocial risks12 or preterm infants13) and limited to short-term follow-up studies showing some sustained benefits during preschool or middle childhood. Only a few trials have shown persisting long-term benefits on select adolescent or adult development outcomes.14 15 The acclaimed adult economic payoffs for investing in early childhood programmes have primarily emerged from two small-scale studies in the United States: the Abecedarian Project16 and the Perry Preschool project.17 However, as more studies have become available, diminishing intervention impacts have been observed over time, suggesting that general claims of the longer-term benefits of early interventions may be overestimated.18
Despite the considerable number of parenting interventions that have been evaluated in low-income and middle-income countries (LMICs),3 5 there have been far fewer follow-up studies in LMICs as compared with HICs. One of the oldest and most prominent examples is the Jamaica Home Visiting programme. In a small efficacy trial, 127 undernourished infants under age 2 years from poor neighbourhoods of Kingston, Jamaica, were randomly assigned to receive weekly home visits from nurses and one of four interventions over a 2-year period: psychosocial stimulation, nutritional supplementation, stimulation and supplementation, or standard healthcare services.19 This intervention cohort has been followed to date across childhood, adolescence and early adulthood, with results revealing sustained benefits of the early stimulation intervention on adolescent and early adult outcomes, such as higher educational attainment, reduced depression and higher earnings at the age of 22 years.20 21 The positive results from this small efficacy study have been widely cited in support of investing and making policy decisions about the potential of scaling up early parenting interventions in LMICs.
Our study aimed to contextualise and synthesise these findings with the emerging body of follow-up studies. We review the literature on parenting interventions delivered during the first 3 years of life in LMICs that also completed at least one subsequent follow-up evaluation. We summarise intervention characteristics, follow-up study designs and intervention effects over time on a broad and inclusive range of child and parent outcomes. Finally, we highlight the implications of our findings with regard to the design, implementation and evaluation of future parenting interventions, and discuss possible strategies for sustaining programme benefits over the life course.
Methods
Search strategy
A systematic literature review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. The methods were prespecified and documented in a protocol (PROSPERO number CRD42020199665). Six electronic bibliographic databases (MEDLINE, Embase, PsycINFO, CINAHL, Web of Science and Global Health Library) were searched for peer-reviewed, published articles from database inception until 18 July 2020. A string of search terms combined keywords for concepts relating to parenting, early childhood development (ECD), randomised controlled trials (RCTs) and LMICs (online supplemental table S1). A similar search strategy was used for a separate review investigating the immediate effects of parenting interventions on ECD and parenting outcomes.8 Reference lists of relevant studies were scanned for any additional studies that may have been missed.
bmjgh-2020-004067supp001.pdf (1.2MB, pdf)
Selection criteria
Full-text, peer-reviewed articles in English were included if they met the following criteria: (1) parenting interventions that aimed to improve caregiver interactions, behaviours, knowledge, beliefs, attitudes or practices with their children in order to primarily improve ECD; (2) targeted caregivers and young children during the period of early childhood or specifically preconception through the first 3 years of life; (3) interventions evaluated using a randomised controlled study design; (4) had at least one follow-up study that was conducted at least 1 year after the primary postintervention endpoint; and (5) measured a developmental outcome in one of the follow-up studies. Studies were excluded if they met any of the following criteria: (1) represented interventions that did not focus on parenting for ECD; (2) targeted a population of children who were, on average, older than 36 months (eg, preschoolers and school-aged children); or (3) did not conduct a follow-up assessment after the primary postintervention evaluation round.
Data extraction
Two reviewers (JJ and research assistant) independently screened the titles and abstracts of each study identified in the systematic search. Full texts of selected studies were reviewed to assess eligibility. Reference lists of included studies and previous reviews were examined to identify any potentially relevant publications not found through the electronic search. Any discrepancy between the reviewers was resolved through discussion and consensus.
Two reviewers (JJ and HOP) independently extracted data from each eligible study using a structured form. The main categories of data that were extracted for each study included characteristics of the sample, intervention details, timeline of follow-up, outcome measures used in follow-up studies and findings over time. Follow-up studies and results were organised according to the original trial. Any discrepancies were resolved through discussion and consensus.
Outcomes
The primary outcomes focused on measures of child development, which included children’s cognitive, language, motor, executive functioning, and socioemotional and behavioural outcomes. Secondary outcomes included any other child-level outcomes over the life course, including education, physical and mental health, and economic productivity. We also considered parent-level outcomes, such as parenting behaviours or parental depressive symptoms. We aimed to be as inclusive as possible in our review of secondary outcomes.
Risk of bias assessment
Two reviewers (JJ and HP) independently assessed risk of bias in included studies using the Cochrane Collaboration Risk of Bias Tool. Categorical ratings of high, low or unclear were assigned with regard to random sequence generation, blinding of participants and personnel, incomplete outcome data and selective reporting in each study. Any discrepancies were resolved through discussion and consensus.
Data synthesis
The main results for each trial were summarised in a table that described the original intervention, the number of follow-up studies, the relevant outcome measures assessed and the intervention effects for each outcome. The outcomes and specific measures used across all studies were summarised. Intervention effects were narratively synthesised by type of outcomes (ie, child-level or parent-level outcomes) and timing of follow-up (ie, short-term (1–3 years), medium-term (4–9 years) or long-term (10+ years)). In multiarm trials, we focused on the main effect of the parenting intervention. For example, with studies that used 2×2 factorial cluster RCT design, we compared the two arms that received the parenting intervention to the other two that did not receive the parenting intervention. Due to the varied nature of timing of follow-up studies and outcomes assessed, we primarily conducted a descriptive synthesis of results.
We conducted exploratory meta-analyses on any child development outcome that was repeatedly measured by at least two trials across two out of the three follow-up time frames. As applicable, we calculated effect sizes or the standardised mean differences (SMDs) in the outcome between the parenting intervention and control arms divided by the pooled SD. We reported the effect sizes for each study across follow-ups. Using a stratified random effects meta-analysis model, we explored subgroup differences in the pooled effect sizes by timing of follow-up (ie, postintervention, short-, medium- and long-term). We descriptively compared pooled effects over time by magnitude of estimates rather than statistical testing between subgroups, given the limited number of studies. Figures illustrating the effect sizes across studies and follow-up time points were created in R. Meta-analyses and forest plots were conducted in Stata V.16.
Patient and public involvement
Patients or the public were not involved in the design and conduct of this research.
Results
Search result details
The structured search identified 6620 unique records, and we found an additional 15 relevant articles through scanning references and one article that was published after the search was conducted and identified based on authors’ personal knowledge (online supplemental figure S1). Ultimately, a total of 24 articles met the inclusion criteria. These articles corresponded to seven unique intervention cohorts.
Intervention and implementation characteristics
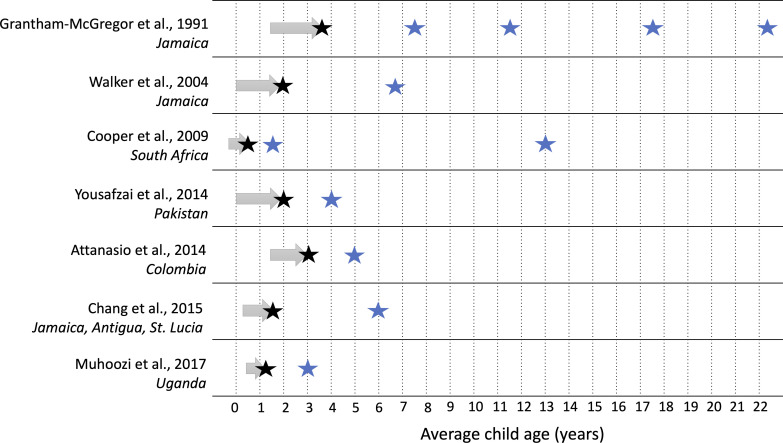
Table 1 presents details of the intervention content, setting, duration, intensity and original study designs of the seven RCTs included in the review. All seven interventions targeted mothers and incorporated components of psychosocial stimulation to enhance engagement in play and early learning activities or responsive caregiving to improve ECD outcomes. Three of the trials also provided nutritional support (supplementation and/or infant feeding education)19 22–24; one was embedded into an existing cash transfer programme22; and one was delivered as part of routine child health visits.25 Collectively, the interventions were conducted in seven countries: Jamaica, Uganda, Colombia, South Africa, Pakistan and a multisite study in the Caribbean (Jamaica, Antigua and St. Lucia). Publication dates of original trial results ranged from 1991 to 2017. Enrolled sample sizes of the trials ranged from 12719 to 1411.24 Three of the seven RCTs used a 2×2 factorial design with stimulation, nutrition and combined intervention arms in addition to a control arm (with one study including a non-stunted population control group),19 22 24 whereas the remaining four trials tested an intervention against a control group (with one study including an additional normal birthweight control group). The original interventions began between pregnancy and 18 months of age and lasted between 6 and 24 months (figure 1). Intervention delivery occurred through weekly contacts in two trials, approximately biweekly contacts in three trials, in two stages of weekly home visits after a 5-month break in one trial, and during five routine health visits over 15 months in one trial. The total programme contacts ranged from 525 to 96 contacts.19
Table 1.
Summary of parenting interventions and populations included in systematic review (in order of original trial publication date)
| Primary impact paper, country | Study design (arms, n) |
Sample size at enrolment | Setting | Population and child age at enrolment | Intervention dosage, total duration (contacts, n) | Original intervention description and control condition |
| Grantham-McGregor et al,19 Jamaica |
2×2 factorial individual-level RCT (among stunted children) also with a non-stunted control:
|
Stimulation (stunted): 64 No stimulation (stunted): 65 |
Urban | Children aged 9–24 months with height-for-age <−2 SDs, mothers with singleton pregnancy, BW >1/8 kg, housing and maternal education below predefined levels, no obvious physical or mental disabilities | Weekly home visit total duration of 24 months (96 contacts) | Stimulation: community health aides visited the homes for 1 hour/week and taught the mothers how to play with their children to promote their development. Homemade toys were left in the home at each visit, and the mothers were encouraged to play with their children daily. Supplementation: 1 kg milk-based formula/week Control: free medical care was available to all children. Children in the four stunted groups were visited every week by a community health aide, and a history of the previous week’s illnesses was recorded. |
| Walker et al,36 Jamaica |
Individual-level RCT among LBW children, also with a NBW control:
|
Intervention (LBW): 70 Control (LBW): 70 |
Urban | Enrolled LBW, term newborns whose mothers had an education level below three secondary-evel examination passes; excluded twins, those with congenital abnormalities, receiving special care nursery, and HIV-positive mothers | Weekly home visits from birth to 2 months of age (first 8 weeks, 60 min/visit); break for 5 months, then weekly home visits again from 7 to 24 months of age (30 min/visit); total duration of 19 months (76 contacts) | The first phase during the child’s first 8 weeks of life focused on improving the mothers’ responsiveness to their infants. Community health workers encouraged mothers to converse with and sing to their infants, respond to their cues, show affection and focus their attention on the environment. The second phase of intervention began after a 5-month interval and was conducted from 7 to 24 months of age, during which the community health worker demonstrated play techniques to the mother and involved her in a play session with the child. Toys made from commonly available recyclable materials were left in the home each week. Control condition unclear, likely standard of care services for LBW |
| Cooper et al,28 South Africa |
Individual-level RCT:
|
Intervention: 220 Control: 229 |
Periurban | Enrolled pregnant women during third trimester | Two home visits in pregnancy, 14 home visits in the first 6 months; 1 hour/home visit, total duration of 9 mo (16 contacts) | Trained community volunteer women provided mothers with psychological support to encourage maternal sensitive and responsive interactions with her infant and improve her infant attachment relationship (ie, supporting the management of infant distress and sensitising mothers to infant social cues and attachment needs). Control condition: standard of care involving fortnightly visits by a community health worker who assessed the physical and medical progress of mothers and infants, and encouraged well child visits at the local clinic |
| Yousafzai et al,24 Pakistan |
2×2 factorial cluster RCT:
|
Responsive stimulation: 757 No responsive stimulation: 732 |
Rural | Children aged 0–2.5 months without signs of severe impairments | Monthly home vists (30 min/session) and monthly group sessions (80 min/session), total duration of 24 months (48 contacts) | For the responsive stimulation intervention, LHWs promoted caregiver sensitivity, responsiveness and developmentally appropriate play between caregiver and child (using adapted version of care for child development). For the enhanced nutrition intervention, LHWs provided nutrition education, and all children aged 6–24 months in this group were given a multiple micronutrient powder as part of home visit. Control condition: standard-of-care services provided by LHWs, including health, hygiene and basic nutrition education |
| Attanasio et al,22 Colombia |
2×2 factorial cluster RCT:
|
Stimulation: 720 No stimulation: 709 |
Multiple regions, at-scale | Targeted socioeconomically vulnerable families who were beneficiaries (poorest 20% of households) of the Familias en Acción conditional cash transfer programme Enrolled children 12–24 months |
Weekly home visits total duration of 18 months (72 contacts) | Parenting intervention: mother leaders demonstrated play activities using low cost or homemade toys, picture books, and form boards. These materials were left in the homes for the week after the visit and were changed weekly. The aims of the visits were to improve the quality of maternal–child interactions and to assist mothers to participate in developmentally appropriate learning activities, many centred on daily routines. Nutrition intervention: daily micronutrient sprinkles for child, which were distributed to households every 2 weeks. Control condition: existing Familias en Acción government conditional cash transfer programme |
| Chang et al,25 Jamaica, Antigua, St. Lucia |
Cluster RCT:
|
Intervention: 251 Control: 250 |
Select regions in each country | Mother and infants at the postnatal visit to primary health clinic 6–8 weeks; excluded infants born preterm, multiple births, or those admitted to the special care nursery for >48 hours after birth |
Five routine primary health clinic visit for infants at 3, 6, 9, 12 and 18 months of age, total duration of 15 months (five contacts) |
Intervention integrated into routine primary health services for infants. Responsive stimulation messages were delivered through short video films played in health facility waiting area. Community health workers facilitated group discussions about the films with mother–child dyads and provided demonstrations and opportunities for mothers to practise stimulation activities. During well-baby visit, nurse reinforced short film messages about stimulation and provided mothers with message cards to take home. At ages 9 and 12 months, nurses gave the parents a picture book, and at 18 months a three-piece puzzle to take home. Control condition: usual primary care for infants at community health clinics |
| Muhoozi et al,23 Uganda |
Cluster RCT:
|
Intervention: 263 Control: 248 |
Rural | Targeted impoverished mothers; enrolled children aged 6–8 months, excluding those with congenital malformations, physical disorder, or mental illness |
Three supervised group meetings (6–8 hours each), monthly mothers group meetings+monthly home visits; total duration of 6 months (15 contacts) | Intervention focused primarily on infant complementary feeding, cooking demonstrations, and hygiene and sanitation, and additionally emphasised the importance of play for early child development. Full-day group meetings were facilitated by bachelor-level nutritionists, and monthly home visit and mothers peer group sessions were facilitated by volunteer mother. Control condition unclear |
BW, birth weight; LBW, low-birthweight; LHW, Lady Health Worker; NBW, normal-birthweight; RCT, randomised controlled trial.
Figure 1.
Evaluation rounds of included parenting interventions. Note: Arrows represent intervention timing and duration. Black stars represent postintervention evaluation. Blue stars represent follow-up evaluations.
Risk of bias across the trials was generally low for blinding of outcome assessors and selective reporting across studies (online supplemental table S2). Risk of bias for allocation concealment and random sequence generation for the original trials was mostly unclear. Incomplete outcome data particularly for the follow-up studies were high in half of the trials. Given the nature of psychoeducational and behavioural parenting interventions that involve parents’ active participation, blinding of participants was not possible.
Follow-up study details
The seven trials included in this review correspond to a total of 11 follow-up evaluations that were conducted one or more years after an immediate postintervention evaluation. Figure 1 presents the number and timing of follow-up evaluations for each of the included trials. The numbers of follow-up rounds per trial were one (five trials), two (one trial) and four (one trial). Four trials conducted short-term follow-ups with assessments 1–3 years after intervention completion; three had medium-term follow-ups 4–9 years after intervention completion; and two covered long-term follow-ups 10+ years after intervention completion. The oldest mean age at follow-up was 22.6 years. The proportion of the original sample revisited during the follow-ups ranged from 29% (a random subset by design)26 to 98%27 (table 2).
Table 2.
Effects of parenting interventions on child development and parent-level outcomes across follow-up studies
| Primary impact paper, country | Post intervention evaluation round |
Child age at assessment | Analytical sample size (% of originally enrolled) | Child development outcomes assessed: domains (measure) | Parenting intervention impacts on child development outcomes | Parent outcomes: domains (measure) | Parenting intervention impacts on parent outcomes |
| Grantham-McGregor et al,19 Jamaica |
One of five19 | 3–4 years (primary endpoint) | 127 (98%) | Global developmental quotient, which includes hearing and speech, hand and eye, performance, and locomotor subscales (Griffiths Mental Development Scales) | Stimulation intervention improved all the subscales and overall developmental quotient. The stimulation x supplementation interaction term was not significant in any of the regressions. | Stimulation in the home (modified HOME) | The HOME score of the treatment group was 16% greater than that of the control group.20 |
| Two of five27 | 7–8 years | 127 (98%) | School achievement (WRAT) Intelligence quotients (Stanford Binet) Language comprehension (PPVT) Visual reasoning ability (Raven’s Progressive Matrices) Categorical fluency (naming as many items as possible in 1 min) Verbal analogies (11 analogical reasoning problems) and long-term semantic memory (free recall) Paired-associate learning task (French learning test) Auditory working memory (digit span) Visual–spatial working memory (Corsi blocks) Fine motor coordination (Lafayette Grooved Pegboard Test) Factor analysis of the development measures constructed (PCA with varimax rotation) resulted in three factors: general cognitive factor (first factor had most tests loading onto it), perceptual–motor factor and long-term semantic memory |
Stimulation arm had significantly higher scores on child development factor 2, no other factors or outcomes. Sign test conducted to examine the direction (not magnitude) of the effects for the child development outcomes, supplemented and combined group had better scores than the control group on more tests than would be expected by chance (14/15, p<0.01), and stimulated group did better than control in 13/15 (p<0.05) | Stimulation (13 questions about stimulation in the home) | There was no difference between the treatment and control groups.20 | |
| Three of five33 34 | 11–12 years | 116 (90%) | General intelligence (WISC-R; verbal and performance subscales) Visual reasoning ability (Ravens Progressive Matrices) Language comprehension (PPVT) Verbal analogies (no specific test mentioned) Vocabulary (modified subset of the Stanford Binet) Auditory working memory (two tests digit span forwards and backwards) Visual–spatial memory (Corsi blocks) Visual information processing and sustained attention (Search Test) Ability to inhibit responses and the speed of processing: modified Stroop Tests School and home behaviours (Rutter Teacher and Parent Scales) School achievement (WRAT) |
Children who had received stimulation, with or without supplementation, had significantly higher scores on the WISC-R Full Scale and Verbal scale, Ravens Progressive Matrices, and the Vocabulary Test. | Stimulation in the home (HOME-like questions, including the presence of homework facilities, reading and play materials, and interactions with adults) | There was no difference between the treatment and control groups.20 | |
| Four of five21 51 | 17–18 years | 103 (80%) | Cognitive function (WAIS) Non-verbal reasoning (Raven’s Progressive Matrices) Visual spatial working memory (Corsi blocks test) Auditory working memory (digit span forwards and backwards subsets of the WAIS) Language (Verbal Analogies Test and PPVT) Reading ability (Reading Test 2–Revised) Math ability (WRAT for math) Education (highest grad attained, or current grad) Self-esteem (How I Think About Myself Questionnaire) Anxiety (What I Think and Feel Questionnaire) Depression (Short Mood and Feelings Questionnaire) Antisocial behaviour (Behaviour and Activities Checklist) Attention deficit Cognitive problems or lack of attention Hyperactivity Oppositional behaviour Social behaviour (sexual relationships, pregnancy, contact with the police, exposure to violence) |
Children who received psychosocial stimulation had significantly better scores on the WAIS Full Scale and Verbal Subscale, and on the PPVT, Verbal Analogies test, and sentence completion and context comprehension reading tests. After adjustment for covariates, the benefits remained significant and the effects of stimulation approached significance for Raven’s Progressive Matrices and the performance subscale of the WAIS. Multivariate analysis of variance with all behavioural outcomes as the dependent variables and supplementation and stimulation as factors indicated a significant effect of stimulation. Participants who received stimulation reported less anxiety, less depression and higher self-esteem, and parents reported fewer attention problems. These differences are equivalent to effect sizes of 0.40–0.49 SD. No effect on antisocial behaviour, cognitive problems, lack of attention, hyperactivity, oppositional behaviour or social behaviours |
None | None | |
| Five of five 20 52 | 22–23 years | 105 (83%) | Cognition/IQ (WAIS) Educational achievement (reading and mathematics from WRAT, Expanded Form; highest grade level attained; secondary level examination passes; expulsion from school; postsecondary school education or skills training) General Knowledge (a test of practical general knowledge useful for daily living in Jamaica) Mental health (Short Mood and Feelings Questionnaire; anxiety was assessed with the State-Trait Anxiety Inventory; Social inhibition subscale from the adapted Inventory on Interpersonal Problems). Antisocial behaviour, arrests, convictions (self-reported involvement in fights, use of weapons, stealing, burglary, rape and gang membership; participant reports of arrests and convictions also were collected). Factor analysis with varimax rotation was used to reduce the number of items related to violent behaviour and to identify underlying constructs (four factors). Other behaviour (relationships with parents and with partners, sexual relationships, number of children and age at birth of first child, alcohol and drug use, church attendance and community involvement) and earnings (log monthly earnings) |
Stimulation had significant benefits to IQ and mathematics and reading scores. Stimulation benefitted general knowledge in the residents; among the resident sample, stimulation increased the highest grade level attained and the number of secondary-level examination passes, with similar non-significant trends for the total sample. Stimulation led to significant reductions in symptoms of depression and in social inhibition but was not associated with levels of anxiety. The stimulation groups tended to be less likely to be involved in fights (OR=0.36) and were significantly less likely to be involved in more serious violent behaviour (OR=0.33). There were no significant differences among the groups in alcohol consumption, cigarette smoking, marijuana use, detention by the police, being charged with a crime, being convicted of a crime, the quality of their relationships with their mothers, fathers, or partners, or in the number of sexual partners, condom use, use of birth control, or additional training after secondary school. The estimated impacts on log earnings show that the intervention had a large and statistically significant effect on earnings. Average earnings from full-time jobs are 25% higher for the treatment group than for the control group, and the impact is substantially larger for full-time permanent jobs. |
None | None | |
| Walker et al,36 Jamaica |
One of two36 | 2 years (primary endpoint) | 130 (93%) | Global developmental quotient, which includes hearing and speech, hand and eye performance, and locomotor subscales (Griffiths Scales) | The intervention did not improve global developmental quotient. For the subscales, improvements were observed in the hand and eye and performance subscales; but not the hearing and speech and locomotor subscales. | Maternal stimulation (HOME) measured at child age 12 months | Intervention did not improve total HOME score. Improvements were observed in avoidance of restriction and punishment, and maternal involvement subscales, but not in the three other subscales (emotional and verbal responsivity, organisation of the environment, and play materials). |
| Two of two32 | 6.8 years | 112 (80%) | IQ (WPPSI), vocabulary (PPVT), Memory (Digit Span Forward Test, Corsi Blocks Test) Attention (Test of Everyday Attention for Children), reading (Early Reading Assessment), behaviour (SDQ) | The intervention group had significantly better scores in performance IQ (d=0.38), visual–spatial memory (d=0.53), and fewer behaviour difficulties (d=0.40) than the control group. No difference between groups for full-scale IQ, digit span memory, attention, PPVT, early reading. | Parenting practices (HOME- middle childhood) | No difference between groups in HOME- middle childhood | |
| Cooper et al, 2009 South Africa28 |
One of three28 | 6 months (primary endpoint) | 354 (79%) | None | None | Mother–child interactions (structured play interaction coded for maternal sensitivity and intrusive–coercive control), clinical diagnosis of maternal depression (DSM-IV diagnosis) and maternal depressive symptoms (EPDS) | Mothers in the intervention group were significantly more sensitive (d=0.24) and less intrusive (d=0.26) in their interactions with their infants. No significant reductions in maternal depressive disorder. However, reductions were observed in maternal depressive symptoms |
| Two of three27 37 | 18 months | 342 (76%) | Attachment security (Ainsworth strange situation procedure, coded for secure and insecure attachments), cognitive development (BSID-II) | The intervention was also associated with a higher rate of secure infant attachments (OR=1.70, p<0.05). No significant differences in insecure attachments. Intervention trended towards significant improvement in cognitive development (d=0.20, p=0.09). | None | None | |
| Three of three53 | 13 years | 333 (74%) | Language (KABC-II, specifically the Riddles Subtest), behaviour (CBCL) and self-esteem (Self-Esteem Questionnaire) | Parenting intervention did not improve any child outcomes. | Maternal depressive symptoms (PHQ-9) | Parenting intervention did not reduce maternal depressive symptoms | |
| Yousafzai et al,24 Pakistan |
One of two24 35 | 2 years (primary endpoint) | 1411 (95%) | Cognitive, language, motor and socioemotional development (BSID-III) | Responsive stimulation intervention improved child cognitive (d=0.6), language (d=0.7) and motor development (d=0.5). However, no effect was observed for child socioemotional development. | Maternal knowledge of early childhood development (developed by authors), parenting practices (HOME, FCI), mother–child interactions (OMCI), depressive symptoms (SRQ) | Responsive stimulation intervention improved maternal knowledge (d=1.1), practices (HOME, d=0.9) and mother–child interactions (d=0.8). However, no effect was observed for maternal depressive symptoms (d=0.1). |
| Two of two30 | 4 years | 1302 (87%) | Child IQ (WPPSI), executive functioning (fruit Stroop task, knock-tap task, big–little task, go/no go task, forward word span and separated dimensional change card sort), preacademic skills (Bracken School Readiness Assessment, Third Edition), prosocial behaviours (SDQ), motor development (Bruininks-Oseretsky Test for Motor Proficiency-II, Brief Form), preschool enrolment rates | Responsive stimulation intervention improved IQ (d=0.1), executive function (d=0.3), preacademic skills (d=0.35) and prosocial behaviours (d=0.2). No differences were observed for behavioural problems, motor development or preschool enrolment rates. | Mother–child interactions (OMCI), parenting practices (HOME early childhood version and FCI) and maternal depressive symptoms (SRQ) | Responsive stimulation intervention improved mother–child interactions (d=0.25) and parenting practices (HOME, d=0.3). However, no differences were observed for maternal depressive symptoms. | |
| Attanasio et al,22 Colombia |
One of two22 | 30–42 months (primary endpoint) | 1263 (88%) | Cognitive, receptive language, expressive language, fine motor and gross motor development (BSID-III) | Parenting intervention improved cognitive scores (d=0.26) and receptive language (d=0.22); no impact on expressive language, and fine and gross motor scores | Maternal stimulation practices and play materials (FCI), depressive symptoms (CES-D) | Parenting intervention improved the amount of stimulation (play activities and play materials) being provided by parents in the home (d=0.34); no effect of parenting intervention on maternal depression. |
| Two of two54 | 4.5–5.5 years | 1256 (88%) | Cognition (Woodcock-Munoz), language (Woodcock-Munoz, PPVT), school readiness (Daberon Screening for School Readiness), executive function (pencil tapping task), child behaviour (SDQ and Children’s Behaviour Questionnaire) | Parenting intervention did not improve any child outcomes. | Maternal stimulation practices and play materials (FCI), depressive symptoms (CES-D) | Parenting intervention did not improve any maternal outcomes. | |
| Chang et al,25 Jamaica, Antigua, St. Lucia | One of two25 | 18 months (primary endpoint) |
426 (85%) |
Global developmental quotient, which includes hearing and speech, hand and eye, and performance subscales (Griffiths Scales); vocabulary (MacArthur-Bates Short Form of the CDI) |
Intervention improved cognitive development subscale of Griffiths; no impacts on other subscales or global developmental quotient of Griffiths or vocabulary score | Maternal knowledge of care practices (developed by authors), parenting practices (HOME), depressive symptoms (CES-D) | Intervention improved maternal knowledge of care practices (d=0.4); no impacts on parenting practices or maternal depressive symptoms. |
| Two of two31 | 6 years | 262 (66% of the original subsample from Jamaica; however, this follow-up subsample (only Jamaica) represents 52% of original trial, which also included Antigua and St. Lucia) |
Cognitive development (WPPSI-IV), behaviour (SDQ) | Intervention did not improve child outcomes. | Maternal involvement (Parent Involvement in Children’s Education Scale, Parental Involvement in Children’s Literacy Development and Family Involvement Questionnaire); self-efficacy (Brief Parental Self Efficacy Scale); depressive symptoms (CES-D) |
No impacts on maternal involvement or self-efficacy. Results for depressive symptoms not reported in paper | |
| Muhoozi et al,23 Uganda |
One of two23 29 | 12–16 months (primary endpoint) | 467 (91%) | Cognitive, language, motor and socioemotional development (BSID-III, ASQ) | Intervention improved cognitive and motor development. However, no differences were observed for language or personal–social development. | Maternal depressive symptoms (BDI and CES-D) | Intervention reduced maternal depressive symptoms (CES-D, d=−0.70). |
| Two of two26 29 | 3 years | 147 (95%; of 155 randomly selected subsample by design; however subsample revisited represents 29% of original trial) | Cognitive, language, motor and socioemotional development (BSID-III, ASQ and MSEL) | Intervention improved cognitive, language and motor development (eg, BSID-III effect sizes 0.57, 0.56 and 0.50, respectively). However, no difference was observed for personal–social development. | Maternal depressive symptoms (BDI and CES-D) | Intervention reduced maternal depressive symptoms (CES-D, d=−0.51). |
ASQ, Ages and Stages Questionnaire; BDI, Beck Depression Inventory; BSID, Bayley Scales of Infant Development; CBCL, Child Behavior Checklist; CDI, Communicative Development Inventories; CES-D, Center for Epidemiological Studies-Depression; DSM, Diagnostic and Statistical Manual of Mental Disorders; EPDS, Edinburgh Postnatal Depression Scale; FCI, Family Care Indicators; HOME, Home Observation for Measurement of the Environment; KABC, Kaufman Assessment Battery for Children; MSEL, Mullen Scales of Early Learning; OMCI, Observation of Mother-Child Interactions; PCA, principal component analysis; PHQ-9, Patient Health Questionnaire-9; PPVT, Peabody Picture Vocabulary Test; SDQ, Strengths and Difficulties Questionnaire; SRQ, Self-Reporting Questionnaire; WAIS, Weschler Adult Intelligence Scale; WISC-R, Wechsler Intelligence Scale for Children-Revised; WPPSI, Wechsler Preschool and Primary Scale of Intelligence; WRAT, Wide Range Achievement Test.
Measurement
Developmental outcomes and assessment tools varied substantially across studies and depending on child age (table 2). Cognitive development or IQ was the most commonly assessed outcome (assessed at 10 follow-ups), followed by behavioural or socioemotional (assessed at 9 follow-ups). The next most common assessments were language (six follow-ups), school readiness, achievement or academic outcomes (five follow-ups) and motor development (three follow-ups). For the long-term follow-ups of the original trial by Grantham-McGregor et al19 (at ages 18 and 22 years), a range of other outcomes were assessed in addition to youth developmental skills, such as mental health symptoms, other behaviours (eg, parenthood and substance use) and earnings.
Fewer parent-level outcomes were assessed in follow-up studies. Eight of 11 follow-ups assessed at least one parent-level outcome. Parenting practices was evaluated in five follow-ups, as was parental depressive symptoms (although one study did not report results in text). Other parent-level outcomes were assessed once (eg, mother–child interactions and self-efficacy) (table 2).
Intervention results over time
Intervention results are presented here by the timing of evaluation rounds: postintervention and short-term, medium-term and long-term effects. For postintervention results, six of the seven studies assessed immediate impacts on child development, and all found intervention improvements in at least one ECD outcome. Postintervention impacts ranged from relatively small impacts on only certain ECD outcomes in some studies to medium-to-large impacts on all ECD outcomes assessed. For example, Attanasio et al22 found small improvements in only cognition and receptive language but no significant impacts on expressive language, and fine and gross motor scores. On the other hand, Grantham-McGregor et al found large impacts on the global score, as well as all subscales of the Griffiths Mental Development Scales. The intervention by Cooper et al28 did not evaluate an ECD outcome at endline but observed improvements in mother–infant interactions.
Four interventions conducted a short-term follow-up in the first 1–3 years following intervention endline. Of these, three found sustained intervention improvements on at least one ECD outcome. One year after intervention endline (at 18 months of age), Cooper et al found infants in the intervention arm had a higher odds of secure attachment, though no significant differences were found for cognitive development. In Uganda, Atakunda et al26 29 reported that the intervention improved cognitive, language and motor development, but not socioemotional development, at 2 years following intervention endline (age 3 years), and reduced maternal depressive symptoms. In Pakistan, 2 years postintervention endline (age 4 years), Yousafzai et al30 found that children in the responsive stimulation group had sustained higher IQ, executive function, preacademic skills and prosocial behaviours, but no differences in behaviours problems, motor development and preschool enrolment rates, compared with those who did not receive responsive stimulation. Mother–child interactions and parenting practices were also sustained in the responsive stimulation group, but no differences were observed in maternal depressive symptoms. In contrast, the follow-up to the trial by Attanasio et al did not find any sustained effects on ECD (ie, cognitive, language, school readiness, executive function and child behaviour) or maternal outcomes (ie, maternal stimulation and depressive symptoms) at 2 years postintervention (age 5 years).
Three interventions conducted a medium-term follow-up evaluation between 4 and 9 years after intervention completion. In the 4.5-year follow-up to the study by Chang et al25 (age 6 years), Smith et al31 found no effects on the two measured child outcomes (cognitive abilities or socioemotional difficulties) or the two measured parent outcomes (parent involvement and parental self-efficacy). In their 5 year follow-up (age 6.8 years), Walker et al32 found sustained intervention benefits for a few select outcomes: higher scores on child performance IQ and visual spatial memory subscales, and significant reductions in behavioural difficulties. However, there were no treatment differences for the remaining majority of outcomes: full-scale IQ, digit span memory, attention, PPVT or early reading. The original trial by Grantham-McGregor et al had two medium-term follow-up studies 4 and 8 years after intervention completion. In the 4-year follow-up (7–8 years), Grantham-McGregor et al27 found no differences in any child outcome measures when comparing those that were randomised to the stimulation arm compared with the control (10+ outcome measures). After combining all ECD outcomes through a data-driven factor analysis, they found impacts on one of three factors (ie, perceptual–motor factor score). However, in the 8-year follow-up (11–12 years), Walker et al33 found sustained intervention improvements in 4 of the 12 child cognitive outcomes, and Chang et al34 did not find improvements in behavior or school achievement. Neither intervention found any medium-term sustained improvements in maternal stimulation in the home.
Two interventions conducted a long-term follow-up 10 or more years after the end of the intervention. Children from the intervention in South Africa by Cooper et al were followed up 12.5 years after the end of the intervention (age 13 years). Adolescents’ language, behaviour and self-esteem outcomes were assessed, as well as maternal depressive symptoms, but there were no intervention differences in any of these outcomes. Children from the intervention in Jamaica by Grantham-McGregor et al were reassessed 14 and 18 years following the primary endpoint. At the 14-year follow-up (age 17–18 years), adolescents randomised to the stimulation intervention had sustained gains in cognitive and language development, academic skills, as well as less anxiety, fewer depressive symptoms and higher self-esteem. No differences were observed for several other outcomes (eg, social, antisocial and hyperactivity behaviours). At the 18-year follow-up (age 22–23 years), persisting intervention benefits were observed in youth IQ and log monthly earnings, and less depression, violent behaviours and involvement in fights. No differences were seen for various other health behaviour (eg, smoking, alcohol and contraceptive use), education and crime outcomes. Parental outcomes were not assessed at either of the follow-ups at 14 or 18 years.
Illustrative examples and exploratory meta-analyses for impacts on cognitive and behavioural development over time
Cognitive development was the most frequently measured outcome across trials and follow-up rounds. An illustrative comparison of the follow-up effects on cognitive development is presented in figure 2. Eleven follow-up studies across all seven trials evaluated cognitive development outcomes. Two of the four short-term follow-ups demonstrated sustained benefits on cognitive development, whereas the other two studies did not find any significant short-term benefits. Of the four medium-term follow-ups, Grantham-McGregor et al found that the initial intervention effect on cognitive development faded out after 4 years but resulted in a significant difference after 8 years. In the other two follow-ups in Jamaica by Walker et al and Smith et al, there were no benefits observed for either trial after 5 years. Finally, with regard to long-term follow-up results, the trial by Grantham-McGregor et al found sustained improvements on cognitive development after 14 and 18 years, whereas Cooper et al found null effects again after 12.5 years. The second most commonly evaluated outcome across trials and follow-ups was behavioural development in eight studies across all seven trials. With the exception of significant improvements after 5 years in the trial by Walker et al, there were no differences observed in behavioural development in any of the individual follow-up studies (online supplemental figure S2).
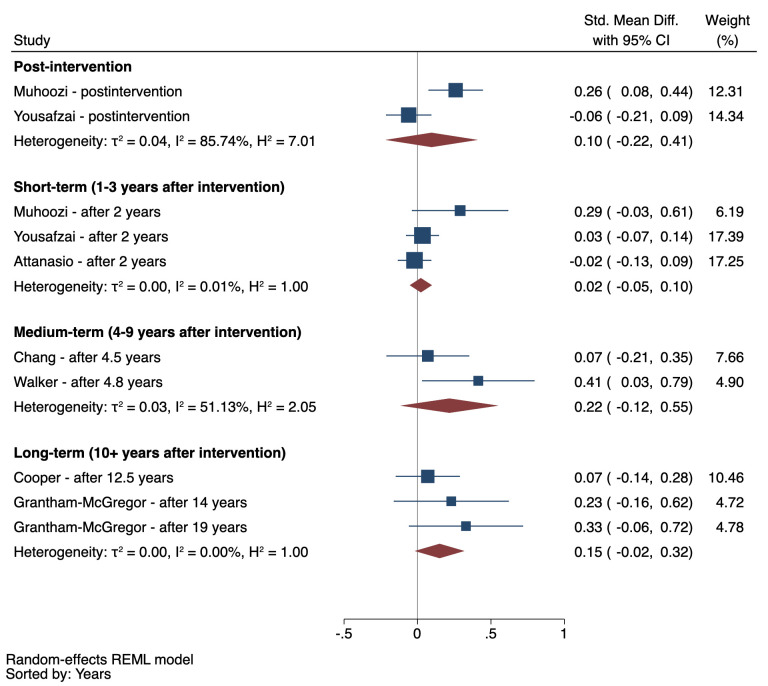
Figure 2.
Parenting intervention effects on cognitive development outcomes for each trial across follow-up studies. Note: markers with black dots represent immediate postintervention trial results. For Cooper et al,28 there was no postintervention assessment of cognitive development.
Exploratory meta-analyses—stratified by follow-up period (ie, postintervention, short-term, medium-term and long-term effects)—are presented for cognitive and behavioural development outcomes in figures 3 and 4, respectively. See online supplemental table S3 for specific outcome measures used from each study. Results indicated a robust positive postintervention effect for cognitive development (SMD=0.46) that generally faded out over time, with the magnitude of the pooled effect reduced by 41% to 52% of the postintervention pooled effect size (figure 3). Although there was a small pooled effect on cognitive development in the short-term (SMD=0.21), the pooled effects were not significant in medium-term or long-term. For child behaviour, results revealed no detectable pooled effects postintervention or in the short-term, medium-term, or long-term. Although the magnitude of the pooled effects appears to increase for medium-term and long-term results, the individual trials that measured child behaviour in longer-term follow-ups did not also measure postintervention effects on behaviour, which precludes assessment of the magnitude of fade-out effects for this outcome over time.
Figure 3.
Short-term, medium-term and long-term pooled effects of parenting interventions on cognitive development outcomes. Note: REML, random-effects meta-analysis.
Figure 4.
Short-term, medium-term and long-term pooled effects of parenting interventions on behavioural outcomes. REML, random-effects meta-analysis.
Discussion
Our systematic review identified seven RCTs of parenting interventions that conducted a follow-up evaluation of the original trial cohort. Follow-ups were mostly short-term, within 1–3 years after programme completion; only two trials had long-term follow-ups (10+ years) that tracked cohorts from early childhood into adolescence or young adulthood.
Although there were consistent intervention benefits on multiple ECD and parent-level outcomes immediately after programme completion, follow-up results revealed a general fading of effects over time across all trials. The sustainability of intervention effects over time appeared to be associated with the magnitude of immediate postintervention effects on ECD outcomes. For example, with cognitive development, immediate impacts ranged from small effect sizes in four of the studies (SMD=0.2–0.3) to medium-to-large effect sizes for the remaining three studies (SMD=0.5–0.9). The three trials with larger immediate postintervention impacts showed significant sustained benefits in the short-term,19 23 24 whereas the other trials with small postintervention impacts did not show sustained benefits at any subsequent follow-up evaluation for any outcomes. Our results suggest there may be a threshold of immediate gains required—perhaps to the magnitude of at least moderate-sized postintervention effects (SMD>0.5)—in order to activate the potential for longer-term sustained benefits on ECD. Additional follow-up studies with larger samples are needed to confirm these trends, especially considering the wide CIs associated with most estimates.
The two interventions that achieved medium-to-large immediate gains in caregiving and parent-level outcomes were those that similarly had larger postintervention effects on ECD and subsequently sustained short-term benefits on ECD. More specifically, Yousafzai et al35 found large initial effects on maternal knowledge of ECD, stimulation and mother–child interactions, and sustained benefits on ECD and parent outcomes in the short-term. The trial by Muhoozi et al found medium-sized initial reductions in maternal depressive symptoms and sustained reductions in depression and improvements in ECD outcomes in the short-term.29 On the other hand, Attanasio et al,22 Cooper et al,28 Chang et al25 and Walker et al36 found small, if any, postintervention effects on maternal outcomes and no follow-up effects on any maternal or ECD outcomes over time. Given that improvements in parenting are generally the primary pathway through which these interventions improve child outcomes,4 if parenting behaviours are not meaningfully improved postintervention, then fadeout effects on ECD outcomes are even more likely. Our results highlight the importance of targeting and sufficiently improving parental behaviours and well-being in order to sustain longer-term programme impacts on ECD outcomes beyond the completion of parenting interventions.
While we identified a potential trend between initial impacts on ECD and parenting outcomes and sustainability of intervention effects of time, there are also a number of other factors that may explain the heterogeneity in follow-up results. First, intervention theories of change and target populations varied across trials. For example, half of the programmes enrolled birth cohorts and included components to enhance maternal sensitivity and responsiveness beginning during the postnatal period,24 28 36 compared with other interventions that focused primarily on increasing cognitive stimulation, distributed play materials to the households every week as part of the programme, and more directly engaged a broader and older age range of children between 9 and 24 months at enrolment.19 22 Variations in programme components and theories of change may reasonably explain why certain interventions did not improve particular ECD outcomes (eg, no impact of postnatal maternal sensitivity intervention on later child cognitive development outcomes37) and the null overall effects observed for behavioural development, which may require alternative interventions that have a stronger focus on social learning theory.38 The majority of interventions concluded prior to child age 2 years, with the exception of Attanasio et al22 that supported children up until age 3 years, and Grantham-McGregor et al19 that also engaged some children older than 3 years of age, depending on their initial age at enrolment. The transition to preschool is a critical developmental period, during which continued support for parents and children may confer additional advantages that may produce sustained effects on later outcomes.39
Second, intervention implementation characteristics also varied substantially in terms of dosage, duration, delivery agents and scale. For example, the original Jamaica Home Visiting programme was the most intensive and involved weekly 1-hour home visits for 24 months, delivered by community health aides, among a small sample in a relatively contained geographical area in the capital city,19 compared with a programme in Colombia that was much larger, integrated at scale into the existing conditional cash transfer programme and delivered by volunteer mothers through weekly home visits for 18 months.22 It has been suggested that more frequent and longer programme durations are associated with greater immediate postintervention effects of early childhood interventions.40 It is likely that sufficient programme exposure, as well as quality implementation, is even more crucial in order to produce longer-term enduring effects. In spite of these trends, it is worth noting that the intervention in Uganda, which had the shortest duration of 6 months, found sustained improvements in ECD outcomes and reductions in maternal depressive symptoms after a 2-year follow-up.26 29 These unique findings may be explained by the fact that this was primarily a research study (ie, outside of existing community service delivery platform) and used bachelor-level session facilitators that were likely substantially better trained and more skilled than lay community members used in other trials.
Third, characteristics of the study population and context varied widely. For example, the trials in Jamaica targeted stunted and low-birthweight children, and the trials in Colombia and Uganda targeted poor households. Prior studies have suggested that disadvantaged children may be more likely to benefit from early interventions.41 Others have suggested that interventions for disadvantaged children may increase likelihood of observing programme effects considering their additional vulnerabilities and already likely delayed developmental trajectories in the absence of any early intervention.42 At the same time, broader population-level socioeconomic deprivations can also undermine the sustainability of programme gains. For example, weak community health services, food insecurity or the lack of access to preprimary school education in low-income contexts can compromise the environments needed to subsequently sustain gains in children’s developmental skills.43
Taken together, our results highlight several gaps and considerations for future research. First, the majority of trials were relatively small efficacy studies, greatly limiting the ability to detect smaller effects in longer-term follow-ups. Moreover, many outcomes assessed in the follow-up rounds were not theoretically justified, and few parent-level outcomes were measured in the follow-up studies. Yet, behavioural changes in caregiving knowledge, skills and practices with their young child are a key theoretical pathway of parenting interventions.27 Our results emphasise the need for developing and applying theories of change to investigations of follow-up effects, which can inform decisions about which outcomes to assess and ensure hypothesised mechanisms are adequately captured.
Few trials have conducted post hoc analyses of potential mediators underlying intervention follow-up effects. Of notable exception, the trial in Pakistan found that sustained improvements in maternal scaffolding skills explained benefits of the intervention on children’s intelligence and executive functioning,44 and sustained improvements in maternal and paternal stimulations explained sustained intervention benefits to children’s cognitive and socioemotional development outcomes.45 Improved measurement of parenting outcomes across follow-ups and longitudinal mediation analyses are needed to understand common mechanisms that drive sustained treatment gains and identify processes that can be harnessed in future parenting interventions to increase the potential for longer-term impacts.
Although the current evidence for intervention effects on child or parent outcomes is limited in the short-term and even moreso inconclusive in the longer term, it is worth mentioning two additionally plausible interpretations of the present findings. Prior studies have suggested ‘sleeper’ effects with regard to potential long-term effects of parenting interventions.18 46 Sleeper effects refer to a phenomenon whereby an intervention produces no immediate postintervention effect (or a small effect) that is latent in the short-term, requires time to fully materialise and then gradually appears at a later follow-up.18 47 48 In addition, there may be potential effects that are not being captured using the current measures or for outcomes that were not assessed. Both of these possibilities support continued rounds of follow-up studies in order to explore whether sleeper or unmeasured effects might be a possible explanation for mixed short-term and seemingly null medium-term impacts. The trajectory of follow-up results from the Grantham-McGregor et al study indicated a large immediate postintervention impact, a null medium-term impact, but then a rebounding and sustained positive long-term effect. Based on these results, it appears possible that treatment impacts may fluctuate in the short-term to medium-term. Therefore, multiple waves of follows-ups are needed in order to determine longer-term patterns and potential trajectories of treatment effects.
There are several limitations of our review that are worth highlighting. First, longitudinal trials are often subject to loss to follow-up. The prevalence of loss to follow-up among the sample revisited by design ranged from 2% to 34%. Although some studies stated no observed differences between those who were reassessed and those who were lost to follow-up, others did not specify and therefore results may be subject to bias. Second, as already mentioned, most included trials were relatively small efficacy studies that did not present power calculations to determine whether the sample size was sufficient to detect follow-up treatment effects, which complicates interpretation of null results. Third, many studies did not report quantitative values for each stated outcome or provide details regarding measurement adaptation, reliability and validity. Fourth, quantitative data synthesis for effects over time on cognitive and behavioural development were exploratory in nature. Given the few trials represented and the heterogeneity in interventions, outcome measures and timing, pooled estimates should be interpreted with caution. Finally, our study only included published articles, which introduces the potential for possibly overestimating long-term effects, considering how initial null or weak findings are less likely to conduct follow-up evaluation and be disseminated by authors (ie, publication bias).
Conclusions
The findings from our systematic review reveal a dearth of follow-up evaluations of parenting interventions in LMICs. Although parenting interventions have shown robust, wide-ranging immediate postintervention benefits on ECD and parenting outcomes, our review suggests that there is currently limited evidence of sustained short-term impacts and inconclusive evidence regarding medium-term or long-term effects based on only two small efficacy trials. Additional follow-up evaluations are needed to provide a fuller picture of the potential medium-term and long-term intervention effects. In conclusion, parenting interventions during early childhood should not be seen as a ‘silver bullet’, especially in the contexts of poverty and other psychosocial stressors. Future parenting intervention should consider other types of multicomponent interventions, such as father-inclusive parenting programmes49 or parental mental health promoting interventions,50 which may have more transformative benefits to the family environment, and potentially in turn sustain programme benefits for child and parent outcomes over time. Ultimately, accessible and high-quality services for children, parents and families and continued support through complementary interventions are critical for ultimately improving population health and development across the life course.
Footnotes
Handling editor: Soumyadeep Bhaumik
Twitter: @joshuadjeong
Contributors: JJ conceived the study, designed the protocol, conducted the database search, reviewed studies for eligibility, conducted the analyses and drafted the manuscript. JJ and HOP extracted the data and created the visualisations. JJ, HOP and GF contributed to the interpretation of data and critical revision of the manuscript and approved the final draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Lu C, Black MM, Richter LM. Risk of poor development in young children in low-income and middle-income countries: an estimation and analysis at the global, regional, and country level. Lancet Glob Health 2016;4:e916–22. 10.1016/S2214-109X(16)30266-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bornstein MH. Positive parenting and positive development in children. : Lerner RM, Jacobs F, Wertlieb D, . Handbook of applied developmental science: promoting positive child, adolescent, and family development through research, policies, and programs. SAGE Publications, 2002: 187–209. [Google Scholar]
- 3.Britto PR, Lye SJ, Proulx K, et al. Nurturing care: promoting early childhood development. Lancet 2017;389:91–102. 10.1016/S0140-6736(16)31390-3 [DOI] [PubMed] [Google Scholar]
- 4.Jeong J, Pitchik HO, Yousafzai AK. Stimulation interventions and parenting in low- and middle-income countries: a meta-analysis. Pediatrics 2018;141:e20173510. 10.1542/peds.2017-3510 [DOI] [PubMed] [Google Scholar]
- 5.Aboud FE, Yousafzai AK. Global health and development in early childhood. Annu Rev Psychol 2015;66:433–57. 10.1146/annurev-psych-010814-015128 [DOI] [PubMed] [Google Scholar]
- 6.Dowdall N, Melendez-Torres GJ, Murray L, et al. Shared Picture Book Reading Interventions for Child Language Development: A Systematic Review and Meta-Analysis. Child Dev 2020;91:e838–99. 10.1111/cdev.13225 [DOI] [PubMed] [Google Scholar]
- 7.Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 2003;129:195–215. 10.1037/0033-2909.129.2.195 [DOI] [PubMed] [Google Scholar]
- 8.Jeong J, Franchett EE, Ramos C, et al. Parenting interventions to promote early child development in the first three years of life: a global systematic review and meta-analysis. revision 2021. [DOI] [PMC free article] [PubMed]
- 9.World Health Organization . Nurturing care for early childhood development: a framework for helping children survive and thrive to transform health and human potential. Geneva: World Health Organization, 2018. [Google Scholar]
- 10.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science 2006;312:1900–2. 10.1126/science.1128898 [DOI] [PubMed] [Google Scholar]
- 11.Nores M, Barnett WS. Benefits of early childhood interventions across the world: (under) investing in the very young. Econ Educ Rev 2010;29:271–82. 10.1016/j.econedurev.2009.09.001 [DOI] [Google Scholar]
- 12.Fergusson DM, Boden JM, Horwood LJ. Nine-year follow-up of a home-visitation program: a randomized trial. Pediatrics 2013;131:297–303. 10.1542/peds.2012-1612 [DOI] [PubMed] [Google Scholar]
- 13.Nordhov SM, Rønning JA, Dahl LB, et al. Early intervention improves cognitive outcomes for preterm infants: randomized controlled trial. Pediatrics 2010;126:e1088–94. 10.1542/peds.2010-0778 [DOI] [PubMed] [Google Scholar]
- 14.Eckenrode J, Campa M, Luckey DW, et al. Long-term effects of prenatal and infancy nurse home visitation on the life course of youths: 19-year follow-up of a randomized trial. Arch Pediatr Adolesc Med 2010;164:9–15. 10.1001/archpediatrics.2009.240 [DOI] [PubMed] [Google Scholar]
- 15.McCormick MC, Brooks-Gunn J, Buka SL, et al. Early intervention in low birth weight premature infants: results at 18 years of age for the infant health and development program. Pediatrics 2006;117:771–80. 10.1542/peds.2005-1316 [DOI] [PubMed] [Google Scholar]
- 16.Campbell FA, Pungello EP, Burchinal M, et al. Adult outcomes as a function of an early childhood educational program: an Abecedarian project follow-up. Dev Psychol 2012;48:1033–43. 10.1037/a0026644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Belfield CR, Nores M, Barnett S. The high/scope Perry preschool program cost–benefit analysis using data from the age-40 followup. Journal of Human Resources 2006;41:162–90. [Google Scholar]
- 18.van Aar J, Leijten P, Orobio de Castro B, et al. Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clin Psychol Rev 2017;51:153–63. 10.1016/j.cpr.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 19.Grantham-McGregor SM, Powell CA, Walker SP, et al. Nutritional supplementation, psychosocial stimulation, and mental development of stunted children: the Jamaican study. Lancet 1991;338:1–5. 10.1016/0140-6736(91)90001-6 [DOI] [PubMed] [Google Scholar]
- 20.Gertler P, Heckman J, Pinto R, et al. Labor market returns to an early childhood stimulation intervention in Jamaica. Science 2014;344:998–1001. 10.1126/science.1251178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker SP, Chang SM, Powell CA, et al. Effects of early childhood psychosocial stimulation and nutritional supplementation on cognition and education in growth-stunted Jamaican children: prospective cohort study. Lancet 2005;366:1804–7. 10.1016/S0140-6736(05)67574-5 [DOI] [PubMed] [Google Scholar]
- 22.Attanasio OP, Fernández C, Fitzsimons EOA, et al. Using the infrastructure of a conditional cash transfer program to deliver a scalable integrated early child development program in Colombia: cluster randomized controlled trial. BMJ 2014;349:g5785. 10.1136/bmj.g5785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muhoozi GKM, Atukunda P, Diep LM, et al. Nutrition, hygiene, and stimulation education to improve growth, cognitive, language, and motor development among infants in Uganda: a cluster-randomized trial. Matern Child Nutr 2018;14:e12527. 10.1111/mcn.12527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yousafzai AK, Rasheed MA, Rizvi A, et al. Effect of integrated responsive stimulation and nutrition interventions in the lady health worker programme in Pakistan on child development, growth, and health outcomes: a cluster-randomised factorial effectiveness trial. Lancet 2014;384:1282–93. 10.1016/S0140-6736(14)60455-4 [DOI] [PubMed] [Google Scholar]
- 25.Chang SM, Grantham-McGregor SM, Powell CA, et al. Integrating a parenting intervention with routine primary health care: a cluster randomized trial. Pediatrics 2015;136:272–80. 10.1542/peds.2015-0119 [DOI] [PubMed] [Google Scholar]
- 26.Atukunda P, Muhoozi GKM, van den Broek TJ, et al. Child development, growth and microbiota: follow-up of a randomized education trial in Uganda. J Glob Health 2019;9:010431. 10.7189/jogh.09.010431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grantham-McGregor SM, Walker SP, Chang SM, et al. Effects of early childhood supplementation with and without stimulation on later development in stunted Jamaican children. Am J Clin Nutr 1997;66:247–53. 10.1093/ajcn/66.2.247 [DOI] [PubMed] [Google Scholar]
- 28.Cooper PJ, Tomlinson M, Swartz L, et al. Improving quality of mother-infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ 2009;338:b974. 10.1136/bmj.b974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atukunda P, Muhoozi GKM, Westerberg AC, et al. Nutrition, hygiene and stimulation education for impoverished mothers in rural Uganda: effect on maternal depression symptoms and their associations to child development outcomes. Nutrients 2019;11:1561. 10.3390/nu11071561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yousafzai AK, Obradović J, Rasheed MA, et al. Effects of responsive stimulation and nutrition interventions on children's development and growth at age 4 years in a disadvantaged population in Pakistan: a longitudinal follow-up of a cluster-randomised factorial effectiveness trial. Lancet Glob Health 2016;4:e548–58. 10.1016/S2214-109X(16)30100-0 [DOI] [PubMed] [Google Scholar]
- 31.Smith JA, Chang SM, Lopez Boo F, et al. Are benefits from a parenting intervention delivered through the health services sustainable? follow-up of a randomized evaluation in Jamaica. Acad Pediatr 2021. 10.1016/j.acap.2021.01.003. [Epub ahead of print: 09 Jan 2021]. [DOI] [PubMed] [Google Scholar]
- 32.Walker SP, Chang SM, Younger N, et al. The effect of psychosocial stimulation on cognition and behaviour at 6 years in a cohort of term, low-birthweight Jamaican children. Dev Med Child Neurol 2010;52:e148–54. 10.1111/j.1469-8749.2010.03637.x [DOI] [PubMed] [Google Scholar]
- 33.Walker SP, Grantham-Mcgregor SM, Powell CA, et al. Effects of growth restriction in early childhood on growth, IQ, and cognition at age 11 to 12 years and the benefits of nutritional supplementation and psychosocial stimulation. J Pediatr 2000;137:36–41. 10.1067/mpd.2000.106227 [DOI] [PubMed] [Google Scholar]
- 34.Chang SM, Walker SP, Grantham-McGregor S, et al. Early childhood stunting and later behaviour and school achievement. J Child Psychol Psychiatry 2002;43:775–83. 10.1111/1469-7610.00088 [DOI] [PubMed] [Google Scholar]
- 35.Yousafzai AK, Rasheed MA, Rizvi A, et al. Parenting skills and emotional availability: an RCT. Pediatrics 2015;135:e1247–57. 10.1542/peds.2014-2335 [DOI] [PubMed] [Google Scholar]
- 36.Walker SP, Chang SM, Powell CA, et al. Psychosocial intervention improves the development of term low-birth-weight infants. J Nutr 2004;134:1417–23. 10.1093/jn/134.6.1417 [DOI] [PubMed] [Google Scholar]
- 37.Murray L, Cooper P, Arteche A, et al. Randomized controlled trial of a home-visiting intervention on infant cognitive development in peri-urban South Africa. Dev Med Child Neurol 2016;58:270–6. 10.1111/dmcn.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barlow J, Bergman H, Kornør H, et al. Group-based parent training programmes for improving emotional and behavioural adjustment in young children. Cochrane Database Syst Rev 2016;8:CD003680. 10.1002/14651858.CD003680.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barnett WS. Effectiveness of early educational intervention. Science 2011;333:975–8. 10.1126/science.1204534 [DOI] [PubMed] [Google Scholar]
- 40.Yousafzai AK, Aboud F. Review of implementation processes for integrated nutrition and psychosocial stimulation interventions. Ann N Y Acad Sci 2014;1308:33–45. 10.1111/nyas.12313 [DOI] [PubMed] [Google Scholar]
- 41.Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet 2011;378:1325–38. 10.1016/S0140-6736(11)60555-2 [DOI] [PubMed] [Google Scholar]
- 42.Bailey D, Duncan GJ, Odgers CL, et al. Persistence and Fadeout in the impacts of child and adolescent interventions. J Res Educ Eff 2017;10:7–39. 10.1080/19345747.2016.1232459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Black MM, Walker SP, Fernald LCH, et al. Early childhood development coming of age: science through the life course. Lancet 2017;389:77–90. 10.1016/S0140-6736(16)31389-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Obradović J, Yousafzai AK, Finch JE, et al. Maternal scaffolding and home stimulation: key mediators of early intervention effects on children's cognitive development. Dev Psychol 2016;52:1409–21. 10.1037/dev0000182 [DOI] [PubMed] [Google Scholar]
- 45.Jeong J, Obradović J, Rasheed M, et al. Maternal and paternal stimulation: Mediators of parenting intervention effects on preschoolers’ development. J Appl Dev Psychol 2019;60:105–18. 10.1016/j.appdev.2018.12.001 [DOI] [Google Scholar]
- 46.Smith JD, Cruden GH, Rojas LM, et al. Parenting interventions in pediatric primary care: a systematic review. Pediatrics 2020;146:e20193548. 10.1542/peds.2019-3548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clarke A, Clarke AM. ?Sleeper effects? in development: Fact or artifact? Developmental Review 1981;1:344–60. 10.1016/0273-2297(81)90030-7 [DOI] [Google Scholar]
- 48.Schweinhart LJ, Montie J, Xiang Z. Lifetime effects: the High/Scope Perry preschool study through age 40. Ypsilanti, MI: High/Scope Press, 2005. [Google Scholar]
- 49.Rempel JK, Rempel LA, Hoa DTP, et al. Parenting teamwork: the impact of a Fathering intervention on mothers and infants in Vietnam. Child Dev 2020;91:e345–64. 10.1111/cdev.13244 [DOI] [PubMed] [Google Scholar]
- 50.Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health 2015;3:e458–69. 10.1016/S2214-109X(15)00099-6 [DOI] [PubMed] [Google Scholar]
- 51.Walker SP, Chang SM, Powell CA, et al. Effects of psychosocial stimulation and dietary supplementation in early childhood on psychosocial functioning in late adolescence: follow-up of randomised controlled trial. BMJ 2006;333:472. 10.1136/bmj.38897.555208.2F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Walker SP, Chang SM, Vera-Hernández M, et al. Early childhood stimulation benefits adult competence and reduces violent behavior. Pediatrics 2011;127:849–57. 10.1542/peds.2010-2231 [DOI] [PubMed] [Google Scholar]
- 53.St Clair MC, Skeen S, Marlow M, et al. Relationships between concurrent language ability and mental health outcomes in a South African sample of 13-year-olds. PLoS One 2019;14:e0221242. 10.1371/journal.pone.0221242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Andrew A, Attanasio O, Fitzsimons E, et al. Impacts 2 years after a scalable early childhood development intervention to increase psychosocial stimulation in the home: a follow-up of a cluster randomised controlled trial in Colombia. PLoS Med 2018;15:e1002556. 10.1371/journal.pmed.1002556 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-004067supp001.pdf (1.2MB, pdf)