Abstract
Background:
Life disruptions caused by the novel coronavirus (COVID-19) pandemic are particularly salient for young adults. Some young adults may engage in unhealthy eating practices to cope with social distancing and isolation during the pandemic, which could increase incidental weight gain.
Purpose:
To examine the association of eating to cope with the pandemic with body weight change pre vs. post-spread of COVID-19 in young adults.
Methods:
Data included baseline (October/2018-October/2019) and follow-up (May/2020-July/2020) assessments from an ongoing longitudinal cohort recruited from Southern California. A diverse sample of participants (54% Hispanic; age=19.72[0.47] years; N=1820) completed online self-report measures of weight at baseline and follow-up and were given a checklist of pandemic coping behaviors including overeating (yes/no) and eating high fat or sugary foods (yes/no) to cope with social distancing and isolation during the pandemic.
Results:
With and without adjusting for confounders, young adults who did vs. did not report overeating to cope with the pandemic gained more weight from baseline to follow-up (5.55 vs. 2.54 lbs). Unhealthy food intake to cope with the pandemic was not associated with weight change. Baseline weight moderated the association of eating coping practices with weight change such that individuals with higher baseline weight gained more weight if they engaged in eating to cope behaviors vs. not (ps≤.001).
Conclusions:
Unhealthy eating behavior to cope with the pandemic and corresponding body weight increases may be occurring in young adults. Interventions to promote healthy eating practices in young adults warrant consideration for weight gain prevention during the pandemic.
Keywords: COVID-19, pandemic, obesity, weight change, overeating, eating behavior
The novel coronavirus (COVID-19) pandemic has had a profound impact on American lives [1,2]. The COVID-19 pandemic has involved travel restrictions, self-quarantine, and stay-at-home orders to stop or limit the spread of the virus. In order to accomplish this, many local and state governments closed non-essential businesses including: dine-in services at restaurants and bars, gyms, salons, and other recreational indoor activities; required residents to stay at home except for essential activities and outdoor recreation; and required residents to practice social distancing from all persons not residing in one’s residence. These measures have led to critical changes in Americans’ finances, education, employment, and lifestyle [3,4], resulting in high levels of stress, anxiety, and depression [2].
Young adults may be particularly susceptible to adverse mental health concerns related to the pandemic. Many young adults do not have established careers and may be particularly likely to suffer loss of employment or work [5]. Further, college students are facing educational disruptions caused by transition to remote learning modalities or concerns about exposure to the virus for universities that continue on-campus classes [6]. Additionally, young adulthood is already a development period marked by increased desire for social affiliation [7] and risk of mental health problems [8], both of which may amplify the adverse effects of pandemic-related social isolation and loneliness. All of these factors are known to act as stressors and increase negative affective states, reduce positive affective states, and lead to mental health problems [9–11].
One maladaptive way to cope with stress and negative emotions is unhealthy eating patterns, such as eating more than one usually would or eating unhealthy calorie-rich, nutrient poor foods [12,13]. In general, emotional eating is prominent among young adults [14] and predicts weight gain [15]. Perceived stress, depressive symptoms, financial strain, and loneliness—all factors that might be exacerbated during the COVID-19 pandemic—are related to higher emotional eating and overeating [16–19]. Recent research reported that many adults report increased binge eating, overeating, using food to cope, and unhealthy food intake during the COVID-19 pandemic [20–22]. This is concerning given that increased overeating and unhealthy food intake during the COVID-19 pandemic could lead to incidental weight gain, which could increase risk of long-term weight retention and morbidity [23,24]. Whether many young adults are engaging in unhealthy eating to cope with the pandemic and whether this coping practice has increased incidental weight gain is unknown. If this is the case, the obesity and chronic disease epidemic in the United States could be perpetuated and exacerbated if public health measures are not initiated to address this unhealthy coping practice during the COVID-19 pandemic.
The current longitudinal observational study examined the prevalence of engaging in overeating and unhealthy food intake to cope with the pandemic and its association with pre vs. post pandemic body weight in young adults. It was hypothesized that engaging in overeating and unhealthy eating to cope with pandemic would be associated with weight gain, and effects would remain after adjusting for relevant covariates. Given evidence that emotional and other unhealthy eating practices differ by gender, ethnicity, age, weight, and depressive symptoms [16–19], exploratory analyses examined these factors as correlates of eating to cope with pandemic and moderators of their association with weight increases.
Method
Participants and Procedure
Participants were enrolled in the Happiness and Health prospective cohort study, which began in 2013 when participants were in ninth grade (Mage=14.1 years; N=3396) [25]. Recruitment occurred in 10 Los Angeles area high schools selected based on sociodemographic and regional diversity.
Participants completed eight waves of in-person data collection while in high school. Those consenting as adults to continue participating in the cohort (N=2548), were invited to be surveyed online post-high school at Wave 9 (collected October 2018-October 2019; baseline for the current study) and Wave 10 (May-July 2020; follow-up) data. There were 1959 consenting participants (62% women; Mage at baseline=19.28 years; SD=0.47) who completed baseline and follow-up. The study protocol was reviewed and approved by the University of Southern California Institutional Review Board.
Measures
Weight and body mass index (BMI).
Participants self-reported their weight (write in numerical value response in pounds) and height (in feet and inches) at baseline and follow-up. Height was assessed at baseline and follow-up, and responses were strongly correlated (r=.95). BMI was calculated using the standard BMI formula [26].
Eating to cope with the pandemic.
In a module of the survey labeled “Behavioral actions specific to the COVID-19 Pandemic”, participants were asked, “To cope with social distancing and isolation, are you doing any of the following? Select all that apply.” Two options included unhealthy food intake (i.e., “eating high fat or sugary foods”) and overeating (i.e., “eating more food than usual”). Respondents checked a box if they engaged in each behavior. This single item assessment approach is consistent with other large epidemiological studies [27, 28].
Covariates.
Participants also reported gender (male/female), age (in years, continuous), and Hispanic ethnicity (yes/no), and race (White/non-White). At baseline, participants completed the 10-item Center for Epidemiological Studies Depression Scale-Short Form [29]. Days between assessments was calculated to control for differences in the length of time between assessment points.
Statistical Analyses
Descriptive statistics were examined as well as variability in weight change. Chi-squared and t-tests were used to investigate differences in COVID-19 related eating to cope behaviors by gender, ethnicity, age, baseline weight, and depressive symptoms. For each eating to cope with the pandemic measure (i.e., overeating and unhealthy food intake), separate 2 × 2 between-by-within ANOVAs were tested using self-reported weight as the dependent variable. These included the independent variables of the respective eating coping behavior (yes vs. no) as a between-subjects variable and timepoint (baseline vs. follow-up) as a within-subject variable, with the interaction term indicating differences in changes in weight from baseline to follow-up as a function of the respective eating coping variable.
Next, multivariable linear regression models were calculated using weight change scores as the outcome and a coping eating variable as predictor; models were adjusted for gender, ethnicity, race, age, baseline weight, baseline depressive symptoms, and days between assessments. Finally, exploratory two-way multiplicative interactions were evaluated by including a product interaction term of gender, ethnicity, race, age, baseline weight, depressive symptoms, and days between assessments with each eating to cope variable in models evaluating the association eating coping behaviors with changes in weight. Multiple imputation was used to account for missing data on covariates. Analyses were conducted in SPSS version 25.0 (IBM Corp., Armonk, NY). For adjusted and significant interaction models, supplementary analyses were run using BMI instead of weight and using logistic models with weight gain versus weight loss/weight maintenance as the outcome.
Results
Descriptive Results
Of the 1959 participants who completed both waves, 139 participants were missing weight at baseline or follow-up, leaving 1820 participants for the analytic sample. The median date of completion was December 11, 2018 (Range: October 24, 2018-October 31, 2019; Interquartile range: 72 days) for the baseline survey and June 19, 2020 (Range: May 18, 2020-July 21, 2020; Interquartile range: 20 days) for the follow-up survey. The sample was diverse regarding ethnicity (54% Hispanic) and race (33% White, 25% Asian, 7% Black, 4% Native American, 5% Pacific Islander, 32% multiple races, 19% other). At baseline, the majority of participants met criteria for normal weight (55%) followed by overweight (23%), obesity (16%), and underweight (6%). Illustrated in Table 1, the sample was early emerging adults with low levels of depressive symptoms.
Table 1.
Descriptive Statistics of Participant Characteristics, by Eating to Cope with the Pandemic
| |
Stratified by Overeating to Cope with the Pandemic |
Stratified by Unhealthy Food Intake to Cope with the Pandemic |
|||||
|---|---|---|---|---|---|---|---|
| Pooled Sample (N=1820) | No (n=1257) | Yes (n=563) | p-Value for Test of Group Differences | No (n=1183) | Yes (n=637) | p-Value for Test of Group Differences | |
| Female gender, N (%) | 1119 (61%) | 728 (58%) | 391 (69%) | <.001 | 686 (58%) | 433 (68%) | <.001 |
| Age, mean (SD), years | 19.72(0.46) | 19.73(0.47) | 19.68(0.44) | .07 | 19.73(0.47) | 19.68(0.43) | .03 |
| Ethnicity, Hispanic, N (%) | 981 (54%) | 671 (53%) | 309 (55%) | .54 | 645 (55%) | 336 (53%) | .44 |
| Race, White, N (%) | 1223 (67%) | ||||||
| Baseline weight, mean (SD), lbs |
155.00(41.44) | 154.14(39.59) | 156.91(45.28) | 21 | 154.73(40.64) | 155.48(42.92) | .71 |
| Baseline depression, mean (SD) | 9.63(6.34) | 9.07(6.25) | 10.88(6.35) | <.001 | 9.00(6.26) | 10.81(6.31) | <.001 |
Note. P-value for omnibus group differences from χ2 (categorical variable) or t (continuous variable) test; Depressive symptoms measured by Center for Epidemiologic Depression Scale – 10 item measure of past week symptoms from 0 (never) – 3 (yxx) sum (range; 0– 30).
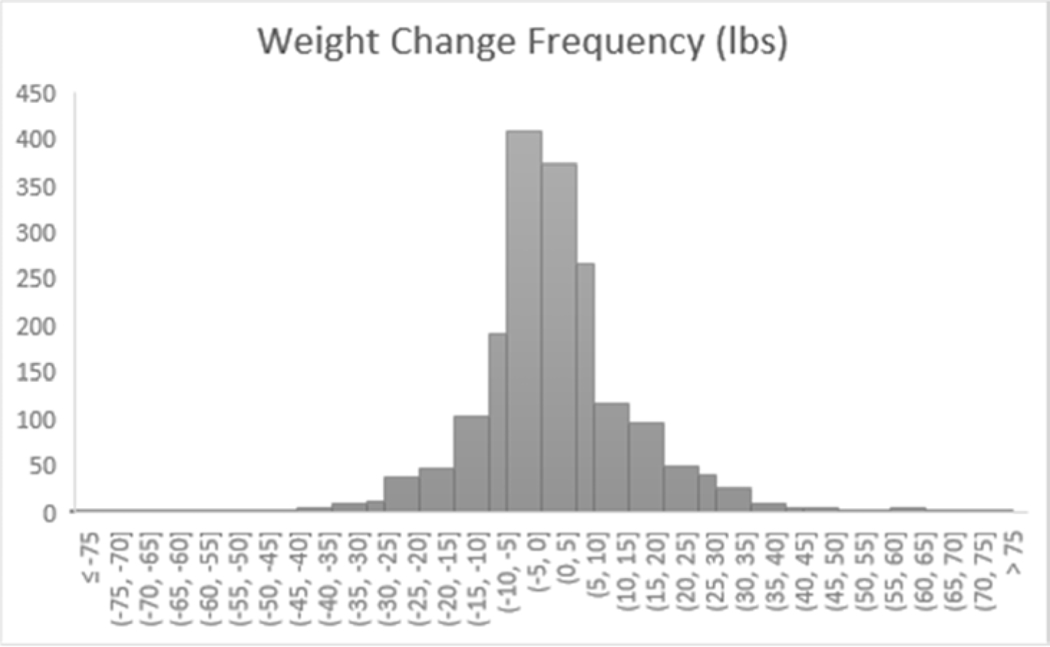
Figure 1 shows the variability in weight change in the overall sample (Mweight change=3.47 lbs [SD=14.57]; M%weightchange=2.5% [8.6%]). Most participants maintained or gained/lost a few pounds with a minority gaining or losing a more significant amount of weight. Thirty-one percent (n=563) of participants reported overeating to cope with the pandemic and 35% (n=637) reported eating unhealthy foods to cope with pandemic. In examining co-occurrence of these eating behaviors, 18% of participants reported both overeating and eating unhealthy foods to cope with the pandemic, 13% reported only overeating only, 17% reported unhealthy eating only, and 52% reported neither.
Figure 1.
Distribution of weight change from baseline to follow-up in the overall across the sample
Association of Participant Characteristics with Eating to Cope with Pandemic
Table 1 displays the sample descriptive statistics stratified by pandemic-related eating behaviors. Female sex, higher baseline depressive symptoms, and younger at age at [baseline or follow-up] were positively associated overeating and unhealthy food coping eating. There were no differences in eating-related coping behaviors by ethnicity or baseline weight.
Body Weight as a Function of Time Point and Eating to Cope with the Pandemic
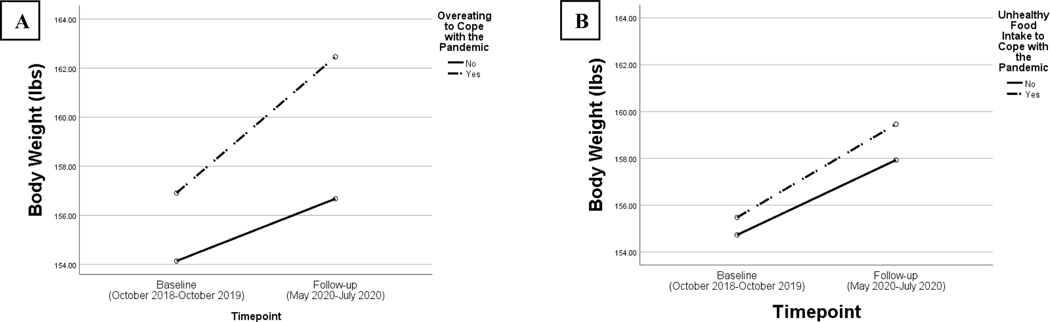
Overeating to cope with the pandemic.
A two-way between-by-within mixed ANOVA found a main effect of time point, F(1, 1818)=120.88, p<.001, eta-square=.06, indicating an increase in weight in the overall sample. There was a main effect of overeating to cope with the pandemic, F(1, 1818)=4.12, p=.04, eta-square=.002, indicating that averaged across both time points, participants who reported overeating to cope with the pandemic tended to have higher weight. There was a significant interaction of overeating to cope with the pandemic x timepoint, F(1, 1818)=16.80, p<.001, eta-square=.01. Figure 2a shows the interaction between overeating and timepoint. Weight gain from baseline to follow-up was higher in those who reported overeating (Mdifference=5.55 lbs) compared to those who did not (Mdifference=2.54 lbs), with a difference in difference of 3.01 lbs. Follow-up, one-way within-subject ANOVAs stratified by overeating to cope with the pandemic found that time point was significant in both groups, indicating weight gain occurred in both groups. However, the effect size was larger in the group that did vs. did not report overeating to cope with the pandemic (partial eta squared=.12 versus .02, respectively).
Figure 2.
(A) Interaction of overeating to cope with the pandemic and timepoint on body weight. (B) Non-significant interaction of unhealthy food intake to cope with the pandemic and timepoint on body weight.
Unhealthy food intake to cope with the pandemic.
The parallel two-way between-by-within mixed ANOVA using the unhealthy food intake to cope measure replicated the main effect of time point, F(1, 1818)=100.36 p<.001, eta-square=.05. However, there was no main effect of unhealthy eating to cope, F(1, 1818)=0.31, p=.58, eta-square<.001, nor any interaction of COVID-19 related unhealthy eating x timepoint, F(1, 1818)=1.19, p=.28, eta-square=.001. Figure 2b shows the non-significant interaction between unhealthy eating and timepoint.
Multivariable Linear Regressions of Pandemic Related Eating Behaviors and Weight Change
Adjusted models.
Table 2 shows results of multivariable linear regressions predicting weight change (i.e., follow-up – baseline weight difference value). After controlling for depressive symptoms, gender, age, ethnicity, race, baseline weight, and days between assessments, overeating to cope with the pandemic was associated with greater increases in weight, with a difference-in-difference in follow-up vs. baseline weight gain between those who do vs. do not engage in overeating coping of 3.27 lbs (p<.001). Unhealthy food intake to cope with the pandemic was unrelated to weight change paralleling the unadjusted ANOVA result. Hispanic ethnicity was the only covariate associated with weight change such that Hispanic young adults gained more weight. Results were similar when using BMI change or weight gain versus weight loss/maintenance as the outcome (see Supplementary Tables 1 and 2, respectively).
Table 2.
Parameter Estimates from Multivariable Linear Regression Models Predicting Weight Change
| Parameter | Unstandardized B | SE | p |
|---|---|---|---|
|
Model 1 | |||
| Age | −0.15 | 0.85 | .86 |
| Gender | −1.32 | 0.76 | .08 |
| Hispanic versus non-Hispanic ethnicity | 2.56 | 0.69 | <.001 |
| White versus non-White race | 0.53 | 0.73 | .47 |
| Baseline weight | −0.03 | 0.01 | .001 |
| Days between assessments | 0.01 | .01 | .05 |
| Depressive symptoms | −0.10 | 0.06 | .07 |
| Overeating to cope with the pandemic | 3.27 | 0.75 | <.001 |
| Model 2 | |||
| Age | −0.15 | 0.85 | .86 |
| Gender | −1.04 | 0.76 | .17 |
| Hispanic versus non-Hispanic ethnicity | 2.61 | 0.70 | <.001 |
| White versus non-White race | 0.49 | 0.73 | .50 |
| Baseline weight | −0.03 | 0.01 | .003 |
| Days between assessments | 0.01 | 0.01 | .03 |
| Depressive symptoms | −0.08 | 0.06 | .14 |
| Unhealthy food intake to cope with the pandemic | 1.00 | 0.72 | .17 |
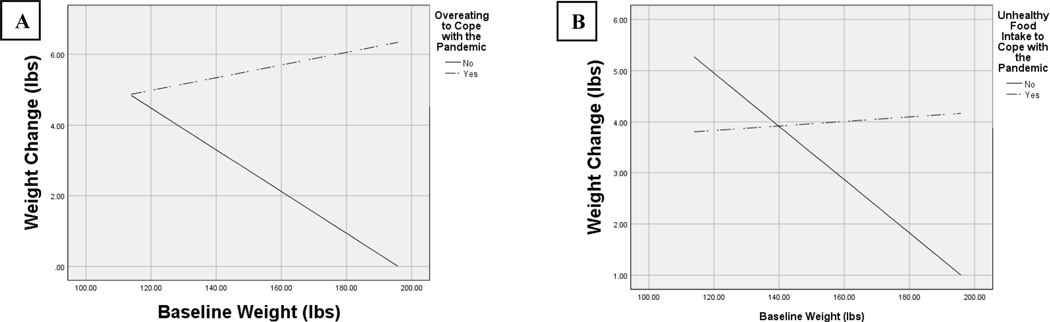
Moderator analysis.
A significant interaction was found for the interaction of overeating to cope with the pandemic with baseline weight (p<.001; see Figure 3a) in the prediction of weight increase from baseline to follow-up. Additionally, a significant interaction was found for COVID-19 related unhealthy food intake and baseline weight in the predication of weight change (p=.001; see Figure 3b). Among individuals with higher baseline weight, engaging in overeating or eating unhealthy foods to cope with pandemic were associated with more weight gain compared to not engaging in behaviors. There were no differences in weight gain as a function of eating to cope with the pandemic among those with lower weights. Interactions were similar when using baseline BMI instead of weight. All other interactions with covariates explored were non-significant. Results were similar when using BMI change as the outcome (see Supplementary Table 3), but interactions were not significant with weight gain versus weight loss/maintenance as the outcome (see Supplementary Tables 4).
Figure 3.
(A) Interaction of overeating to cope with the pandemic and baseline weight predicting weight change (defined as weight at follow-up minus baseline weight). (B) Interaction of unhealthy food intake to cope with the pandemic and baseline weight predicting weight change (defined as weight at follow-up minus baseline weight).
Discussion
This study provides new evidence that there was an appreciable prevalence of eating-related unhealthy behaviors to cope with social distancing and isolation during the pandemic (48% reported one or more behavior) in this young adult sample. We also found that overeating to cope with the pandemic was associated with greater weight gain in young adults. Given that these practices might adversely impact metabolic health and previous evidence that there is a bi-directional effect between eating-related coping and adverse mental health in young people [30], these data highlight potential public health concerns that warrant attention.
Women and individuals experiencing more depressive symptoms were more likely to engage in COVID-19 related overeating and unhealthy eating in this study. These results are consistent with previous evidence collected prior to the pandemic that female gender and depression are associated with dysregulated eating behaviors (e.g., overeating, emotional eating) [16–19]. This study provides new data extending these findings to maladaptive eating-related coping behaviors in the context of the COVID-19 pandemic. It is possible that the pandemic worsened depressive symptoms or negatively impacted other coping behaviors (e.g., physical activity, social interaction), and thus unhealthy eating behaviors were used to compensate.
Young adults in this study that reported overeating to cope with the conditions of the pandemic gained more weight in the time period before vs. after the onset of the pandemic compared to those that did not. It is possible that this result does not reflect causal mechanisms. Perhaps individuals who are inclined to gain weight and engage in overeating to cope in any stressful situation are those who reported overeating to cope with the pandemic in this study. However, we controlled for factors that are risk factors for maladaptive eating coping behaviors and young adult weight gain, such as gender and depressive symptoms [16–19], and the difference in weight gain between the two groups remained.
While confounding cannot be ruled out, the public health importance of the association identified here warrants consideration. The mean change in weight of 5.55 pounds among those reporting overeating to cope with the pandemic was observed in this sample assessed on average about 13 weeks into the pandemic. We cannot determine how much of the weight change occurred in the time period preceding the interval between the baseline assessment (Median baseline survey date: Dec 2018) and prior to the worldwide spread of COVID-19 in March 2020. However, findings remained after controlling for days between assessments. If the prevalence of overeating coping behaviors and the rate of weight gain per month observed were to remain consistent as the pandemic continues, the cumulative population health impact in the young adult age group could be problematic, particularly among women as they were more likely to report more overeating to cope with the pandemic. Another concern is that incidental weight gain during the COVID-19 pandemic and any new unhealthy eating behaviors adopted to cope with the pandemic may be retained indefinitely.
Moderation analyses showed that COVID-19 related overeating and unhealthy eating had a greater effect on body weight change among young adults who weighed more before the pandemic. This is consistent with research suggesting that adults with overweight and obesity are more at risk for further weight gain [31,32]. Therefore, the pandemic may increase the probability of young adults shifting from overweight to obesity or from obesity to severe obesity rather than from normal weight to overweight, which may compound with already-established risk for weight gain in young adults with overweight and obesity [31,32]. Evidence suggests that severe obesity is most strongly associated with health risk [33]. Results like the current study raise concern whether the pandemic may be pushing more young adults with overweight or obesity towards high-risk ranges in the continuum of bodyweight.
There was also a main effect of Hispanic ethnicity on weight gain. However, results showed that eating to cope with the pandemic did not differ by ethnicity nor was there an interaction between ethnicity and eating to cope with the pandemic. It is possible that Hispanic individuals may have experienced greater severity of eating to cope—either more occurrences or mood food consumed during eating episodes. Research suggests that the pandemic has had a disproportionate impact on Hispanics in the United States [34], which could be associated with other health-compromising behaviors—including changes in physical activity, sleep, and diet quality and availability.
Strengths of this study include adequate size and sociodemographic diversity of the sample and the longitudinal design containing data before and after COVID-19. Yet, there are several limitations. First, weight and height were collected using self-report, which is subject to reporting biases and errors. If weight was underestimated, effects may be much larger than what was found. Next, eating behaviors were assessed with single item measures, and as a result, amount of food consumed and frequency of behaviors cannot be discerned. More fine-grained data on eating behaviors and diet quality may reveal different relationships with weight change over COVID-19. Further, the eating behavior questions were anchored to social distancing and isolation aspects of the pandemic, yet other aspects of the pandemic may have been associated with change in eating behavior.
Also, while demographics and depressive symptoms were controlled for, there are other possible confounders that should be mentioned. It is possible that individuals who engaged in use of food to cope with the COVID-19 pandemic would have engaged in food coping behavior regardless of the pandemic or experienced other changes that caused weight gain. Even if young adults who reported using food to cope with the pandemic would have engaged in coping-related overeating or unhealthy eating regardless of the pandemic, it is probable that food-related coping during the pandemic would be uniquely detrimental to weight, given changes in other energy-balance behaviors that have been observed [35–37]. Finally, whether these results generalize nationally and to other age periods is unknown.
In conclusion, these data found that an appreciable proportion of young adults from Southern California reported using food to cope with the COVID-19 pandemic. Use of this coping strategy was associated with greater increases in body weight pre vs. post pandemic, and this is strongest among individuals with higher baseline body weight. Dissemination of eating regulation and healthy coping strategies is of critical importance during COVID-19 to prevent weight gain and unhealthy eating patterns. In the current context, telehealth, mobile health (e.g., smartphone apps), and ecological momentary interventions as well as mass media messaging that unhealthy eating strategies may be of relevance to buffer any adverse impact of the pandemic on obesity [38]. Further, weight maintenance strategies, such as daily self-weighing and self-monitoring, may be useful for weight gain prevention during COVID-19 [39–40].
Supplementary Material
Implications and Contribution:
Unhealthy eating behaviors to cope with the pandemic are prominent among young adults and negatively impact weight. Failure to mitigate unhealthy eating to cope during the pandemic may have a detrimental impact on young adult’s long-term weight trajectory.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute under Award Number R01CA229617 (Barrington-Trimis/Leventhal), National Institute on Drug Abuse Award Number K24DA048160, and National Institute of Diabetes and Digestive and Kidney Diseases Award Number K01DK124435 (Mason). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors have no conflicts of interest to disclose. TBM wrote the first draft of the paper, and no payments were received for writing this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Carter P, Anderson M, Mossialos E. Health system, public health, and economic implications of managing COVID-19 from a cardiovascular perspective. Eur Heart J. 2020. 10.1093/eurheartj/ehaa342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020; 0020764020915212. 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- 3.Goodell JW. COVID-19 and finance: Agendas for future research. Financ Res Lett. 2020; 101512. 10.1016/j.frl.2020.101512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mogaji E. Financial Vulnerability During a Pandemic: Insights for Coronavirus Disease (COVID-19). Research Agenda Working Papers. 2020; 57–63. 10.2139/ssrn.3564702 [DOI] [Google Scholar]
- 5.Pew Research. Majority of Americans who lost a job or wages due to COVID-19 concerned states will reopen too quickly, 2020. Retrieved from: https://www.pewresearch.org/fact-tank/2020/05/15/majority-of-americans-who-lost-a-job-or-wages-due-to-covid-19-concerned-states-will-reopen-too-quickly/ft_2020-05-15_jobloss_02/
- 6.Sahu P. Closure of universities due to Coronavirus Disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020; 12. doi: 10.7759/cureus.7541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fraley R, Davis KE. Attachment formation and transfer in young adults’ close friendships and romantic relationships. Pers Relationship. 1997; 4:131–144. 10.1111/j.1475-6811.1997.tb00135.x [DOI] [Google Scholar]
- 8.Twenge JM, Cooper AB, Joiner TE, et al. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019; 128:185–199. 10.1037/abn00004109. [DOI] [PubMed] [Google Scholar]
- 9.Goossens L Emotion, affect, and loneliness in adolescence. In Jackson S & Goossens L. (Eds.), Handbook of adolescent development (p. 51–70). Psychology Press, 2006. [Google Scholar]
- 10.Lee SA, Mathis AA, Jobe MC, Pappalardo EA. Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale. Psychiatry Res. 2020; 113112. 10.1016/j.psychres.2020.113112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rohde N, Tang KK, Osberg L, Rao P. The effect of economic insecurity on mental health: Recent evidence from Australian panel data. Soc Sci Med. 2016; 151:250–258. 10.1016/j.socscimed.2015.12.014 [DOI] [PubMed] [Google Scholar]
- 12.Boggiano MM, Wenger LE, Turan B, et al. Eating tasty food to cope. Longitudinal association with BMI. Appetite. 2015; 87:365–370. 10.1016/j.appet.2015.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011; 137:660–681. 10.1037/a0023660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychological Association. Stress in America™ Are teens adopting adults’ stress habits?, 2014. Retrieved from https://www.apa.org/news/press/releases/stress/2013/stress-report.pdf
- 15.Frayn M, Knäuper B. Emotional eating and weight in adults: a review. Curr Psychol. 2018; 37:924–933. 10.1007/s12144-017-9577-9 [DOI] [Google Scholar]
- 16.Mason TB. Loneliness, eating, and body mass index in parent–adolescent dyads from the Family Life, Activity, Sun, Health, and Eating study. Pers Relationship. 2020; 27:420–432. 10.1111/pere.12321 [DOI] [Google Scholar]
- 17.Mason TB, Heron KE, Braitman AL, Lewis R J. A daily diary study of perceived social isolation, dietary restraint, and negative affect in binge eating. Appetite. 2016; 97:94–100. 10.1016/j.appet.2015.11.027 [DOI] [PubMed] [Google Scholar]
- 18.Mason TB, Lewis RJ. Profiles of binge eating: the interaction of depressive symptoms, eating styles, and body mass index. Eat Disord. 2014; 22:450–460. 10.1080/10640266.2014.931766 [DOI] [PubMed] [Google Scholar]
- 19.Spinosa J, Christiansen P, Dickson JM, et al. From socioeconomic disadvantage to obesity: The mediating role of psychological distress and emotional eating. Obesity. 2019; 27:559–564. 10.1002/oby.22402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020; 12:1583. 10.3390/nu12061583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. Int J Eat Disord. 2020. 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang SD, Devjani S, Dunton GF, Mason TB. Effects of COVID-19 pandemic stress on dysregulated eating and feeding behaviors and body mass index in Los Angeles mothers. Manuscript submitted for publication. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper JA, Tokar T. A prospective study on vacation weight gain in adults. Physiol Behav. 2016; 156:43–47. 10.1016/j.physbeh.2015.12.028 [DOI] [PubMed] [Google Scholar]
- 24.Xu X, Mishra GD, Dobson AJ, Jones M. Short-term weight gain is associated with accumulation of multimorbidity in mid-aged women: a 20-year cohort study. Int J Obes. 2019; 43:1811–1821. 10.1038/s41366-018-0250-7 [DOI] [PubMed] [Google Scholar]
- 25.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence JAMA. 2015; 314:700–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garrow JS, Webster J. Quetelet’s index (W/H2) as a measure of fatness. Int J Obes. 1985;9:147–153. [PubMed] [Google Scholar]
- 27.Austin SB, Ziyadeh NJ, Corliss HL, et al. Sexual orientation disparities in purging and binge eating from early to late adolescence. J Adolesc Health. 2009;45:238–245. 10.1016/j.jadohealth.2009.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mason TB, Heron KE. Do depressive symptoms explain associations between binge eating symptoms and later psychosocial adjustment in young adulthood? Eat Behav. 2016;23:126–130. 10.1016/j.eatbeh.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 29.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994; 10:77–84. [PubMed] [Google Scholar]
- 30.Polivy J, Herman CP. Mental health and eating behaviours: a bi-directional relation. Can J Public Health. 2005; S43–S46. [PubMed] [Google Scholar]
- 31.Malhotra R, Østbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obesity. 2013;21:1923–1934. 10.1002/oby.20318 [DOI] [PubMed] [Google Scholar]
- 32.Williamson DF, Kahn HS, Remington PL, Anda RF. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med.1990;150:665–672. [PubMed] [Google Scholar]
- 33.Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res 2004; 12:1936–1943. 10.1038/oby.2004.243 [DOI] [PubMed] [Google Scholar]
- 34.Macias Gil R, Marcelin JR, Zuniga-Blanco B, et al. COVID-19 pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. J Infect Dis. 2020;222:1592–1595. doi: 10.1093/infdis/jiaa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tison GH, Avram R, Kuhar P, et al. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med. 2020. 10.7326/M20-2665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marelli S, Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2020;1–8. 10.1007/s00415-020-10056-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Górnicka M, Drywień ME, Zielinska MA, Hamułka J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: A Cross-sectional online survey PLifeCOVID-19 study. Nutrients. 2020;12:2324. 10.3390/nu12082324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010; 15:1–39. 10.1348/135910709X466063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laitner MH, Minski SA, Perri MG. The role of self-monitoring in the maintenance of weight loss success. Eat Behav. 2016; 21:193–197. 10.1016/j.eatbeh.2016.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005; 30:210–216. 10.1207/s15324796abm3003_5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.