Abstract
Background:
This systematic review investigated the clinical effects of inhalation aromatherapy for the treatment of sleep problems such as insomnia.
Methods:
Studies on sleep problems and inhalation aromatherapy, published in Korean and international journals, were included in the meta-analysis. Five domestic and international databases, respectively each, were used for the literature search. Keywords included sleep disorder, sleep problems, insomnia, and aroma inhalation, and the related literature was further searched. After the screening, selected articles were assessed for their quality and conducted the risk of bias using RevMan 5.0, a systematic literature review was then conducted. A meta-analysis comparing the averages was conducted on studies that reported numerical values. Additionally, meta-analysis of variance and meta-regression analyses were performed.
Results:
Meta-analysis of the 34 studies using the random-effects model revealed that the use of aromatherapy was highly effective in improving sleep problems such as insomnia, including quantitative and qualitative sleep effects (95% confidence interval [CI], effect sizes = 0.6491). Subgroup analysis revealed that the secondary outcomes including stress, depression, anxiety, and fatigue were significantly effective. The single aroma inhalation method was more effective than the mixed aroma inhalation method. Among the single inhalation methods, the lavender inhalation effect was the greatest.
Conclusion:
Inhalation aromatherapy is effective in improving sleep problems such as insomnia. Therefore, it is essential to develop specific guidelines for the efficient inhalation of aromatherapy.
Ethics and dissemination:
Ethical approval is not required because individual patient data are not included. The findings of this systematic review were disseminated through peer-reviewed publications or conference presentations.
PROSPERO registration number:
CRD42020142120.
Keywords: aromatherapy, inhalation, insomnia, meta-analysis, sleep problems, systematic literature review
1. Introduction
During sleep, humans undergo physical and mental stress recovery and rejuvenation.[1–3] Sleep deprivation is common among the current generation and up to 18% of the world's population experiences insomnia.[4,5] In Korea, >2 million people were diagnosed with insomnia over a period of 5 years (2013–2017), according to the National Health Insurance Corporation. A meta-analysis on sleep-related studies assessed the factors related to sleep disorders and found that stress, a psychological result, exhibited the highest correlation with sleep disorders.[5,6] However, stress coexists with other diseases in the current generation, and therefore it is challenging to treat sleep disorders by only addressing the stress. Additionally, prescriptions for sleep problems include sleep inducers and sleeping pills, which may lead to other problems in daily life.[7] For example, a sleep disorder patient led to a traffic accident a day after ingesting sleeping pills, which stay in the body longer than other drugs.[8] Recently, interest in programs using psychological interventions and complementary alternative medicine has increased to reduce the side effects of prescription drugs and improve the quality of life of insomnia patients.[9] However, there are limitations in these program applications to those with sleep disorders. Most programs last 50 minutes per session and are performed at least once a week. As sleep disorder programs are conducted for a longer period rather than a single session,[5] adults that work during the day or at night[10–12] have difficulties in participating in such programs. Additionally, those with sleep disorders experience depression, anxiety, and panic disorder, which also leads to difficulties in program participation.[13–16]
Aroma inhalation therapy for treating sleep disorders has recently been gaining great interest. Inhalation of aromatic oil particles that stimulate the olfactory sense, directly affect the central nervous system responsible for controlling human emotions and physiological functions. It regulates the autonomic nervous system, endocrine system, and immune system, leading to therapeutic effects on the body.[17] Another advantage of aromatherapy is that individuals can choose their preferred scents, and those that cannot participate in sleep disorder programs can also undergo aromatherapy regardless of the time and place. In Korea, recent studies on aroma inhalation therapy have been reported in professional groups (such as night shift nurses, metropolitan workers) experiencing sleep disorders.[11,12] However, information on specific methods such as the type of aroma used and the usage time is unclear.[14] Therefore, this study quantitatively analyzed the effects of aroma inhalation therapy for sleep disorders and assessed the most effective oil for sleep. This study provides information on the aroma that can be used by anyone to improve sleep problems in their daily life and obtain the maximum beneficial effects of sleep.
2. Methods
2.1. Study registration
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (registration number, CRD42020142120) on March 02, 2020, and has been reported following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines for systematic reviews.[18]
2.2. Study design
This systematic literature review and meta-analysis analyzed the reported effects of the aroma inhalation method on the improvement of sleep problems.
2.3. Data sources
The literature search was conducted by 3 researchers and 2 methodologists with information collated from domestic and foreign databases, including 5 Korean-language databases (Oriental Medicine Advanced Searching Integrated System [OASIS], Korean Studies Information Service System [KISS], Research Information Service System [RISS], Korean Medical Database [KMbase], and Korea Citation Index [KCI]) and 6 English-language databases (MEDLINE via PubMed, EMBASE via Elsevier, the Allied and Complementary Medicine Database [AMED] via EBSCO, the Cochrane Central Register of Controlled Trials [CENTRAL], the Cumulative Index to Nursing and Allied Health Literature [CINAHL] via EBSCO, and PsycARTICLES via ProQuest). We also searched the “gray literature” that including unpublished articles. There were no language restrictions.
2.4. Search strategies
A presearch was conducted based on the MeSH term for the treatment of sleep disorders using aromatherapy. Subsequently, search terms that were included in the search strategy were implemented following the procedure. The search terms were as follows: “Insomnia,” “Sleep Disorder,” “Sleep Problem,” “Aroma Therapy,” and “Aroma Inhalation therapy.” In addition, for Ovid-MEDLINE, EMBASE, and SIGN, and PubMed, search filters used in the Shojania et al[19] study were used to increase the specificity of the searches. Furthermore, existing systematic literature reviews and Cochrane reviews of relevant topics were considered when constructing the search strategy.
2.5. Study selection
2.5.1. Types of studies
Studies selected were the randomized control trials (RCTs). Studies that used inappropriate random sequence generation methods such as alternate allocation were excluded. Studies included systematic reviews in experimental studies where meta-analyzed figures were provided, which investigated sleep disorders and sleep problems associated with the inhalation of aroma oil. Specifically, the selection of the thesis was done using the criteria of the core questionnaire PICO (Patient/Participants/Population/Problem, Intervention, Comparison, and Outcome) in this study. Furthermore, to check the effectiveness of aroma inhalation in improving sleep problems, the types of aroma, and methods of aroma mixing were included as adjustment parameters. However, other designs such as in vivo, in vitro, case reports or studies, retrospective studies, qualitative studies, uncontrolled trials, and trials, that failed to provide detailed results, were excluded. Details of the study design are outlined in Table 1.
Table 1.
Study type selection according to PICO.
| Criteria factor | Standard contents |
| Research method | RCTs conducted with the quantitative research method (except for retrospective studies, in vivo, in vitro, case reports or studies, qualitative studies, and uncontrolled trials) |
| Research design | RCT studies |
| Purpose | Reasonable for the research purposes should be revealed. |
| Participants/Patients | Participants with insomnia and sleep disorders diagnosed using standardized diagnostic tools such as the DSM-5; there was no restriction on the sex or race of the participants or sleep problems and disorders. |
| Intervention/Moderate variables | Direct/Indirect (such as necklace) inhalation method of aromatherapy |
| Comparator | There was no restriction. |
| Outcomes | -Primary outcomesEffect on quality of sleep (1) Pittsburgh Sleep Quality Index (PSQI) (2) SHV (Synder-Halpern and Verran, 1987) (3) Insomnia Severity Index (4) Korean Sleep Scale A (5) Q.O.S (Quality of Sleep) (6) VAS (7) Stanford Sleepiness Scale (8) NRS (Numeric Rating Scale) |
| -Secondary outcomes (1) Depression (Beck Depression Inventory) (2) Stress (Physical stress, Psychological stress) (3) Status anxiety (4) Fatigue | |
| Data statistics | All sorts of values, such as mean, standard deviation, t and f values, calculated effect size |
2.5.2. Types of participants
We included studies on people with undiagnosed sleep problems and patients, aged 20 to 60 years, with sleep disorders diagnosed using standardized diagnostic tools such as the Diagnostic and Statistical Manual of Mental Disorders-5. There were no restrictions on the sex or race of the participants.
2.5.3. Types of interventions
The intervention methods were aroma inhalation methods.
2.6. Types of outcome measures
2.6.1. The primary outcomes
Primary outcomes were sleep quantitative and qualitative inventories
-
a.
Effect on the quantitative sleep time, which was evaluated using the following measures:
-
(1)
The activity recorder (actigraphy)[20] records the activity during sleep when worn on the wrist or ankle.
-
(2)
Polysomnography (PSG)[21] test measures the physiological changes that occur during sleep by measuring the EEG, EMG, ECG, snoring, respiration, and diagnoses of the disorder
-
(3)
The sleep diary[22,23] used to measure the patient's sleep habits, sleep hygiene, and sleep problems for 2 weeks, and to evaluate the progress of the treatment.
-
(4)
Total sleep time (TST)[24]: insufficient sleep if total sleep time was lower than.[25]
-
(5)
Sleep onset latency (SOL)[26,27]: insufficient sleep when the elevation delay time was more than 30 minutes.
-
(6)
Wake-up Sleep On Time (WASO)[28]: If the awakening time was >30 minutes after the elevation, the sleep is considered insufficient.
-
(7)
Sleep Efficiency (SE)[29]: Sleep efficiency of ≤85% was considered insufficient.
-
(1)
-
b.
Effect on quality of sleep
Patient reporting tools used, with proven reliability and validity, are as follows:
-
(1)
The Pittsburgh Sleep Quality Index (PSQI)[30] consists of 19 self-reporting questions about sleep quality and discomfort over the past month. The total score ranges from 0 to 21; the lower the total score, the better the quality of sleep, and the higher the total score, the worse the sleep quality.
-
(2)
The Insomnia Severity Index (ISI),[31] developed to assess insomnia, is a self-reporting measure that comprises a total of 7 questions. It is a 5-point scale with higher scores indicating more serious insomnia.
-
(3)
The Medical Outcome Study Sleep Scale,[32] consists of 12 questions, measured in the range of 0 to 100; the lower the score, the better the quality of sleep.
-
(4)
The Stanford Sleep Questionnaire (SSQ)[33,34] has 7 classes, with subjective sleepiness levels of 1 to 7; lower scores indicate better sleep quality.
-
(5)
The Women's Health Initiative Insomnia Rating Scale (WHIIRS)[35] consists of 5-item scales for sleep initiation and maintenance and evaluates the subjective sleep quality. The lower the score, the better the sleep quality.
-
(6)
Sleeping measure[36] consists of 15 questions and is a 4-point scale. It has a range of up to 60 points from a minimum of 15 points, and a higher score indicates better sleep.
2.6.2. The secondary outcomes
Secondary medical outcomes reported were depression, stress, anxiety, and decreased fatigue. They were assessed as follows;
-
(1)
Change in the degree of depression as measured by validated assessment tools such as the Hamilton Depression Scale (HAMD)[37] and the Beck Depression Inventory (BDI).[38]
-
(2)
Stress was measured using the perceived stress scale (PSS).[39,40]
-
(3)
Anxiety was measured using the State-Trait Anxiety Inventory State version (STAI).[41]
-
(4)
Fatigue was measured using the fatigue symptom inventory (FSI).[42]
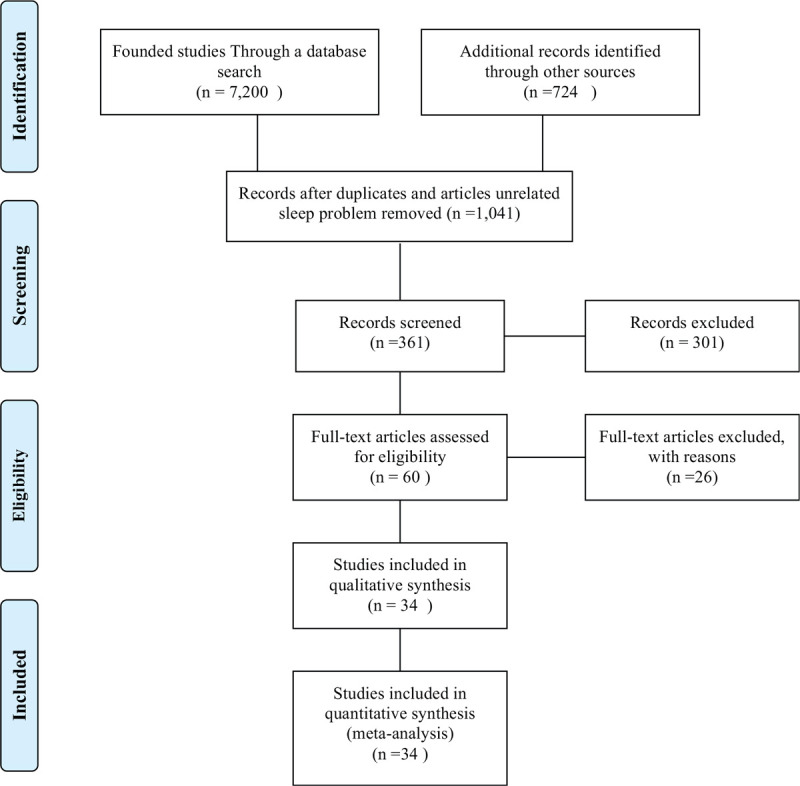
2.7. Study selection
Screening procedure is as follows. Domestic and international online databases were searched. A total of 7924 articles, including 7200 articles registered with keywords of “aroma” and “sleep problems” from 2000 to 2019 and 724 additional articles from other search sources, were collected. Among them, a total of 1240 papers that were duplicates and 5643 articles that were not conducted on humans and subjects with sleep problems, were excluded. A total of 21 articles on meta-analysis, including systemic literature reviews and 659 studies on non-aroma inhalation therapy were excluded from the remaining 1041 articles. A total of 301 studies that did not report improved sleep and 26 articles that did not correspond to Participants, Intervention, Control, Outcomes & Study Design for the systemic literature review were excluded. In the end, a total of 34 articles were selected and numerical values were reported in all these articles. The meta-analysis was performed and results were reported following the PRISMA guidelines (Guidelines Flow Diagram).[18]
Figure 1.
Guidelines flow diagram.
2.8. Data coding extraction
Using a standardized data collection form, 3 independent researchers cross-checked the data extraction process. Discrepancies were resolved through discussion with other researchers. The coding plate was constructed, as shown in Table 2, to analyze the extracted data. The coding of data for this study was based on a meta-analysis of various aromatherapy effects on the sleep disorders reported by Hwang and Shin.[3] In addition, based on the paper by Lillehei and Halcon,[43] basic information (author, year, and title), method of intervention (direct or indirect aromatherapy), and interventions (aroma type: single or mixed, study group characteristics: general, patient, etc) were included in the proceedings (total sessions, weekly sessions, session hours). To ensure the reliability of the meta-analysis coding, one researcher with experience in the meta-analysis, one researcher with a major in applied statistics of research methodology and meta-analysis, and one specialist from oriental neurological psychiatry that used aromas to treat insomnia, were cross-coded as well. During the course of coding, the paper, which showed no consensus or required more confirmation, an expert on insomnia was consulted. The coding analysis table is shown in Table 2.
Table 2.
Data coding extraction.
| Variables | Moderator | ||
| Outcomes | Primary outcomes | ||
| Secondary outcomes | |||
| Kinds of aroma | Single | Lavender, phytoncide, rosemary, | |
| Rosadamascence | |||
| Mixed | Sweet orange, Rosewood marjoram | ||
| Ylang-Ylang, Bergamot, Basil exotic | |||
| Cymbopogon marini | |||
| Aniba rosaeodora, Roman Chamomile | |||
| Citrus bergamia | |||
| Grapefruit, Citrus paradisi, | |||
| Geranium, Neroli, | |||
| Citrus aurantium L. var | |||
| Subjects | Cardiac diseases | Patients with cardiac stentsThe heart disease | |
| Participants | Patients | Section | Cesarean sectionColectomy, hysterectomy |
| pneumonectomy | |||
| Psychological disorders or problems | Sleep disorders such as insomnia, sleep problems, anxiety disorder, schizophrenia | ||
| ETC. | Pain patient, essential hypertension, patient undergoing hemodialysis | ||
| Coronary arteriography patient, patient in an intensive care unit | |||
| Non-patients | |||
| Job kind | Night shift nurses, subway worker (night shift) | ||
| Nation | Domestic | Korea | |
| Others | |||
| Inhalation | Direct | ||
| Methods | Indirect | ||
2.9. Quality assessment of articles
Quality assessment of articles was conducted using Review Manager version 5.3 software (Cochrane, London, UK), to assess the risks of random selection, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The risk was evaluated as “low, high, and unclear.”[44]
2.10. Literature evaluation and sorting
Results from the included 34 papers following the systematic literature review were analyzed, encoded, and arranged into forms. The forms included the selection of research design, number of participants, criteria for participant selection and exclusion, measurement variables and tools, result variables, and statistical values. To ensure accuracy during the process, 2 researchers independently conducted the evaluations, and the results were cross-checked and compared for inter-rater agreement.
2.11. Meta-analysis
The data analysis procedure included the verification of publication bias errors, verification of homogeneity and heterogeneity, calculation of total effect size, and meta-analysis of variance (meta-ANOVA) for aromatherapy over time and period of intervention (meta-ANOVA with aroma type, aroma single or mixed/research group, and aroma direct and indirect effects). In addition, the size of the calibration effect (Hedge g) was used to give weight to the number of cases studied. This required Hedge g to be calibrated due to the intergroup effect size and Cohen d tends to overestimate the effect size when the sample is small.[45] Finally, for the analysis of the data, such as effectiveness size and homogeneity verification, a statistical program for meta-analysis (Comprehensive Meta-Analysis version 2.0 [Biostat Inc, NJ]) was used. All analysis process was consulted by a meta-analysis expert.
2.12. Additional analyses
For additional analyses, meta-regression analysis was performed using the primary and secondary outcomes as continuous variables.
2.13. Ethics and dissemination
Ethical approval was not required because the data used in this systematic review were not individual patient data; therefore, there were no concerns regarding privacy.
3. Results
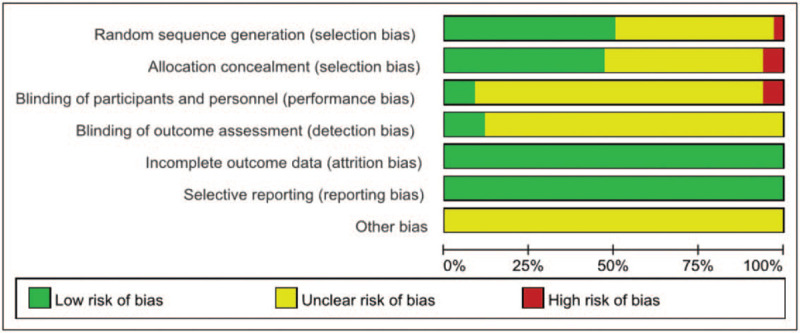
3.1. Quality assessment results
For the quality assessment of articles, there was a high risk of bias in blinding of participants and personnel, which was a performance bias, and in the allocation concealment and random sequence generation, which were selection biases. Additionally, an unclear risk of bias was observed for blinding of outcome assessment, which was detection and other biases. However, low risk was observed for incomplete outcome data and selective reporting (Figs. 2 and 3).
Figure 2.
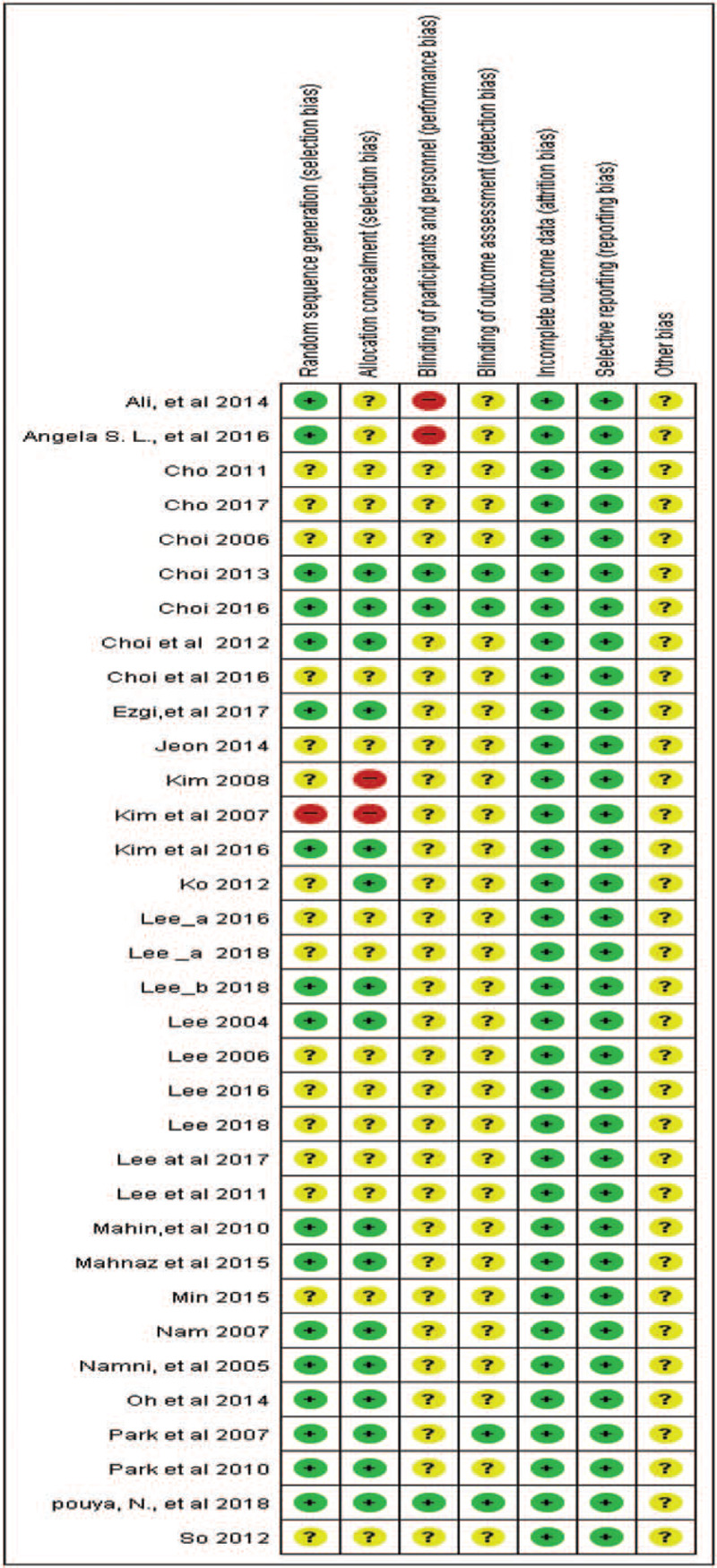
Risk of bias included in the study.
Figure 3.
The risk of bias using RevMan.
3.2. Systematic literature review evaluation and sorting results
The systemic literature review results are as follows. Among the 34 studies (Tables 3 and 4), 13 articles (37.2%) and 21 articles (62%) used single and mixed aromas, respectively. Among the 13 articles that used single aroma oil for inhalation, lavender aroma oil was used in 10 studies (76%). Additionally, lavender was used in 16 papers that used mixed aromas. This finding suggests a bias of oils related to sleep and it is necessary to assess why lavender aroma improves sleep. A total of 3, 13, and 18 articles performed indirect inhalation (necklace, etc), a mix of indirect and direct inhalation, and direct inhalation, respectively. Tools used to analyze main effects and evaluate improvements in sleep disorders included the sleep scale A developed in Korea (9 studies), Pittsburg sleep quality index (4 studies), and Snyder-Halpern and Verran[46] sleep scale (8 studies). Assessment of secondary effects showed both decreased psychological problems such as depression and anxiety, and the physiological functions, including blood pressure and fatigue. As a result, the systematic literature review demonstrated that aroma inhalation therapy was beneficial in improving sleep.
Table 3.
Studies included in the systematic review and meta-analysis.
| Ko, Ye Jung. Effects of lavender fragrance inhalation method on sleep, depression and stress of institutionalized elderly. Journal of East-West Nursing Research, 2012, 18.2: 74–80. |
| Kim, O.J. The effect of aroma inhalation method on stress, anxiety and sleep pattern in patients undergoing hemodialysis. Unpublished master's thesis, Chung-Ang University, Seoul, 2007. |
| Park, Sihyun, et al. The effect of aroma inhalation therapy on fatigue and sleep in nurse shift workers. Journal of East-West Nursing Research, 2012, 18.2: 66–73. |
| Choi, Eun-Mi; Lee, Kyung-Sook. Effects of aroma inhalation on blood pressure, pulse rate, sleep, stress, and anxiety in patients with essential hypertension. Journal of Korean Biological Nursing Science, 2012, 14.1: 41–48. |
| Oh, Hyun-Mi; Jung, Geum-Sook; Kim, Ja Ok. The effects of aroma inhalation method with roll-on in occupation stress, depression and sleep in female manufacture shift workers. Journal of the Korea Academia-Industrial cooperation Society, 2014, 15.5: 2903–2913. |
| Kim, WonJong; Hur, Myung-Haeng. Inhalation effects of aroma essential oil on quality of sleep for shift nurses after night work. Journal of Korean Academy of Nursing, 2016, 46.6: 769–779. |
| Park, S., et al. The effects of aroma therapy on sleep disorder patients with musculoskeletal pain. J Oriental Rehab Med, 2010, 20: 215–230. |
| Choi, Jae-won, et al. Phytoncide aroma inhalation and exercise combination therapy mood state, college life stress and sleep of college students. Journal of Digital Convergence, 2016, 14.12: 633–644. |
| Lee, Sun-Ok; Hwang, Jin-Hee. Effects of aroma inhalation method on subjective quality of sleep, state anxiety, and depression in mothers following cesarean section delivery. Journal of Korean Academy of Fundamentals of Nursing, 2011, 18.1: 54. |
| Lee Gyeong-Jae. A Study on the Effect of Aroma on Sleep and Fatigue of Subway Crew. Graduate School of Glocal Integration at Sunmoon University: Natural healing studies 2018. Master thesis. |
| Choi Seo Yeon. (The) effects of aroma oil inhalation therapy on appetite, sleep, and stress in middle-aged overweight women: a randomized controlled trial. Graduate School of Chung-Ang University: Graduate School of Nursing and Nursing Studies. 2016. Doctoral thesis. |
| Lee Sook-hyun. Effects of Aromatherapy on Stress Response, Sleep and Immunity in Middle-Aged Women. Graduate School of Eulji University: Nursing and Nursing Studies. 2018. Doctoral thesis. |
| Lee Yoo-jin. The Inhalation Effects of Aroma Essential Oil on Stress, Sleep Quality and Immunity of Shift work Nurses: A Parallel group Randomized Controlled Trial. Graduate School of Clinical Nursing at Eulji University: Clinical nursing education major clinical nursing education. 2018. Master thesis. |
| Cho, M.Y. The effects of Aromatherapy on Anxiety, Vital sign & Sleep of PCI patients hospitalized in intensive care units. Unpublished master's, Eulji University, Daejeon, 2011. |
| Choi Myung-ja. The Effects of Aromatherapy on Alleviation of Stress Among Schipzophrenic Patients. Graduate School of Health at Chosun University: Alternative Medicine. 2006. |
| Lee, M. H. The effect of aroma therapy on the comfort, anxiety and sleep of heart stent spiled patients hospitalized in intensive care unit. Unpublished master's, Dong-A University, Pusan, 2006. |
| Cho Eun-hee. The Effects of Aromatherapy on Stress, and Sleep Quality in ICU patients. Graduate School of Clinical Nursing at Eulji University: Clinical nursing education major, clinical nursing education. 2017. |
| Lee Jin-kyung. The Effect of Aroma Inhalation on Fatigue and Sleep: Focused on Mothers with Preschool Children. Graduate School of Alternative Medicine at Kyunggi University: A major in alternative medicine and psychiatric treatment. 2017. |
| Min Kyung-min. The effect of inhaling orange, lavender and chamomile roman aromas on the quality of sleep and fatigue of shift working nurses. Chung-Ang University Graduate School: Graduate School of Nursing and Nursing Studies. 2015. |
| Kim Hye-yeon. (The) effect of aromatheray on anxiety and sleep of patients with coronary angiography. Dankook University Graduate School: Graduate School of Nursing and Clinical Nursing in 2008. |
| So Hae-Ran. The Effect of Aroma Inhalation on Pain, Anxiety, Vital Sign and Sleep of Patients with Colon Resection. Gachon University Graduate School of Nursing: Senior Nursing Education. 2012. |
| Choi Jeong-hee. Effects of Aroma Inhalation Therapy on Pain, Stress, Nausea·Vomiting and Sleep of Patients Following a Hysterectomy. Graduate School of Gachon University: Nursing for the Elderly 2013. |
| Lee Won-jin. Effects of Aroma Inhalation to Blood Pressure, Pain and Quality of Sleep in Patients with Pulmonary Resection. Graduate School of Ewha Women's University: Department of Nursing Science. 2016. |
| Jeon WhaYoung. Aromatherapy effects on sleep improvement and depression in middle-aged women. Chosun University: Alternative Medicine, 2015. |
| Nam Jung-ja. Effects of aromatherapy and massage on sleep disturbance and problematic behaviors on elderly with dementia. Graduate School of Ewha Womans University: Department of Nursing Science, 2008. |
| Lillehei, Angela Smith, et al. Well-being and self-assessment of change: Secondary analysis of an RCT that demonstrated benefit of inhaled lavender and sleep hygiene in college students with sleep problems. Explore, 2016, 12.6: 427–435. |
| Nematolahi, Pouya, et al. Effects of Rosmarinus officinalis L. on memory performance, anxiety, depression, and sleep quality in university students: a randomized clinical trial. Complementary therapies in clinical practice, 2018, 30: 24–28. |
| Lee, Mi-kyoung, et al. The effects of aromatherapy essential oil inhalation on stress, sleep quality and immunity in healthy adults: Randomized controlled trial. European Journal of Integrative Medicine, 2017, 12: 79–86. |
| Afshar, Mahnaz Keshavarz, et al. Lavender fragrance essential oil and the quality of sleep in postpartum women. Iranian Red Crescent Medical Journal, 2015, 17.4. |
| Lee, Sung-Hee. Effects of aroma inhalation on fatigue and sleep quality of postpartum mothers. Korean Journal of Women Health Nursing, 2004, 10.3: 235–243. |
| Hajibagheri, Ali; Babaii, Atye; Adib-hajbaghery, Mohsen. Effect of Rosa damascene aromatherapy on sleep quality in cardiac patients: a randomized controlled trial. Complementary therapies in clinical practice, 2014, 20.3: 159–163. |
| Karadag, Ezgi, et al. Effects of aromatherapy on sleep quality and anxiety of patients. Nursing in critical care, 2017, 22.2: 105–112. |
| Goel, Namni; Kim, Hyungsoo; Lao, Raymund P. An olfactory stimulus modifies nighttime sleep in young men and women. Chronobiology International, 2005, 22.5: 889–904. |
| Moeini, Mahin, et al. Effect of aromatherapy on the quality of sleep in ischemic heart disease patients hospitalized in intensive care units of heart hospitals of the Isfahan University of Medical Sciences. Iranian journal of nursing and midwifery research, 2010, 15.4: 234. |
Table 4.
Systematic literature review evaluation and sorting results.
| Study (year) | Aroma (single/mixed) | Application | Research design | Nation | Samplesize (n) | Primary outcome | Secondary outcome | Subject character |
| 1. Ko (2012) | Lavender (single) | Direct inhalation | Equivalent control /RCT | Korea. | 39 (exp: 18, cont: 21) | Korea Sleep Scale A(+) | Depression(−)Stress(−) | An elderly person living in a facility |
| 2. Kim et al (2007) | Lavender, sweet orange2:1 (Mixed) | Direct inhalation | Equivalent control /RCT | Korea. | 50 (exp: 25, cont: 25) | Korea Sleep Scale A(+) | Stress (−)Anxiety(−) | Chronic hemodialysis patients |
| 3. Park et al (2007) | Lavender, Rosewood 1: 1 (Mixed) | Direct inhalation | Nonequivalent control /RCT | Korea. | 60 (exp: 30, cont: 30) | Sleep Quality Scale(+) | Fatique(−) | Nurse Shift Workers |
| 4. Choi et al (2012) | Lavender Marjoram, Ylang-Ylang 4: 3: 3 (Mixed) | Direct inhalation | Equivalent control /RCT | Korea | 36 (exp: 20, cont: 16) | Sleep state(−)SleepSatisfaction(+) | Stress(−)Anxiety(−) | Patients with essential hypertension |
| 5. Oh et al (2014) | Bergamot, Lavender, Ylang-Ylang, Jojoba oil 1: 1: 1: 1 (Mixed) | Inirect inhalation | Nonequivalent control group/RCT | Korea | 52 (exp: 26, cont: 26) | Korea Sleep Scale A(+) | Depression(−)Job stress(−) | Female production workers |
| 6. Kim et al (2016) | Lavender | Direct and indirect inhalation | Nonequivalent control group/RCT | Korea | 60 (exp: 30, cont: 30) | -Quality of Sleep [QOS](+)-[NRS])(+) [VSH](+)-([NoA])(+) | Night shift nurse | |
| 7. Park et al (2010) | Lavender, Vergamot, Basil exotic 2: 2: 1 (Mixed) | Direct and indirect inhalation | Equivalent control group | Korea | 60 (exp: 30, cont: 30) | Korea Sleep Scale A(+) | Patients with musculoskeletal pain | |
| 8. Choi et al (2016) | Phytoncide | Direct inhalation | RCT | Korea | 34 (exp: 14, cont: 20) | Korea Sleep Scale A(+) | -College Life Stress(−)-Feeling Scale L FS | University students |
| 9. Lee et al (2011) | Lavender | Direct inhalation | Nonequivalent control group /RCT | Korea | 67 (exp: 33, cont: 34) | Korea Sleep Scale A(+) | (State-Trait Anxiety Inventory(−)Depression (−) | Cesarean section mother |
| 10. Lee (2018) | Cymbopogon marini, Aniba rosaeodora, Citrus bergamia 1: 1: 1 (Mixed) | Direct inhalation | Nonequivalent control Group /RCT | Korea | 60 (exp: 30, cont: 30) | -Quality of Sleep [QOS] (+) | Japan Society for Occupational Health (Fatique)(−) | Subway crew in shift work |
| 11. Choi (2016) | Grapefruit, Citrus paradisi, Geranium, Neroli 4: 2: 3 (Mixed) | Direct inhalation | RCT | Korea | 54 (exp: 27, cont: 27) | -Quality of Sleep [QOS](+) (Synder Halperm Verran: VHS)VSH sleep scale(+) | -Visual analog scale: (VAS)(NPY/ GLP-1 | Overweight middle-aged woman |
| 12. Lee (2018) | Lavender, Ylang-Ylang, Marjoram 4: 1: 5 (Mixed) | Direct inhalation/Indirect inhalation | RCT | Korea | 62 (exp: 31, cont: 31) | Verran & Synder-Halpern Sleep (+) | -Subjective stress response (NRS)(−)-Physiological stress response(−) | A middle-aged woman |
| 13. Lee (2018) | Lavender, Ylang-Ylang, Neroli 4: 2: 1 (Mixed) | Direct inhalation | RCT | Korea | 63 (exp: 31, cont: 32) | -Quality of Sleep [QOS](+)- NRS (Numeric Rating Scale)(+) -VSH-(Actigraph[63])-(Turbidimetric Immnuassay, TIA) | Stress(−)-NRS (Numeric Rating Scale)-Serum cortisol levels | Night shift nurse |
| 14. Cho (2011) | Lavender, Roman Chamomile, Neroli2: 1: 0.5 (Mixed) | Direct inhalation | Non-equivalent control group pretest-/RCT | Korea | 56 (exp: 28, cont: 28) | -VSH (Snyder-Halpern and Verran )[46] Sleep Scale | Anxiety-(STAI-KYZ)-Blood pressure | Patient with cardiac stent intubation |
| 15. Choi (2011) | Roman Chamomile, Lavender, Marjoram, Sandalwood3: 2: 1: 1 (Mixed) | Direct inhalation | Non-equivalent control group /RCT | Korea | 74 (exp: 37, cont: 37) | Korea Sleep Scale A(+) | Stress(−)PWI(+) | Schizophrenic |
| 16. Lee (2006) | Lavender, Roman Chamomile2: 1 (Mixed) | Direct inhalation/Indirect inhalation | Nonequivalent control Group/RCT | Korea | 40 (exp: 20, cont: 20) | -VSH(+) | -ComfortGeneral comfort questionnnaire-Anxiety (−) | Patient with cardiac stent intubation |
| 17. Cho (2017) | Lavender | Direct inhalation | Nonequivalentcontrol Group/RCT | Korea | 60 (exp: 30, cont: 30) | -VSH(+) | -Subject Stress-NRS(−)- (Stress Index [S.I])- (Blood pressure) | Clinical pulmonary infection score |
| 18. Lee (2016) | Bergamot, Lavender, sweet Majoram1: 2: 1 (Mixed) | Direct inhalation/Indirect inhalation | Nonequivalent control group /RCT | Korea | 40 (exp: 19, cont: 20) | -VSH(+) | -Fatique (Japan Society for Occupational Health) | General |
| 19. Min (2015) | Sweet Orange, Lavender, Chamomile | Direct inhalation/Indirect inhalation | Nonequivalent control Group /RCT | Korea | 60 (exp: 30, cont: 30) | -Quality of Sleep [QOS](+) | -Fatigue (japan Society for Occupational Health) | Night shift nurse |
| 20. Kim (2008) | Bergamot, Lavender, Ylang-Ylang, 3: 3: 1 (Mixed) | Direct inhalation/Indirect inhalation | Non-equivalent control group /RCT | Korea | 39 (exp: 18, cont: 18) | -VSH(+)-Sleep satisfaction (VAS)[66](−) | -Anxiety (−) | Coronary angiography patients |
| 21. So (2012) | Lavender, Sweet Orange, Meichang: 2: 1: 1 (Mixed) | Direct inhalation/Indirect inhalation | Nonequivalent control group/RCT | Korea | 70 (exp: 35, cont: 35) | Visual Analogue Scale: VAS(−) | -Pain (−) (VisualAnalogue Scale: VAS)-Anxiety(−)-Vitals signal | The paitients done colon resection |
| 22. Choi (2013) | Lavender, Mandarin, Majoram3: 2: 1 (Mixed) | Direct inhalation/Indirect inhalation | Nonequivalent control group/RCT | Korea | 60 (exp: 30, cont: 30) | -Korea Sleep Scale A(+)-VAS(−) | -Pain(−)/-Stress (−)-Cotisol-Index of nausea vomiting & retching | Hysterectomy patient |
| 23. Lee (2016) | Chamomile, Sweet Orange1: 2 (Mixed) | Direct inhalation/Indirect inhalation | RCT | Korea | 53 (exp: 27, cont: 26) | -VSH(+) | -Pain(−) | Pneumonectomy |
| 24. Jeon (2014) | Argan Oil, sweat almond oil Lavender geranium, Chamaecyparis obtusa essence (not information) | Direct inhalation/Indirect inhalation | RCT | Korea | 19 (exp: 12, cont: 7) | -Korea Sleep Scale A(+)-VAS(−) | -Depression(−) | Middle women |
| 25. Nam (2007) | Lavender | Direct inhalation/Indirect inhalation | RCT | Korea | 36 (exp: 18, cont: 18) | -Researcher devised sleep disorder observation record (−) | Problem behavior measurement (Kim, 2003[66]) | |
| 26. Lillehei et al (2016) | Lavender | Direct inhalation | RCT | USA | 76 (exp: 38, cont: 38) | -PSQI (Pittsburgh Sleep Quality Index)(−) | -Self Assessment of Change Questionair (not.sig) | College students with sleep problems |
| 27. pouya Nematolahi et al (2018) | Rosemary | Direct inhalation | RCT | IRAN | 68 (exp: 34, cont: 34) | -PSQI (Pittsburgh Sleep Quality Index)(−) | -HAS(−)_HAD(−)-Memory (not sig.) | General |
| 28. Lee et al (2017) | Lemon, eucalyptus, tea tree, peppermint4: 2: 2: 1 (Mixed) | Direct inhalation | RCT | Kor | 60 (exp: 30, cont: 30) | -QOS(−)-time of sleep(+) | -Stress Index(−)-Depression(−) | General |
| 29. Mahnaz et al (2015) | Lavender | Direct inhalation | RCT | IRAN | 158 (exp79, cont: 79) | QOS | ||
| 30. Lee (2004) | Lavender, eucalyptusNot information | Direct /Indirect inhalation | RCT | Kor | 51 (exp25, cont: 26) | QOS(−)-SHV(+)/-VAS(−) | -Rhoten Fatique(−) | |
| 31. Ali, et al (2014) | Rosa damascence | Indirect inhalation | RCT | IRAN | 60 (exp30, cont: 30) | −PSQI(−) | Cardiac patients | |
| 32. Ezgi, et al (2017) | Lavender | Indirect inhalation | RCT | Turkey | 60 (exp30, cont: 30) | −PSQI(−) | -BAI(−) | Sleep disorder and anxiety patietns |
| 33. Namni, et al (2005) | Lavender | Direct inhalation | RCT | USA | 31 (exp16, cont: 15) | −Stanford Sleepiness Scale(−)-The Profile of Mood State Questionnaire(−) | General | |
| 34. Mahin, et al (2010) | Lavender | Direct inhalation | RCT | IRAN | 64 (exp32, cont: 32) | QOS(−) | General |
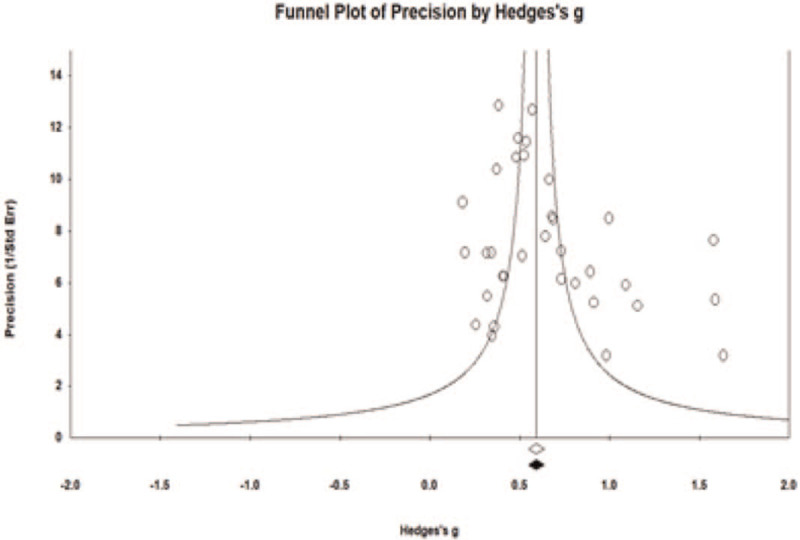
3.3. Publication bias analysis
The final 34 selected papers, shown in Table 5 (effect size case = 273), were analyzed for publication bias. In this study, we examined the publication bias (Figs. 2 and 3) of the papers collected through the funnel plot (Fig. 4) and analyzed the bias of the samples in a complementary manner using the estimation and fill method. As shown in Figs. 5 and 6, the funnel plot is somewhat symmetrical and had no issues with bias.[47] In addition, sensitivity analysis, which is the estimation additive (Trim & Fill) of the complementary methods of Duvall and Tweedie,[48] resulted in the same calibration and observation values of the coordinated study (Table 6).
Table 5.
Effect size based on research duration of the time and times.
| Variables | K | ES (g) | SE | 95% CI | P | QB (df) |
| Inhalation time | ||||||
| 24 hours | 32 | 0.476 | 0.060 | 0.358–0.594 | .000 | 5.637 (1)∗ |
| Before sleep | 139 | 0.661 | 0.049 | 0.564–0.758 | .000 | |
| The number of aroma inhalation | ||||||
| 1 | 104 | 0.699 | 0.059 | 0.583–0.816 | .000 | 3.504 (2) |
| 2 | 10 | 0.645 | 0.154 | 0.344–0.946 | .000 | |
| 3 | 25 | 0.534 | 0.073 | 0.390–0.678 | .000 | |
| N | ES (g) | SE | 95% CI | P | ||
| Nation | ||||||
| Korea | 25 | 0.724 | 0.071 | 0.586–0.863 | .000 | 7.766∗∗ (1) |
| the others | 9 | 0.470 | 0.058 | 0.357–0.583 | .000 | |
Figure 4.
Funnel plot of the publication bias.
Figure 5.
Forest plot of the aroma inhalation therapy.
Figure 6.
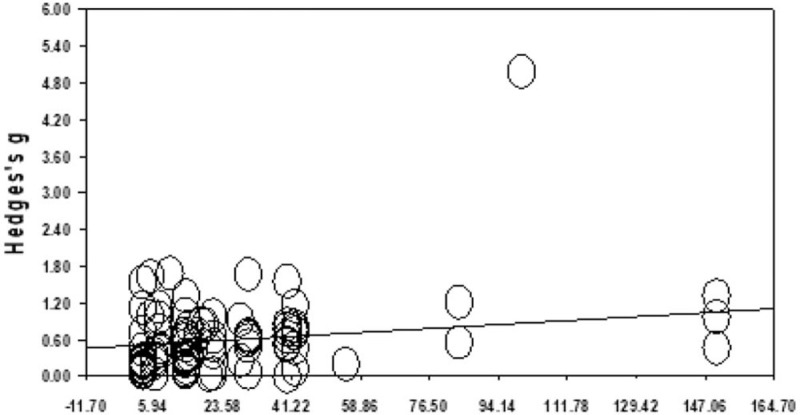
The regression analysis of aroma therapy program according to years about for the slope of the primary outcome.
Table 6.
Result of the Trim and Fill.
| Studies trimmed | ESc | 95% CI | Q | |
| Observed values | 0.64971 | 0.54224–0.75719 | 193.51456 | |
| Adjusted values | 0 | 0.64971 | 0.54224–0.75719 |
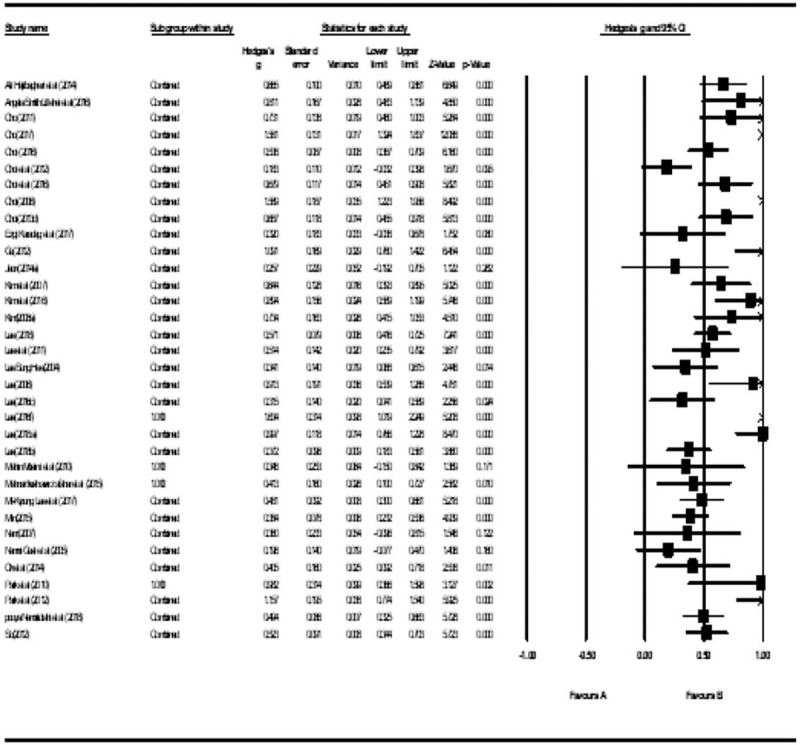
3.4. Verification of homogeneity and overall effect size of aroma inhalation effect on sleep problem
The results of the evaluation of the total effect size of aromatherapy, calculated from 172 effect sizes culled from the 34 studies included in the present study, are shown in Table 4. The homogeneity test was performed at a significance level of P < .05, resulting in the application of the random effect model, which was determined to be heterogeneous by rejecting the null hypothesis at 193.515 (P < .01).[49] The value of I, which represents the ratio of the total variance contrast study, was 82.947, which is >50 and thus had significant heterogeneity. In addition, since each study was assessed differently by different researchers, estimates of population effect size were not the same. Therefore, the analysis reported in this paper was conducted using a random-effect model, since the size of the effects assessed by the researchers varied, and was statistically significant through heterogeneity analysis (Table 7). The total effect size for sleep problems was 0.650 and the 95% confidence interval for the total effect size ranged from 0.542 to 0.757. This is equivalent to 73% to 76% if the U-index, the cumulative distribution analysis method of effect size, is presented. The effect size of 0.65 implies that the control group showed 50% effectiveness in the experiment, whereas the effectiveness ranged from 73% to 76% for the experimental group. Therefore, the experimental group exceeded the median value of the control group (50% for the control group) with a success rate of 73% to 76%. Thus, the program effectiveness of the experimental group that used aromatherapy for sleep problems can be interpreted as 23 to 26 higher than the program effectiveness of the control group (Rosenthal and Rubin[50]). The criteria of Cohen[51] and Wolf[52,53] were to interpret the magnitude of the effects assessed in the meta-analysis. Cohen[51] interpreted the average effect size (d) below 0.2 as a small effect size, 0.5 as a medium effect size, and 0.8 as a large effect size. Wolf[52] has an educational significance if its effect size is >0.25. At least 5 studies, the criteria for interpretation were presented as significant at a practical and therapeutic level. According to this criterion, the overall average effect size of the aroma inhalation method for sleep problems was 0.65, which was greater than the middle effect size. Thus, the groups that conducted the aromatherapy program had a more significant outcome on the overall average effect size compared with those that did not (Fig. 5).
Table 7.
Validation of the homogeneity and effect size of the primary outcomes.
| Model | N | K | ES (g) |  |
95% CI | Q(df) | I2 |
| Fixed | 34 | 172 | 0.593 | 82.86 | 0.551–0.636 | 193.515(33) | 82.947∗∗ |
| Random | 34 | 172 | 0.650 | 84.05 | 0.542–0.757 |
3.5. Effect sizes of secondary outcomes
After each classification for negative effects analysis, the differences between each group, and the size of the effects were verified. The effect size of each program was as follows: stress (effect sizes [ES](g) = 0.838, P < .01), (anxiety (g) = 0.599, P < .01), other (blood pressure, appetite, pain, etc) (ES(g) = 0.592, P < .01), (depression(g) = 556, P < .01), and (fatigue(g) = 0.544, P < .01), demonstrating a statistically significant effect size. However, the differences in effects between the groups were not statistically significant. That is, even though inhalation of aromas had a significant effect on stress, anxiety, depression, and fatigue, it did not exhibit a statistically significant difference (Table 8).
Table 8.
The effect size of secondary outcomes.
| Secondary outcomes | K (%) | ES (g) | SE | 95% CI | P | QB (df) |
| Stress | 30 | 0.838 | 0.154 | 0.535–1.140 | .000 | 2.913(4) |
| Anxiety | 10 | 0.599 | 0.138 | 0.328–0.869 | .000 | |
| ETC (blood pressure, appetite, pain) | 27 | 0.592 | 0.081 | 0.434–0.750 | .000 | |
| Depression | 6 | 0.556 | 0.116 | 0.329–0.783 | .000 | |
| Fatigue | 10 | 0.544 | 0.089 | 0.370–0.719 | .000 |
3.6. Effect size according to intervention factors
In the meta-analysis, the modulating effect analysis according to the arbitrator more directly validated the difference in effect size among subgroups and allowed the effect on the average effect size to be verified through the study-level variables that describe the effect size, that is, the covariates or modifiers. In this study, we attempted to determine the statistical significance by conducting differential verification and regression analysis for each variable.
3.7. Individual effect size and meta-ANOVA test of category
3.7.1. The types of aroma (single or mixed)
After classifying the effects of single and compound aromas on sleep problems, the differences between groups and their sizes were analyzed. The difference in the size of the effects between the 2 groups (single aromas vs composite aromas) was (ES(g) = 0.720, P < in the case of single aromas .01), and (ES(g) = 0.576, P < .01) for composite aromas; each effect size was statistically significant. In addition, the effect of using a single aroma was significantly higher than that of the composite aromas (Q = 2.38(1) and P < .05) (Table 9).
Table 9.
The effect sizes of aroma types (single or mixed).
| K (%) | ES (g) | SE | 95% CI | P | QB (df) | |
| Single | 59 (34.5%) | 0.720∗∗ | 0.081 | 0.561–0.879 | .000 | 2.38∗ (1) |
| Mixed | 112 (65.5%) | 0.576∗∗ | 0.047 | 0.484–0.667 | .000 |
3.7.2. Analysis of effect size based on types of study subjects (clinical group and general [shift workers and non-shift workers])
The clinical (ES(g) = 0.782, P < .01) and general groups (ES(g) = 0.538, P < .01) (where the effect of the inhalation of aromas was statistically significant) exhibited a statistically significant inter-difference (Q(df) = 6.759(1), P < .05). This means that the aroma inhalation effect is also a night shift in the general population (ES(g) = 0.682, P < .01), General (ES(g) = 0.483, P < .01); each of the aroma inhalation was statistically significant for sleep but the difference between groups in the general population was not significant. This means that aroma inhalation has varying effects on different sleep disorders, without any significant difference recorded between the groups for shift workers or non-committal groups (Table 10).
Table 10.
Effect size based on types of study subjects (clinical group and general [shift workers and non-shift workers]).
| K (%) | ES (g) | SE | 95% CI | P | QB (df) | |
| Clinical group | 60 | 0.782 | 0.083 | 0.620–0.944 | .000 | 6.759 (1)∗ |
| General | 111 | 0.538 | 0.044 | 0.452–0.624 | .000 | |
| Non-night shift workers | 76 | 0.483 | 0.039 | 0.407–0.559 | .000 | 3.186 (1) |
| Night shift workers | 35 | 0.682 | 0.104 | 0.477–0.886 | .000 |
3.7.3. Analysis of effect size based on research duration of the time and times
As a mediator, the size of the effect of aroma inhalation on sleep problems was analyzed for 24 hours and before bedtime (1–3 times), that is, if aroma was inhaled from 1 to 3 times before bed (ES(g) = 0.661, P < .01), or if a 24 hours aroma necklace was worn or aroma was continuously inhaled using tools for indirect inhalation (ES(g) = 0.476; P < .01). This resulted in a greater effect of premagnetic inhalation than a 24 hours duration, indicating a statistically significant difference (Q(df) = 5.637, P < .05). Therefore, continuous inhalation of 1 to 3 times was more effective than 24 hours indirect inhalation for the amelioration of sleep problems, and that the differences in direct and indirect inhalation, rather than the duration of time, elicited a change in the size of the effects. In addition, after analyzing the effects of 1 to 3 cycles of inhalation before going to bed (the first time was [ES(g) = 0.699 and P < .01], [ES(g) = 0.645 and P < .01], the third [ES(g) = 0.534, P < .01]), each group showed a statistically significant effect but differences between groups were not statistically significant. Although there were differences in the effects of direct and indirect inhalation methods, the session not resulting in a statistically significant change could be due to the size of the effects. Next, the effectiveness of aroma inhalation in alleviating sleep problems was analyzed on a national scale; Korea (ES(g) = 0.724; P < .01) and other countries (ES(g) = 0.470, P < .01). A statistically significant difference (Q(df) = 7.766, P < .01) was observed. This was also observed in the SR analysis however the studies of aroma inhalation methods for improvement of sleep disorders or sleep problems were statistically significant compared with other countries. This indicates that in Korea, there is an active study of the effect of aroma inhalation on sleep disorders and sleep problems, and as well as an interest in their efficacy. The results are shown in Table 5.
3.8. Additional analysis
3.8.1. A regression analysis of the main effects and sub-effects of the aroma inhalation period
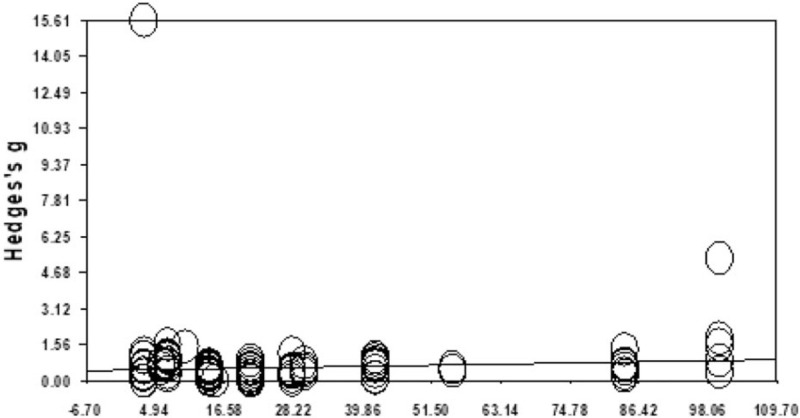
For each study, the effect size was analyzed according to the total number of sessions and was reanalyzed after the number of aroma inhalation sessions was coded as a continuous variable. As a result, the slope (β=) in the main effect size (0.00367, P < .01) was statistically significant (Intercept: 0.50136, P < .01) (τ = 0.13179, P < .01). These results show that the effect increases as the total number of sessions increases. In addition, the slope (β=) in the regression analysis of the size of the negative effects (0.00405, P = .01) and intercept (0.47506, P < .01) was statistically significant (τ = 0.24879; P < .01). This shows that the impact of the negative effects also increased as the total number of sessions increased. The regression results for assembly acquisition are the same as those outlined in Table 11 and Figs. 6 and 7.
Table 11.
A regression analysis of the main effects and sub-effects of the aroma inhalation period.
| SE | –95% CI | +95% CI | Z | τ2 | ||
| β | 0.00367 | 0.00103 | 0.00166 | 0.00568 | 3.57951 | 0.13179∗∗ |
| Intercept | 0.50136 | 0.04030 | 0.42237 | 0.58035 | 12.44002 | |
| β | 0.00405 | 0.00119 | 0.00173 | 0.00638 | 3.41241 | 0.24879∗∗ |
| Intercept | 0.47506 | 0.04471 | 0.38743 | 0.56269 | 10.62532 |
Figure 7.
The regression analysis of aroma therapy program according to years about for the slope of secondary outcome.
4. Discussion
Sleep disorders, including insomnia, are one of the most common diseases that affect people in the current modern society.[54,55] Persistent sleep deprivation leads to the consumption of sleep inducers and sleeping pills.[56,57] However, some of these drugs tend to lead to overdose and addiction, and the sleep symptoms from the drugs persist can until the next day, impacting daily life activities.[8] As a result, discussions on various alternative treatments such as aromatherapy have recently gained attention.[21] When the aroma is inhaled, the aroma molecules enter the olfactory epithelium through the nasal roof and stimulate the olfactory neurons. This leads to the secretion of hormones in the pituitary gland as well as peptides.[17] In particular, endorphin, which is one of the secreted peptides, is effective for treating sleep disorders caused by depression and anxiety, and in reducing pain and chronic stress.[58]
This study conducted a systematic literature review and meta-analysis to assess the clinical efficacy of aroma inhalation therapy in the treatment of sleep problems in patients diagnosed with insomnia, using published reports until June 2019. Previous studies that analyzed the effects of aroma on sleep problems were mostly conducted with massage therapy in parallel.[3] However, massage therapy requires help from someone else and there is a limit on it being performed alone.[59] Therefore, this study analyzed studies that assessed the aroma inhalation therapy as the sole manner for reducing sleep problems without much effort and help from anyone else.
The results are as follows: first, lavender was used as the aromatic oil in most of the studies. In both types of studies that used single aromatic oil and mixed oils, lavender was used most widely used. As reported by studies,[60,61] lavender makes the body feel heavy and provides a sense of stability, also, because of its natural sedation, lavender balm is an example of Western folk medicine that solves the problem of insomnia using a pillow filled with lavender, which may be the reason for its usage in most studies.
Additionally, the quality assessment of studies showed that there was a high risk for performance and selection bias. This was because specific descriptions of research subject assignment and randomization were not described in the studies. Further studies to correct for these biases are necessary. Moreover, unclear risk of detection bias was observed; however, there was no specific report on the blinding of outcome assessment. Thus, as mentioned in previous studies, outcome assessment must be conducted carefully on studies regarding aroma.[17] Second, the meta-analysis results are as follows. No statistically significant publication bias was observed in the studies. However, lavender was used in most studies, as seen in the systematic review results. This suggests that lavender may be the preferred aroma oil for sleep; however, there may be differences in the commercially available aroma.[62] Therefore, qualitative research on aromatherapists is recommended.
Analysis of effect size showed that the effect size of aroma inhalation therapy in primary and secondary outcomes was greater than the medium effect size, which indicates significant outcomes. Additional analysis was performed to assess the difference in effects by comparing the single and complex mixed aromas. As a result, the effects of a single aroma were greater than those of the mixed aroma. This finding is consistent with previous reports,[63] indicating that a single aroma is more effective for treating sleep problems. Moreover, the effects of aroma inhalation were greater in those experiencing sleep disorders compared with those that complained of general sleep problems. This finding demonstrates that aroma inhalation therapy may play a role as a complementary and alternative method. As a result, it was estimated that aroma inhalation therapy would be effective not only for sleep disorders but also for patients suffering from various psycho-emotional disorders and severe diseases such as cancer, in the same context as stated in previous studies.[64–66] This study aimed to identify significantly greater effects among aroma inhalation time and frequency, and the following are the results of the analysis of aroma inhalation methods. It was observed that the effects were the greatest before falling asleep and that there was no difference in the frequency of aroma inhalation. Thus, it is recommended that lavender oil be used for direct inhalation before sleep to solve sleep problems in the future.
The limitations of the current study are as follows. First, this study was conducted on papers published until June 2019, and studies published in 2020 were not included. This was done to analyze the results of 10 years. Therefore, a meta-analysis including papers published from late 2019 to the present of 2020 is recommended. Second, the method was limited to the inhalation of aroma oils, and methods such as massage were excluded. This was to help those experiencing sleep problems find an effective self-method that is not restricted by time and place. Therefore, future studies on the analysis of various intervention methods using aroma in addition to inhalation methods are recommended. Third, this study was only conducted on aroma oils and therefore a comparative advantage analysis could not be performed. Future studies that can conduct network meta-analysis for comparative advantage analysis are recommended. Fourth, lavender aroma oil was used in most of the selected studies. It is highly likely that aroma experts and researchers judged that the unique scent of lavender to be optimal for providing mental and physical stability related to sleep. However, the specific reason for the use of lavender could not be addressed in the current study. Therefore, further qualitative studies on the selection of lavender oil are necessary. Nonetheless, the findings of this study may be used as basic data to create a program that will help reduce sleep problems using aroma oils in the future.
5. Conclusion
The quality assessment of studies demonstrated a high risk of performance bias and selection bias. Unclear risk of detection bias was observed; however, there was no specific report on blinding of assessment outcomes. Lavender was the most used aroma oil related to sleep. The intervention method was mainly direct inhalation and secondary outcomes such as stress, anxiety, and depression were evaluated. Meta-analysis showed that the effects of aroma inhalation therapy were significant in mediating sleep problems. Additionally, the evaluation of secondary outcomes showed that it had a significant effect size in reducing the stress emotion, anxiety, and depression. In detail, aroma inhalation therapy with single oil was more beneficial before going to sleep for insomnia patients rather than those with general sleep problems. Finally, primary and secondary outcome analyses demonstrated that the effects increased significantly as the number of therapy sessions increased.
Author contributions
Conceptualization: Moon Joo Cheong.
Data curation: Moon Joo Cheong, Hyung Won Kang.
Formal analysis: Moon Joo Cheong.
Investigation: Moon Joo Cheong.
Project administration: Moon Joo Cheong, Hyung Won Kang.
Resources: Moon Joo Cheong, Hyung Won Kang.
Supervision: Moon Joo Cheong, Hyung Won Kang.
Writing – original draft: Moon Joo Cheong, Hyung Won Kang.
Writing – review & editing: Moon Joo Cheong, Hyung Won Kang, Sungchul Kim, Jee Su Kim, Byeonghyeon Jeon, Hyeryun Lee, Yu Ra Lee, Yeoung-Su Lyu.
Footnotes
Abbreviations: Actigraphy = activity recorder, AMED = Allied and Complementary Medicine Database, BDI = Beck Depression Inventory, CENTRAL = Cochrane Central Register of Controlled Trials, CINAHL = Cumulative Index to Nursing and Allied Health Literature, DSM-5 = Diagnostic and Statistical Manual of Mental Disorders-5, ES = effect sizes, FSI = fatigue symptom inventory, HAMD = Hamilton Depression Scale, ISI = insomnia severity index, KCI = Korea Citation Index, KISS = Korean studies Information Service System, KMbase = Korean Medical Database, MEDLINE = Medical Literature Analysis and Retrieval System Online, or MEDLARS Online, meta-ANOVA = meta-analysis of variance, OASIS = Oriental Medicine Advanced Searching Integrated System, PICOS = Participants, Intervention, Control, Outcomes & Study Design, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-analysis, PSG = polysomnography, PSQI = Pittsburgh Sleep Quality Index, PSS = perceived stress scale, RCT = randomized controlled trial, RISS = research information service system, SE = sleep efficiency, SOL = sleep onset latency, SSQ = Stanford Sleep Questionnaire, STAI = state-trait anxiety inventory, TST = total sleep time, WASO = wake-up sleep on time, WHIIRS = Women's Health Initiative Insomnia Rating Scale.
How to cite this article: Cheong MJ, Kim S, Kim JS, Lee H, Lyu YS, Lee YR, Jeon B, Kang HW. A systematic literature review and meta-analysis of the clinical effects of aroma inhalation therapy on sleep problems. Medicine. 2021;100:9(e24652).
Consent for publication: Not applicable.
Availability of data and material: Not applicable.
This research was funded by the Ministry of Health and Welfare and was supported by the Korea Health Industry Promotion Agency's Health and Medical Technology R&D Project (Grant number: HI20C1951). The funding source will have no input in the interpretation or publication of the study results.
The authors declare that they have no conflict of interest.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
DSM-5 = Diagnostic and Statistical Manual of Mental Disorders-5, RCT = randomized controlled trial.
CI = confidence interval; ES = effect sizes; K = the number of effect sizes; P = P-value; QB = difference verification between groups; SE = standard error.
P < .05.
P < .01.
CI = confidential interval; ES = effect sizes; K = the number of effect sizes; QB = difference verification between groups; SE = standard error.
CI = confidential interval; ES = effect sizes; K = the number of effect sizes; QB = difference verification between groups; SE = standard error.
∗P < .05.
P < .01.
CI = confidence interval; ES = effect sizes; K = the number of effect sizes; P = P-value; QB = difference verification between groups; SE = standard error.
CI = confidence interval; ES = effect sizes; K = the number of effect sizes, P = P-value, QB = difference verification between groups, SE = standard error.
P < .05.
P < .01.
CI = confidence interval two dependent; ES = effect sizes; K = the number of effect sizes, QB = difference verification between groups, SE = standard error.
P < .05.
∗∗P < .01.
CI = confidence interval; SE = standard error; Z = value of standard normal deviate.
∗P < .05.
P < .01.
∗∗∗P < .001.
References
- [1].Kyle SD, Morgan K, Espie CA. Insomnia and health-related quality of life. Sleep Med Rev 2010;14:69–82. [DOI] [PubMed] [Google Scholar]
- [2].Smagula SF, Stone KL, Fabio A, et al. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev 2016;25:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hwang E, Shin S. The effects of aromatherapy on sleep improvement: a systematic literature review and meta-analysis. J Altern Complement Med 2015;21:61–8. [DOI] [PubMed] [Google Scholar]
- [4].Wanniarachige D, Murphy S, Titiloye A, et al. GP172 Should healthcare professionals routinely recommend a commercially available sleep movement monitor for babies? Arch Dis Child 2019;104:A99–100. [Google Scholar]
- [5].Chan WS, Levsen MP, McCrae CS. A meta-analysis of associations between obesity and insomnia diagnosis and symptoms. Sleep Med Rev 2018;40:170–82. [DOI] [PubMed] [Google Scholar]
- [6].Herron K, Farquharson L, Wroe A, et al. Development and evaluation of a cognitive behavioural intervention for chronic post-stroke insomnia. Behav Cogn Psychother 2018;46:641–60. [DOI] [PubMed] [Google Scholar]
- [7].Galinsky AM, Ward BW, Joestl SS, et al. Sleep duration, sleep quality, and sexual orientation: findings from the 2013–2015 National Health Interview Survey. Sleep Health 2018;4:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mendelson WB. A review of the evidence for the efficacy and safety of trazodone in insomnia. J Clin Psychiatry 2005;66:469–76. [DOI] [PubMed] [Google Scholar]
- [9].Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: a systematic review. Explore (NY) 2007;3:585–91. [DOI] [PubMed] [Google Scholar]
- [10].Lee JT, Lee KJ, Park JB, et al. The Relations between Shiftwork and Sleep Disturbance in a University Hospital Nurses. Korean J Occup Environ Med 2007;19:223–30. [Google Scholar]
- [11].Yang EK, Choi IR, Kim SM. The impact of sleep disorder and job stress on turnover intention of shift-working nurses. Korean J Stress Res 2017;25:255–64. [Google Scholar]
- [12].Kim KS. Effects of subway workers’ night working on metabolic syndrome. Ann Occup Environ Med 2016;11:413–4. [Google Scholar]
- [13].Lee H, Lim YJ, Jung HY, et al. Sleep disturbance, physical activity and health related quality of life in patients with chronic obstructive pulmonary disease. J Korean Gerontol Soc 2011;31:607–21. [Google Scholar]
- [14].Park YJ, Kim YS. A convergence study of depression, health-related quality of life and sleep disturbance according to the level of physical activity of hemodialysis patients. J Digit Converg 2018;16:345–55. [Google Scholar]
- [15].Jung J, Lee EH, Yang YJ, et al. Sleep pattern and factors causing sleep disturbance in adolescents with cancer before and after hospital admission. Asian Oncol Nurs 2017;17:143–50. [Google Scholar]
- [16].Kim SJ, Na H. A study of the relationships between compassion fatigue, compassion satisfaction, depression, anxiety, and sleep disorders among oncology nurses. Asian Oncol Nurs 2017;17:116–23. [Google Scholar]
- [17].Koo BS, Park KS, Ha JH, et al. Inhibitory effects of the fragrance inhalation of essential oil from Acorus gramineus on central nervous system. Biol Pharm Bull 2003;26:978–82. [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement [published correction appears in Int J Surg. 2010;8(8):658]. Int J Surg 2010;8:336–41. [DOI] [PubMed] [Google Scholar]
- [19].Shojania KG, Sampson M, Ansari MT, et al. How quickly do systematic reviews go out of date? A survival analysis. Ann Intern Med 2007;147:224–33. [DOI] [PubMed] [Google Scholar]
- [20].Lichstein KL, Stone KC, Donaldson J, et al. Actigraphy validation with insomnia. Sleep 2006;29:232–9. [PubMed] [Google Scholar]
- [21].Roland PS, Rosenfeld RM, Brooks LJ, et al. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg 2011;145: 1 suppl: S1–5. [DOI] [PubMed] [Google Scholar]
- [22].Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012;35:287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Haythornthwaite JA, Hegel MT, Kerns RD. Development of a sleep diary for chronic pain patients. J Pain Symptom Manage 1991;6:65–72. [DOI] [PubMed] [Google Scholar]
- [24].MacFarlane JG, Cleghorn JM, Brown GM, et al. The effects of exogenous melatonin on the total sleep time and daytime alertness of chronic insomniacs: a preliminary study. Biol Psychiatry 1991;30:371–6. [DOI] [PubMed] [Google Scholar]
- [25].Buysse DJ, Ancoli-Israel S, Edinger JD, et al. Recommendations for a standard research assessment of insomnia [published correction appears in Sleep. 2006 Nov 1;29(11):1380]. Sleep 2006;29:1155–73. [DOI] [PubMed] [Google Scholar]
- [26].Haynes SN, Adams A, Franzen M. The effects of presleep stress on sleep-onset insomnia. J Abnorm Psychol 1981;90:601–6. [DOI] [PubMed] [Google Scholar]
- [27].Gross RT, Borkovec TD. Effects of a cognitive intrusion manipulation on the sleep-onset latency of good sleepers. Behav Ther 1982;13:112–6. [Google Scholar]
- [28].Wilson DL, Barnes M, Ellett L, et al. Decreased sleep efficiency, increased wake after sleep onset and increased cortical arousals in late pregnancy. Aust N Z J Obstet Gynaecol 2011;51:38–46. [DOI] [PubMed] [Google Scholar]
- [29].Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- [30].Monk TH, Reynolds CF, Kupfer DJ, et al. The Pittsburgh sleep diary. J Sleep Res 1994;3:111–20. [PubMed] [Google Scholar]
- [31].Kim JH. Types of mindfulness meditation and their implications for cognitive behavioral therapy. Cogn Behav Pract 2004;4:27–44. [Google Scholar]
- [32].Hays RD, Martin SA, Sesti AM, et al. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med 2005;6:41–4. [DOI] [PubMed] [Google Scholar]
- [33].Lee BK. The effects of mindfulness-based stress reduction (MBSR) program on pain and anxiety in cancer patients. Korean J Stress Res 2013;21:263–74. [Google Scholar]
- [34].Krouse HJ, Davis JE, Krouse JH. Immune mediators in allergic rhinitis and sleep. Otolaryngol Head Neck Surg 2002;126:607–13. [DOI] [PubMed] [Google Scholar]
- [35].Shahid A, Wilkinson K, Marcu S, Shapiro CM. Women's Health Initiative Insomnia Rating Scale (WHIIRS). S.T.O.P., T.H.A.T., One Hundred Other Sleep, Scales 2011;New York, NY: Springer, 403–404. [Google Scholar]
- [36].Oh JJ, Song MS, Kim SM. Development and validation of Korea sleep scale A. J Korean Acad Nurs 1998;28:563–72. [Google Scholar]
- [37].Bech P, Allerup P, Gram LF, et al. The Hamilton depression scale. Evaluation of objectivity using logistic models. Acta Psychiatr Scand 1981;63:290–9. [DOI] [PubMed] [Google Scholar]
- [38].Beck AT, Steer RA, Brown GK, et al. Beck depression inventory-II. San Antonio 1996;78:490–8. [Google Scholar]
- [39].Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Measuring Stress 1994;10:1–2. [Google Scholar]
- [40].Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span J Psychol 2006;9:86–93. [DOI] [PubMed] [Google Scholar]
- [41].Spielberger CD. State-trait anxiety inventory. The Corsini Encyclopedia of Psychology 2010;1–11. [Google Scholar]
- [42].Servaes P, Verhagen C, Bleijenberg G. Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer 2002;38:27–43. [DOI] [PubMed] [Google Scholar]
- [43].Lillehei AS, Halcon LL. A systematic review of the effect of inhaled essential oils on sleep. J Altern Complement Med 2014;20:441–51. [DOI] [PubMed] [Google Scholar]
- [44].John Wiley & Sons; 2019;Higgins JP, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 25–32. [Google Scholar]
- [45].Academic Press, Hedges LV, Olkin I. Statistical Methods for Meta-analysis. 2014. [Google Scholar]
- [46].Snyder-Halpern R, Verran JA. Instrumentation to describe subjective sleep characteristics in healthy subjects. Res Nurs Health 1987;10:155–63. [DOI] [PubMed] [Google Scholar]
- [47].Oxford University Press, Littell JH, Corcoran J, Pillai V. Systematic Reviews and Meta-analysis. 2008. [Google Scholar]
- [48].Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. [DOI] [PubMed] [Google Scholar]
- [49].Higgins JP, Green S. Cochrane handbook for systematic reviews. The Cochrane Collaboration, vol. 5. West Sussex, England: John Wiley & Sons Ltd.; 2008. [Google Scholar]
- [50].Rosenthal R, Rubin DB. Statistical analysis: summarizing evidence versus establishing facts. Psychol Bull 1985;97:527–9. [Google Scholar]
- [51].Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1988;Hillsdale, NJ: Lawrence Earlbam Associates, 77–83. [Google Scholar]
- [52].Sage, Wolf FM. Meta-analysis: Quantitative Methods for Research Synthesis. 1986. [Google Scholar]
- [53].Rosenthal R, Cooper H, Hedges L. Parametric measures of effect size. Handb Res Synth 1994;621:231–44. [Google Scholar]
- [54].Drake CL, Roehrs T, Roth T. Insomnia causes, consequences, and therapeutics: an overview. Depress Anxiety 2003;18:163–76. [DOI] [PubMed] [Google Scholar]
- [55].Wang MY, Wang SY, Tsai PS. Cognitive behavioural therapy for primary insomnia: a systematic review. J Adv Nurs 2005;50:553–64. [DOI] [PubMed] [Google Scholar]
- [56].Smolensky MH, Di Milia L, Ohayon MM, et al. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev 2011;43:533–48. [DOI] [PubMed] [Google Scholar]
- [57].Kamel NS, Gammack JK. Insomnia in the elderly: cause, approach, and treatment. Am J Med 2006;119:463–9. [DOI] [PubMed] [Google Scholar]
- [58].Academic Press, Martin RA, Ford T. The Psychology of Humor: An Integrative Approach. 2018;25–26. [Google Scholar]
- [59].Yoshiyama K, Arita H, Suzuki J. The effect of aroma hand massage therapy for people with dementia. J Altern Complement Med 2015;21:759–65. [DOI] [PubMed] [Google Scholar]
- [60].Buchbauer G, Jirovetz L, Jäger W, et al. Aromatherapy: evidence for sedative effects of the essential oil of lavender after inhalation. Z Naturforsch C J Biosci 1991;46:1067–72. [DOI] [PubMed] [Google Scholar]
- [61].Cavanagh HM, Wilkinson JM. Lavender essential oil: a review. Aust Infect Control 2005;10:35–7. [Google Scholar]
- [62].Toda M, Morimoto K. Evaluation of effects of lavender and peppermint aromatherapy using sensitive salivary endocrinological stress markers. Stress Health 2011;27:430–5. [Google Scholar]
- [63].Şentürk A, Tekinsoy Kartin P. The effect of lavender oil application via inhalation pathway on hemodialysis patients’ anxiety level and sleep quality. Holist Nurs Pract 2018;32:324–35. [DOI] [PubMed] [Google Scholar]
- [64].Bilia AR, Guccione C, Isacchi B, et al. Essential oils loaded in nanosystems: a developing strategy for a successful therapeutic approach. Evid Based Complement Alternat Med 2014;2014:651593.1–14. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [65].Elsevier Health Sciences, Tisserand R, Young R. Essential Oil Safety-e-book: A Guide for Health Care Professionals. 2013;20–75. [Google Scholar]
- [66].Cheong MJ, Lee GE, Kang HW, et al. Clinical effects of mindfulness meditation and cognitive behavioral therapy standardized for insomnia: a protocol for a systematic review and meta-analysis. Medicine (Madr) 2018;97:e13499.1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


