Abstract
Purpose
Among patients with chronic obstructive pulmonary disease (COPD), adherence to inhaled medication leads to fewer exacerbations and improved health status. The goal of the present study was to evaluate the effects of medication reminders via the BreatheMate device on adherence in patients with COPD.
Patients and Methods
A 6-month, phase 4, randomized, multicenter, open-label US study (NCT02864342) enrolled 138 patients aged ≥40 years with moderate to very severe COPD and ≥10 pack-year smoking history. Patients in the intervention (n = 68) and control (n = 70) groups received the BreatheMate device, smartphone application, and vouchers to redeem pressurized metered-dose inhalers (pMDIs) for the prescribed 2 puffs of budesonide/formoterol 160/4.5 μg twice daily. The intervention group also received twice-daily electronic reminders to take budesonide/formoterol. The primary endpoint was the mean number of sets of adherent puffs/day (4 puffs: 2 puffs within 60 minutes, twice daily) over 6 months. Secondary endpoints included adherence by three 60-day intervals, usage days, prescription refills, and Clinical COPD Questionnaire (CCQ) score. Study enrollment terminated early due to issues with inconsistent syncing.
Results
A higher mean proportion of adherent days (77.6% vs 60.2%; P <0.001) and sets of adherent puffs/day (1.61 vs 1.33; P <0.001) were recorded for the intervention group versus the control group. Intervention group adherence was higher than that of the control group for each 60-day interval (P <0.001); the intervention group was 3.07 (95% confidence interval: 1.49–6.52) times more likely than the control group to be adherent for ≥80% of study days. Overuse (>2 sets of 2 puffs/day), underuse (<2 sets of 2 puffs/day), and no use days were lower in the intervention group versus control (P <0.05). Patients aged ≥65 years had higher adherence (P <0.001).
Conclusion
Medication reminders through the BreatheMate device and application produced greater adherence to inhaled therapy in patients with COPD.
Keywords: chronic obstructive pulmonary disease, telemedicine, adherence, pressurized metered-dose inhaler
Plain Language Summary
For patients with chronic obstructive pulmonary disease (COPD), studies have shown that adherence to an inhaled medication regimen (consistently taking inhaled medications as prescribed) can lead to fewer exacerbations and better health status. The goal of this study was to determine how twice-daily medication reminders sent to patients through a smartphone application affected patients’ adherence to a prescribed, twice-daily inhaled medication. To accomplish this objective, the study used a smartphone application and a Bluetooth device, which recorded each time patients actuated their inhaler. The results from the group of patients who received medication reminders (intervention group) were compared to results from a control group of patients who also used the Bluetooth device to record their medication use but did not receive twice-daily reminders. The results of the study show that patients who received medication reminders were more likely to use their medication as prescribed than patients who did not receive reminders. These findings suggest that receiving daily medication reminders could help to improve adherence among patients with COPD who use a daily inhaled medication.
Introduction
Despite the availability of efficacious therapy, studies suggest nonadherence to treatment (eg, no use or underuse) is high among patients with chronic obstructive pulmonary disease (COPD).1 Adherence to inhaled medications ranges from 47% to 57%2 and may be less than 40%, depending on the prescribed dosing regimen.3 It has also been suggested that treatment adherence in COPD is lower than adherence for treatments of other conditions.1,4 Adherence is especially important in COPD, as poor adherence is associated with a greater frequency of exacerbations, increased morbidity and mortality, higher health care costs, and greater economic burden.3,5 Reasons cited for lower adherence in COPD include patient age,3 variations in daily symptoms,6 confusion with daily dosing schedules,6 and patient understanding of treatment.7 However, it is noteworthy that the method by which medication adherence is measured (ie, direct vs indirect measurements) can impact the accuracy of the results and thus, indirect methods of assessing adherence may be an additional factor in studies that report lower adherence.8 Direct, objective measures of adherence may provide further insight on adherence to inhaled therapy in patients with COPD.
As a result of the negative impacts of poor adherence, methods to improve patient adherence to inhaled therapy, such as use of electronic medication reminders, are being explored. Indeed, results from a study of electronic reminders in patients with asthma show significant improvements in inhaled corticosteroid (ICS) adherence for patients receiving a daily audible reminder at patient-chosen, predetermined times, compared with a control group who did not receive reminders.9 A separate study of medication reminders in children with asthma also reported significant improvements in adherence.10 “Connected devices”—for example, a medical device that wraps around the patient’s pressurized metered-dose inhaler (pMDI) and, with patient consent, transmits medical information to a health care provider or clinical study coordinator via connection to a smartphone or wireless internet signal—are also being explored as potential methods to improve adherence to inhaled therapy.11 Although studies of medication reminders with connected devices in patients with asthma have been reported, few studies in patients with COPD have been published.12 Given the reports of low adherence and the wide range of studies indicating significant negative long-term impacts of low adherence on disease status and health-related quality of life in COPD, patients with COPD, in particular, could potentially benefit from connected devices with daily reminders that improve medication adherence.
The BreatheMate Bluetooth monitoring device is a patient support tool designed to monitor twice-daily budesonide/formoterol use by attaching to the inhaler and automatically detecting and recording the date and time of each dispersal of medication. This device pairs with a smartphone application, which then transmits the medication usage data to the study site. The present study is the first study conducted of the BreatheMate Bluetooth monitoring device; the objective of this study was to measure the effects of electronic reminders on treatment adherence in patients diagnosed with COPD.
Patients and Methods
This study was a 6-month, phase 4, multicenter, open-label, controlled, randomized study (ClinicalTrials.gov: NCT02864342) conducted at eight research sites within the United States. The study was conducted in compliance with the principles of the Declaration of Helsinki and Good Clinical Practice.
Patients
Target enrollment for this study was 414 patients, with an expected dropout rate of 15%, yielding 352 evaluable patients (80% power) for the primary endpoint. The target enrollment of 414 patients was not reached as a result of early termination of study enrollment due to cellular connectivity and syncing issues related to the study-issued smartphones, which prevented adequate safety monitoring of patients. The study enrolled patients aged ≥40 years with a ≥10 pack-year smoking history and COPD, confirmed by spirometry-verified post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity ratio <0.70 diagnosed within the preceding 3 years. Patients were required to have moderate to very severe COPD, as indicated by their most recent post-bronchodilator FEV1 <80% of predicted. Patients were also required to have been on an inhaled corticosteroid/long-acting beta-2 agonist (ICS/LABA) combination therapy approved for COPD for ≥3 months prior to screening, and already using, or be willing to switch to, a budesonide/formoterol (160/4.5 µg) pMDI. Budesonide/formoterol is a combination medicine consisting of an ICS (budesonide) and a LABA (formoterol) administered by a pMDI; prescribed use is 2 puffs administered twice daily.13 All participants provided written informed consent prior to participation in this study. Participants also received fair compensation for participation in this study.
Additional details regarding study eligibility are included in the Supplemental Methods.
Randomization and Study Arms
Patients who met all inclusion criteria and none of the exclusion criteria were randomly assigned 1:1 to the intervention group or the control group via unique randomization codes generated via interactive web response systems/interactive voice response systems, which were built and managed by a third party. There was no stratification by site or any other parameter, and allocation of patients to treatment groups was unblinded. Both groups received a study-issued smartphone device with a connection to the study databases. The control group received their established therapy and the BreatheMate medication monitoring device, whereas the intervention group received their established therapy and a BreatheMate medication monitoring device that provided twice-daily (once in the morning and once in the evening) auditory and visual reminders (beeps and flashes) via the BreatheMate device and a supportive application on the smartphone device. This smartphone application prompted patients in the intervention arm with reminders of the importance of taking budesonide/formoterol (preemptive as well as missed dose reminders), weekly reminders to complete the Clinical COPD Questionnaire (CCQ), and monthly reminders to obtain budesonide/formoterol pMDI refills and attach them to the BreatheMate device.
Study Procedures
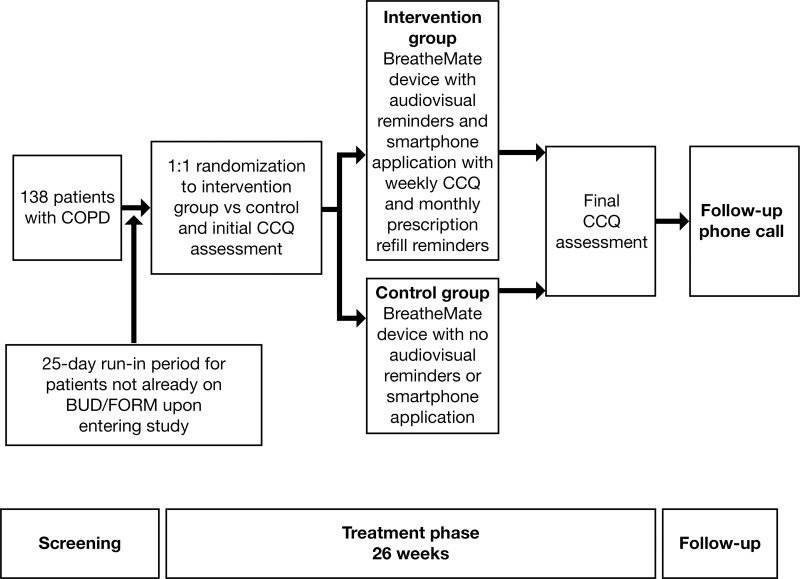
Patients entering the study on a stable dose of budesonide/formoterol were enrolled at Visit 1, which was followed by a 26-week treatment period (Figure 1). Patients who converted to budesonide/formoterol entered a 25-day run-in period and were randomized at Visit 2, followed by the 26-week treatment period.
Figure 1.
Study flow chart.
Note: BreatheMate patient enrollment, treatment, and follow-up.
Abbreviations: BUD/FORM, budesonide/formoterol; CCQ, Clinical COPD Questionnaire; COPD, chronic obstructive pulmonary disease.
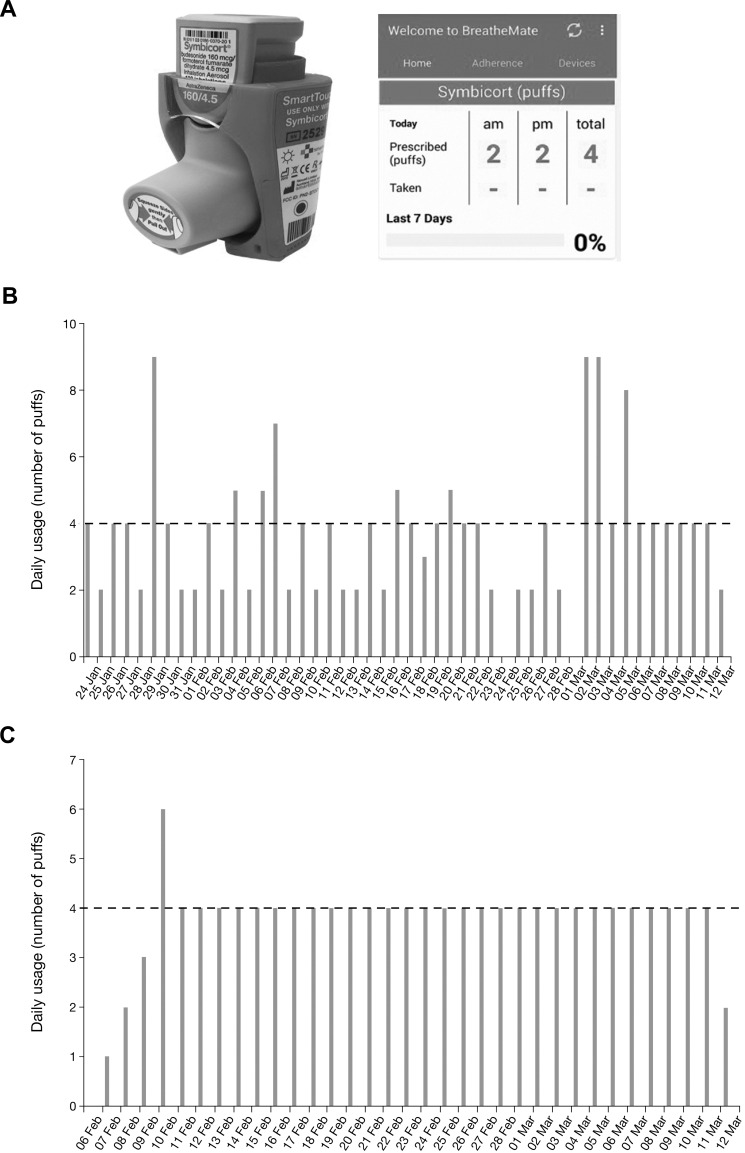
All patients received information on proper technique for medication inhalation, proper dosing (2 puffs of budesonide/formoterol 160/4.5 µg pMDI, twice daily), vouchers for the budesonide/formoterol pMDI to be redeemed at a pharmacy, and the BreatheMate medication monitoring device with instructions on inserting the budesonide/formoterol pMDI into the device. The medication monitoring system consisted of the BreatheMate Bluetooth device and the study-supplied smartphone with the BreatheMate application pre-loaded (Figure 2A). The smartphone application recorded the date and time of each actuation of the inhaler to measure treatment adherence over time (Figure 2B and C).
Figure 2.
BreatheMate, smartphone application, and example patient data.
Notes: (A) Image of BreatheMate device attached to pMDI and screenshot of the smartphone application. (B) Data recorded via the BreatheMate device show representative results for a patient in the control group (note that the dotted line represents the prescribed number of puffs/day prescribed for appropriate use). (C) Data recorded via the BreatheMate device show representative results for a patient in the intervention group, who received daily reminders to take their medication (note that the dotted line represents the prescribed number of puffs/day prescribed for appropriate use).
Abbreviation: pMDI, pressurized metered-dose inhaler.
All patients received on-site instruction on how to use the device during randomization. All patients received a telephone call 4 days after randomization to resolve any issues with the BreatheMate device or smartphone application. Two weeks after randomization, each patient’s results were checked for technical issues (ie, no data received) by the study coordinator. All patients received a phone call 90 days after randomization to assess the incidence of adverse events (AEs) and concomitant medication usage. Patients returned to the clinic at Week 26 for Visit 3 (end-of-treatment visit). A final follow-up call occurred 30 days after Visit 3 to assess the incidence of AEs and concomitant medication usage since the end-of-treatment visit. Patients were also provided with a helpline phone number in case of questions regarding the BreatheMate device or smartphone application.
Medication use information was recorded via the BreatheMate Bluetooth device and collected using the BreatheMate service. Study days in which a patient did not take budesonide/formoterol were termed “no use”, study days in which a patient took between 1 and 3 puffs were termed “underuse”, and study days in which a patient took ≥5 puffs were termed “overuse”. Overuse alerts (when patients used >10 puffs/day) were monitored and intervened upon with direct patient contact from the study site investigator. Medication use data were accessible to study investigators and study coordinators through a secure BreatheMate web portal.
COPD symptom control was measured using the CCQ, which is a 10-item questionnaire evaluating a patient’s COPD frequency and severity, with responses ranging from 0 to 6. Items on the CCQ are grouped into three domains: COPD symptoms, patient functional state, and patient mental state.14 To calculate the mean total CCQ score, individual questions were equally weighted, summed, and divided by 10 (number of CCQ items). CCQ results were collected upon randomization (Visit 1 or 2) via the smartphone application for those in the intervention arm and via pencil and paper for those in the control arm. CCQ results were collected at the end of treatment (Visit 3) for both the control and intervention groups using the pencil and paper questionnaire. For patients in the intervention group, the CCQ was also completed on a weekly basis via the BreatheMate app.
Outcomes
The primary outcome measure was the impact of medication reminders on budesonide/formoterol adherence, measured as the mean number of adherent sets of puffs/day for 6 months in patients with COPD: given that budesonide/formoterol is prescribed as a twice-daily regimen of 2 puffs, with one set of 2 puffs taken in the morning and the second set of 2 puffs taken in the evening, an adherent set was defined as 2 puffs taken within 60 minutes of each other.
Secondary endpoints included the mean number of sets of adherent puffs/day by 2-month intervals, as well as the mean total number and proportion of adherent days by patient and the mean number of prescription refills over the 26-week study period. An adherent day was defined as two adherent sets of 2 puffs occurring within a single calendar day (recorded as a value of 2 for an adherent day, 0 otherwise). As defined a priori, patients with ≥80% adherent days during their device time on study were defined as being adherent. Secondary endpoints also included mean CCQ scores at baseline and end of treatment, along with the mean change in scores over the study period, and mean CCQ scores (both total and stratified by domain) at each 2-month study interval for the intervention group.
A post hoc analysis was conducted to compare adherence in patients aged <65 and ≥65 years. A subsequent analysis also compared adherence in patients with and without a major protocol violation during the device time on study.
Safety
Safety was evaluated based on reported AEs and serious AEs.
Patient and Provider Satisfaction
Patient satisfaction with the BreatheMate device and smartphone application for those in the intervention arm was evaluated with a survey concerning ease of use, appearance, and device feel. Study investigators and coordinators were surveyed to assess the BreatheMate web portal’s ease of use, design, and accessibility, as well as their patients’ medication adherence and refills.
Statistical Analyses
The full analysis set (FAS) included all patients who were screened, randomized, and inhaled ≥1 dose of the study budesonide/formoterol. The per-protocol (PP) analysis set consisted of all patients who met all eligibility criteria and were screened, randomized, and took ≥1 inhalation of study budesonide/formoterol, with ≥60 days of device time on study and without any major protocol deviations. The primary and secondary endpoints for this study were analyzed using both the FAS and the PP sets; missing values were not imputed. Comparisons of mean medication use and the effect of reminders (intervention group) on medication adherence were performed preliminarily using a t-test (mean number of sets of puffs/day) and then by analysis of covariance (ANCOVA; sets of puffs/day in the 60-day interval, mean and total adherent days, prescription refills, and subgroup analyses), as appropriate. Patient demographics, baseline characteristics, and CCQ scores were summarized with descriptive statistics; categorical variables were compared using a chi-squared test and continuous variables were compared with a t-test.
To identify potential covariates associated with adherence, univariate and multivariable logistic regressions were used to model the odds of patients having a proportion of adherent days ≥80% during device time on study. For multivariable logistic regressions, only covariates from the univariate models that reached a significance threshold ≤0.25 were added. Covariates from the multivariable model that reached a significance threshold ≤0.15 were used for all secondary outcome ANCOVA models.
Results
Patients
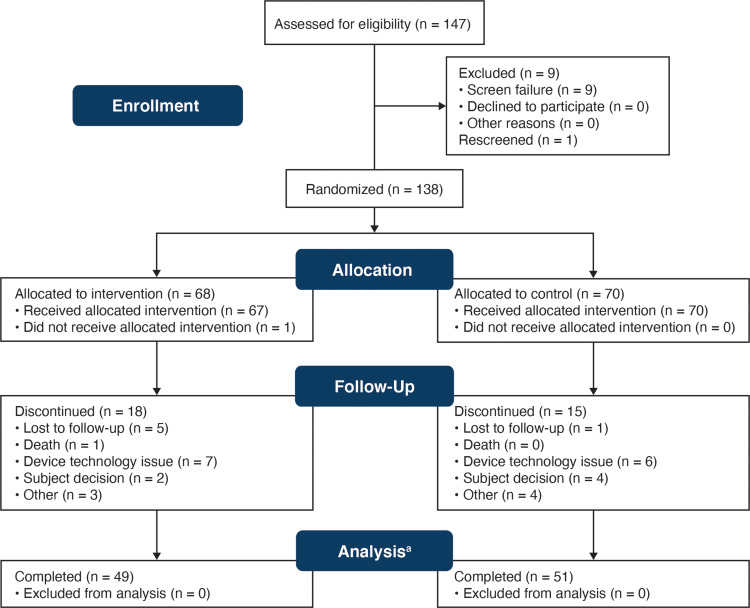
In total, 138 patients were enrolled in the study: 70 were randomized to the control arm (no reminders), and 68 were randomized to the intervention arm (daily auditory and visual medication reminders via smartphone). The FAS (n = 137) included all 70 patients in the control group and 67 patients in the intervention group (1 patient in the intervention group did not take any inhalations of budesonide/formoterol; Figure 3). Patient demographics and baseline CCQ scores for these groups are reported in Table 1. There were no significant differences in patient age, race, or sex between the two groups. However, the mean baseline total and domain CCQ scores (symptom, functional, and mental) were higher for the control group compared with the intervention group, indicating worse baseline COPD status.
Figure 3.
CONSORT flow diagram.
Note:aThe n = 100 patients who completed the study also comprised the per-protocol analysis set, which consisted of all patients who met all eligibility criteria and were screened, randomized, and took ≥1 inhalation of study budesonide/formoterol, with ≥60 days of device time on study and without any major protocol deviations.
Abbreviation: CONSORT, Consolidated Standards of Reporting Trials.
Table 1.
Patient Demographics
| Characteristics | Control (n = 70) | Intervention (n = 67) | P value |
|---|---|---|---|
| Age at enrollment (years) | |||
| Mean (SD) | 66.6 (8.21) | 66.7 (8.72) | 0.898 |
| Male, n (%) | 37 (52.9) | 40 (59.7) | 0.420 |
| Race, n (%) | |||
| White | 55 (78.6) | 53 (79.1) | 0.420 |
| Black | 11 (15.7) | 14 (20.9) | |
| Other | 4 (5.7) | 0 (0) | |
| Baseline CCQ scoresa | |||
| Total, mean (SD) | 2.8 (0.97) | 2.3 (0.91) | 0.002 |
| Symptom, mean (SD) | 3.0 (1.08) | 2.5 (1.20) | 0.021 |
| Functional, mean (SD) | 2.7 (1.37) | 2.3 (0.94) | 0.024 |
| Mental, mean (SD) | 2.4 (1.35) | 1.7 (1.26) | 0.003 |
| COPD severity | |||
| Moderate, n (%) | 22 (31.4) | 24 (35.8) | |
| Severe/very severe, n (%) | 48 (68.6) | 43 (64.2) | |
| Exacerbations (past 12 mo)b | |||
| Mean (SD) | 0.8 (1.63) | 0.7 (1.02) | |
| ≥1 Comorbidity, n (%) | 70 (100) | 67 (100) | |
| ≥1 Comedication, n (%) | 70 (100) | 67 (100) |
Notes: aBaseline CCQ scores were missing for four patients in the intervention group. bExacerbation history was missing for one patient in the control group.
Abbreviations: CCQ, Clinical COPD Questionnaire; COPD, chronic obstructive pulmonary disease; SD, standard deviation.
The control and intervention groups had comparable median patient time on the study device (5.89 and 5.92 months, respectively, for the FAS). Fifty-five (79%) patients in the control arm and 49 (72%) patients in the intervention arm completed the study. Fifty-one (51%) control patients and 49 (49%) intervention patients met the eligibility criteria, with no major protocol deviations and ≥60 days of device time, and thus were included in the PP analysis set (n = 100). Of all 137 patients in the FAS, there were major protocol deviations in 34 (25%) patients. Most major protocol deviations were related to eligibility and entry criteria.
Outcomes
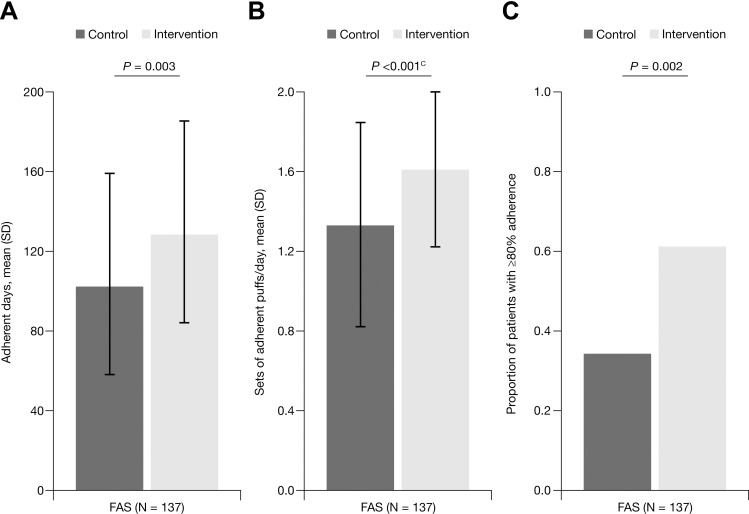
In the FAS, there was a significantly higher mean number of adherent sets of puffs/day for patients in the intervention group (1.61; standard deviation [SD], 0.389) compared with patients in the control group (1.33; SD, 0.509; P <0.001; Figure 4).
Figure 4.
Mean adherence to budesonide/formoterol during the study: FAS.
Notes: Budesonide/formoterol adherence among control and intervention group patients during the study, quantified as (A) the number of adherent daysa for device time on study, (B) the number of adherent setsb of puffs per day for device time on study, and (C) patients with ≥80% adherence for device time on study. aAn adherent day was defined as 2 puffs taken within 60 minutes of each other, occurring twice in a single calendar day. bAn adherent set of puffs was defined as 2 puffs taken within 60 minutes of each other. cIndicates the Satterthwaite t-statistic is reported.
Abbreviations: FAS, full analysis set; SD, standard deviation.
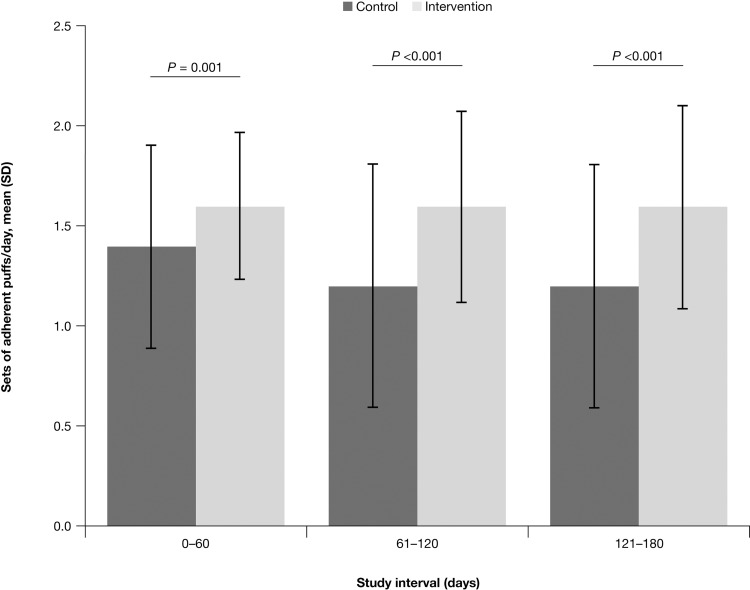
The mean number of adherent days was significantly higher for the intervention group (128.4; SD, 50.75) compared with the control group (102.3; SD, 50.76; P = 0.003), and a greater proportion of patients in the intervention group (61.2%) than in the control group (34.3%; P = 0.002) were ≥80% adherent during device time on study in the FAS (Figure 4). In addition, in the FAS, patients in the intervention group also had a significantly higher mean number of sets of adherent puffs/day than the control group for each of the three different 60-day study intervals (P <0.001; Figure 5). Furthermore, the mean number of sets of adherent puffs in the control group decreased over time after the first 60-day study interval. However, there were no significant decreases in the mean number of sets of adherent puffs among study intervals for the intervention group. Similar results were observed for the PP analysis set.
Figure 5.
Mean sets of adherent budesonide/formoterol puffs/day during each 60-day study interval: FAS.
Note: Budesonide/formoterol adherence among control and intervention group patients across three different 60-day study intervals.
Abbreviations: FAS, full analysis set; SD, standard deviation.
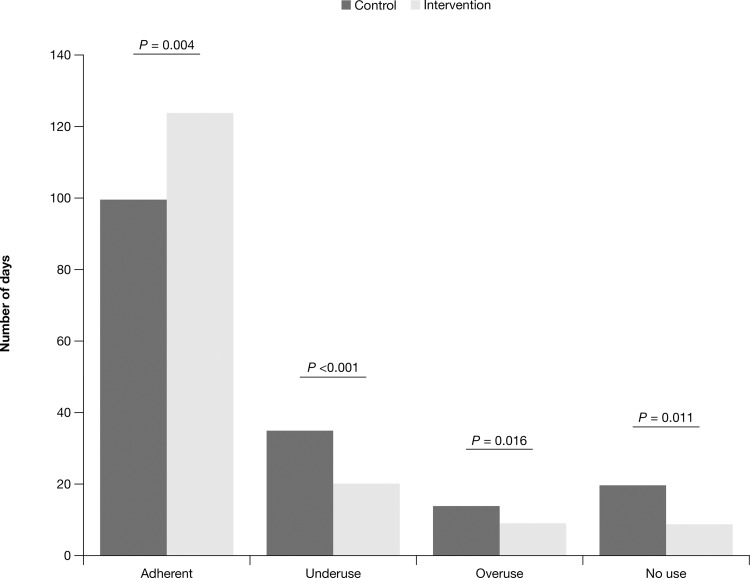
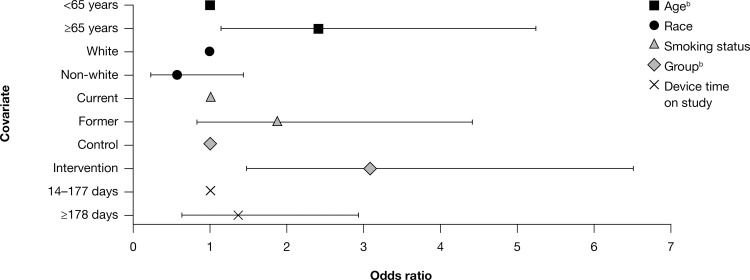
In the FAS, 79% of total patient days were adherent (two sets of 2 puffs in a day) for the intervention group compared with 61% of total patient days for the control group. Compared with the control group, the intervention group had a significantly greater number of adherent days and overall percentage of adherence (P <0.05; Figure 6). Furthermore, there was a significantly higher mean proportion of adherent days for patients in the intervention group compared with the control group (77.6% vs 60.2%, respectively; P <0.001). In the FAS, patients in the intervention group had 3.07 (95% confidence interval [CI], 1.49–6.52) times the odds of being adherent during their device time on study compared with the control group, after adjusting for smoking status, age, and race (P = 0.003; Figure 7). Patients aged ≥65 years in the FAS, without respect to the treatment group, had 2.42 (95% CI, 1.14–5.24) times the odds of being adherent compared with patients aged <65 years (P = 0.023). A similar percentage of expected budesonide/formoterol prescription fills was observed between the control (90.6%) and intervention (93.8%) groups.
Figure 6.
Number of adherent,a underuse,b overuse,c and no used days: FAS.
Notes: Classification of budesonide/formoterol use by patients in the control and intervention groups over the course of the study. aAdherent days are the number of study days a patient was adherent (exactly two sets of 2 puffs [4 puffs total], with both puffs of a set taken within 60 minutes of each other) with their budesonide/formoterol medication. bUnderuse days are the number of study days a patient took between 1 and 3 inhalations of their budesonide/formoterol medication on a given day. cOveruse days are the number of study days a patient took ≥5 inhalations of their budesonide/formoterol medication. dNo use days are the number of days a patient did not take their budesonide/formoterol medication.
Abbreviation: FAS, full analysis set.
Figure 7.
Odds of ≥80% adherence by subgroup: FAS (95% CI).a
Notes: Odds of adhering to budesonide/formoterol treatment across patient demographic subgroups. aLogistic regression model. The odds ratio for the reference group in each category is set to 1. bP <0.05.
Abbreviations: CI, confidence interval; FAS, full analysis set.
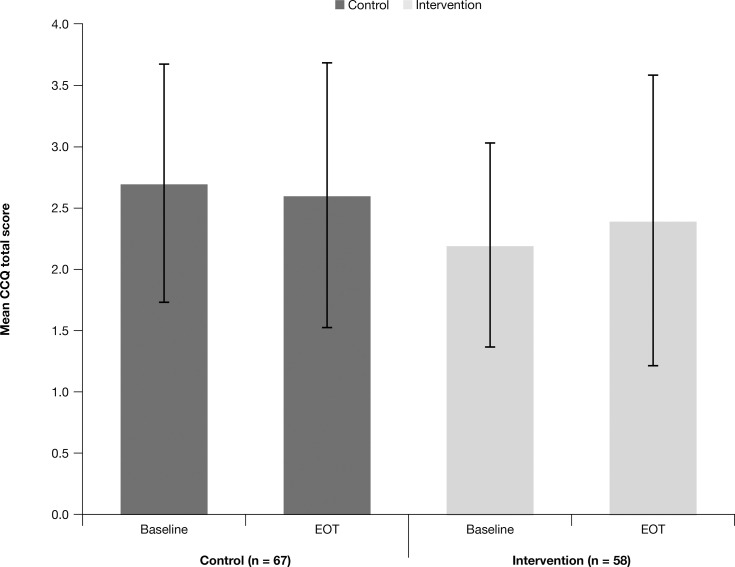
The intervention group had a significantly lower number and proportion of “no use”, “underuse”, and “overuse” study days relative to the control group (P <0.05 for all; Figure 6). Overuse alerts occurred for <0.1% of total patient days for both the control and intervention groups and were not associated with an AE or medication overdose, as determined by direct, real-time contact with the patient. There were no significant changes in COPD symptoms as measured by the CCQ over the course of the study (Figure 8).
Figure 8.
Mean CCQ scores at baselinea and EOTb: FAS.
Notes: CCQ scores range from 0 to 6, with higher values indicative of poorer health status. aBaseline is the date of randomization. bEOT is the latest date among assessments completed around the date the final phone/device was returned.
Abbreviations: CCQ, Clinical COPD Questionnaire; COPD, chronic obstructive pulmonary disease; FAS, full analysis set; EOT, end-of-treatment visit.
After adjusting for COPD severity and baseline cardiac comorbidities (events coded by system organ class term “cardiac disorders”), in the PP analysis set, patients in the intervention group aged ≥65 years were approximately 4.8 times more likely to be adherent during ≥80% of their device time on study compared with patients aged <65 years (P = 0.026). For the control group in the PP analysis set, adherence was not associated with age. Similarly, after controlling for COPD severity and all baseline comorbidities, relative to patients aged <65 years in the intervention group, patients aged ≥65 years were approximately 4.6 times more likely to be adherent during ≥80% of their device time on study (P = 0.030). In the FAS, patients with major protocol violations were significantly less likely to be adherent than patients without major protocol violations during ≥80% of the device time on study (odds ratio, 0.213; P = 0.002).
Safety
Similar percentages of patients who experienced AEs and serious AEs were observed between the control (31.3% and 11.9%, respectively) and the intervention group (30% and 7.1%, respectively; Supplemental Table 1).
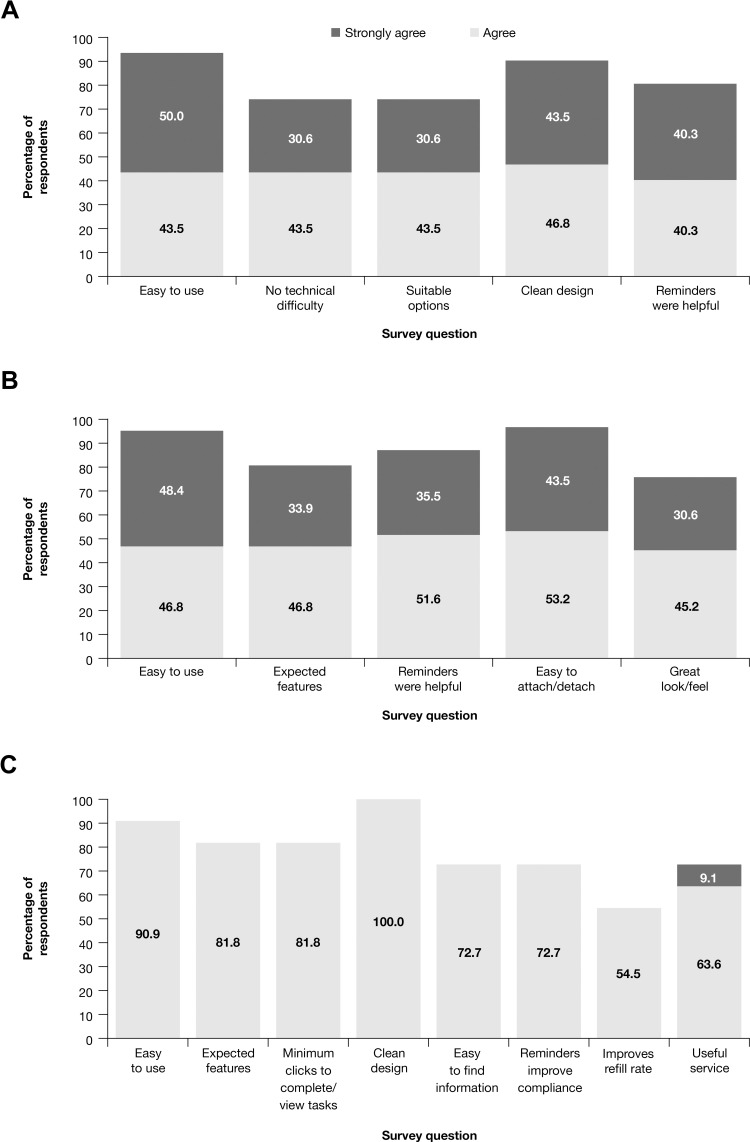
Patient and Provider Satisfaction
Based on survey responses from the FAS, a majority of patients reported the BreatheMate device and application were easy to use and that they had a clean look and feel, with suitable options and features; patients also felt the medication reminders were helpful in ensuring they used their medication as prescribed (Figure 9A and B). In the FAS intervention group, patient satisfaction was similar across all device and application survey questions for patients aged <65 and patients aged ≥65 years.
Figure 9.
Patient and provider satisfaction reports.
Notes: Patient satisfaction with (A) the smartphone application and (B) the BreatheMate device, as well as (C) study investigator/coordinator satisfaction with the BreatheMate web portal,a respectively. aSome physicians (n = 5) did not use the web portal. All eight study coordinators did use the web portal.
In addition to patients, the study investigators and coordinators were also surveyed to evaluate satisfaction with the BreatheMate web portal. Consistent with the patient feedback, a majority of the study investigators/coordinators responding to the survey reported the web portal was clean, uncluttered, easy to use, easy to understand, had the expected features, and was easy to navigate for the desired information (Figure 9C). Most study investigators/coordinators agreed the reminders improved daily medication adherence and prescription refills and that, overall, the device would be useful to them in helping patients to manage their condition (Figure 9C).
Technical Issues
Syncing issues were discovered during the enrollment period of this study and were found to be due to poor connectivity between the study-supplied smartphone device and the cellular network, which resulted in the loss of connection to the investigational study databases for extended periods of time for some patients. Although the periodic loss of cellular connectivity is expected in any study that involves a mobile device, the sponsor discovered that 17% of smartphones had not connected to the databases for over 28 days at a time (and therefore the databases were missing uploads of data related to their usage). This connectivity issue prompted the sponsor to conduct a risk assessment, which determined that loss of connectivity was unlikely to be associated with any safety issues for patients and that mitigations were already in place to reduce any risk of patient harm. The impact was limited to a lack of overuse alerts received by investigators (which were issued when patients used >10 puffs in a rolling 24-hour period) and a lack of medication refill reminders for patients, and this was also not expected to affect satisfaction with the system. However, the syncing issue did result in the discontinuation of some patients from the study due to their inability to sync their data with the databases. These discontinuations, combined with low study recruitment, prompted the sponsor to make a strategic decision to stop enrollment for the study.
A post hoc power analysis determined that at significance level α = 0.05, a two-sided Satterthwaite t-test had 94.93% power to detect the observed difference in means (0.28, where number of patients: nintervention = 67, ncontrol = 70; mean: µintervention = 1.61, µcontrol = 1.33; SD: σintervention = 0.389, σcontrol = 0.509). In this case, the actual power was higher than originally planned because the observed effect size was greater than the initially hypothesized effect size of 0.18, while the observed SDs were smaller than the 0.6 hypothesized value.
Discussion
In this study, the intervention group received daily medication reminders through the BreatheMate device attached to their budesonide/formoterol pMDI as well as through a smartphone application. This intervention group had a significantly higher number of adherent budesonide/formoterol puffs/day than those in the control group, who did not receive the daily reminders. The intervention group also had significantly higher numbers of adherent puffs/day in each 60-day study interval and, after adjusting for age, race, and smoking status, had more than three times the odds of being adherent ≥80% of days during the time on the study device compared with the control group. These findings demonstrate that daily medication reminders via a connected device can improve ICS/LABA adherence in adults diagnosed with COPD over short-term (6-month) follow-up. Indeed, the results from this study are consistent with other reports of daily reminders for inhaled therapies, which demonstrate a significant improvement in adherence to ICS therapy in patients with asthma over similar durations of follow-up.9,10
Results from subgroup analyses in the PP population indicate that, after adjusting for COPD severity and baseline comorbidities, patients aged ≥65 years in the intervention group were 4.6 times more likely to be adherent ≥80% of days during their time on study when compared with patients aged <65 years. Given the lack of an association of adherence with age among patients in the control group, the results suggest patients aged ≥65 years are more likely to demonstrate improved adherence in response to medication reminders. This result may seem counterintuitive based on the perception that younger patients are more experienced using Bluetooth-enabled and smartphone technology. However, this result may reflect that older patients are more likely to understand the value and importance of their treatment in preventing disease progression and, therefore, are more likely to heed the reminders.
An advantage to leveraging connected devices for medication reminders lies in their ability to directly quantify the actuation of the connected inhaler, thereby avoiding problems associated with less direct methods of measuring adherence. It is noteworthy that, in this study, patients in the intervention group had significantly fewer days in which they underused, overused, or did not use their budesonide/formoterol inhaler. This observation might suggest that in addition to improving adherence, medication reminders may have the potential to reduce medication misuse, though additional studies would be necessary to directly address this question. Furthermore, adherence among patients in the intervention group remained high and did not diminish over the course of the study. This is especially striking given that there were no daily incentives (eg, gamification, patient management education, or personalization of the reminders/how a patient’s disease status might be improved by enhanced adherence) for patients to use their medication as reminded. Notably, prior retrospective, interventional, and modeling studies have also demonstrated that improved adherence can yield net cost savings in COPD, even after accounting for increases in medication costs,3,5,15,16 and that this may be achieved using straightforward measures such as consolidation of treatment to a once-daily single inhaler therapy15 or by brief community pharmacist interventions.16 Similarly, the findings of this present study underscore the potential for even a simple, basic reminder, made possible by smart technology in this case, to serve as a cost-effective tool for enhancing treatment adherence.
An advantage of real-time information regarding the timing of medication usage is that it provides greater context for evaluating adherence when compared with dose counters or medication refill information. For example, with real-time data, it is possible to confirm patients are using their maintenance medication the correct number of times and at the correct intervals as opposed to simply using more or fewer puffs when they are more or less symptomatic. In this study, the medication was provided at no cost for both the control and intervention groups, and this may be a factor in the lack of a difference in the number of medication refills. It is also possible that simply by knowing they were taking part in a study that was monitoring medication use, patients may well have been more likely to adhere to their medication regimen. As such, it is important to note that the effect of medication reminders and prescription refill alerts may be greater in the real world.
An advantage of the BreatheMate device and application is that the date and time of each inhaler use were recorded. This additional information allows investigators and health care providers to identify trends and timing patterns in patient’s medication usage, which can be compared with additional information (eg, environmental factors) to gain better insight into a patient’s COPD. This additional insight may be useful to health care providers, given reports that poor patient understanding of COPD may contribute to poor adherence to therapy.7,17 Furthermore, in keeping with this notion, survey results indicate a majority of the study investigators who responded either agreed or strongly agreed that the BreatheMate reminders would improve patient adherence and that they would be useful in helping their patients to manage their condition. A majority of patients who responded to these surveys also reported finding the BreatheMate device/application easy to use and that medication reminders were helpful.
This study has several limitations. Primarily, cellular connectivity issues with the smartphone devices issued in this study resulted in inconsistent reporting of results, which eventually resulted in the early discontinuation of this study. Therefore, only 138 of the planned 414 subjects were randomized, resulting in altered statistical power and some imbalance in the background characteristics of the randomized subjects. Although the post hoc power analysis described above indicates the study still maintained above 90% power to detect an observed difference between the treatment groups, the reduced sample size may have resulted in larger variance for parameter estimation in the statistical models. This may have exaggerated the estimated effect sizes, resulting in an increased risk of Type I errors (false positives). These limitations may affect the reproducibility of the study results. Beyond the unexpected technical issues that arose, this study was not designed to evaluate a long-term intervention using BreatheMate and thus does not provide insights into possible effects of alarm fatigue with long-term use. In terms of the final enrolled study population, the mean age was approximately 67 years; older patients could have had less technologic familiarity with the smartphone application or decreased facility with the BreatheMate device, which may have, in turn, affected their uptake of the system, although medication reminders could still have been helpful in improving adherence regardless of age.
There were no significant changes in CCQ scores and no significant differences in prescription refills between the control and intervention groups over the 6-month study period. Given the difference in CCQ scores between the control and intervention groups at the outset, having CCQ as the only measure of symptoms, as well as the reduced sample size and short duration of the study, may have limited the ability of this study to identify clinical benefits arising from the use of the BreatheMate device and smartphone application. This finding may have also been somewhat limited by the BreatheMate device itself: the device was equipped to record inhaler use, but it was not designed to confirm inhalation of the administered dose or to ensure proper inhalation technique, which is important for adequate drug delivery, efficacy of the therapy, and thereby disease control and treatment outcomes.18 Improper technique when using the inhaler may have contributed to the lack of differences in CCQ scores. In addition, seasonality of COPD symptoms may have contributed to the lack of effect: enrollment was conducted between the months of August and April, and therefore some patients recruited towards the beginning or end of this period may have had only part or none of their winter symptoms captured during the 6-month study. Finally, although the CCQ is a validated questionnaire for the evaluation of self-reported COPD symptoms,14 clinical COPD outcome measures such as FEV1 and exacerbation incidences were not captured. However, the present study was designed as a real-world evaluation of COPD adherence and symptoms, and because clinical measures such as FEV1 may not be assessed routinely in all practices, especially for patients followed in primary care, they were not included in this study design.
Conclusion
In this study, patients with COPD who received daily medication reminders were significantly more likely to be adherent to their ICS/LABA therapy than patients who did not receive any reminders. Adherence to treatment did not decrease for patients in the intervention group, who received medication reminders and were significantly less likely to underuse, overuse, or not use their ICS/LABA treatment compared with patients in the control group. The effects of medication reminders on ICS/LABA adherence were more pronounced in patients aged ≥65 years. A longer-term study will be needed to identify clinical benefits associated with the improved treatment adherence demonstrated by this study.
Acknowledgments
Medical writing support was provided by Shane Walton, PhD, of MedErgy (Yardley, PA, USA), in accordance with Good Publication Practice (GPP3) guidelines and funded by AstraZeneca (Wilmington, DE, USA). The authors thank Jill Davis of AstraZeneca, who participated in the conception of the study, protocol review, and initial interpretation of results; and Melanie Morris of AstraZeneca, who provided study support. Selected data from this paper were presented at the 28th Annual Congress of the European Respiratory Society (September 15-19, 2018; Paris, France) as a late-breaking poster presentation and discussion with interim findings. The poster’s abstract was published in Eur Respir J. 2018;52(Suppl. 62):PA1988. http://doi.org/10.1183/13993003.congress-2018.PA1988.
Funding Statement
This study was supported by AstraZeneca (Wilmington, DE, USA).
Abbreviations
AE, adverse event; ANCOVA, analysis of covariance; BUD/FORM, budesonide/formoterol; CCQ, Clinical COPD Questionnaire; CI, confidence interval; CONSORT, Consolidated Standards of Reporting Trials; COPD, chronic obstructive pulmonary disease; EOT, end-of-treatment visit; FAS, full analysis set; FEV1, post-bronchodilator forced expiratory volume in 1 second; ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; pMDI, pressurized metered-dose inhaler; PP, per-protocol; SD, standard deviation.
Data Sharing Statement
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Ethics Approval
This study was approved by an institutional review board (Copernicus Group IRB, Cary, NC, USA).
Author Contributions
All authors made substantial contributions to the study’s conception, design, data acquisition, analysis, and/or interpretation; participated in drafting the manuscript or revising it critically for substantial intellectual content; agreed to submit the manuscript to this journal; gave final approvals of the submitted version; and agree to be accountable for all aspects of this publication.
Disclosure
Gerard J Criner has received research grants from AstraZeneca, Boehringer Ingelheim, Novartis, Respironics, MedImmune, Actelion, Forest, Pearl, Ikaria, Aeris, PneumRX, and Pulmonx; has equity interest in HGE Health Care Solutions, Inc. and HGE Technologies; and has consulted for Almirall, Boehringer Ingelheim, and Holaira. Kristen A Hahn is an employee of IQVIA, which was contracted by AstraZeneca to collect and analyze study data. Therese Cole and Kari Kastango were employees of IQVIA at the time this study was conducted. Therese Cole is currently affiliated with Advanced Clinical, Deerfield, IL, USA. Kari Kastango is currently affiliated with Everest Clinical Research, Little Falls, NJ, USA. James Eudicone and Ileen Gilbert are employees of AstraZeneca. The authors report no other conflicts of interest in this work.
References
- 1.George M. Adherence in asthma and COPD: new strategies for an old problem. Respir Care. 2018;63(6):818–831. doi: 10.4187/respcare.05905 [DOI] [PubMed] [Google Scholar]
- 2.Normansell R, Kew KM, Stovold E. Interventions to improve adherence to inhaled steroids for asthma. Cochrane Database Syst Rev. 2017;4:CD012226. doi: 10.1002/14651858.CD012226.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toy EL, Beaulieu NU, McHale JM, et al. Treatment of COPD: relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med. 2011;105(3):435–441. doi: 10.1016/j.rmed.2010.09.006 [DOI] [PubMed] [Google Scholar]
- 4.Neugaard BI, Priest JL, Burch SP, Cantrell CR, Foulis PR. Quality of care for veterans with chronic diseases: performance on quality indicators, medication use and adherence, and health care utilization. Popul Health Manag. 2011;14(2):99–106. doi: 10.1089/pop.2010.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Boven JF, Chavannes NH, van der Molen T, Rutten-van Mölken MP, Postma MJ, Vegter S. Clinical and economic impact of non-adherence in COPD: a systematic review. Respir Med. 2014;108(1):103–113. doi: 10.1016/j.rmed.2013.08.044 [DOI] [PubMed] [Google Scholar]
- 6.Dhamane AD, Schwab P, Hopson S, et al. Association between adherence to medications for COPD and medications for other chronic conditions in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:115–122. doi: 10.2147/COPD.S114802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2013;14:109. doi: 10.1186/1465-9921-14-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100 [DOI] [PubMed] [Google Scholar]
- 9.Charles T, Quinn D, Weatherall M, Aldington S, Beasley R, Holt S. An audiovisual reminder function improves adherence with inhaled corticosteroid therapy in asthma. J Allergy Clin Immunol. 2007;119(4):811–816. doi: 10.1016/j.jaci.2006.11.700 [DOI] [PubMed] [Google Scholar]
- 10.Chan AH, Stewart AW, Harrison J, Camargo CA, Black PN, Mitchell EA. The effect of an electronic monitoring device with audiovisual reminder function on adherence to inhaled corticosteroids and school attendance in children with asthma: a randomised controlled trial. Lancet Respir Med. 2015;3(3):210–219. doi: 10.1016/S2213-2600(15)00008-9 [DOI] [PubMed] [Google Scholar]
- 11.Merchant R, Szefler SJ, Bender BG, et al. Impact of a digital health intervention on asthma resource utilization. World Allergy Organ J. 2018;11(1):28. doi: 10.1186/s40413-018-0209-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sumino K, Locke ER, Magzamen S, et al. Use of a remote inhaler monitoring device to measure change in inhaler use with chronic obstructive pulmonary disease exacerbations. J Aerosol Med Pulm Drug Deliv. 2018;31(3):191–198. doi: 10.1089/jamp.2017.1383 [DOI] [PubMed] [Google Scholar]
- 13.SYMBICORT® (Budesonide and Formoterol Fumarate Dihydrate) [Package Insert]. Dunkerque, France: AstraZeneca Dunkerque Production; 2017. [Google Scholar]
- 14.van der Molen T, Willemse BW, Schokker S, Ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2003;1:13. doi: 10.1186/1477-7525-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miravitlles M, Marin A, Huerta A, Carcedo D, Villacampa A, Puig-Junoy J. Estimation of the clinical and economic impact of an improvement in adherence based on the use of once-daily single-inhaler triple therapy in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2020;15:1643–1654. doi: 10.2147/COPD.S253567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Boven JFM, Tommelein E, Boussery K, et al. Improving inhaler adherence in patients with chronic obstructive pulmonary disease: a cost-effectiveness analysis. Respir Res. 2014;15(1):66. doi: 10.1186/1465-9921-15-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDonald VM, Higgins I, Gibson PG. Managing older patients with coexistent asthma and chronic obstructive pulmonary disease: diagnostic and therapeutic challenges. Drugs Aging. 2013;30(1):1–17. doi: 10.1007/s40266-012-0042-z [DOI] [PubMed] [Google Scholar]
- 18.Gregoriano C, Dieterle T, Breitenstein AL, et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: data from a randomized controlled trial. Respir Res. 2018;19:237. doi: 10.1186/s12931-018-0936-3 [DOI] [PMC free article] [PubMed] [Google Scholar]