The impact of the severe acute respiratory syndrome coronavirus 2 pandemic on sports in the United States was truly felt the second week of March 2020, beginning with the cancellation of the Ivy League women’s and men’s basketball tournaments on March 10 and the announcement of the first coronavirus disease 2019 (COVID-19) positive player in the National Basketball Association (NBA) on March 11. Since then, guidance on returning to play (RTP) after COVID-19 infection has been the subject of much discussion. In this Leadership Page, I have asked Eugene H. Chung, MD, FACC, chair of the American College of Cardiology’s (ACC’s) Sports and Exercise Cardiology Leadership Council, and Richard Kovacs, MD, MACC, founding co-chair of the Sports and Exercise Cardiology Leadership Council, to reflect on present recommendations and share their thoughts on future directions for RTP decision-making in athletes recovered from COVID19.
—Athena Poppas, MD, FACC
Early Game Plan and Intra-Game Adjustments
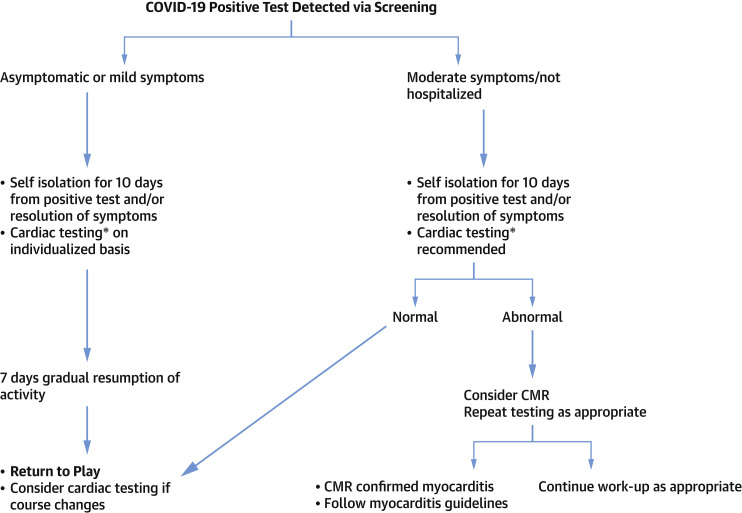
In May 2020, experts on behalf of the ACC Sports and Exercise Cardiology Section proposed an RTP algorithm for competitive athletes (1). Given our limited understanding of the impact of COVID-19 on the athlete’s heart at the time, a relatively conservative approach was warranted. This algorithm, as well as other documents from around the same time, recommended cardiac evaluation to assess for presence of cardiac injury after COVID-19 infection (2,3). With experience gained caring for athletes of all levels during the spring and summer of 2020, the ACC Sports and Exercise Cardiology Leadership Council convened a writing group to update the first algorithm (4). Major updates to the first algorithm were: 1) RTP recommendations for high school aged athletes; 2) RTP recommendations for master-level (i.e., post-collegiate) athletes; 3) suggested reduction of self-isolation period from 14 to 10 days, in keeping with updated Center for Disease Control (CDC) guidelines; 4) discussion of pitfalls of over-interpretation of myocardial injury and myocarditis by cardiac magnetic resonance imaging (CMR) in athletes; and 5) de-emphasis of cardiovascular testing in those with mild or no symptoms (4). As cardiovascular screening protocols are focused on asymptomatic, mildly asymptomatic, and less commonly, moderately symptomatic competitive athletes seeking to RTP, an adapted algorithm from the most recent recommendations is shown in Figure 1 .
Figure 1.
Adapted Return to Play Algorithm for Athletes
∗Cardiac testing to include electrocardiogram (ECG), high-sensitivity cardiac troponin (hs-cTn), and echocardiogram (Echo). Cardiac magnetic resonance imaging (CMR) may be included as part of initial screening, depending on local recommendations, as in the case of the Big Ten Conference. Adapted from Kim et al. (4). COVID-19 = coronavirus disease 2019.
How Did We Get Here?
Early in the pandemic, concerns about the cardiovascular sequelae associated with COVID-19 infection drove discussions about the potential impact on recovered athletes RTP. An early study on hospitalized patients with COVID-19 reported acute cardiac injury, defined as troponin levels >99th percentile, and electrocardiographic (ECG) and/or echocardiographic abnormalities in up to 28%, significantly higher that what would be expected in non–COVID-19 acute viral infections (5). Another study demonstrated COVID-19 in the myocardium of 61.5% of consecutive autopsy cases, even in the absence of acute myocarditis (6). Puntmann et al. (7) raised concerns about myocardial inflammation detected by CMR in relatively asymptomatic recovering outpatients. Publicized case reports of prominent professional and collegiate athletes raised additional concerns about COVID-19 related myocarditis. Furthermore, acute right ventricular (RV) dysfunction was commonly reported in severely ill COVID-19 patients and attributed to the increased pulmonary vascular resistance (8). RV dysfunction can be challenging to distinguish from exercise-induced cardiac remodeling and thus presents particular challenges to sports cardiologists (8).
While the aforementioned studies have limitations in their direct applicability to the athlete population, they indeed generated much discussion about the impact of COVID-19 on the hearts of athletes. Myocarditis is a leading cause of sudden cardiac death in athletes. RTP recommendations after myocarditis remain predicated on normalization of ventricular function, normalization of any biomarker elevations, resolution of ECG changes, and absence of arrhythmias on stress testing and/or ambulatory ECG monitoring (1,4).
In September 2020, researchers from The Ohio State University reported the first case series of myocarditis in athletes. They found myocarditis by CMR in 4 out of 26 scanned athletes; and another 8 had late gadolinium enhancement (LGE) suggesting prior myocardial injury (9). At the time of this writing, there are now at least 2 additional single-center reports of varying incidences of myocarditis in COVID-19–positive athletes and abnormalities on CMR. These studies highlight the potential and nuances required of CMR and the need for continued investigation on short-term and long-term impacts of abnormal findings. An international expert panel recently published a comprehensive set of recommendations on use of different imaging modalities in RTP decisions (8).
These data, however, have limitations. Longitudinal follow-up data on clinical outcomes are not yet available, and future study is needed on control groups comprising subjects without illness and subjects with viral illnesses other than COVID-19.
Future Directions
As discussed in the most recent statement from the ACC Sports and Exercise Cardiology Leadership Council, future revisions to guidelines should be shaped by data (4). Observational registry data from professional and collegiate athletic organizations are forthcoming. A national collegiate registry, led by Aaron Baggish, MD, Jonathan Drezner, MD, and Kimberly Harmon, MD, will better inform us on the incidence and prevalence of COVID-19 and potential cardiac involvement from >70 U.S. Division I athletic programs. The Big Ten Conference is setting up a cardiac registry from 14 schools that will report observational data but also incorporate control groups. Core laboratories in the areas of clinical/biomarkers, ECG, echocardiography, CMR, and epidemiology will independently review all cardiac evaluations (10). (Disclosure: Drs. Chung and Kovacs are Steering Committee members of the Big Ten Cardiac Registry.)
There are a number of topics we hope are addressed by the forthcoming registries.
-
•
CMR is a nuanced modality, and while the best for defining cardiac abnormalities, it requires particular expertise in its performance and interpretation (8), and it is not always readily accessible. Even within the Big Ten, one institution is approximately a 2-h drive from the nearest CMR-capable referral center. Future studies will ideally follow athletes longitudinally and incorporate controls groups that are healthy and have non-COVID-19–related infection. Until we have more data, a pragmatic approach that uses CMR on an individualized basis seems reasonable (8,10).
-
•
Symptoms have been the starting triage point for expert-led RTP algorithms to date, but they can be subtle, minimized, or even denied when one is eager to return to play. Symptoms may manifest later during the gradual resumption of activity period in the form of exercise intolerance or may linger longer and require extended recovery time. In the latest ACC Sports and Exercise Cardiology Council recommendations, it seemed reasonable to group together the mildly symptomatic and asymptomatic, followed by moderate/nonhospitalized and severe/hospitalized categories. However, the distinction between moderate and mildly symptomatic is still not so clear. For example, is any fever of <3 days duration a mild symptom? Is 4 days of fever significantly worse than 3? Does persistence of anosmia and aguesia over 14 days reflect long-term central nervous system involvement and potential dysautonomia? For athletes recovering from COVID-19, continued symptoms might warrant cardiovascular testing on a case-by-case basis before gradual resumption of sport (4).
-
•
The RTP algorithms have leaned on the most recent myocarditis guidelines to determine recommendations regarding recovery time and reevaluation before RTP (4). As highlighted by a recent expert consensus statement, COVID-19 has raised critical questions on predicting myocardial injury, temporal characteristics of injury versus inflammation, effect of varying infections on the heart, and significance of long-term abnormalities on imaging (8). Myocarditis is a clinical diagnosis that is supported by findings on history and physical, biomarkers, ECG, echocardiography, and/or CMR. In many of the studies mentioned above, the diagnosis of myocarditis was given based on imaging findings alone, the clinical relevance of which require further study. Registry data and controlled cohort studies will help answer some of the above questions.
-
•
Wearable and mobile digital health technology applications are expanding at breathtaking speed. Watch, wrist, ring, and finger sensors, and patch form factors offer varying options for detecting arrhythmias, monitoring activity, heart rate (HR), heart rate variability (HRV), sleep, oxygen saturation, and other parameters that could be monitored for early warning signs of infection and facilitate management of the athlete’s wellbeing.
-
•
Long-term prognosis and “employability” for the select few collegiate athletes aspiring to professional careers requires clarity. Athletes eligible to participate in league scouting combines, such as the National Football League (NFL) and NBA, have extensive cardiac screening, and the impact of imaging findings can have important ramifications for their contracts. Further data are necessary to objectively address this issue, which can have a major economic impact for some individuals.
-
•
Disparities in care should be addressed. Some teams/conferences/leagues have greater resources to test athletes before RTP. Recommendations for testing and RTP need to assure that all athletes receive optimal care.
Forthcoming registry studies should provide a clearer picture of the risk of myocarditis in the short term in athletes, guide future RTP algorithms, and initiate long-term study of the effects of COVID-19 on the heart. The ACC Sports and Exercise Cardiology Section, the ACC COVID-19 Hub, and the JACC Journals will play a critical role in developing new decision pathways and informing cardiovascular clinicians about this important and fast-changing topic. In the meantime, a pragmatic approach, gradual return to activity, continued surveillance for changes in symptoms, and compliance with the latest public health recommendations are warranted for the athlete returning to play after infection with COVID-19.
References
- 1.Phelan D., Kim J.H., Chung E.H. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) infection. JAMA Cardiol. 2020;5:1085–1086. doi: 10.1001/jamacardio.2020.2136. [DOI] [PubMed] [Google Scholar]
- 2.Baggish A., Drezner J.A., Kim J., Martinez M., Prutkin J.M. Resurgence of sport in the wake of COVID-19: cardiac considerations in competitive athletes. Br J Sports Med. 2020;54:1130–1131. doi: 10.1136/bjsports-2020-102516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatia R.T., Marwaha S., Malhotra A. Exercise in the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) era: a questions and answer session with the experts endorsed by the Section of Sports Cardiology & Exercise of the European Association of Preventive Cardiology (EAPC) Eur J Prev Cardiol. 2020;27:1242–1251. doi: 10.1177/2047487320930596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim J.H., Levine B.D., Phelan D. Coronavirus disease 2019 and the athletic heart: emerging perspectives on pathology, risks, and return to play. JAMA Cardiol. 2020 Oct 26 doi: 10.1001/jamacardio.2020.5890. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linder D., Fitzek A., Brauninger H. Association of cardiac infection with SARS-CoV-2 in confirmed COVD-19 autopsy cases. JAMA Cardiol. 2020;5:1281–1285. doi: 10.1001/jamacardio.2020.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puntmann V.O., Carerj M.L., Wieters I. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phelan D., Kim J.H., Elliott M.D. Screening of potential cardiac involvement in competitive athletes recovering from COVID-19: an expert consensus statement. J Am Coll Cardiol Img. 2020;13:2635–2652. doi: 10.1016/j.jcmg.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajpal S., Tong M.S., Borchers J. Cardiovacular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. 2021;6:116–118. doi: 10.1001/jamacardio.2020.4916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rink L.D., Daniels C.J., Boersma D. Competitive sports, the coronavirus disease 2019 pandemic, and Big Ten athletics. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.007608. [DOI] [PMC free article] [PubMed] [Google Scholar]