Abstract
Background:
Technology can enhance support for families caring for persons living with dementia but must be acceptable to be adopted. The FamTechCare clinical trial engaged caregivers in videorecording care encounters that were reviewed by an expert panel who provided tailored feedback. The intervention reduced caregiver depression and improved caregiver competence. This mixed methods study reports on caregiver satisfaction and utilization of the intervention, and expert panel evaluation of the intervention.
Methods:
A convergent parallel mixed methods design was used to evaluate the satisfaction, usability, and feasibility of the FamTechCare intervention. In the multisite randomized controlled trial, caregiver-person living with dementia dyads were randomized to the FamTechCare video support or attention control telephone support groups. Caregivers completed a satisfaction survey at the completion of the 3-month trial. Utilization was evaluated using the number and duration of videos submitted and calls received by caregivers. Relationships between participant characteristics and their satisfaction and utilization were evaluated. Feasibility of the intervention was assessed through content analysis of interviews with the expert panel.
Results:
The majority of caregivers in both groups reported benefits from participation. More FamTechCare caregivers found the interventionist support to be helpful (p=.001) and effective (p=.020) compared to attention control caregivers. FamTechCare caregivers of persons with more severe dementia were more likely to report that videorecording intruded on their privacy (p=.050). Caregiver age, gender, and education, dyad relationship, rural status, and type and severity of dementia were not associated with ratings of acceptability, ease of use, or intervention utilization. The expert panel described the FamTechCare intervention as useful and identified adaptations to enhance feasibility.
Conclusion:
Regardless of age, gender, and relationship, caregivers found the intervention acceptable and easy to use and rated the expert feedback as effective in addressing care challenges. Further adaptation may be needed for FamTechCare to be readily implemented.
Keywords: Alzheimer Disease, Behavioral Symptoms, Caregivers, Dementia, Telemedicine
Introduction
Cost-effective dementia care that supports quality of life is a worldwide public health priority (World Health Organization, 2012). The population of persons living with dementia is projected to expand from 47 million in 2015 to 132 million by 2050 (Prince, Comas-Herrera, Knapp, Guerchet, & Karagiannidou, 2016). In the United States alone, it is estimated that informal caregivers currently provide 18.5 billion hours of unpaid care annually (Alzheimer’s Association, 2019). Supporting caregivers is a critical component to meeting this growing public health need (World Health Organization, 2017).
The demands of dementia caregiving, particularly managing behavioral and psychological symptoms of dementia (BPSD), lead to negative outcomes for both caregivers (e.g., declining well-being) and persons living with dementia (e.g., nursing home placement) (Feast, Moniz-Cook, Stoner, Charlesworth, & Orrell, 2016; Monin & Schulz, 2009; Porter et al., 2016). Caregiver well-being and satisfaction are adversely associated with caregiving competence and stress, making it essential to create interventions that support caregivers in managing dementia caregiving challenges (Quinn et al., 2019).
Technology provides an opportunity to reach and support caregiver-person living with dementia dyads using individualized and tailored approaches (Hopwood et al., 2018). Caregivers recognize the potential benefits of technology as a resource to assist in caregiving and report a desire to use technology for personalized professional consultation and guidance for providing care (American Association of Retired Persons, 2016). Currently, a number of technologies available to support family caregivers range from simple provision of information, to support programs with peers and/or professionals, to actual training, as well as psychotherapy for caregivers (Bossen, Kim, Williams, Steinhoff, & Strieker, 2015; Egan et al., 2018; Hopwood et al., 2018; Scott et al., 2016; Topo, 2008; Waller, Dilworth, Mansfield, & Sanson-Fisher, 2017).
These technological interventions that connect caregivers to professionals, peers, and education have generally demonstrated modest benefits in improving caregiver mental health outcomes (Deeken, Rezo, Hinz, Discher, & Rapp, 2019; Hopwood et al., 2018). Many of these interventions do not focus on the caregiver-person living with dementia dyad and may be limited by the perspective and retrospective recall of the caregiver which further limits the ability to accurately tailor interventions. Available telehealth technology exists that allows caregivers to connect to providers while overcoming these limitations. The FamTechCare telehealth intervention tested such technology in the Supporting Family Caregivers with Technology clinical trial.
FamTechCare Clinical Trial
FamTechCare is a multicomponent telehealth intervention engaging family caregivers of persons living with dementia in videorecording challenging care situations and behaviors. Caregivers submit videos that are reviewed by an interdisciplinary team who provide tailored feedback to improve care (Figure 1). Dementia caregivers were provided with a telehealth video-monitoring unit (VMU) that includes an iPad Mini with the videorecording application, a Bluetooth remote, and an iPad stand. Along with an individual training session in the caregiver’s home on the use of the VMU, the caregiver received a binder with detailed instructions, including step-by-step images, as a resource for the VMU. The innovative videorecording application, Behavior Capture (https://behaviorimaging.com, Boise, ID), utilizes buffering technology that captures events before the recording is initiated. When the caregiver triggered the record button, the captured video footage included buffered video from the 5 minutes prior to the initiation of the recording. Caregivers were able to manually trigger the recording on the iPad Mini or by using a Bluetooth remote that could be kept with the caregiver during daily activities. The recommended set-up included having the iPad placed on an iPad stand in the location of the care encounter with the application open and running. By using this set up recordings could be easily triggered when a challenging care encounter arose and both the caregiver and person living with dementia could be captured in the video. Caregivers then reviewed the recordings and decided whether to delete the videos or upload them to the HIPAA-secure Behavior Connect website for review by the expert team.
Figure 1.
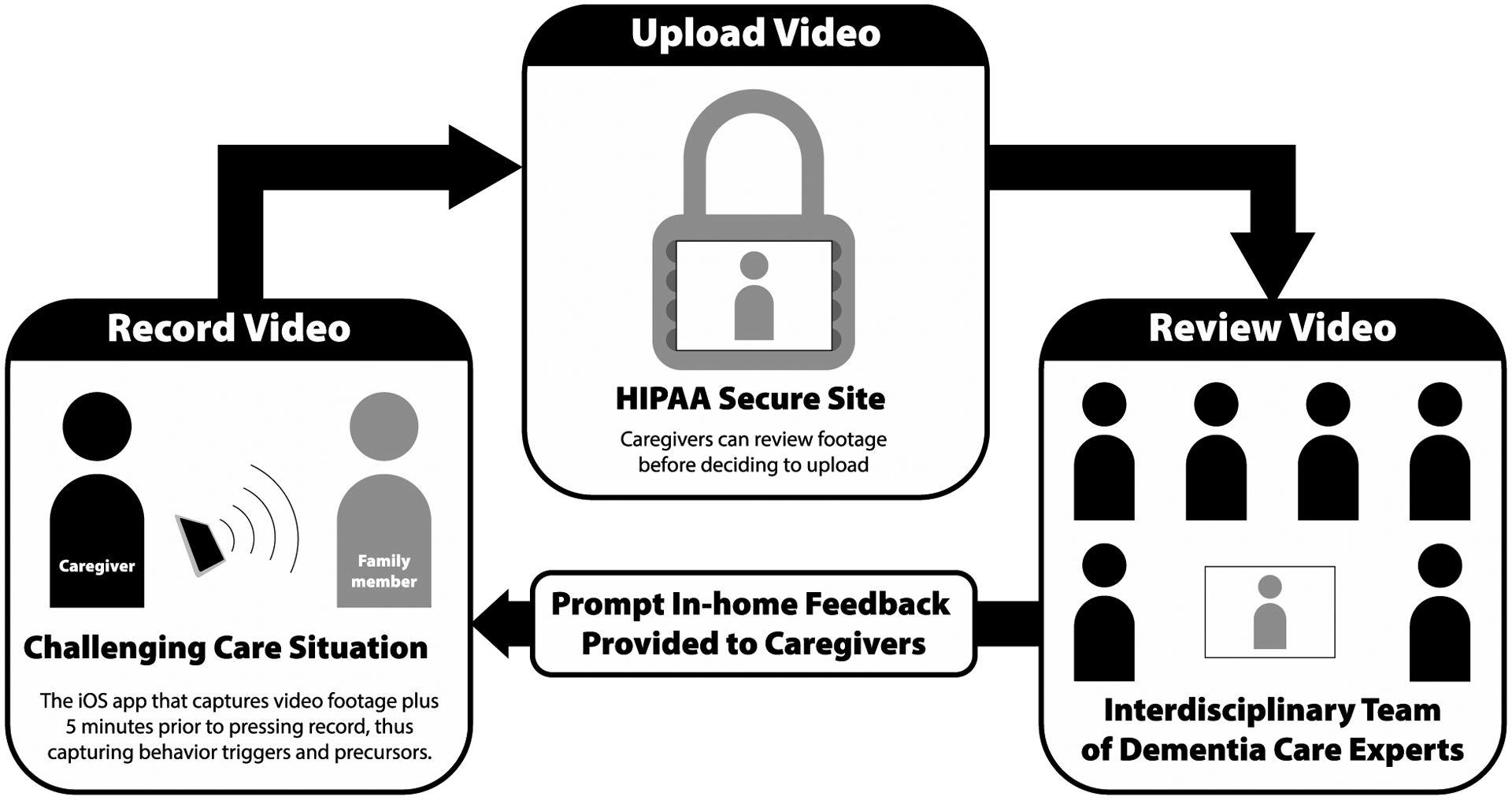
FamTechCare Study Procedure
Graphic Design by Chris Lorenzen for Kristine Williams © 2016.
The uploaded videorecordings were all screened by a designated team member within 24-hours of submission to ensure there were no immediate safety concerns and to identify the portions of videos for weekly expert review. Caregivers received feedback on all videos sent for review, however the portions of the videos that were not deemed relevant (e.g., if the recording was not stopped and the dyad left the room) or were repetitive were not observed by the expert team. The interdisciplinary video review team included research and clinical professionals from the fields of nursing, geriatric psychiatry, social work, and psychology. Videos were reviewed in person or remotely using Zoom web conferencing; a share-screen feature allowed review group members to watch and discuss the videos simultaneously and to develop tailored interventions. The feedback from the expert team was then relayed to each caregiver during a scheduled weekly phone call with the interventionist.
The FamTechCare group was compared to the attention control group whose participants received a weekly scheduled phone call with the interventionist in which they retrospectively reported care challenges and received care guidance. The interventionist was either a nurse or social worker with a master’s degree, who was also a member of the expert team. To reduce the disadvantage of being randomly assigned to the attention control group, these caregivers were also provided with the VMU and were trained to record and submit weekly videos. Caregivers and study personnel were unblinded to the group assignment following consent, so attention control caregivers were aware they would not receive weekly video feedback if videos were created with the VMU. However, their videos were reviewed by the expert team and feedback was provided at the completion of the 3-month trial after all outcomes and surveys were completed, to provide them with some benefit for submitting videos. The main outcome analysis and results of FamTechCare clinical trial are reported elsewhere (Williams et al., 2019). The FamTechCare group had greater reductions in caregiver depression and gains in caregiver perceived competence after 3 months compared to the attention control group.
Purpose
Effective interventions must be acceptable and easy to use to be adopted and utilized by caregivers. This paper reports the satisfaction, utilization, and feasibility of the FamTechCare telehealth intervention during the FamTechCare clinical trial. The effects of dyad characteristics on satisfaction and utilization were quantitatively evaluated and qualitative analysis of interviews with expert team members were used to evaluate feasibility and to identify adaptations for future implementation.
Methods
Design
A convergent parallel mixed methods design was used to evaluate the satisfaction, usability, and feasibility of the FamTechCare intervention, that was tested in a randomized controlled trial (Williams et al., 2018; Williams et al., 2019). The randomized controlled trial was conducted to test the effects of the FamTechCare intervention versus telephone-support on caregiver psychosocial outcomes (e.g., depression) at two research sites in the Midwest. In this mixed methods analysis, the quantitative satisfaction and usability data are evaluated concurrently with the qualitative feasibility information to achieve a greater understanding of the FamTechCare intervention and potential for future applications. Human subject and ethics approval was obtained at both sites.
Sample
Caregiver-person living with dementia dyads were recruited between October 2014 and June 2018. Inclusion criteria for persons living with dementia were a dementia diagnosis and living at home. Persons living with dementia were excluded if diagnosed with Huntington’s disease, schizophrenia, manic-depressive disorder, deafness, or intellectual disability. Informed consent was obtained from all participants or their surrogate decision makers, and assent was obtained from persons living with dementia who were unable to consent independently. Caregiver-person living with dementia dyads were randomly assigned to the experimental (FamTechCare) group or the attention control group. To meet recruitment goals and family needs, more than one family caregiver for each person living with dementia was able to enroll, and those dyads were cluster-randomized to the same treatment group.
Data collection occurred at two study sites, both midwestern universities. Study Site 1 was based at a College of Nursing. Recruitment strategies were community-based and included advertisements in local magazines and newspapers, presentations at local caregiving meetings, and mass email notifications through the university community. Study Site 2 was based in an NIA-designated Alzheimer’s Disease Center, where recruitment was primarily completed through electronic medical record screening using a partial HIPPA waiver. Some community recruitment was also utilized. See the published FamTechCare protocol for specific details on participant recruitment and eligibility, the protection of human subjects, intervention development, study procedures, and fidelity (Williams et al., 2018).
Data Collection
Demographic information was collected for both caregivers and persons living with dementia. Dementia severity was measured with the Functional Assessment Scale (FAST). The FAST is a 16-item scale assessing function and dementia symptoms in which a score of 1 indicates normal adult function and a score of 8 indicates severe dementia (Reisberg, 2007; Sclan & Reisberg, 1992). Rural residence was categorized into rural (≥20% of county population rural) and not rural (<20% of county population rural).
Satisfaction.
Satisfaction with video monitoring was measured at the end of the 3-month trial with a 13-item survey. A 5-point Likert scale (1=strongly disagree to 5=strongly agree) was used to assess ease of use and perceived satisfaction with the VMU and telehealth feedback. Eight items that referred to the VMU pertained only to the FamTechCare participants. Five additional items assessed satisfaction with interventionist feedback and were rated by both the FamTechCare and attention control participants.
Utilization.
Utilization was measured using four variables: the number and duration of submitted videos during the study (for FamTechCare participants only) and the number and duration of telephone calls during the study (for both FamTechCare and attention control participants). Number and duration of videos was not evaluated for the attention control group because they did not receive the video support intervention.
Feasibility.
At the end of the 4-year trial all current members of the expert team were invited to participate in a semistructured interview focused on feasibility of the FamTechCare intervention. Eight of nine members completed an interview lasting less than one hour. One member, a geriatric psychiatry nurse practitioner, did not complete an interview due to scheduling conflicts. The four former members (i.e., a nurse practitioner, nurse researcher, geriatric psychiatrist, and a clinical psychologist) from the expert teams were not contacted for interviews as they had all left the institutional sites. All of these members were replaced on the team at the time of their departure and there is no reason to believe their responses would differ from the members interviewed. The interview guide assessed strengths and weaknesses of the intervention and suggestions for future implementation.
Data Analysis
Demographic characteristics of caregivers and persons living with dementia were summarized with descriptive statistics. The analysis included only dyads with family caregivers who completed at least four weeks in the trial (91.6% completion rate at 4 weeks). See the main analysis for description of the final sample (Williams et al., 2019). SAS software (version 9.4) was used for all statistical analyses.
Satisfaction.
Due to small counts in some categories of responses on the satisfaction questionnaire, the scale responses “strongly” and “somewhat” were combined for both ends of the scale, resulting in a 3-point scale (disagree, neutral, agree). Responses to eight items pertaining to the VMU were summarized using frequencies and percentages for the FamTechCare group.
The relationships between satisfaction with the VMU and dyad characteristics were evaluated for four questions related to ease of use, privacy, purpose, and acceptability. These four questions were selected due to their general relevance to the use of in-home videorecording for caregiver support. Dyad characteristics included the dementia severity (i.e., mean FAST score) and type of dementia for the person living with dementia, caregiver age, gender and education, dyad relationship, rural residence status, and study site. For this analysis, neutral responses were combined with the disagree or agree responses in order to compare caregivers who were positive about using VMU to those who were negative or neutral about using VMU. The combination of neutral with agree or disagree was based on the wording of the question. Neutral was combined with agree for negatively worded questions and combined with disagree for positively worded questions. The relationships between satisfaction with VMU and continuous dyad characteristics (i.e., dementia severity, caregiver age) were tested using the Wilcoxon rank-sum test, and relationships between satisfaction and categorical characteristics (i.e., type of dementia, caregiver gender and education, dyad relationship, rural residence status, and study site) were tested using Fisher’s exact test.
Responses to five items pertaining to satisfaction with interventionist feedback were summarized using frequencies and percentages and compared between the FamTechCare and attention control groups using Fisher’s exact test. For this analysis, the 3-point scale (disagree, neutral, agree) was used.
Utilization.
Relationships between dyad characteristics and the number and duration of videos submitted was evaluated for the experimental group; and, relationships between dyad characteristics and the number and duration telephone calls received by caregivers was evaluated for both the experimental and attention control groups. The Wilcoxon rank-sum test was used to evaluate the relationship between utilization and caregiver gender, dyad relationship, rural residence status, and study site. The Kruskal-Wallis test was used to evaluate the relationship between utilization and caregiver education and the dementia type for the person living with dementia. The Spearman’s rho coefficient was used to evaluate the relationship between utilization and dementia severity (i.e., mean FAST score) and caregiver age.
Feasibility.
Expert interviews were evaluated using qualitative content analysis (Elo & Kyngas, 2008; Hsieh & Shannon, 2005). Meaning units were identified and then condensed into themes (Hsieh & Shannon, 2005). Revision of themes occurred until saturation was reached. A second coder reviewed coding and theme development for agreement.
Results
Sample Characteristics
The FamTechCare study included 84 dyads made up of 83 caregivers and 71 persons living with dementia (9 persons living with dementia had more than one caregiver enrolled, and 1 caregiver provided care for two persons living with dementia). Forty-three dyads received the FamTechCare intervention, and 41 dyads received the attention control intervention. The majority of caregivers cared for their spouse (66.3%), were female (71.2%), and had a mean age of 64.2±12.8 years (range = 32.0–90.0). Over half of the persons living with dementia had moderately severe dementia (50.7%). Demographic characteristics for caregivers and persons living with dementia are reported in Table 1. There were no significant differences (p<.05) in demographic characteristics between the FamTechCare and attention control groups.
Table 1.
Demographic Characteristics of Caregivers and Persons Living with Dementia (PLWD)
| FamTechCare | Attention Control | ||||
|---|---|---|---|---|---|
| Caregivers | N | Mean±SD | N | Mean±SD | |
| Age (years) | 42 | 64.6±12.2 | 41 | 63.9±13.7 | |
| 41 | 4.4±3.0 | 41 | 3.8±3.5 | ||
| n | % | n | % | ||
| Gender | |||||
| Female | 30 | 71.4 | 29 | 70.7 | |
| Male | 12 | 28.6 | 12 | 29.3 | |
| Race/Ethnicity | |||||
| Non-Hispanic white | 37 | 88.1 | 40 | 97.6 | |
| African American | 4 | 9.5 | 1 | 2.4 | |
| More than one race | 1 | 2.4 | 0 | 0.0 | |
| Relationship to PLWD | |||||
| Spouse | 29 | 69.1 | 26 | 63.4 | |
| Child/Spouse of child | 12 | 28.6 | 15 | 36.6 | |
| Other | 1 | 2.4 | 0 | 0.0 | |
| Education level | |||||
| Less than Bachelor’s degree | 19 | 45.2 | 15 | 36.6 | |
| Bachelor’s degree | 13 | 31.0 | 20 | 48.8 | |
| Master’s degree or higher | 10 | 23.8 | 6 | 14.6 | |
| Persons Living with Dementia | N | Mean±SD | N | Mean±SD | |
| Age (years) | 39 | 75.5±9.7 | 32 | 75.9±9.3 | |
| n | % | n | % | ||
| Gender | |||||
| Male | 24 | 61.5 | 18 | 56.3 | |
| Female | 15 | 38.5 | 14 | 43.8 | |
| Race/Ethnicity | |||||
| Non-Hispanic white | 37 | 94.9 | 31 | 96.9 | |
| African American | 2 | 5.1 | 1 | 3.1 | |
| Education level | |||||
| Less than Bachelor’s degree | 22 | 56.4 | 17 | 53.1 | |
| Bachelor’s degree | 5 | 12.8 | 9 | 28.1 | |
| Master’s degree or higher | 12 | 30.8 | 6 | 18.8 | |
| Type of dementia | |||||
| Alzheimer’s disease | 21 | 53.9 | 16 | 50.0 | |
| Other diagnosed dementia | 15 | 38.5 | 9 | 28.1 | |
| Unknown | 3 | 7.7 | 7 | 21.9 | |
| Dementia Stage (FAST) | |||||
| Incipient | 0 | 0.0 | 1 | 3.1 | |
| Mild | 10 | 25.6 | 10 | 31.3 | |
| Moderate | 7 | 18.0 | 6 | 18.8 | |
| Moderately severe | 21 | 53.9 | 15 | 46.9 | |
| Severe | 1 | 2.6 | 0 | 0.0 | |
Satisfaction
Table 2 summarizes FamTechCare caregiver responses to the satisfaction with the VMU questions. The majority of FamTechCare caregivers reported the VMU was easy to set up and use (75.6%) and found it easy to transfer recordings to the expert team (75.6%). Having the VMU in their home was acceptable (85.4%) for the majority of caregivers, and the VMU did not intrude on the majority of caregivers’ privacy (63.4%). Because many caregivers used the manual iPad button to initiate a recording, nearly half of the responses relating to use of the remote-control were missing.
Table 2.
Summary of Responses to Satisfaction with the Video Monitoring Unit (VMU) Questions (FamTechCare Caregivers)
| Statement | N | Response | |||||
|---|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | |||||
| n | % | n | % | n | % | ||
| It was easy to set up and use the VMU. | 41 | 5 | 12.2 | 5 | 12.2 | 31 | 75.6 |
| It was easy to use the remote control to record behaviors. | 22 | 2 | 9.1 | 10 | 45.5 | 10 | 45.5 |
| It was easy to place the VMU around our home to video behavior. | 41 | 8 | 19.5 | 5 | 12.2 | 28 | 68.3 |
| The VMU training was helpful. | 41 | 0 | 0.0 | 4 | 9.8 | 37 | 90.2 |
| It was easy to capture the behavior on video. | 40 | 10 | 25.0 | 6 | 15.0 | 24 | 60.0 |
| The VMU intruded on my privacy. | 41 | 26 | 63.4 | 7 | 17.1 | 8 | 19.5 |
| It was easy to transfer recordings via the internet. | 41 | 5 | 12.2 | 5 | 12.2 | 31 | 75.6 |
| Having the VMU in our home was acceptable. | 41 | 1 | 2.4 | 5 | 12.2 | 35 | 85.4 |
Note. Percentages may not sum to 100 due to rounding.
Table 3 displays bivariate relationships between responses to four questions about general satisfaction with the VMU (i.e., ease of use, privacy, capturing behavior, and acceptability) and dyad characteristics. Greater dementia severity was associated with caregiver perception that the VMU intruded on their privacy (mean FAST score=6.0±1.0 for agree/neutral responses vs. 5.4±1.1 for disagree responses, p=.050), and caregivers at study Site 1 found it easier to capture the behavior on video than caregivers at site 2 (81.8% for agree responses at site 1 vs. 33.3% for agree responses at site 2, p=.003). Caregiver age, caregiver gender, dyad relationship, rural status, caregiver education, and type of dementia were not significantly related to satisfaction with in-home videorecording (p>.05).
Table 3.
Relationships between Satisfaction with Video Monitoring Unit (VMU) and Dyad Characteristics (FamTechCare Caregivers)
| It was easy to set up and use the VMU | The VMU intruded on my privacy | It was easy to capture the behavior on video | Having the VMU in our home was acceptable | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Disagree/ neutral |
Agree | Disagree | Agree/ neutral |
Disagree/ neutral |
Agree | Disagree/ neutral |
Agree | |||||
| n=10 | n=31 | n=26 | n=15 | n=16 | n=24 | n=6 | n=35 | |||||
| Characteristic | Mean±SD | Mean±SD | p | Mean±SD | Mean±SD | p | Mean±SD | Mean±SD | p | Mean±SD | Mean±SD | p |
| Dementia severity | 5.4±1.2 | 5.7±1.0 | .355 | 5.4±1.1 | 6.0±1.0 | .050 | 5.6±1.1 | 5.6±1.1 | .912 | 5.5±1.2 | 5.6±1.1 | .753 |
| 62.7±15.1 | 64.9±11.5 | .695 | 63.1±12.7 | 66.6±11.5 | .511 | 66.1±10.4 | 63.4±13.7 | .691 | 66.8±13.0 | 63.9±12.3 | .755 | |
| n (%) | n (%) | p | n (%) | n (%) | p | n (%) | n (%) | p | n (%) | n (%) | p | |
| CG gender: | .694 | 1.000 | .729 | 1.000 | ||||||||
| Male | 2 (16.7) | 10 (83.3) | 8 (66.7) | 4 (33.3) | 4 (33.3) | 8 (66.7) | 2 (16.7) | 10 (83.3) | ||||
| Female | 8 (27.6) | 21 (72.4) | 18 (62.1) | 11 (37.9) | 12 (42.9) | 16 (57.1) | 4 (13.8) | 25 (86.2) | ||||
| Dyad relationship: | .697 | .484 | .150 | .648 | ||||||||
| Spouse | 7 (25.0) | 21 (75.0) | 17 (60.7) | 11 (39.3) | 13 (46.4) | 15 (53.6) | 5 (17.9) | 23 (82.1) | ||||
| Child | 2 (16.7) | 10 (83.3) | 9 (75.0) | 3 (25.0) | 2 (18.2) | 9 (81.8) | 1 (8.3) | 11 (91.7) | ||||
| Rural residence: | .660 | 1.000 | .210 | .567 | ||||||||
| Rural | 1 (14.3) | 6 (85.7) | 5 (71.4) | 2 (28.6) | 1 (14.3) | 6 (85.7) | 0 (0.0) | 7 (100.0) | ||||
| Not rural | 9 (26.5) | 25 (73.5) | 21 (61.8) | 13 (38.2) | 15 (45.5) | 18 (54.6) | 6 (17.7) | 28 (82.4) | ||||
| Study site: n (%) | .727 | .212 | .003 | 1.000 | ||||||||
| Site 1 | 6 (27.3) | 16 (72.7) | 16 (72.7) | 6 (27.3) | 4 (18.2) | 18 (81.8) | 3 (13.6) | 19 (86.4) | ||||
| Site 2 | 4 (21.1) | 15 (79.0) | 10 (52.6) | 9 (47.4) | 12 (66.7) | 6 (33.3) | 3 (15.8) | 16 (84.2) | ||||
| CG education: | .586 | .921 | .255 | 1.000 | ||||||||
| < Bachelor’s | 6 (33.3) | 12 (66.7) | 11 (61.1) | 7 (38.9) | 9 (52.9) | 8 (47.1) | 3 (16.7) | 15 (83.3) | ||||
| Bachelor’s | 2 (15.4) | 11 (84.6) | 8 (61.5) | 5 (38.5) | 3 (23.1) | 10 (76.9) | 2 (15.4) | 11 (84.6) | ||||
| ≥ Master’s | 2 (20.0) | 8 (80.0) | 7 (70.0) | 3 (30.0) | 4 (40.0) | 6 (60.0) | 1 (10.0) | 9 (90.0) | ||||
| Dementia type: | .751 | 1.000 | .438 | .613 | ||||||||
| Alzheimer’s | 6 (27.3) | 16 (72.7) | 14 (63.6) | 8 (36.4) | 10 (45.5) | 12 (54.6) | 3 (13.6) | 19 (86.4) | ||||
| Other diagnosed | 3 (18.8) | 13 (81.3) | 10 (62.5) | 6 (37.5) | 6 (40.0) | 9 (60.0) | 2 (12.5) | 14 (87.5) | ||||
| Unknown | 1 (33.3) | 2 (66.7) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 3 (100.0) | 1 (33.3) | 2 (66.7) | ||||
Note. Percentages may not sum to 100 due to rounding. Dementia severity=FAST score; CG=Caregiver; Rural=≥ 20 % rural, not rural=< 20 % rural; Bachelor’s=Bachelor’s degree, Master’s=Master’s degree; p-values were calculated for Wilcoxon rank-sum test for dementia severity and caregiver age, Fisher’s exact test for caregiver gender, dyad relationship, rural status, study site, caregiver education, and type of dementia.
Table 4 summarizes and compares satisfaction with interventionist feedback between the FamTechCare and attention control caregivers. Compared to the attention control caregivers, more FamTechCare caregivers agreed that feedback from the nurse was helpful (75.6% vs. 48.4%, p=.001), the ideas to change the behavior were good (78.1 vs. 54.8%, p=.017), and the care suggestions were effective (75.6% vs. 61.3%, p=.020). Neither group agreed it would have been better for the nurse to visit in person (7.3% and 14.7%, p=.427). The majority in both groups would recommend the interventions to others (80.5% and 81.8%, p=1.000).
Table 4.
Summary of Responses to Satisfaction with Intervention Questions (FamTechCare and Attention Control Caregivers)
| Statement | Group | N | Response | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | |||||||
| n | % | n | % | n | % | ||||
| Feedback from the nurse was helpful. | FTC | 41 | 4 | 9.8 | 6 | 14.6 | 31 | 75.6 | .001 |
| Control | 31 | 0 | 0.0 | 16 | 51.6 | 15 | 48.4 | ||
| Good ideas were given to change behavior. | FTC | 41 | 2 | 4.9 | 7 | 17.1 | 32 | 78.1 | .017 |
| Control | 31 | 0 | 0.0 | 14 | 45.2 | 17 | 54.8 | ||
| Care suggestions were effective. | FTC | 41 | 4 | 9.8 | 6 | 14.6 | 31 | 75.6 | .020 |
| Control | 31 | 0 | 0.0 | 12 | 38.7 | 19 | 61.3 | ||
| It would have been better for the nurse to visit in person. | FTC | 41 | 22 | 53.7 | 16 | 39.0 | 3 | 7.3 | .427 |
| Control | 34 | 14 | 41.2 | 15 | 44.1 | 5 | 14.7 | ||
| I would recommend this to others. | FTC | 41 | 1 | 2.4 | 7 | 17.1 | 33 | 80.5 | 1.000 |
| Control | 33 | 0 | 0.0 | 6 | 18.2 | 27 | 81.8 | ||
Note. Percentages may not sum to 100 due to rounding; FTC=FamTechCare; p-values were calculated for Fisher’s exact test; A number of control caregivers failed to complete the survey because they felt the questions were not applicable.
Utilization
FamTechCare caregivers received on average 9.1±2.5 (range = 2.0–12.0) out of a potential 12 weekly phone calls, totaling on average 132.8±94.4 minutes (range = 11.0–357.0). Similarly, attention control group received on average 8.5±3.1 calls (range = 1.0–12.0), totaling on average 136.0±110.4 minutes (range = 15.0–460.0). FamTechCare caregivers submitted on average 21.0±27.9 videos, totaling 149.6±310.7 minutes. The number of and duration of all the videos submitted over the 12-week study period varied among the dyads, ranging from one to 172 videos of less than 1 minute to 1729 minutes in duration. Two FamTechCare dyads submitted only one video each that were not reviewed by the expert team due to poor quality. The duration of videos was associated with duration of telephone calls; caregivers who sent more videos received more feedback even though this relationship was not statistically significant (ρ=.29, p=.062).
The associations between utilization variables and dyad characteristics are detailed in Table 5 for FamTechCare caregivers and Table 6 for attention control caregivers. For both groups, there were no statistically significant relationships between the number and duration of phone calls and caregiver age, caregiver gender, caregiver education, dyad relationship, rural residence, and type and severity of dementia. Nevertheless, male caregivers participated in more telephone calls than female caregivers in both the FamTechCare (10.3±1.5 vs. 8.6±2.7, p=.064) and attention control (9.8±3.0 vs. 8.0±3.0, p=.074) groups. However, gender differences in the duration of telephone calls were less pronounced.
Table 5.
Bivariate Relationships between Utilization and Dyad Characteristics (FamTechCare Caregivers)
| Phone calls | Videos | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of phone calls | Phone call duration (min) | Number of videos | Video duration (min) | ||||||
| Characteristic | N | ρ | p | ρ | p | ρ | p | ρ | p |
| Dementia severity | 42 | −.16 | .312 | −.03 | .836 | .06 | .714 | −.02 | .884 |
| Caregiver age | 42 | −.06 | .698 | .15 | .330 | .21 | .175 | .14 | .391 |
| N | Mean±SD | p | Mean±SD | p | Mean±SD | p | Mean±SD | p | |
| Caregiver gender | |||||||||
| Male | 12 | 10.3±1.5 | .064 | 135.9±94.1 | .879 | 17.7±13.8 | .709 | 121.3±224.3 | 1.000 |
| Female | 30 | 8.6±2.7 | 134.6±96.2 | 21.7±32.1 | 162.4±346.7 | ||||
| Dyad relationship | |||||||||
| Spouse | 29 | 9.3±2.5 | .290 | 141.5±90.8 | .195 | 22.2±32.7 | .921 | 166.5±352.4 | .876 |
| Child | 12 | 8.5±2.7 | 106.2±95.3 | 17.0±13.4 | 118.4±223.9 | ||||
| Rural residence | |||||||||
| Rural (≥ 20 % rural) | 7 | 9.1±3.0 | .946 | 112.5±78.1 | .558 | 15.3±12.1 | 1.000 | 52.4±41.8 | .503 |
| Not rural (< 20 % rural) | 35 | 9.1±2.5 | 139.4±97.8 | 21.6±30.2 | 170.3±341.3 | ||||
| Study site | |||||||||
| Site 1 | 22 | 9.1±2.4 | .800 | 149.9±81.1 | .117 | 28.5±36.1 | .038 | 257.6±408.8 | .002 |
| Site 2 | 20 | 9.2±2.8 | 118.5±107.0 | 11.8±10.1 | 33.0±28.9 | ||||
| Caregiver education | |||||||||
| < Bachelor’s degree | 19 | 9.5±2.4 | .433 | 145.2±100.5 | .455 | 24.5±39.6 | .675 | 259.2±446.9 | .814 |
| Bachelor’s degree | 13 | 9.4±1.7 | 135.0±74.6 | 16.0±9.9 | 53.6±43.3 | ||||
| ≥ Master’s degree | 10 | 8.0±3.5 | 115.5±111.4 | 18.8±15.2 | 70.6±53.1 | ||||
| Type of dementia | |||||||||
| Alzheimer’s | 22 | 9.0±2.6 | .898 | 141.5±87.8 | .558 | 24.2±36.7 | .519 | 224.0±418.4 | .651 |
| Other diagnosed | 17 | 9.4±2.3 | 135.9±107.7 | 17.6±13.3 | 75.9±87.5 | ||||
| Unknown | 3 | 8.7±4.2 | 82.0±68.2 | 9.7±9.9 | 36.1±31.2 | ||||
Note. p-values were calculated with Wilcoxon rank-sum test for caregiver gender, dyad relationship, rural residence, and study site; with Kruskal-Wallis test for caregiver education and dementia type; and with Spearman’s rho coefficient for dementia severity (i.e., mean FAST) and caregiver age.
Table 6.
Bivariate Relationships between Utilization and Dyad Characteristics (Attention Control Caregivers)
| Number of phone calls | Phone call duration (min) | ||||
|---|---|---|---|---|---|
| Characteristic | N | ρ | p | ρ | p |
| Dementia severity | 41 | −.17 | .297 | −.03 | .835 |
| Caregiver age | 41 | .16 | .304 | .02 | .890 |
| N | Mean±SD | p | Mean±SD | p | |
| Caregiver gender: n (%) | |||||
| Male | 12 | 9.8±3.0 | .074 | 149.0±122.3 | .639 |
| Female | 29 | 8.0±3.0 | 130.6±107.0 | ||
| Dyad relationship: n (%) | |||||
| Spouse | 26 | 9.0±3.1 | .121 | 145.6±97.2 | .171 |
| Child | 15 | 7.7±2.8 | 119.3±132.2 | ||
| Rural residence: n (%) | |||||
| Rural (≥ 20 % rural) | 14 | 7.6±3.5 | .240 | 112.1±122.4 | .164 |
| Not rural (< 20 % rural) | 27 | 9.0±2.8 | 148.3±103.9 | ||
| Study site: n (%) | |||||
| Site 1 | 20 | 8.9±3.6 | .187 | 179.3±111.6 | .009 |
| Site 2 | 21 | 8.2±2.5 | 94.7±94.2 | ||
| Caregiver education: n (%) | |||||
| < Bachelor’s degree | 15 | 8.6±3.1 | .842 | 83.3±52.7 | .068 |
| Bachelor’s degree | 20 | 8.3±3.1 | 161.0±124.7 | ||
| ≥ Master’s degree | 6 | 9.2±3.3 | 184.2±130.5 | ||
| Type of dementia: n (%) | |||||
| Alzheimer’s | 23 | 8.9±2.8 | .328 | 124.4±120.8 | .325 |
| Other diagnosed | 10 | 7.0±3.8 | 150.3±127.1 | ||
| Unknown | 8 | 9.4±2.5 | 151.3±45.0 | ||
Note. p-values were calculated with Wilcoxon rank-sum test for caregiver gender, dyad relationship, rural residence, and study site; with Kruskal-Wallis test for caregiver education and dementia type; and with Spearman’s rho coefficient for dementia severity (i.e., mean FAST) and caregiver age.
With respect to study sites there were some differences in utilization for both the FamTechCare and attention control groups. Even though the numbers of telephone calls were similar between sites for both groups, the calls were longer for Site 1 (179.3±111.6 vs. 94.7±94.2, p=.009, in the attention control group and 149.9± 81.1 vs. 118.5± 107.0, p=.117, in the FamTechCare group). FamTechCare caregivers at Site 1 sent more videos (28.5±36.1 vs. 11.8±10.1, p=.038) of longer durations (257.6±408.8 vs 33.0±28.9, p=.002) than FamTechCare caregivers at Site 2. For the FamTechCare group there were no statistically significant relationships between the number and duration of videos and caregiver age, caregiver gender, caregiver education, dyad relationship, rural residence, and type and severity of dementia.
Feasibility
Four themes emerged from the evaluation of feasibility of the FamTechCare intervention by the expert team: (1) Clinician and Caregiver Support; (2) Barriers; (3) Modifications; and, (4) Collaboration.
Clinician and caregiver support.
Seven of the eight experts noted that the videos provide a better understanding of dyad challenges. Specifically, videos allow for events to be captured and reviewed that are better seen than verbally described. Experts believed that the caregivers would not have been able to provide the same amount of detail in conversation that the video allows. One geriatric nurse practitioner related the videos back to her clinical practice, noting that “video data definitely helped [provide advice to caregivers]…it was way different than when we see patients in clinic and hear them tell stories.” Later the same clinician noted that “…the videos did enlighten the caregiving process for me as a clinician and helped me provide more helpful feedback.” Others commented that behavior of persons living with dementia is often different at home from what the provider sees in clinic, so advice based on home behavior is preferable. Additionally, experts reported the value of videos for overcoming concerns related to the accuracy of verbal reports due to concerns related to caregiver bias and/or recall.
The experts also identified the benefits of video providing more comprehensive information about specific care situation and the environment. Physically seeing inside the home was critical to better understand the context of caregiving challenges. One nurse researcher noted that “being able to see into the home environment and the behavior of the person with dementia added a dimension you wouldn’t get by just talking to the caregiver.” Experts gave specific examples related to identifying fall risks, extraneous noise, and surroundings during meals. One expert described that “the caregiver complained that the person with dementia was repetitive about asking for coffee and couldn’t find the coffee when prompted.” The video showed a new coffee maker that was recently purchased. The team suggested using the old, traditional coffee maker that the person with dementia could recognize and knew how to use. It was noted that this video allowed for individualized and situation specific feedback that otherwise could not have been provided.
Over half of the experts also noted the benefit of interventions developed by an interdisciplinary team of dementia care experts who have varied backgrounds and experiences. As one nurse researcher explained, “The diverse experience of the panel and expertise enhanced the intervention. The panel brought differing suggestions which added to strengths and provided families with multiple approaches and resources rather than a one size fit most approach.”
Barriers.
All experts asserted that the biggest barrier to the FamTechCare intervention was the inconsistent quality of the videos submitted. Experts noted that caregivers struggled to create high quality videos due to challenges in physically capturing the moment, the complexity of the technology, and in identifying which care challenges to capture and send. The experts always noted that better videos led to better advice. One expert described that although “[videos allowed] better view within the home, the videos are still not capturing everything.”
Some experts found the technology was too complex and required more training; however, most noted that the challenge was not with the mechanics of using the iPad but rather in getting the correct timing to capture the care challenge. Experts were concerned that the buffering component of the application, that allowed for capture of antecedent behavior, was not consistently helpful because the iPad would be in the wrong room, positioned poorly, or the behavior of the person living with dementia would be so extreme that the caregiver was unable to trigger the recording. An expert explained, “Many of the moments that are most challenging to caregivers are the most difficult to capture.”
Half of the experts described privacy as a barrier to receiving quality videos and expressed concern that the recordings occasionally appeared staged rather than natural. One expert stated, “Caregivers still want to control the story they tell and don’t always want to send videos that make themselves or the person with dementia look bad.” Another expert expressed concerns that “people behave differently on camera. They do not react the same because they know they are being filmed.” Experts also suggested that the privacy concerns with the FamTechCare intervention may lessen with future generations as technology and sharing videos on social media platforms become more integrated into daily life.
About half of the experts interviewed agreed that the intervention should be provided by the primary care provider of persons living with dementia to increase continuity of care. The experts noted barriers to this model that included lack of nursing/social work staff to screen videos, challenges assembling an interdisciplinary team to review videos, costs of equipment, and timeliness of providing video feedback within current practices. One expert noted “Currently FamTechCare is doable. It’s not too much work, but the question is who will pay for and manage it.” However, another expert asserted that it cannot be streamlined into clinical practice because “providers don’t have time and often don’t care about dementia…it’s unrealistic to think providers would be interested or have time for videos.” This expert later described FamTechCare as more feasible outside the traditional healthcare system and more as a community-based resource that does not operate within the healthcare system.
Due to these concerns about feasibility, some experts suggested that FamTechCare should be tested with a community-based partnership. One expert noted, “It’s not enough to say call [community resource], we need to help coordinate and take the work off the caregiver to organize and find resources.” Experts disagreed about how the intervention should interface with the person living with dementia’s care team. Some experts suggested that the FamTechCare team provide a written report of suggestions to individual providers while other experts asserted that the videos should be viewed by the providers themselves.
Modifications.
Suggested modifications to the FamTechCare intervention focused primarily on providing additional training to the caregivers about both the technology and the goals of the intervention. Experts suggested that training should focus more on capturing high-quality videos of the caregiver’s priority care situations, and that positive reinforcement should be given when caregivers send these types of videos. One expert felt additional training in each caregivers home would be beneficial in order to identify where to place the iPad as well as providing additional training on how to physically capture the video, including using the Bluetooth remote. Some experts felt the VMU equipment itself should be altered with ideas including mounting multiple videorecording devices within the home, finding a better iPad stand so caregivers do not hold the iPad to record, and using the Behavior Capture application on personal smartphones to create the videos.
Experts also differed on views related to identifying caregiver-person living with dementia dyads who would benefit from the FamTechCare intervention. Some felt that participants should be better screened to assure that only dyads with significant care challenges amenable to the intervention are included. Other experts asserted that any interested dyads could benefit and should be included. Another expert suggested that FamTechCare is more appropriate for rural rather than urban populations in that “videos are most helpful for people who are remote and physically can’t get to a provider…for rural populations the videos would probably be worth it [costs of implementation].”
Collaboration.
The experts also discussed their role on the expert panel and what the video review panel should look like going forward. Six of the eight experts strongly felt that an interdisciplinary team approach to video review was needed and that the intervention would be significantly limited if videos were reviewed by only one person. A social worker stated that “a positive aspect was having a team to talk through the problems with and share options together; we would not have that synergy with only one person watching. Families also liked having several experts; it made placing the camera at home more worthwhile.”
The majority of the experts identified that a social worker and a healthcare provider with prescribing privileges were essential for reviewing the videos and providing feedback. A social worker was considered critical to assist the family with community resources and family dynamics. A healthcare provider with a background in psychiatry or neurology was preferred. Experts noted that a nurse practitioner was ideal because they could fill both the provider and nursing roles by delivering medical and nursing knowledge. If the healthcare provider was not a nurse practitioner, then experts said a nurse should be added to the review team. An occupational therapist was also identified as a needed expert. The experts also discussed how a certain level of expertise is required, remarking that, “It’s not just enough to connect with a nurse or a social worker; the caregiver needs a professional that would actually be helpful.”
Discussion
The majority of study participants were satisfied with the intervention, both the FamTechCare video-based and telephone-support feedback, reflecting the needs of family members caring for a loved one with dementia at home. Most notably, the attention control group found the phone-call based intervention effective and satisfying, which emphasizes the need for support beyond usual care for the growing population of dementia family caregivers. However, more caregivers in the FamTechCare group found the feedback effective and satisfying, reflecting added benefit from the video-based feedback. These findings correspond to the study’s primary outcome findings of significantly greater reductions in caregiver depression and increases in competence for FamTechCare caregivers compared to attention-control caregivers (Williams et al., 2019).
The primary outcome analysis also determined greater effects on reducing depression, both statistically and clinically, for rural caregivers in the FamTechCare group (Williams et al., 2019). This was similarly reflected in the current satisfaction analysis, although non-significantly (p=.567), in which 100% of rural FamTechCare caregivers reported intervention acceptability while 82.4% of non-rural caregivers reported intervention acceptability. However, rural caregivers did not utilize the intervention more. They sent less videos which equated to a smaller total duration of videos. This finding may highlight the experts’ perception that the quality rather than the quantity of videos has the greatest impact on the quality of expert advice.
Overall utilization was very similar in the FamTechCare and attention control telephone-support groups. Differences between the groups and study sites occurred only for the number and duration of videos submitted. Experts at both study sites identified a need for better quality videos. Time spent on technology training did not differ between sites; 50 minutes on average (SD = 17 minutes) at Site 1 and 52 minutes on average (SD = 15 minutes) at Site 2. With respect to satisfaction, caregivers at Site 1 also reported finding it easier to capture behaviors on video compared to caregivers at Site 2. The two sites followed the same protocols and had monthly meetings over the entire 4-year trial to ensure intervention fidelity, although additional factors not recognized by the study team may have contributed to these slight differences between sites. Future research should determine the most effective methods to implement technology training. No other characteristics of the caregivers or persons living with dementia in the dyads correlated with utilization. This finding suggests that the intervention was acceptable to all types of caregiver-person living with dementia dyads.
Caregiver satisfaction and utilization were high. However, more caregivers of persons living with dementia with severe dementia reported that the intervention presented a privacy issue. This may be due to concern about recording loved ones during very sensitive care situations, such as personal care and behavioral and psychological symptom management, that are more common challenges in advanced dementia. However, caregivers who noted privacy concerns and those caring for persons with more advanced dementia submitted as many videos as other caregivers, possibly indicating that the need for support outweighed their privacy concerns. The expert team also noted privacy issues focused on capturing intimate care moments and noted that caregivers often sent videos that were unrelated to the caregiver’s verbal report of their greatest difficulties. The experts suggested a need for more training and direction to caregivers for capturing their most challenging moments in order to get the most effective feedback.
This study did not find the technology be overly challenging for older adults. Most participants did not report issues with the technology; although, this could be because the participants who volunteered were comfortable using or learning to use an iPad. Based on our time records, an average of 8.4 minutes (range 0–90 minutes) was spent assisting the families with technology challenges after the initial training. The most common challenge was related to the software updates automatically issued to the iPads. Some updates could be ignored until the end of the study; however, others made changes to the study-specific settings or forced caregivers to log into the iPad in a way that was not addressed in training. One of the greatest caregiver technology challenges was the use of the Bluetooth remote to initiate recordings. Many caregivers failed to use the remote control to trigger videos possibly reflecting a lack of comfort with this Bluetooth technology and the remote-control interface.
The expert panel described the FamTechCare intervention as useful, particularly in its ability to provide detailed data to support individualized guidance for caregivers. Interventions that are individualized to the caregiver-person living with dementia dyad and focus both directly and indirectly on challenging behaviors in the physical and social environment have the best effect on person living with dementia behavior and caregiver outcomes (Caspar, Davis, Douziech, & Scott, 2018; Gilhooly et al., 2016). The FamTechCare intervention meets these criteria by providing dementia care experts video data during dyadic interactions in the home. The FamTechCare intervention overcomes reliance on caregiver recall, that may limit the information clinicians use to form recommendations. The expert panel confirmed that the FamTechCare intervention effectively allowed for tailoring interventions to specific needs and that seeing the dyad inside the home fostered better guidance.
The expert panel also expressed concerns related to the feasibility of the current FamTechCare intervention, specifically its readiness for adoption into the healthcare system. Future research is needed that focuses on adapting the FamTechCare intervention for use within community and/or healthcare settings. The expert panel identified a need for modifications to the technology and training in order to capture optimal content and quality of video data. Prior to the FamTechCare clinical trial, a pilot study was completed with older adults using an iPad Mini or iPod touch and the Behavior Capture application in which the older adults were evaluated completing the 10 steps (e.g., open app, position device, change front-back camera setting) needed to accomplish the videorecording (Williams, Pennathur, Bossen, & Gloeckner, 2016). Based on the evaluations, it was concluded that an iPad Mini would be the best device, and alterations were made to the application to simplify the upload process. Following the pilot study, changes to the application user interface and the instruction manual were also completed. The satisfaction survey indicated that caregivers found the use of the technology acceptable, indicating that the quality of the videos may not be solely related to technologic challenges.
Future research should evaluate ways to overcome the difficulties of creating high quality videos and identify specific ways to aide caregivers in capturing the encounters they perceive as the most challenging. Being unable to consistently capture these most challenging care situations is a current limitation to the FamTechCare intervention. Our study emphasized positive reinforcement and a nonjudgmental approach to build trust with caregivers. However, caregivers may have still felt uncomfortable submitting videos of certain intimate or uncomfortable care situations. Caregivers sometimes submitted videos of care situations other than those they originally identified as most challenging, we found that allowing caregivers to select challenging care situations for review that may change over the 3-month study, best met their need for support.
Evaluating the cost-effectiveness of the intervention is perhaps one of the most important aspects to understanding the future feasibility and implementation of the FamTechCare intervention. The FamTechCare intervention unsurprisingly cost more than the telephone support intervention with over two-thirds of the costs being equated to the VMU equipment and expert team salaries. However, the incremental cost-effectiveness ratios for caregiver depression and competence demonstrated that the FamTechCare intervention does remain within a dementia caregivers’ willingness-to-pay threshold making the intervention cost-effective. The methods and results of the cost-effectiveness analysis are reported elsewhere (Shaw, Williams, Lee, & Coleman, In Press).
A limitation of our study was limited diversity in the sample. We enrolled mostly older non-Hispanic participants in dyads including spouses of persons with moderate-stage dementia. This lack of variance may have limited power to detect differences due to dyad characteristics. In relation to privacy concerns, dyads that self-selected to enroll in the study were aware that videorecording was required yet found it acceptable to enroll. This likely influenced the high ratings of utilization and satisfaction. Fewer attention control caregivers (n=33) returned the satisfaction questionnaire than FamTechCare caregivers (n=41). This may have influenced the mean ratings of satisfaction by the control group. Lastly, 9 persons living with dementia had multiple caregivers interested in participating and thus these 9 persons living with dementia were included in multiple dyads. All caregivers completed their own satisfaction questionnaire. However, for utilization, some caregivers completed their own phone calls while others completed them as a group. In these multiple caregiver situations, the video time was applied to each caregiver as the VMU stayed with the person living with dementia. Thus, due to the multi-caregiver groups the analysis was not completely independent.
The correlation between videos submitted and amount of feedback received suggests that recording videos was effective in eliciting feedback. Failure of some caregivers to consistently submit weekly videos may indicate the burden of study participation, competing priorities, or a lack of need for this frequent feedback. Some trends in the data should be evaluated in ongoing research (e.g., non-significant correlations between age and videos submitted and between male caregiver gender and number of calls received).
Conclusion
Participants in the FamTechCare clinical trial were highly satisfied with the intervention, and even the attention control group caregivers reported benefit from the phone-based intervention. However, satisfaction was higher for the video-based intervention group. The expert panel found the video data valuable for providing tailored feedback and noted that video data improves the ability to provide needed caregiver support. We did not find significant relationships between dyad characteristics (i.e. age, gender, relationship) and satisfaction and utilization ratings, indicating the value of the intervention was similar across numerous dyads. Future research should replicate this intervention and evaluate the optimal frequency for video submission and feedback to optimize support for family caregivers at home. Based on this research, FamTechCare provides acceptable and easy-to-use caregiver support that was adopted by participants. With these findings and those of enhanced caregiver health and well-being outcomes from the intervention (Williams et al., 2019), future research should test implementation of FamTechCare across care settings.
Footnotes
Declaration of interest statement
The Authors declare that there is no conflict of interests.
References
- Alzheimer’s Association. (2019). 2019 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 15(3), 321–387. doi: 10.1016/j.jalz.2019.01.010 [DOI] [PubMed] [Google Scholar]
- American Association of Retired Persons. (2016). Caregivers & Technology: What they want and need. Retrieved January 25, 2019 from http://www.aarp.org/content/dam/aarp/home-and-family/personal-technology/2016/04/Caregivers-and-Technology-AARP.pdf
- Bossen AL, Kim H, Williams KN, Steinhoff AE, & Strieker M (2015). Emerging roles for telemedicine and smart technologies in dementia care. Smart Homecare Technology and Telehealth, 3, 49–57. doi: 10.2147/shtt.S59500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspar S, Davis ED, Douziech A, & Scott DR (2018). Nonpharmacological management of behavioral and psychological symptoms of dementia: What works, in what circumstances, and why? Innovations in Aging, 2(1). doi: 10.1093/geroni/igy001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeken F, Rezo A, Hinz M, Discher R, & Rapp MA (2019). Evaluation of technology-based interventions for informal caregivers of patients with dementia: A meta-analysis of randomized controlled trials. The American Journal of Geriatric Psychiatry, 27(4), 426–445. doi: 10.1016/j.jagp.2018.12.003 [DOI] [PubMed] [Google Scholar]
- Egan KJ, Pinto-Bruno AC, Bighelli I, Berg-Weger M, van Straten A, Albanese E, & Pot AM (2018). Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: A systematic review. Journal of the American Medical Directors Association, 19(3), 200–206.e201. doi: 10.1016/j.jamda.2017.10.023 [DOI] [PubMed] [Google Scholar]
- Elo S, & Kyngas H (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Feast A, Moniz-Cook E, Stoner C, Charlesworth G, & Orrell M (2016). A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. International Psychogeriatrics, 28(11), 1761–1774. doi: 10.1017/s1041610216000922 [DOI] [PubMed] [Google Scholar]
- Gilhooly KJ, Gilhooly ML, Sullivan MP, McIntyre A, Wilson L, Harding E, … Crutch S (2016). A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatrics, 16, 106. doi: 10.1186/s12877-016-0280-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood J, Walker N, McDonagh L, Rait G, Walters K, Iliffe S, … Davies N (2018). Internet-based interventions aimed at supporting family caregivers of people with dementia: Systematic review. Journal of Medical Internet Research, 20(6), e216. doi: 10.2196/jmir.9548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Monin JK, & Schulz R (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24(3), 681–695. doi: 10.1037/a0016355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter CN, Miller MC, Lane M, Cornman C, Sarsour K, & Kahle-Wrobleski K (2016). The influence of caregivers and behavioral and psychological symptoms on nursing home placement of persons with Alzheimer’s disease: A matched case–control study. SAGE Open Med, 4, 2050312116661877. doi: 10.1177/2050312116661877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Comas-Herrera A, Knapp M, Guerchet M, & Karagiannidou M (2016). World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia. Retrieved January 25, 2019 from https://www.alz.co.uk/research/WorldAlzheimerReport2016.pdf [Google Scholar]
- Quinn C, Nelis SM, Martyr A, Victor C, Morris RG, & Clare L (2019). Influence of positive and negative dimensions of dementia caregiving on caregiver well-being and satisfaction with life: Findings from the IDEAL study. The American Journal of Geriatric Psychiatry. doi: 10.1016/j.jagp.2019.02.005 [DOI] [PubMed] [Google Scholar]
- Reisberg B (2007). Global measures: Utility in defining and measuring treatment response in dementia. International Psychogeriatrics, 19(3), 421–456. doi: 10.1017/s1041610207005261 [DOI] [PubMed] [Google Scholar]
- Sclan SG, & Reisberg B (1992). Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. International Psychogeriatrics, 4(1), 55–69. doi: 10.1017/S1041610292001157 [DOI] [PubMed] [Google Scholar]
- Scott JL, Dawkins S, Quinn MG, Sanderson K, Elliott KE, Stirling C, … Robinson A (2016). Caring for the carer: A systematic review of pure technology-based cognitive behavioral therapy (TB-CBT) interventions for dementia carers. Aging and Mental Health, 20(8), 793–803. doi: 10.1080/13607863.2015.1040724 [DOI] [PubMed] [Google Scholar]
- Shaw CA, Williams KN, Lee RH, & Coleman CK (In Press). Cost-effectiveness of a telehealth intervention for in-home dementia care support: Findings from the FamTechCare clinical trial. Research in Nursing and Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topo P (2008). Technology studies to meet the needs of people with dementia and their caregivers: A literature review. Journal of Applied Gerontology, 28(1), 5–37. doi: 10.1177/0733464808324019 [DOI] [Google Scholar]
- Waller A, Dilworth S, Mansfield E, & Sanson-Fisher R (2017). Computer and telephone delivered interventions to support caregivers of people with dementia: A systematic review of research output and quality. BMC Geriatrics, 17(1), 265. doi: 10.1186/s12877-017-0654-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Blyler D, Vidoni Eric D, Shaw C, Wurth J, Seabold D, … Van Sciver A (2018). A randomized trial using telehealth technology to link caregivers with dementia care experts for in‐home caregiving support: FamTechCare protocol. Research in Nursing and Health, 41(3), 219–227. doi: 10.1002/nur.21869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Pennathur P, Bossen A, & Gloeckner A (2016). Adapting telemonitoring technology use for older adults. Research in Gerontological Nursing, 9(1), 17–23. doi: 10.3928/19404921-20150522-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams KN, Perkhounkova Y, Shaw CA, Hein M, Vidoni ED, & Coleman CK (2019). Supporting family caregivers with technology for dementia home care: A randomized controlled trial. Innovations in Aging, 3(3), 1–19. doi: 10.1093/geroni/igz037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2012). Dementia: A Public Health Priority. Retrieved January 25, 2019 from https://www.who.int/mental_health/publications/dementia_report_2012/en/
- World Health Organization. (2017). Global Action Plan on the Public Health Response to Dementia 2017–2025. Retrieved July 17, 2019 from https://www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/


