Abstract
Introduction:
Individuals with social anxiety disorder (SAD) are at elevated risk of loneliness, yet little research has examined loneliness in this population. Cognitive-behavioral group therapy (CBGT) and mindfulness-based stress reduction (MBSR) have demonstrated efficacy in treating SAD, yet research has not examined whether they lead to reductions in loneliness.
Methods:
This sample comprised 108 individuals with SAD who were randomized to CBGT, MBSR, or a waitlist control (WL); WL participants were re-randomized to CBGT or MBSR following WL. Assessments were completed pre- and post-treatment, and 3-, 6-, 9-, and 12-month follow-up assessments.
Results:
Compared to WL, individuals in CBGT and MBSR were less lonely at post-treatment; there was no difference between treatments after treatment or during follow-up. Greater reductions in social anxiety from pre- to post-treatment predicted lower levels of loneliness during follow-up. Greater reductions in loneliness from pre- to post-treatment also predicted lower levels of social anxiety during follow-up.
Discussion:
Individuals who experience reductions in their social anxiety during treatment may also feel less lonely following treatment. Reductions in loneliness also lead to improvements in social anxiety. Future research should continue to examine the relationship between social anxiety and loneliness and how interventions for SAD may help reduce loneliness.
Keywords: social anxiety, loneliness, CBGT, MBSR
Introduction
Loneliness refers to the painful experience of feeling socially disconnected from others. Loneliness is a rising public health concern, and rates of loneliness have increased in recent years (Chaterjee, 2018). Loneliness develops when there is a discrepancy between an individual’s desired and actual social relationships (Peplau & Perlman, 1982). It affects people of all ages and is related to feeling that one does not have a core person with whom to share one’s life, lacks familial and friend relationships, or is not included as a part of a larger network (e.g., group, school, team, identity; S. Cacioppo, Grippo, London, Goossens, & Cacioppo, 2015).
Loneliness is related to a variety of physical and psychological health problems, including cognitive decline, obesity, alcoholism, anxiety, depression, suicidality, and premature mortality (S. Cacioppo et al., 2015). Although loneliness has been associated with all mental disorders, it is most strongly associated with social anxiety disorder (SAD; Meltzer et al. 2013). Importantly, individuals with social anxiety seem to be at particular risk of experiencing loneliness, possibly due to their fears of negative evaluation and frequent experiences of social isolation and rejection (Alden & Taylor, 2004; J. Cacioppo & Hawkley, 2005; Fung et al., 2017; Teo et al., 2013). A recent longitudinal study by Lim, Rodebaugh, Zyphur, and Gleeson (2016) found that social anxiety was a unique prospective predictor of loneliness, suggesting that social anxiety may have a role in the onset and maintenance of loneliness. Because loneliness affects both quality of life and longevity (S. Cacioppo et al., 2015), it is critically important to identify ways to reduce the burden of loneliness among at-risk individuals, as rates of loneliness continue to rise.
Research on interventions for loneliness indicates targeting social cognitions is an important treatment strategy to reduce loneliness. A meta-analysis by Masi, Chen, Hawkley, and Cacioppo (2011) reviewed four intervention strategies that may indirectly target loneliness: improving social skills, enhancing social support, increasing opportunities for social contact, and addressing maladaptive social cognitions. They noted that most interventions for loneliness studied to date have only been examined through single-group and nonrandomized studies; however, of the few studies that were randomized comparisons, the interventions that most effectively led to reductions in loneliness were those that used strategies that help individuals challenge their maladaptive social cognitions (Masi et al., 2011). Their review also highlighted that group interventions and interventions that enhance opportunities for social interactions have potential for success (Masi et al., 2011). More recent reviews by S. Cacioppo and colleagues (2015) and Mann and colleagues (2017) similarly echoed Masi and colleagues’ conclusions, emphasizing that evidence-based group treatments that target maladaptive social cognitions may be most effective at reducing loneliness. This is consistent with current theories on the etiology of loneliness, which argue that maladaptive social cognitions and negative interpersonal appraisals lead individuals to avoid opportunities for social connection, with loneliness as a result (Käll et al., 2020; Masi et al., 2011). To more directly test these ideas, what is needed is more rigorous treatment outcome research, such as randomized controlled trials (RCTs), to compare interventions to reduce loneliness, especially among at-risk clinical populations.
Despite socially anxious individuals being at great risk for loneliness, and the apparent relevance of social cognitions as a central component underlying loneliness, research examining loneliness among treatment-seeking individuals with SAD or the effects of treatment for SAD on loneliness is lacking. Cognitive-behavioral Group Therapy (CBGT) and Mindfulness-Based Stress Reduction (MBSR) have both demonstrated efficacy as treatments for SAD (e.g., Goldin et al., 2016; Kaplan, Swee, & Heimberg, 2018). However, no research to date has examined loneliness as an outcome of these treatments. Since interventions designed to address maladaptive social cognitions, such as cognitive behavioral therapy (CBT) in either individual or group settings, have demonstrated the largest effect sizes and greatest potential for reducing loneliness (Masi et al., 2011), it is expected that CBGT for SAD would effectively improve loneliness. It is likely that as socially anxious individuals learn to challenge their negative thoughts and begin to engage more fully with their social world through exposure, their experiences of loneliness will decrease. Reductions in loneliness may also facilitate improvements in social anxiety, as individuals avoid fewer social situations and broaden their social opportunities (Haslam et al., 2019). Additionally, mindfulness interventions teach individuals to identify and approach their thoughts with acceptance and non-judgement and reduce their emotional reactivity to thoughts and images (Goldin & Gross, 2010; Kabat-Zinn 1990; Kabat-Zinn & Santorelli, 1993). Thus, it likely that mindfulness-based treatments would also help reduce loneliness (S. Cacioppo et al., 2015).
The Present Study
Due to the limited number of RCTs evaluating interventions to reduce loneliness, there is a pressing need to increase our understanding of the existing interventions that can effectively reduce loneliness among at-risk individuals. The goal of the present study was to examine whether two efficacious treatments for SAD, CBGT and MBSR, lead to reductions in loneliness among treatment-seeking individuals with SAD. We hypothesized that compared to a waitlist control (WL), both CBGT and MBSR would reduce feelings of loneliness at post-treatment. In addition, we hypothesized that both treatments would reduce loneliness at follow-up assessments. We did not hypothesize a difference between treatments, based on findings that both CBGT and mindfulness-based treatments effectively reduce social anxiety and many other outcomes (Arch et al., 2013; Goldin et al., 2016; Hoffman, Sawyer, Witt, & Oh, 2010; Kocovski, Segal, & Battista, 2009). Further, since both treatments were found to lead to significant improvements in social anxiety at post-treatment that were maintained throughout the year following treatment (Goldin et al., 2016), we did not expect to see a difference in loneliness reduction between these treatments at post-treatment or during the follow-up period.
In addition to identifying evidence-based treatments that reduce loneliness, it is critical to identify potential predictors of reductions in loneliness. Therefore, we also sought to examine whether reductions in social anxiety during treatment predict reductions in loneliness at follow-up assessments. We hypothesized there would be a significant main effect of social anxiety change during treatment, such that reduction in social anxiety from pre- to post-treatment would predict lower levels of loneliness during follow-up. We also hypothesized that there would be a main effect of time, such that loneliness would decrease across follow-up assessments. Finally, we hypothesized that there would be a significant interaction between social anxiety change from pre- to post-treatment and time, such that greater reductions in social anxiety from pre- to post-treatment would be associated with greater reductions in loneliness across follow-up time points. As an exploratory aim, we additionally examined whether reductions in loneliness from pre- to post-treatment would similarly predict reductions in social anxiety during follow-up.
Method
Procedure
Participants were drawn from a sample of individuals with SAD who participated in an RCT that investigated the relative efficacy of CBGT and MBSR compared to WL (Goldin et al., 2016). Participants were recruited through clinical referrals and community listings and first completed a telephone screening for eligibility prior to being invited for an in-person diagnostic interview to assess current and lifetime Axis I disorders and clinician-rated severity. All participants provided informed consent and then completed in-person interviews with clinical psychology graduate students or doctoral level clinical psychologists. Prior to treatment, participants also completed an online battery of questionnaires.
Individuals were eligible if they met Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV; American Psychiatric Association, 1994) criteria for generalized SAD as their principal diagnosis, based on the Anxiety Disorders Interview Schedule for the DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). The ADIS-IV-L is a structured diagnostic interview used to assess current and lifetime diagnoses of anxiety disorders according to the DSM-IV and provides a clinician severity rating for each diagnosis on a scale from 0 to 8. The ADIS-IV-L assesses anxiety disorders, as well as current mood, somatoform, and substance use disorders. To meet criteria for generalized SAD, participants had to endorse greater than moderate fear of five or more distinct social situations on the ADIS-IV-L. The ADIS-IV-L has demonstrated adequate interrater reliability (Brown, Di Nardo, Lehman, & Campbell, 2001). As part of the original study (Goldin et al., 2016), clinicians reviewed 20% of the interviews to assess interrater reliability, and there was 100% agreement with the initial diagnosis and rating. Additionally, participants had to obtain a score greater than 60 on the Liebowitz Social Anxiety Scale-Self Report (LSAS-SR; Fresco et al., 2001; Liebowitz, 1987) to be included in the study (i.e., the clinical cutoff score on the LSAS-SR for generalized SAD; Rytwinski et al., 2009).
Exclusion criteria included any pharmacotherapy or psychotherapy in the past year or any experience with the two treatments of interest, including any CBT for anxiety in the past two years as well as any previous experience with MBSR, participation in long-term meditation retreats, or meditation practice for greater than 10 minutes at least three times a week. Additionally, individuals were excluded if they endorsed any history of neurological disorders, cardiovascular disorders, thought disorders, eating disorders, or bipolar disorder, as well as significant symptoms of post-traumatic stress disorder, obsessive-compulsive disorder, major depressive episode in the past month, or any current substance or alcohol abuse or dependence.
Participants
Our treatment sample included 108 treatment-seeking individuals with SAD (55.6% female, Mage = 32.7, SD = 8.0) who were randomly assigned to CBGT (n = 36), MBSR (n = 36), or WL (n = 36). Individuals in the WL condition were randomized to complete CBGT (n = 18) or MBSR (n =18) upon completion of WL. Of the 108 individuals included in the treatment sample, 8 individuals dropped from the study and identified various reasons for not wanting to participate (e.g., anxiety during group exposures, travel distance, time commitment, moved out of the area, etc.). As a result, 100 individuals were included in the post-treatment sample (including treated WL individuals, CBGT: n = 50, MBSR: n = 50).
In addition to completing assessments at pre-treatment, participants additionally completed online self-report assessments at post-treatment/post-WL, and at 3-month, 6-month, 9-month, and 12-month follow-up time points. Eighty-one participants completed at least one assessment during the follow-up period. There were 281 observations across the 81 individuals who participated in follow-up assessments. Attrition analyses were conducted to determine whether social anxiety at pre- or post-treatment, loneliness at pre- or post-treatment, or treatment condition were associated with number of follow-up assessments completed, but results indicated that they were not (p’s > .05).
Interventions
CBGT was administered by PhD-Level psychologists; group leaders were trained by Richard Heimberg, in order to implement his CBGT for SAD protocol (Heimberg & Becker, 2002). CBGT comprised four treatment components: 1) orientation to CBT and psychoeducation about CBT and SAD, 2) learning cognitive restructuring skills to identify and challenge one’s negative, automatic thoughts, 3) engaging in in-session and in-vivo exposures to feared social situations either implemented during session or as homework assignments between sessions, and 4) relapse prevention and termination. CBGT group members additionally used selected portions of Hope, Heimberg, and Turk’s (2010) client workbook to facilitate learning with the CBGT protocol. CBGT groups consisted of six people who met for twelve 2.5 hour weekly sessions. Adherence ratings indicated that CBGT therapists administered the treatment per protocol (see Goldin et al., 2016).
MBSR was administered by a master’s level certified MBSR instructor at the University of Massachusetts Center for Mindfulness, following the outline of the standard curriculum for MBSR created by John Kabat-Zinn (1993). Of note, this MBSR protocol expanded the one-day meditation retreat included in Zinn’s original curriculum to be conducted over four sessions, so that the total treatment was similarly comprised of twelve 2.5 hour weekly sessions, to match the length and duration of CBGT. This treatment emphasizes the use of mindfulness and acceptance strategies to notice and non-judgmentally accept anxious thoughts, feelings, and behavior (Kabat-Zinn & Santorelli, 1993). MBSR group members were additionally given Stahl and Goldstein’s (2010) mindfulness workbook, to facilitate mindfulness practice in session and at home. Adherence ratings indicated that the MBSR therapist administered the treatment per protocol (see Goldin et al., 2016).
Measures
The Liebowitz Social Anxiety Scale-Self-Report (LSAS-SR; Fresco et al., 2001; Liebowitz, 1987) is the self-report version of a widely used 24-item measure of social anxiety. The LSAS-SR includes 11 items that assess reactions to social interactions (e.g., going to a party) and 13 items that assess reactions to performance situations (e.g., acting, performing, or giving a talk in front of an audience). Individuals rate their level of fear and avoidance during the past week for each of the situations, using a 4-point scale ranging from 0 (none/never) to 3 (severe/usually). The ratings are summed for a total score, ranging from 0 to 144. The LSAS-SR has demonstrated good reliability and strong construct validity with other commonly used clinician and self-report measures of social anxiety and avoidance (Baker, Heinrichs, Kim, & Hoffmann, 2002; Fresco et al., 2001; Levin, Marom, Gur, Wechter, & Hermesh, 2002; Oakman, Van Ameringen, Mancini, & Farvolden, 2003; Rytwinski et al., 2009). To evaluate treatment-related change in social anxiety, we calculated a social anxiety change score by subtracting each individuals’ LSAS-SR post-treatment score from their LSAS-SR pre-treatment score. In our sample, the LSAS-SR demonstrated excellent internal consistency (α = .92).
The UCLA-8 Loneliness Scale (ULS-8; Hays & DiMatteo, 1987) is a short version of the UCLA Loneliness Scale (ULS; Russel, 1982; Russell, 1996; Russell, Peplau, & Cutrona, 1980; Russell, Peplau, & Ferguson, 1978), the most widely used measure of loneliness and social isolation. The ULS-8 has 8 items (e.g. “I lack companionship,” “There is no one I can turn to”), rated on a 4-point Likert-type scale, on which individuals endorse how much they agree with each item, from 1 (I have never felt this way) to 4 (I have often felt this way). Two of the items from the original version of the ULS (“I am an outgoing person,” and “I can find companionship when I want it”) were reworded in the revised version of the scale to reflect greater loneliness. Item scores are summed to yield a total score with higher values reflecting higher levels of loneliness. To address our exploratory aim, we calculated a treatment-related loneliness change score by subtracting each individuals’ ULS-8 post-treatment score from their ULS-8 pre-treatment score. The ULS-8 has demonstrated good internal consistency as well as convergent validity with other measures of loneliness (Hays & DiMatteo, 1987). In our treatment sample, the ULS-8 demonstrated adequate internal consistency (α = .60).
Data Analytic Plan
Analyses were conducted using SPSS Statistical Software Version 26 and R Statistical Software Version 3.4.3. To examine whether loneliness changed differentially from pre- to post-treatment/waitlist as a function of treatment condition (CBGT vs. MBSR vs. WL), we examined linear mixed effects models (LMMs) using the MIXED procedure in SPSS. We additionally ran longitudinal LMMs to examine whether loneliness changed differentially between the two treatments (CBGT vs. MBSR) across the follow-up time points (3-, 6-, 9-, and 12-months post-treatment; with time treated as a continuous variable with each unit of time equivalent to three months), including waitlisted participants who were randomized to one of the two treatment groups after the waitlist period. Random intercepts were included in the models. Maximum likelihood estimation was used to address missing data at post-treatment/waitlist and follow-up time points, so cases with missing data were not excluded. We calculated partial eta squared as the measure of effect size for omnibus tests, considering greater than .06 as medium and .14 as large effects. Within-group effect sizes were calculated as Cohen’s d (Cohen, 1988), using the differences in estimated marginal means divided by the pooled within-group standard deviation (Dunlap, Cortina, Vaslow, & Burke, 1996).
Additionally, we examined whether changes in social anxiety from pre- to post-treatment predicted changes in loneliness across follow-up time points (3-, 6-, 9-, and 12-months post-treatment; with time treated as a continuous variable with each unit of time equivalent to three months). We conducted multilevel models (MLMs) with change in social anxiety from pre- to post-treatment, time (3-, 6-, 9-, and 12-months post-treatment), and the interaction between treatment-related social anxiety change and time predicting loneliness across follow-up time points. MLMs were estimated using packages lmer4 (Bates, Maechler, Bolker, & Walker, 2015) and lmerTest (Kuznetsova, Brockhoff, & Christensen, 2017) in R. MLMs included a random intercept and random slope of time during follow-up and were estimated using maximum likelihood.
In the MLM models, time during follow-up (3-, 6-, 9-, and 12-months post-treatment) was included as an observation-level predictor and social anxiety change from pre- to post-treatment was included as a person-level predictor. We controlled for person-level pre-treatment social anxiety, as well as its interaction with time during follow-up, in order to examine the effect of change in social anxiety that occurs from pre- to post-treatment on loneliness during follow-up, regardless of an individual’s baseline level of social anxiety.1 In the first model, we included the unconditional main effects of change in social anxiety from pre- to post-treatment and time during follow-up and controlled for pre-treatment social anxiety. In the second model, we added the interaction between time during follow-up and change in social anxiety from pre- to post-treatment, additionally controlling for the interaction between time during follow-up and pre-treatment social anxiety.
To examine our exploratory aim, whether changes in loneliness from pre- to post-treatment predicted changes in social anxiety during follow-up, we ran MLMs of social anxiety predicted by treatment-related change in loneliness, time during follow-up (3-, 6-, 9-, and 12-months post-treatment), and the interaction between treatment-related change in loneliness and time during follow-up, following the procedures described above.2
Results
Preliminary Analyses
There were no significant differences (p’s > .05) between CBGT, MBSR, and WL across any demographic variables (i.e., gender, age, race, ethnicity, education, marital status, or income). Information regarding the characteristics of participants in each treatment condition are presented in Table 1.
Table 1.
Demographic characteristics of individuals by condition.
| Characteristic | CBGT (n = 36) | MBSR (n = 36) | WL (n = 36) |
|---|---|---|---|
| Male, n (%) | 16 (44.4) | 16 (44.4) | 16 (44.4) |
| Age, years (mean [SD]) | 34.14 (8.05) | 29.90 (7.61) | 34.06 (7.78) |
| Education, years (mean [SD]) | 17.41 (3.29) | 16.22 (1.67) | 16.52 (2.93) |
| Race/Ethnicity, n (%) | |||
| Caucasian/White | 18 (50.0) | 14 (38.9) | 15 (41.7) |
| Asian American | 15 (41.7) | 13 (36.1) | 14 (38.9) |
| Latino/Hispanic | 2 (5.6) | 7 (19.4) | 1 (2.8) |
| African American/Black | 0 (0.0) | 1 (2.8) | 0 (0.0) |
| American Indian/Alaskan Native | 0 (0.0) | 0 (0.0) | 1 (2.8) |
| More than one race | 1 (2.8) | 1 (2.8) | 5 (13.9) |
| Marital Status, n (%) | |||
| Single, never married | 20 (55.6) | 23 (63.9) | 18 (50.0) |
| Married | 12 (33.3) | 8 (22.2) | 16 (44.4) |
| Living with partner | 3 (8.3) | 5 (13.9) | 1 (2.8) |
| Missing or not reported | 0 (0.0) | 0 (0.0) | 1 (2.8) |
| Yearly income, n (%) | |||
| < $10,000 | 3 (8.3) | 3 (8.3) | 1 (2.8) |
| $10,000–$25,000 | 3 (8.3) | 2 (5.6) | 4 (11.1) |
| $25,000–$50,000 | 5 (13.9) | 5 (13.9) | 5 (13.9) |
| $50,000–$75,000 | 6 (16.7) | 5 (13.9) | 3 (8.3) |
| $75,000–$100,000 | 4 (11.1) | 3 (8.3) | 4 (11.1) |
| >$100,000 | 9 (25.0) | 9 (25.0) | 10 (27.8) |
| Missing or not reported | 6 (16.7) | 9 (25.0) | 9 (25.0) |
Note. Demographic information from table by Goldin and colleagues (2016). All comparisons (between-group t-tests or χ2 tests) are nonsignificant, p > .05. CBGT = Cognitive-behavioral Group Therapy; MBSR = Mindfulness-Based Stress Reduction; WL = Waitlist.
Primary Analyses
Treatment Effects on Loneliness
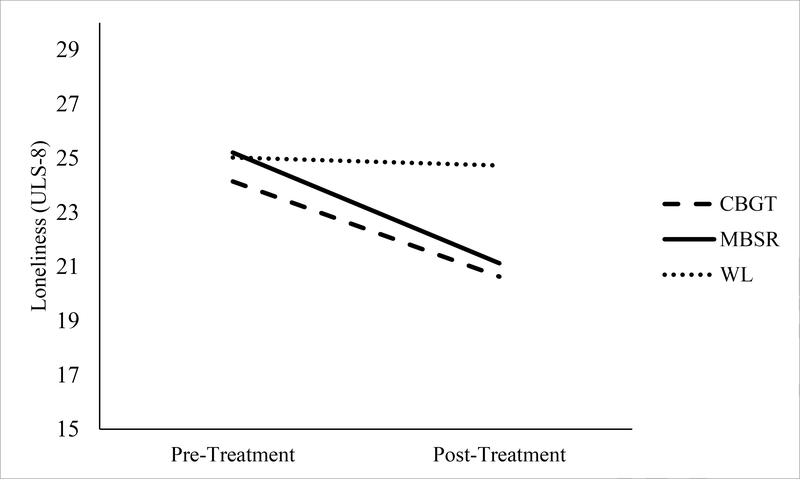
LMMs indicated there was a significant main effect of time, such that loneliness scores decreased from pre- to post-treatment/waitlist, F(1, 104.05) = 35.78, p < .01, ηp2 = 0.26. There was also a main effect of treatment condition on loneliness, F(2, 115.36) = 3.38, p = .04, ηp2 = 0.06. Importantly, there was a significant treatment condition by time interaction, F (2, 104.02) = 7.36, p = .001, ηp2 = 0.12 (see Figure 1). Planned contrasts using estimated marginal means revealed that loneliness at post-treatment/waitlist was significantly lower for CBGT versus WL, t(102.48) = 2.96, p = .004, d = 0.29, and for MBSR versus WL, t(103.82) = 3.57, p = .001, d = 0.34. There was no significant difference in loneliness between CBGT and MBSR at post-treatment, t(105.86) = 0.53, p = .60, d = .05. See Table 2 for estimated marginal means and standard errors relevant to this set of analyses.
Figure 1.
Trajectory of change in loneliness from pre- to post-treatment/waitlist for cognitive behavioral group therapy (CBGT), mindfulness-based stress reduction (MBSR), and waitlist (WL) conditions, based on estimated marginal means.
Table 2.
Estimated marginal means (and standard errors) of loneliness at pre-treatment and post-treatment by treatment condition.
| CBGT (n = 36) | MBSR (n = 36) | WL (n = 36) | |
|---|---|---|---|
| Pre-Treatment | 24.14 (0.78) | 25.21 (0.72) | 25.03 (0.78) |
| Post-Treatment | 20.63 (0.83) | 21.13 (0.79) | 24.73 (0.79) |
Note. CBGT = Cognitive-behavioral Group Therapy; MBSR = Mindfulness-Based Stress Reduction; WL = Waitlist.
Next, to examine whether CBGT and MBSR were equally efficacious at reducing loneliness during the follow-up period, we used longitudinal LMMs to examine change in loneliness from post-treatment through 3-, 6-, 9-, and 12-month follow-up assessments for CBGT and MBSR. WL patients who subsequently entered CBGT or MBSR were included in these analyses. There was no significant main effect of time, p > .05, indicating that loneliness scores did not change linearly across follow-ups. There was no significant main effect of treatment condition and no significant interaction between time and treatment condition, p’s > .05, indicating that CBGT and MBSR did not differ in linear change in loneliness during follow-up.
Treatment-Related Social Anxiety Change Predicting Reductions in Loneliness during Follow-up
MLMs examined whether social anxiety change from pre- to post-treatment, time during follow-up (3-, 6-, 9-, and 12-months post-treatment), and the interaction between treatment-related social anxiety change and time predicted loneliness during follow-up, controlling for pre-treatment social anxiety and the interaction between time and pre-treatment social anxiety. Descriptive statistics for study variables included in our MLMs are shown in Table 3. The MLM of the unconditional effects of social anxiety change from pre- to post-treatment and time predicting loneliness during follow-up, controlling for an individual’s social anxiety at pre-treatment, is presented in Table 4.3 Greater reduction in social anxiety from pre- to post-treatment, controlling for pre-treatment social anxiety, predicted lower levels of loneliness on average during follow-up. The interaction between time and social anxiety change from pre- to post-treatment was not significant, p > .05.
Table 3.
Descriptive statistics for study variables included in multilevel models from 3-, 6-, 9- to 12-month follow-up assessment period.
| Variable | M (SD) |
|---|---|
| Time (months) | 10.38 (3.42) |
| Pre-Treatment Social Anxiety (LSAS-SR) | 89.69 (18.24) |
| Social Anxiety Change During Treatment (LSAS-SR) | 38.24 (21.66) |
| Loneliness (ULS-8) | 21.06 (5.63) |
Note. N = 81 individuals; LSAS-SR= Liebowitz Social Anxiety Scale Self-Report. Pre-Treatment Social Anxiety= LSAS-SR score at pre-treatment; Social Anxiety Change During Treatment= LSAS-SR change in score from pre-treatment to post-treatment; ULS-8 = UCLA Loneliness Scale-8 Item Scale; Loneliness score indicates mean loneliness score averaged across follow-up assessments.
Table 4.
Multilevel models of loneliness during follow-up predicted by change in social anxiety from pre- to post-treatment and time during follow-up.
| Loneliness (ULS-8) | |
|---|---|
| Control Variables | |
| Person-Level Pre-Treatment Social Anxiety | 0.110** (0.037) |
| Substantive Effects | |
| Person-Level Social Anxiety Change During Treatment | −0.130*** (0.031) |
| Observation-Level Time (months) | −0.101 (0.054) |
| Observations | 281 |
| Nakagawa & Schielzeth R2 | 0.16 |
| Variance Components | |
| Person Level | 30.26† |
| Observation Level | 3.90 |
| Time Slope | 0.12° |
| Log Likelihood | −740.00 |
| Akaike Inf. Crit. | 1,496.00 |
| Bayesian Inf. Crit. | 1,525.00 |
Note. Table presents unstandardized beta coefficients (b) and standard errors (SE) below. Social anxiety at pre-treatment and social anxiety change in score from pre- to post-treatment measured using the Liebowitz Social Anxiety Scale Self-Report Score (LSAS-SR)
p < .05
p < .01
p < 0.001
p < .05 according to profile confidence intervals
p < .01 according to the deviance test.
Standard errors shown in parentheses.
Treatment-Related Loneliness Change Predicting Reductions in Social Anxiety during Follow-up
MLMs additionally explored whether loneliness change from pre- to post-treatment, time during follow-up (3-, 6-, 9-, and 12-months post-treatment), and the interaction between loneliness change from pre- to post-treatment and time predicted social anxiety during follow-up, controlling for pre-treatment loneliness and the interaction between time and pre-treatment loneliness. The MLM of the unconditional effects of time and loneliness change from pre- to post-treatment predicted social anxiety during follow-up, controlling for an individual’s loneliness at pre-treatment, is presented in Table 5.4 Greater reduction in loneliness from pre- to post-treatment, controlling for pre-treatment loneliness, predicted lower levels of social anxiety on average during follow-up. The interaction between time and loneliness change from pre- to post-treatment was not significant, p > .05.
Table 5.
Multilevel models of social anxiety during follow-up predicted by change in loneliness from pre- to post-treatment and time during follow-up.
| Social Anxiety (LSAS-SR) | |
|---|---|
| Control Variables | |
| Person-Level Pre-Treatment Loneliness | 1.390** (0.451) |
| Substantive Effects | |
| Person-Level Loneliness Change During Treatment | −1.500*** (0.432) |
| Observation-Level Time (months) | −0.230 (0.176) |
| Observations | 278 |
| Nakagawa & Schielzeth R2 | 0.14 |
| Variance Components | |
| Person Level | 123.75† |
| Observation Level | 76.87 |
| Time Slope | 0.44° |
| Log Likelihood | −1,105.00 |
| Akaike Inf. Crit. | 2,225.00 |
| Bayesian Inf. Crit. | 2,254.00 |
Note. Table presents unstandardized beta coefficients (b) and standard errors (SE) below. Social anxiety at pre-treatment and social anxiety change in score from pre- to post-treatment measured using the Liebowitz Social Anxiety Scale Self-Report Score (LSAS-SR)
p < .05
p < .01
p < 0.001
p < .05 according to profile confidence intervals
p < .01 according to the deviance test.
Standard errors shown in parentheses.
Discussion
This study examined whether two efficacious treatments for SAD, CBGT and MBSR, help to reduce loneliness at post-treatment and during a 1-year follow-up period and whether treatment-related reductions in social anxiety predicted reductions in loneliness during the year following treatment.
Our first hypothesis, examining whether CBGT and MBSR would reduce loneliness at post-treatment, was supported; compared to WL, both CBGT and MBSR significantly reduced loneliness at post-treatment. In the original study by Goldin and colleagues (2016), both treatments resulted in significant reductions in social anxiety at post-treatment compared to WL, so it was expected that both treatments would have similar positive effects on loneliness. It appears that these treatments for SAD not only help individuals see improvement in their social anxiety symptoms, but also have the added benefit of alleviating individuals’ experience of loneliness.
Our second hypothesis, examining whether there were differences between the two active treatments during follow-up, was partially supported; there were no differences between treatments at post-treatment or during follow-up period. In the original study by Goldin and colleagues (2016), both treatments resulted in significant reductions in social anxiety that were maintained throughout the year following treatment, so we anticipated that both treatments had the potential to additionally improve loneliness during the year following treatment. However, we saw that loneliness did not decrease linearly across the year following treatment. Although loneliness did not decrease incrementally during follow-up, nor was treatment a significant predictor of change during follow-up, it is possible that there is significant inter-individual variability in participants’ change in loneliness following treatment. Future research could test this as well as examine other predictors of individual trajectories of loneliness in the year following treatment.
Taken together, our findings indicate that CBGT and MBSR were equally effective at reducing loneliness at post-treatment and had similar effects on loneliness throughout the follow-up period. Although these results are congruent with our predictions, it is conceivable that one may have expected there to be differences between treatments. As mentioned previously, Masi et al. (2011)’s meta-analysis indicated that treatment that targets maladaptive social cognitions have shown to most effectively reduce loneliness; therefore, one could argue that CBGT, which explicitly targets maladaptive social cognitions as a key component of treatment through cognitive restructuring, would lead to greater improvements in loneliness than MBSR. Nevertheless, our findings indicate that both CBGT and MBSR led to similar improvements in loneliness; it seems likely that MBSR’s emphasis on helping clients to non-judgmentally notice and examine their maladaptive anxious thoughts may have also helped lonely individuals to target their maladaptive social cognitions, much like CBGT. Interestingly, in a follow-up study to the original RCT (Goldin et al., 2016), Goldin et al. (2017) examined weekly trajectories of social anxiety over the course of both treatments, and found that although both treatments lead to an increase in disputing (or challenging) of one’s maladaptive thoughts on a weekly basis, only disputing or challenging one’s thoughts in MBSR, but not CBGT, led to subsequent weekly decreases in social anxiety; this finding was somewhat surprising, as researchers expected disputing in CBGT to lead to greater subsequent improvements in social anxiety over treatment than MBSR. Nevertheless, their finding provides suggests that MBSR is a treatment that effectively helps individuals to challenge maladaptive social cognitions. From our study, we can conclude that both CBGT and MBSR help to improve loneliness, possibly by helping individuals challenge their maladaptive social thoughts, although more research is needed to directly investigate the mechanisms of change in MBSR and CBGT.
Our next set of hypotheses, examining whether reductions in social anxiety that occur during treatment predict reductions in loneliness during the follow-up period, were partially supported. Importantly, reductions in social anxiety from pre- to post-treatment significantly predicted lower levels of loneliness on average during follow-up, regardless of an individual’s baseline social anxiety. This suggests that as individuals with SAD learn during these treatments to identify and change their relationship with their maladaptive social cognitions, approach rather than avoid social situations, and participate in a group treatment, there are increased opportunities for social connectedness that may facilitate long-term improvements in loneliness. In these models, as above, the main effect of time during follow-up did not significantly predict reductions in loneliness. Although some individuals may see continuing decreases in loneliness following treatment for SAD, others may have a more static or variable course. In addition, time and social anxiety change from pre- to post-treatment did not interact to predict changes in loneliness, which suggests that individuals who experienced a greater change in social anxiety during treatment did not experience a significantly greater rate of change in loneliness across follow-up assessments.
Future research should consider potential mediators of the relationship between treatment-related change in social anxiety and reductions in loneliness (e.g., individual differences in personality, comorbidity, age, connectedness with treatment group, size of social network following treatment, starting a new relationship following treatment, etc.). In addition, future research should examine additional factors that may influence decreases in loneliness after treatment across time that were not examined as part of this study; as postulated by past research, individual’s social skills, perceived social support, and sense of group membership or connection with social groups and the broader community may also affect an individual’s experience of loneliness (S. Cacioppo et al., 2015; Haslam et al., 2019; Mann et al., 2017; Masi et al., 2011), and were not directly targeted by these interventions. Haslam et al. (2019) recently examined the efficacy of a new intervention, GROUPS 4 HEALTH (G4H), which was created to target the development and maintenance of social group memberships to support health, and found that G4H led to greater reductions in loneliness than treatment as usual (TAU), as well as greater reductions in social anxiety and a greater sense of belonging to multiple groups compared to TAU. It appears that interventions, such as G4H, which promote social connectedness may also reduce loneliness and social anxiety, although continued research is needed.
As an exploratory aim, we examined whether reductions in loneliness that occur from pre- to post-treatment predicted reductions in social anxiety in the year following treatment. Reductions in loneliness from pre- to post-treatment did significantly predict lower levels of social anxiety on average during follow-up. This exploration allowed us to deepen our understanding of the interrelated nature of social anxiety and loneliness across time. We can conclude that both social anxiety and loneliness decrease over the course of treatment, and changes in one during treatment may affect levels of the other in the year following treatment. Because individuals with SAD are vulnerable to experiencing loneliness, future research should continue to examine the bidirectional effects of these constructs and how they relate across time to better understand how to alleviate experiences of loneliness.
A few limitations of the current study should be noted. First, this study was a secondary analysis of a RCT of two group treatments for social anxiety for treatment-seeking individuals with generalized SAD, so our sample does not fully represent the population of socially anxious individuals who experience loneliness, as it includes only individuals who are treatment-seeking and who meet the diagnostic clinical threshold for generalized SAD. Second, it is also possible that the group nature of the treatments may have influenced the reductions in loneliness shown across individuals in our sample during follow-up; although research suggests that group-based interventions have strong potential for success (S. Cacioppo et al., 2015), individual therapy is more commonly provided, so more research is needed to determine whether individual CBT may have the same effect on loneliness. Future studies should examine whether CBT and mindfulness and acceptance-based treatments, as well as other individual therapies for social anxiety, can similarly reduce loneliness. This study also relied on self-report measures to examine social anxiety and loneliness. Future research should employ other methods, such as experimental tasks or paradigms, to better capture what specific changes in social anxiety may be occurring over the course of treatment and what may constitute an individual’s subjective experience of loneliness. In addition, the internal consistency of the ULS-8 in our sample was lower than expected, which may lead to increased variability when interpreting our findings. Previous research has provided strong support for the original, revised, and shortened versions of UCLA Loneliness Scale, but future studies may consider including Alternative measures of loneliness when addressing similar research questions. Further our sample consisted primarily of Caucasian/White and Asian American individuals, with few individuals from other groups. Future studies should aim to examine more racially and ethnically diverse samples of individuals seeking treatment. It would be interesting to consider how an individual’s racial or ethnic identity may affect his or her experiences of loneliness; it is possible that an individual’s racial or ethnic identity may protect against experiences of loneliness if they have a strong connection with their racial or ethnic community, but it is also possible that one’s identity as a racial/ethnic minority may exacerbate experiences of loneliness. Finally, our assessments during follow-up were completed at 3-month intervals. Future studies could use more frequent assessments to provide a more nuanced picture of the trajectory of change in loneliness following treatment.
Our study has important implications. First, this study adds to the literature on available evidence-based treatments that can reduce the burden of loneliness. It provides further evidence that interventions that target identifying and changing one’s relationship to maladaptive social cognitions as well as enhancing opportunities for social interactions help to decrease loneliness (S. Cacioppo et al., 2015; Mann et al., 2017; Masi et al., 2017). This study also provides encouragement for implementing group-based interventions to target loneliness. Furthermore, this study explores the efficacy of interventions on loneliness among individuals with mental disorders; because most studies to date have examined loneliness interventions among typical older adult populations (Mann et al., 2017), this study broadens our understanding of how to intervene to address loneliness in populations that may be more vulnerable to experiencing loneliness. Finally, we are the first to examine interventions for loneliness among individuals with SAD, who are at particularly high risk for loneliness. Taken together, this study provides information about the interrelated nature of social anxiety and loneliness, and identifies two specific, evidence-based treatments that can be implemented to help decrease loneliness. Given the significant mental, physical, and societal health costs of loneliness, efforts to alleviate it are important and deserve significant attention. Future research should continue to identify and extend evidence-based treatments that may alleviate loneliness for those at greatest risk of feeling lonely.
Supplementary Material
Highlights.
Individuals with social anxiety disorder (SAD) are at elevated risk for loneliness.
We examined loneliness in a randomized controlled trial of two treatments for SAD.
Individuals who received treatment were less lonely than waitlist controls.
Treatment changes in social anxiety predicted lower loneliness during follow-up.
Treatment changes in loneliness predicted lower social anxiety during follow-up.
Acknowledgments
Funding: This research was supported by an NIMH Grant R01 MH092416, awarded to James J. Gross. ClinicalTrials.gov identifier: NCT02036658.
Footnotes
Declarations of interest: none.
MLMs were run without controlling for pre-treatment social anxiety as a robustness check; because the significance of our results remains pre-dominantly unchanged, we are presenting the more conservative models in this paper, controlling for pre-treatment social anxiety. Additional MLMs were also run including person-level pre-treatment loneliness and its interaction with time as additional control variables. Because the significance of our results remained unchanged when including these additional control variables, we present the simpler models that only control for pre-treatment social anxiety in this manuscript. All additional MLMs without controlling for pre-treatment social anxiety and additionally controlling for pre-treatment loneliness and its interaction with time are available in the supplemental online materials.
Our exploratory MLMs were also run without controlling for pre-treatment loneliness as a robustness check; because the significance of our results remains unchanged, we are presenting the more conservative models in this paper, controlling for pre-treatment loneliness.
A second MLM was run including the interaction between social anxiety change from pre- to post-treatment and time, additionally controlling for the interaction between time and pre-treatment social anxiety. Because the interaction between time and social anxiety change during treatment was not significant, we are presenting the simpler model in this manuscript. This second model including these interactions is available in the supplemental online materials.
A second MLM was run including the interaction between loneliness change from pre- to post-treatment and time, additionally controlling for the interaction between time and pre-treatment loneliness. Because the interaction between time and loneliness change from pre- to post-treatment was not significant, we are presenting the simpler model in this manuscript. This second model including these interactions is available in the supplemental online materials.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alden LE, & Taylor CT (2004). Interpersonal processes in social phobia. Clinical Psychology Review, 24, 857–882. 10.1016/j.cpr.2004.07.006 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, 4th edition (DSM-IV). Washington, D.C.: Author. 10.1007/springerreference_179660 [DOI] [Google Scholar]
- Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, & Craske MG (2013). Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behaviour Research and Therapy, 51, 185–196. 10.1016/j.brat.2013.01.003 [DOI] [PubMed] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, & Hofmann SG (2002). The Liebowitz Social Anxiety Scale as a self-report instrument: A preliminary psychometric analysis. Behaviour Research and Therapy, 40, 701–715. 10.1016/s0005-7967(01)00060-2 [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B, & Walker s. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67, 1–48. https://doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110, 49–58. 10.1037//0021-843x.110.1.49 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2005). People thinking about people: The vicious cycle of being a social outcast in one’s own mind. In Williams KD, Forgas JP, & Von Hippel W, (Eds.), The social outcast: Ostracism, social exclusion, rejection, and bullying (pp. 91–108). New York, NY: Psychology Press. 10.4324/9780203942888 [DOI] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015). Loneliness: Clinical import and interventions. Perspectives on Psychological Science, 10, 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee R (2018, May 1). Americans are lonely a lot, and younger people bear the heaviest burden. National Public Radio. Retrieved from https://www.npr.org/sections/health-shots/2018/05/01/606588504/americans-are-a-lonely-lot-and-young-people-bear-the-heaviest-burden
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Earlbaum Associates, Inc. [Google Scholar]
- Di Nardo PA, Brown TA, & Barlow DH (1994). Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L). New York, NY: oxford University Press. [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, & Burke MJ (1996). Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods, 1, 170–177. 10.1037/1082-989X.1.2.170. [DOI] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, & Goetz D (2001). The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine, 31, 1025–1035. 10.1017/s0033291701004056 [DOI] [PubMed] [Google Scholar]
- Fung K, Paterson D, & Alden LE (2017). Are social anxiety and loneliness best conceptualized as a unitary trait? Journal of Social and Clinical Psychology, 36, 335–345. 10.1521/jscp.2017.36.4.335 [DOI] [Google Scholar]
- Goldin PR, & Gross JJ (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion, 10, 83–91. 10.1037/a0018441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg RG, & Gross JJ (2016). Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 84, 427–437. 10.1037/ccp0000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Morrison AS, Jazaieri H, Heimberg RG, & Gross JJ (2017). Trajectories of social anxiety, cognitive reappraisal, and mindfulness during an RCT of CBGT versus MBSR for social anxiety disorder. Behaviour Research and Therapy, 97, 1–13. 10.1016/j.brat.2017.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam C, Cruwys T, Chang MX-L, Bentley SV, Haslam SA, Dingle GA, & Jetten J (2019). GROUPS 4 HEALTH reduces loneliness and social anxiety in adults with psychological distress: Findings from a randomized controlled trial. Journal of Consulting and Clinical Psychology, 87, 787–801. 10.1037/ccp0000427 [DOI] [PubMed] [Google Scholar]
- Hays RD, & DiMatteo MR (1987). A short-form measure of loneliness. Journal of Personality Assessment, 51, 69–81. 10.1207/s15327752jpa5101_6 [DOI] [PubMed] [Google Scholar]
- Heimberg RG, & Becker RE (2002). Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York, NY: Guilford Press. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, & Turk CL (2010). Managing social anxiety: A cognitive-behavioral therapy approach (2nd ed.). New York, NY: Oxford University Press. [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Dell Publishing; NY, New York. [Google Scholar]
- Kabat-Zinn J, & Santorelli S (1993). Mindfulness-based stress reduction professional training resource manual.
- Käll A, Shafran R, Lindegaard T, Bennett S, Cooper Z, Coughtrey A, & Andersson G (2020). A common elements approach to the development of a modular cognitive behavioral theory for chronic loneliness. Journal of Consulting and Clinical Psychology, 88, 269–282. https://doi: 10.1037/ccp0000454 [DOI] [PubMed] [Google Scholar]
- Kaplan SC, Swee MB, & Heimberg RG (2018). Psychological treatments for social anxiety disorder. In Braddick O (Ed.), Oxford Research Encyclopedia of Psychology. New York: Oxford University Press. doi: 10.1093/acrefore/9780190236557.013.98. Retrieved from http://psychology.oxfordre.com/view/10.1093/acrefore/9780190236557.001.0001/acrefore-9780190236557-e-98 [DOI] [Google Scholar]
- Kocovski NL, Segal ZV, & Battista SR (2009). Mindfulness and psychopathology: Problem formulation. In Didonna F (Ed.), Clinical handbook of mindfulness (pp. 85–98). New York, NY: Springer. 10.1007/978-0-387-09593-6_6 [DOI] [Google Scholar]
- Kuznetsova A, Brockhoff P, & Christensen RHB(2017). lmerTest package: Tests in linear mixed effects models. Journal of Statistical Software, 82, 1–26. 10.18637/jss.v082.i13 [DOI] [Google Scholar]
- Levin JB, Marom S, Gur S, Wechter D, & Hermesh H (2002). Psychometric properties and three proposed subscales of a self-report version of the Liebowitz Social Anxiety Scale translated into Hebrew. Depression and Anxiety, 16, 143–151. 10.1002/da.10064 [DOI] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Trends in Pharmacopsychiatry, 22, 141–173. 10.1159/000414022 [DOI] [PubMed] [Google Scholar]
- Lim MH, Rodebaugh TL, Zyphur MJ, & Gleeson JF (2016). Loneliness over time: The crucial role of social anxiety. Journal of Abnormal Psychology, 125, 620–630. 10.1037/abn0000162 [DOI] [PubMed] [Google Scholar]
- Mann F, Bone JK, Lloyd-Evans B, Frerichs J, Pinfold V, Ma R, …. Johnson S (2017). A life less lonely: The state of the art in interventions to reduce loneliness in people with mental health problems. Social Psychiatry and Psychiatric Epidemiology, 52, 627–638. 10.1007/s00127-017-1392-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Chen H, Hawkley LC, & Cacioppo JT (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15, 219–266. 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, & Brugha TS (2013). Feelings of loneliness among adults with mental disorder. Social Psychiatry and Psychiatric Epidemiology, 48, 5–13. 10.1007/s00127-012-0515-8 [DOI] [PubMed] [Google Scholar]
- Oakman J, Van Ameringen M, Mancini C, & Farvolden P (2003). A confirmatory factor analysis of a self-report version of the Liebowitz Social Anxiety Scale. Journal of Clinical Psychology, 59, 149–161. 10.1002/jclp.10124 [DOI] [PubMed] [Google Scholar]
- Peplau LA, & Perlman D (1982). Perspectives on loneliness. In Peplau LA & Perlman D (Eds.), Loneliness: A sourcebook of current theory, research and therapy (pp. 1–20). New York, NY: Wiley. [Google Scholar]
- Russell DW (1982). The measurement of loneliness. In Peplau LA & Perlman D (Eds.), Loneliness: A sourcebook of current theory, research and therapy (pp. 81–104). New York, NY: Wiley. [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Russell DW, Peplau LA, & Cutrona CE (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39, 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Russell DW, Peplau LA, & Ferguson ML (1978). Developing a measure of loneliness. Journal of Personality Assessment, 42, 290–294. 10.1207/s15327752jpa4203_11 [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, … Hofmann SG (2009). Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. Depression and Anxiety, 26, 34–38. 10.1002/da.20503 [DOI] [PubMed] [Google Scholar]
- Stahl B, & Goldstein E (2010). A mindfulness-based stress reduction workbook. Oakland, CA: New Harbinger. [Google Scholar]
- Teo AR, Lerrigo R, & Rogers MA (2013). The role of social isolation in social anxiety disorder: A systematic review and meta-analysis. Journal of Anxiety Disorders, 27, 353–364. 10.1016/j.janxdis.2013.03.010 [DOI] [PubMed] [Google Scholar]
- Yeginsu C (2018, January 17). U.K appoints a minister for loneliness. The New York Times. Retrieved from https://www.nytimes.com/2018/01/17/world/europe/uk-britain-loneliness.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.