Abstract
Background:
Hip dysplasia is a common source of hip pain and a known cause of early osteoarthritis of the hip.
Purpose:
To (1) define the population-based incidence of hip dysplasia diagnosis in young patients presenting with hip pain in a large geographically defined cohort, (2) analyze trends regarding presentation and diagnosis of hip dysplasia, and (3) report the rate and type of surgical interventions used to treat this population.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A geographic epidemiological database was queried to identify patients aged 14 to 50 years with hip pain between the years 2000 and 2016. Patient medical records were analyzed, and demographic, imaging, clinical, and treatment history were recorded. Incidence trends were examined by use of linear regression with confidence intervals for age and calendar year.
Results:
Overall, 1893 patients were included. Of these, 156 patients (196 hips) had a diagnosis of hip dysplasia. The incidence of hip dysplasia diagnosis in patients who reported hip pain was 12.7 per 100,000 person-years. Patients with dysplasia had a mean age of 26.7 ± 9.8 years, while the highest age-adjusted incidence occurred at age 14 to 18 years in both male and female patients. Female patients had double the age-adjusted incidence of male patients (cases per 100,000 person-years: 16.8 [95% CI, 13.9-19.7] vs 8.7 [95% CI, 6.6-10.8]; P < .01). Of the patients who underwent magnetic resonance imaging, 77% had imaging consistent with labral pathology. Patients were treated with physical therapy (67%), intra-articular steroid injection (29%), hip arthroscopy (10%), and periacetabular osteotomy (9%). The use of hip arthroscopy significantly increased over time (P < .01), whereas the use of steroid injection and periacetabular osteotomy did not (P < .28 and P < .08, respectively).
Conclusion:
The incidence of hip dysplasia diagnosis in patients presenting with hip pain was 12.7 per 100,000 person-years. Female patients had twice the age-adjusted incidence of male patients, and the highest age-adjusted incidence occurred in the age range of 14 to 18 years in both sexes. The use of hip arthroscopy to treat patients with hip dysplasia significantly increased over time.
Keywords: hip dysplasia, hip osteoarthritis, epidemiology, incidence
Hip dysplasia is a common source of hip pain that is present in 20% to 40% of patients with hip osteoarthritis.6 Classically, patients with hip dysplasia report insidious groin pain6 and can be diagnosed based on certain radiographic parameters (Tönnis angle >10° and/or lateral center-edge angle [LCEA] <25°).3 Even though pain is a common presenting symptom, self-reported hip and groin pain has not been shown to be significantly associated with hip dysplasia in cross-sectional studies.8,9 Conversely, hip dysplasia has been linked to degeneration of the hip joint and has been found to be significantly associated with the development of radiological hip osteoarthritis.6,9
Previous studies have estimated the prevalence of hip dysplasia in asymptomatic patients to be between 3.6% and 12.8%, depending on the radiographic indexes used.6,8,9 However, no study has analyzed the incidence of hip dysplasia diagnosis in a large population of patients with hip pain.18 Matsuda et al15 retrospectively analyzed a cohort of 1053 patients treated with hip arthroscopy and found that 13% of the patients had dysplasia; however, that study was limited because it included only patients with severe enough symptoms to warrant treatment with hip arthroscopy. It is therefore important to identify the incidence of hip dysplasia in all patients who report hip pain, because it is likely more representative of the true incidence of symptomatic hip dysplasia.
Patients with dysplasia who experience mild degenerative changes have earlier hip degeneration and a higher probability of undergoing total hip arthroplasty (THA) at 10 years and 20 years compared with patients who have femoroacetabular impingement or normal hip morphologic features.22 Wyles et al23 found that patients with dysplasia who underwent periacetabular osteotomy (PAO) had 10-year THA rates of 11% for Tönnis grade 1 and 53% for Tönnis grade 2 compared with 25% and 74%, respectively, for patients with dysplasia who did not undergo PAO. Patients with higher Tönnis grades at the time of PAO were also shown to have significantly higher probabilities of progression to THA.23 Therefore, it is important to better understand the prevalence of hip dysplasia in patients with hip pain given their early age of presentation and the high success rate of correction via PAO while patients have lower Tönnis grades.6,18,23 Early identification and treatment of hip dysplasia could slow the natural history of hip degeneration to rates more similar to hips with normal morphologic characteristics.23
Currently, there is a paucity of data regarding the incidence of hip dysplasia diagnosis in patients with hip pain. It is important that physicians have information regarding the incidence of hip dysplasia in symptomatic patients, given the high rate of progression to hip osteoarthritis at a young age.22,23 Therefore, the purpose of this study was (1) to define the population-based incidence of hip dysplasia diagnosis in patients presenting with hip pain in a large geographically defined cohort, (2) to analyze trends regarding presentation and diagnosis of hip dysplasia, and (3) to report the rate and type of surgical interventions used to treat this population.
Methods
Institutional review board approval was granted before this study was performed. The Rochester Epidemiology Project (REP) was used to perform a regional population-based cohort study. The REP medical record database contains comprehensive electronic medical records for all Olmstead County citizens treated by a physician in Olmsted County, Minnesota, regardless of the institution where the care was provided (population of 144,260 in 2010).17 The REP was queried to identify patients who met the following criteria: aged between 14 and 50 years, consulted a physician for hip pain between January 2000 and December 2016, had an International Classification of Diseases (ICD) code of 9 or 10 (Table 1), and had 2 hip radiographs performed at least 30 days apart (to ensure that patients had adequate follow-up). A total of 1893 patients were identified. Each patient’s chart was examined, and all relevant items such as clinical, physical therapy, and operative notes (if applicable) and radiographic images were individually examined and manually logged using REDcap software (Version 9.1.0; Vanderbilt University). Exclusion criteria included a history of avascular necrosis, hip fracture, neuromuscular disorder, spinal cord injury, and hip dislocation. Patients without notes or radiographs were also excluded.
Table 1.
ICD Codes for Patient Inclusiona
| Code | Code Description |
|---|---|
| ICD-9 | |
| 719.45 | Hip pain |
| 719.85 | Femoroacetabular impingement |
| 719.95 | Unspecified disorder of joint; pelvic region and thigh |
| ICD-10 | |
| M25.559 | Pain in unspecified hip |
| M25.551 | Pain in hip |
| M25.859 | Other specified joint disorders, unspecified hip |
| M25.852 | Other specified joint disorders, hip |
aICD, International Classification of Diseases.
Anterior-posterior and lateral (cross-table, 45° Dunn, or frog-leg) views were obtained for all 1893 patients, and each radiograph was individually reviewed by an attending surgeon or senior-level orthopaedic surgery resident (H.P.M. and Jun Zhou, MD, PhD). Both reviewers evaluated the first 100 radiographs to standardize radiographic measurements. There was good agreement between reviewers for the first 100 radiographs. Hip dysplasia was diagnosed if patients had a Tönnis angle >10° and/or an LCEA <25°, according to parameters established by Clohisy et al.3 The radiographic parameters set by Clohisy et al are subject to a range of error; however, these values are currently the standard for radiographic reporting of hip dysplasia.
Patients retrospectively diagnosed with dysplasia were reviewed to determine treatment methods and development of symptomatic hip osteoarthritis. Relevant patient demographic information, such as sex, body mass index (BMI), smoking status, comorbidity status, and sport participation, was collected. Initial clinical examination findings, magnetic resonance imaging (MRI) imaging results, physical therapy participation, intra-articular injections, surgeries, and postoperative clinical examinations were recorded for all patients with dysplasia. Dates for onset of hip pain, initial presentation, imaging, injections, and operations were recorded to calculate time to respective outcomes.
Statistical Analysis
Age- and sex-specific rates of hip dysplasia were calculated using the number of retrospectively diagnosed cases of hip dysplasia. The incidence equation used was based on epidemiology guidelines from the US Centers for Disease Control and Prevention, where Incidence = (Number of retrospectively diagnosed cases of hip dysplasia) ÷ (Summed person-years of observation). Olmstead County population estimates were based on decennial census counts. Only patients who were residents of Olmsted County at the time of hip pain and who fulfilled the study criteria were included in the incidence calculations. Because of the racial demographics of this cohort, overall incidence data were adjusted by age and sex to the 2010 White population of the United States. Poisson distribution was assumed to determine the number of incident cases per year for the 95% CIs of incidence values. Incidence trends were examined by use of linear regression with confidence intervals for age and calendar year. Significance in incidence over time by age and sex was determined using the exact Cochran Armitage trend test, where the total was used as the comparison variable. An analysis of variance was performed to determine significance between incidence and age × sex and incidence and year × sex. All analyses were performed using JMP 12.0.1 software (SAS Institute Inc).
Results
Of the 1893 patients who presented with hip pain during the study period, 156 patients (8.4%) presented with radiographic evidence of hip dysplasia. Of the 156 patients diagnosed with hip dysplasia, 40 (26%) were diagnosed with bilateral radiographic evidence of hip dysplasia. Overall, 71 hips (36.2%) were diagnosed with hip dysplasia at the initial clinic visit. Of the cohort of 196 hips, 65.8% (129 hips) were female (Table 2). Patients with dysplasia had a mean ± SD age of 26.7 ± 9.8 years at the time of hip pain, which was comparable with a mean age at presentation of 28.78 ± 8.51 years for the entire cohort of 1893 patients with hip pain. The mean BMI of the patients with hip dysplasia was 27.5 ± 5.0 kg/m2. On radiographic analysis, 71.4% had moderate dysplasia (LCEA <18°), 28.1% had mild dysplasia (LCEA 18°-24°), and 79% (155/196 hips) had Tönnis angle >10°. MRI was performed for 87 hips, and of those, 67 hips (77%) were diagnosed with a labral tear.
Table 2.
Characteristics of Patients Diagnosed With Hip Dysplasia, 2000-2016a
| 2000-2004 (n = 52) | 2005-2009 (n = 52) | 2010-2016 (n = 92) | Total (N = 196) | |
|---|---|---|---|---|
| Age at date of pain, y | 25.2 ± 12.3 | 25.6 ± 10.2 | 28.1 ± 7.7 | 26.7 ± 9.8 |
| Sex | ||||
| Male | 20 (38.5) | 18 (34.6) | 29 (31.5) | 67 (34.2) |
| Female | 32 (61.5) | 34 (65.4) | 63 (68.5) | 129 (65.8) |
| Ethnicity | ||||
| White | — | — | — | 140 (89.7) |
| Black | — | — | — | 5 (3.2) |
| Asian | — | — | — | 6 (3.8) |
| Other | — | — | — | 5 (3.2) |
| Laterality | ||||
| Left | 23 (44.2) | 23 (44.2) | 35 (38.0) | 81 (41.3) |
| Right | 29 (55.8) | 29 (55.8) | 57 (62.0) | 115 (58.7) |
| Body mass index, kg/m2 | 28 ± 5.2 | 27.2 ± 4.9 | 27.3 ± 5.0 | 27.5 ± 5.0 |
| Radiographic findings | ||||
| LCEA 18°-24° | 16 (30.8) | 17 (32.7) | 22 (42.3) | 55 (28.1) |
| LCEA <18° | 35 (67.3) | 35 (67.3) | 70 (134.6) | 140 (71.4) |
| Alpha angle >55° | 37 (71.2) | 40 (76.9) | 70 (76.1) | 147 (75.0) |
| Positive crossover sign | 37 (71.2) | 32 (61.5) | 54 (58.7) | 123 (62.8) |
| Positive posterior wall sign | 39 (75.0) | 39 (75.0) | 69 (75.0) | 147 (75.0) |
| Positive ischial spine sign | 25 (48.1) | 21 (40.4) | 35 (38.0) | 81 (41.3) |
| Hips with MRI | 17 (32.7) | 24 (46.2) | 46 (50.0) | 87 (44.4) |
| Labral tear on MRI | 10 (19.2) | 20 (38.5) | 37 (40.2) | 67 (34.2) |
| Hip dysplasia diagnosis at initial visit | 22 (42.3) | 16 (30.8) | 33 (35.9) | 71 (36.2) |
aData are presented as mean ± SD or No. (% of group). Dashes indicate not applicable (only the total ethnicities were collected). LCEA, lateral center-edge angle; MRI, magnetic resonance imaging.
Population-Based Incidence of Hip Dysplasia Diagnosis
The overall age- and sex-adjusted annual incidence of hip dysplasia diagnosis was 12.7 (95% CI, 10.9-14.5) per 100,000 person-years (Table 3). Table 3 and Figure 1 illustrate the annual incidence of hip dysplasia diagnosis in different age groups separated by sex. Female patients had double the age-adjusted incidence of male patients (16.8 [95% CI, 13.9-19.7] vs 8.7 [95% CI, 6.6-10.8] cases per 100,000 person-years; P < .01). Female patients aged 14 to 18 years had the highest age-adjusted incidence of hip dysplasia diagnosis (31.5/100,000 person-years; P < .01), and female patients aged 26 to 35 years had the second highest age-adjusted incidence (27.1/100,000 person-years). For male patients, the highest age-adjusted incidence of hip dysplasia diagnosis was in those aged 14 to 18 years (14.4/100,000 person-years; P < .06).
Table 3.
Age- and Sex-Specific Annual Incidence of Hip Dysplasia Diagnosis, 2000-2016a
| No. of Cases | Incidence Rate | |||||
|---|---|---|---|---|---|---|
| Age group | Female | Male | Total | Female | Male | Total |
| ≤13 y | 8 | 8 | 16 | 3.6 | 3.2 | 3.3 |
| 14-18 y | 25 | 12 | 37 | 31.5 | 14.4 | 22.7 |
| 19-25 y | 17 | 8 | 25 | 16.6 | 8.3 | 12.6 |
| 26-35 y | 49 | 19 | 68 | 27.1 | 10.6 | 18.9 |
| 36-45 y | 30 | 20 | 50 | 17.6 | 11.8 | 14.7 |
| Total (95% CI) | 129 | 67 | 196 | 16.8 (13.9-19.7)b | 8.7 (6.6-10.8)b | 12.7 (10.9-14.5)c |
aIncidence rate was calculated as number of cases per 100,000 person-years.
bAge-adjusted to the 2010 US population.
cAge- and sex-adjusted to the 2010 US population.
Figure 1.
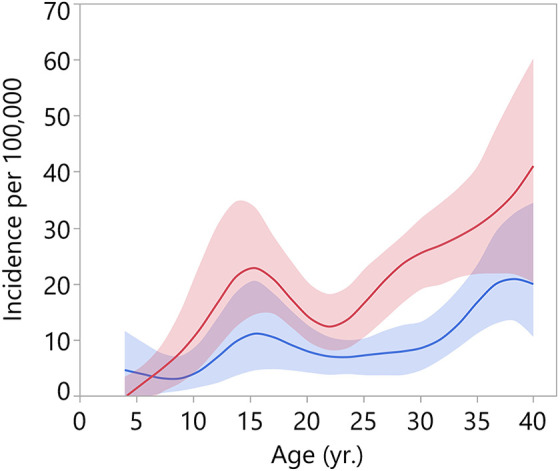
Trends and 95% CIs for age-specific incidence of hip dysplasia diagnosis in male patients (blue) and female patients (red).
Trends in Hip Dysplasia Diagnosis
Table 4 and Figure 2 illustrate the age- and sex-specific annual incidence of hip dysplasia diagnosis (in cases per 100,000 person-years) over a 17-year time period (2000-2016). Total age- and sex-adjusted incidence was highest in the years 2010-2016 (13.9 [95% CI, 11.4-16.8]; P < .41). Total age- and sex-adjusted incidence was similar in the years 2000-2004 and 2005-2009 (11.6 [95% CI, 8.5-14.8] and 11.9 [95% CI, 8.6-15.1]; P < .59). The highest incidence of hip dysplasia diagnosis occurred in 2005-2009 and involved female patients aged 14-18 years (43.8/100,000; P < .01); female patients aged 14-18 and 26-35 years had the highest incidence rates across all years. The highest incidence in male patients occurred during the years 2000-2004 (9.1/100,000). During the years 2000-2004, male patients aged 36 to 45 had the highest incidence rate of hip dysplasia diagnosis (13.3/100,000; P < .01). Male patients aged 14 to 18 had the highest incidence rate across the years 2005-2009 and 2010-2016 (20.9/100,000 and 11.4/100,000; P < .04). Total male and female trends in incidence rates over time were not significant (P < .95 and P < .69, respectively).
Table 4.
Trends in Age- and Sex-Specific Incidence of Dysplasia Over Time of Diagnosis, 2000-2016a
| 2000-2004 | 2005-2009 | 2010-2016 | |||||
|---|---|---|---|---|---|---|---|
| Age Group | No. | Incidence Rate | No. | Incidence Rate | No. | Incidence Rate | P Value |
| Male | |||||||
| ≤13 y | 6 | 8.9 | 1 | 1.4 | 1 | 0.9 | .01 |
| 14-18 y | 3 | 12.4 | 5 | 20.9 | 4 | 11.4 | .04 |
| 19-25 y | 1 | 3.7 | 2 | 7.2 | 5 | 11.8 | .72 |
| 26-35 y | 3 | 6.3 | 4 | 7.7 | 12 | 15.0 | .14 |
| 36-45 y | 7 | 13.3 | 6 | 12.5 | 7 | 10.3 | .01 |
| Total | 20 | 9.1 | 18 | 8.1 | 29 | 8.7 | .96 |
| Female | |||||||
| ≤13 y | 5 | 7.8 | 3 | 4.4 | 0 | 0.0 | .001 |
| 14-18 y | 5 | 21.9 | 10 | 43.8 | 10 | 29.6 | .001 |
| 19-25 y | 1 | 3.7 | 4 | 13.6 | 12 | 26.3 | .01 |
| 26-35 y | 12 | 25.1 | 10 | 19.2 | 27 | 33.3 | .86 |
| 36-45 y | 9 | 17.0 | 7 | 14.4 | 14 | 20.5 | .01 |
| Total | 32 | 14.9 | 34 | 15.4 | 63 | 18.9 | .69 |
| Total (95% CI)b | 11.6 (8.5-14.8) | 11.9 (8.6-15.1) | 13.9 (11.4-16.8) | ||||
aIncidence rate was calculated as number of cases per 100,000 person-years.
bAge- and sex-adjusted to the 2010 US population.
Figure 2.
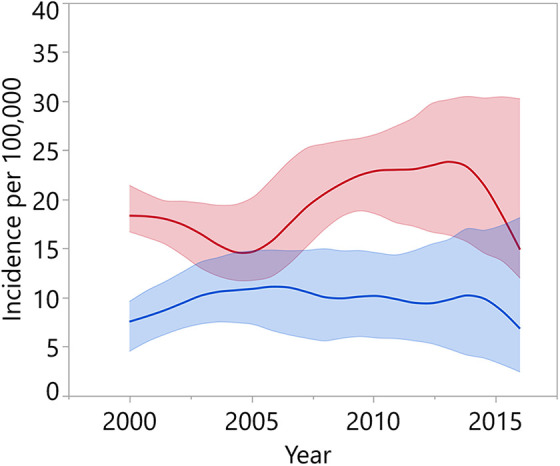
Trends and 95% CIs for age-adjusted incidence of hip dysplasia diagnosis over time in male patients (blue) and female patients (red).
Hip Dysplasia Management Trends Over Time
Table 5 describes the trends in management of hip dysplasia in patients diagnosed with hip pain over time. For patients diagnosed with hip dysplasia, nonoperative treatment with physical therapy was common (67%). Intra-articular steroid injection was administered to 29% of hips (57 hips). The number of intra-articular steroid injections did not change over time (P < .28). Hip arthroscopy was performed in 10% of the entire cohort (20 hips), a number that significantly increased between 2000 and 2016 (P < .01). Hip arthroscopies were performed on 0% (0/52) of the hips diagnosed with dysplasia in the years 2000-2004, 6% (3/52) of the hips diagnosed in the years 2005-2009, and 18% (17/92) of the hips diagnosed in the years 2010-2016. PAO was performed in 9% (17 hips). The number of PAOs did not change significantly over time (P < .08).
Table 5.
Trends in Management of Hip Dysplasia in Patients Diagnosed With Hip Pain, 2000-2016a
| 2000-2004 (n = 52) | 2005-2009 (n = 52) | 2010-2016 (n = 92) | Total (N = 196) | P Value | |
|---|---|---|---|---|---|
| Participation in physical therapy | 33 (63) | 30 (58) | 69 (75) | 132 (67) | .34 |
| Intra-articular steroid injection | 13 (25) | 14 (27) | 30 (33) | 57 (29) | .28 |
| Hip arthroscopy | 0 (0) | 3 (6) | 17 (18) | 20 (10) | .01 |
| Periacetabular osteotomy | 1 (2) | 2 (4) | 14 (15) | 17 (9) | .08 |
aData are reported as No. (% of group).
Discussion
The incidence of hip dysplasia in patients with hip pain is not well established in the literature. This study found that the population-based incidence of hip dysplasia diagnosis in patients presenting with hip pain was 12.7 per 100,000 person-years. Female patients had double the age-adjusted incidence of male patients (16.8 vs 8.7), and the highest age-adjusted incidence occurred in the age range of 14 to 18 years in both sexes. This study also analyzed management trends and found that patients with hip dysplasia were treated with physical therapy (67%), intra-articular steroid injection (29%), hip arthroscopy (10%), and PAO (9%). The use of hip arthroscopy significantly increased; however, the use of intra-articular steroid injection and PAO did not significantly change over time.
Little has been reported in the literature regarding the incidence of hip dysplasia diagnosis or the average age of patients presenting with dysplasia. Previous studies have found the prevalence of hip dysplasia to be between 3.6% and 12.8%8,9; however, this did not account for the age at which patients presented with hip pain. With regard to age, the current study found that patients with dysplasia presented at a mean age of 26.7 ± 9.8 years; however, the highest age-adjusted incidence occurred in the age range of 14 to 18 years in both sexes. Previous studies have reported that symptomatic patients usually present in young/middle adulthood.1,10,12 Lerch et al12 found that the mean age of 78 patients with hip dysplasia presenting with symptomatic hip pain was 29 ± 9 years. Matsuda et al15 reported a mean age of 32 ± 13.8 years in a sample of 133 patients with dysplasia who underwent isolated hip arthroscopy. It is well accepted in the literature that hip dysplasia is a risk factor for the development of hip osteoarthritis, and it has been estimated that that up to 50% of patients with dysplasia develop osteoarthritis by the age of 50 years.6 It is important that these patients are correctly identified upon presentation when they are younger and have less joint space narrowing, a point at which more treatment options are available.6,9,15,18,19
Female patients had double the age-adjusted incidence of hip dysplasia compared with male patients (16.8 vs 8.7, respectively). Female sex has been reported to be a risk factor for the development of hip dysplasia in the literature.6,13 In the current study, 87 hips underwent MRI, and of those, 67 hips (77%) were diagnosed with a labral tear. Labral tears have been shown to be a risk factor for the development of osteoarthritis7,14,16 and were found to be associated with poor outcomes in patients treated with PAO.20 Total age- and sex-adjusted incidence of hip dysplasia diagnosis was highest in the years 2010-2016. It is unclear why incidence was highest during this period, but it could potentially be because of increased physician awareness of hip pathologies compared with the earlier time periods.
Nonoperative management with physical therapy was the most common treatment for patients with dysplasia (67%). At our institution, physical therapy is routinely prescribed as a first-line treatment for patients with hip pain. The number of hip arthroscopy and PAO procedures increased over time; however, the increase was significant only for hip arthroscopy. This was not surprising because the use of hip arthroscopy became more widely adopted in the late 2000s and early 2010s, with especially dramatic increases in hip arthroscopic procedures between 2011 and 2015.2,21 Although the use of hip arthroscopy for patients with dysplasia remains controversial, previous studies have suggested that patients with borderline to mild dysplasia have favorable results with labral repair and capsular plication.1,5,11 More research is needed to see whether PAO changes the natural progression of hip dysplasia. It is important that physicians consider labral pathology when examining patients with dysplasia, because surgical treatment outcomes will be limited in the long term if the labral pathology is not addressed.
There are a few limitations to consider for this study. The study is limited by its retrospective design and the lack of a control group. Physician understanding of hip pain, electronic documentation, and imaging improved over the 16-year period. It is possible that patients in the early time periods were accidentally excluded; however, this should be less likely because dysplasia was confirmed via imaging, and all patients had imaging that was reviewed by board-certified musculoskeletal radiologists at the time of this study. This cohort is based on a pain cohort, not a hip dysplasia cohort. Thus, patients who were 14 to 50 years old who had dysplasia but did not have ICD codes of hip pain and 2 radiographs were excluded from this study. Patients who were diagnosed with dysplasia before age 14 years were also excluded. These younger patients likely presented with more severe dysplasia resulting in earlier operations, and their exclusion could have potentially selected for less severe cases. In addition, asymptomatic patients and those with only 1 set of radiographs were excluded.
It is important to consider unintentional biases that regional databases may introduce. Olmstead County is ranked first overall in Minnesota for clinical care and health factors and eighth for socioeconomic factors.4 Olmstead County is also well above the national average for the ratio of population to primary care physicians and has a much lower percentage of uninsured people younger than 65 years.4 It is possible that areas with lower access to health care or higher rates of uninsured patients may entail delayed care, which could lead to higher progression of hip disease at initial presentation. Ultimately, health disparities may result in patients presenting with more advanced osteoarthritis, thus limiting their ability to undergo joint-preserving procedures. Last, the majority of the patients in this population were White (85.7% in Olmstead County vs the US average of 72.4% in 2010), which could limit the generalizability of these results because the incidence of hip dysplasia varies by ethnicity, with Native Americans having a higher incidence of dysplasia and African Americans having a much lower incidence of dysplasia compared with the White population.13
Conclusion
The incidence of hip dysplasia diagnosis in patients presenting with hip pain was 12.7 per 100,000 person-years. Female patients had twice the age-adjusted incidence of male patients, and the highest age-adjusted incidence occurred in the age range of 14 to 18 years in both sexes. The use of hip arthroscopy to treat patients with hip dysplasia significantly increased over time.
Acknowledgment
The authors thank Jun Zhou, MD, PhD, for his help with reviewing radiographs for this study.
Footnotes
Final revision submitted September 8, 2020; accepted October 9, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was partially funded by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. M.D.L. has a family member who has received consulting fees from Linvatec, Ossur, and Smith & Nephew and royalties from Arthrex, Smith & Nephew, and Thieme. R.J.S. has received consulting fees from Orthaligh and Zimmer and royalties from Zimmer. R.T.T. has received consulting fees from Medical Device Business Services and Medtronic and royalties from DePuy. B.A.L. has received research support from Biomet, Smith & Nephew, and Stryker; consulting fees from Smith & Nephew; speaking fees from Linvatec; and royalties from Arthrex. A.J.K. has received research support from Aesculap/B.Braun, Arthritis Foundation, Ceterix, Exactech, Gemini Medical, and Histogenics; consulting fees from Arthrex, DePuy, JRF Ortho, and Vericel; and royalties from Arthrex; has stock/stock options in Responsive Arthroscopy; and is a board or committee member for the Musculoskeletal Transplantation Foundation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic (No. 17-004959, 030-OMC-17).
References
- 1. Bolia IK, Briggs KK, Locks R, et al. Prevalence of high-grade cartilage defects in patients with borderline dysplasia with femoroacetabular impingement: a comparative cohort study. Arthroscopy. 2018;34(8):2347–2352. [DOI] [PubMed] [Google Scholar]
- 2. Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825–1830. [DOI] [PubMed] [Google Scholar]
- 3. Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl_4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. County Health Rankings & Roadmaps—Minnesota. Robert Wood Johnson Foundation & University of Wisconsin Population Health Institute. Accessed August 5, 2020. https://www.countyhealthrankings.org/app/minnesota/2020/rankings/olmsted/county/outcomes/overall/snapshot
- 5. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41(11):2591–2598. [DOI] [PubMed] [Google Scholar]
- 6. Gala L, Clohisy JC, Beaule PE. Hip dysplasia in the young adult. J Bone Joint Surg Am. 2016;98(1):63–73. [DOI] [PubMed] [Google Scholar]
- 7. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92(5):1162–1169. [DOI] [PubMed] [Google Scholar]
- 9. Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford). 2005;44(2):211–218. [DOI] [PubMed] [Google Scholar]
- 10. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423–429. [DOI] [PubMed] [Google Scholar]
- 11. Larson CM, Ross JR, Stone RM, et al. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44(2):447–453. [DOI] [PubMed] [Google Scholar]
- 12. Lerch TD, Todorski IAS, Steppacher SD, et al. Prevalence of femoral and acetabular version abnormalities in patients with symptomatic hip disease: a controlled study of 538 hips. Am J Sports Med. 2018;46(1):122–134. [DOI] [PubMed] [Google Scholar]
- 13. Loder RT, Skopelja EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lodhia P, Gui C, Chandrasekaran S, et al. The economic impact of acetabular labral tears: a cost-effectiveness analysis comparing hip arthroscopic surgery and structured rehabilitation alone in patients without osteoarthritis. Am J Sports Med. 2016;44(7):1771–1780. [DOI] [PubMed] [Google Scholar]
- 15. Matsuda DK, Wolff AB, Nho SJ, et al. Hip dysplasia: prevalence, associated findings, and procedures from large multicenter arthroscopy study group. Arthroscopy. 2018;34(2):444–453. [DOI] [PubMed] [Google Scholar]
- 16. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J., The Otto E. Aufranc award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. [DOI] [PubMed] [Google Scholar]
- 17. Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ, III. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sankar WN, Duncan ST, Baca GR, et al. Descriptive epidemiology of acetabular dysplasia: the Academic Network of Conservational Hip Outcomes Research (ANCHOR) periacetabular osteotomy. J Am Acad Orthop Surg. 2017;25(2):150–159. [DOI] [PubMed] [Google Scholar]
- 19. Schmitz MR, Murtha AS, Clohisy JC, Group AS. Developmental dysplasia of the hip in adolescents and young adults. J Am Acad Orthop Surg. 2020;28(3):91–101. [DOI] [PubMed] [Google Scholar]
- 20. Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466(7):1633–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Westermann RW, Day MA, Duchman KR, et al. Trends in hip arthroscopic labral repair: an American Board of Orthopaedic Surgery database study. Arthroscopy. 2019;35(5):1413–1419. [DOI] [PubMed] [Google Scholar]
- 22. Wyles CC, Heidenreich MJ, Jeng J, et al. The John Charnley award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475(2):336–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wyles CC, Vargas JS, Heidenreich MJ, et al. Natural history of the dysplastic hip following modern periacetabular osteotomy. J Bone Joint Surg Am. 2019;101(10):932–938. [DOI] [PubMed] [Google Scholar]


