Abstract
Background:
Few studies have attempted to identify risk factors associated with irreparable meniscal tears at anterior cruciate ligament reconstruction (ACLR) and to describe follow-up data, such as the failure rate, after meniscal repair.
Purpose:
To investigate the associations of age, sex, body mass index (BMI), time to surgery (TTS), and preinjury Tegner score with the presence of meniscal injuries and irreparable meniscal tears at primary ACLR.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A retrospective review was performed on 784 patients who underwent primary ACLR by a single surgeon between 2005 and 2017 (406 men and 378 women; mean age, 25.8 years; mean BMI, 23.1; median TTS, 3 months; median preinjury Tegner score, 7). All patients had a minimum follow-up of 12 months (mean postoperative follow-up, 33.0 months). Multivariate logistic regression analysis was conducted to determine the association of patient variables with the presence of meniscal injuries and irreparable meniscal tears during primary ACLR.
Results:
The risk factor for medial meniscal injuries was TTS ≥3 months (odds ratio [OR], 4.213; 95% CI, 3.104-5.719; P < .001). The presence of irreparable medial meniscal tears increased with older age (OR, 1.053; 95% CI, 1.024-1.084; P < .001), higher BMI (OR, 1.077; 95% CI, 1.003-1.156; P = .042), and TTS ≥3 months (OR, 1.794; 95% CI, 1.046-3.078; P = .034). On multivariate analysis, none of the variables were significantly associated with lateral meniscal injuries and irreparable meniscal tears. The failure rate, defined as patients who needed additional medial meniscal surgery after medial meniscal repair, was 4.6%.
Conclusion:
Time from ACL injury to reconstruction of ≥3 months was strongly associated with medial meniscal injuries and irreparable medial meniscal tears at primary ACLR. Older age and increased BMI were also risk factors for the presence of irreparable medial meniscal tears at ACLR.
Keywords: knee, anterior cruciate ligament, meniscus, irreparable meniscal tear
Anterior cruciate ligament (ACL) injury is one of the most common injuries in sport. Although return-to-play rates after ACL reconstruction (ACLR) are higher12,23,31 than those after nonoperative treatment,11,34,37 some athletes with ACL deficiency resume previous levels of activity without surgery.41 However, an ACL deficiency results in abnormal knee kinematics and instability and leads to meniscal and cartilage injury due to recurrent pivoting trauma.13,14,15 Even less active patients have an increased risk of medial meniscal and cartilage injuries compared with active patients.36
Several previous studies28,33,40 have reported the presence of meniscal injury after ACL injury and have recommended early ACLR. Although the meniscus should be preserved as much as possible at ACLR, some meniscal tears are irreparable owing to their complexity and severity.5,10 In addition, it is likely that some of the repaired menisci might rerupture and require additional surgery after a simultaneous ACLR and meniscal repair. However, few studies have attempted to identify risk factors related to irreparable meniscal tear at ACLR and describe follow-up data of the investigated patients regarding progress of the meniscus after a simultaneous ACLR and meniscal repair, such as the failure rate after meniscal repair. Furthermore, most previous studies3,5,7,9,10,17,18,25 have entailed data from multiple surgeons with different treatment decisions and surgical techniques for meniscal tears.
The purpose of this retrospective study was to investigate the associations of age, sex, body mass index (BMI), time from injury to surgery (TTS), and preinjury Tegner score with the presence of meniscal injuries and irreparable meniscal tears at primary ACLR by a single surgeon (T.T.). We hypothesized that (1) the presence of medial meniscal injuries would be increased in young and active patients and (2) older age and increased BMI could lead to meniscal degeneration and thereby reduce the repairability of medial menisci at ACLR.
Methods
This was a retrospective cohort study of 784 patients (406 men and 378 women) who underwent primary ACLR by a single surgeon (T.T.) between 2005 and 2017. The study protocol was approved by the ethics committee of our institution, and informed consent was obtained from all participants. The study inclusion criterion was in-person postoperative follow-up of >12 months. Exclusion criteria were multiligament knee injury, revision ACLR, previous knee injury or surgery on the affected or contralateral knee, follow-up <12 months, age >50 years at the time of surgery, and TTS > 120 months. The flowchart of patient inclusion is shown in Figure 1.
Figure 1.
Flowchart of patient inclusion in the study. ACLR, anterior cruciate ligament reconstruction; TTS, time to surgery.
Tear Classifications
ACLR was performed using bone–patellar tendon–bone autograft42 or via ACL double-bundle reconstruction using hamstring autograft.43 Based on surgical findings, meniscal tear patterns were classified as simple (horizontal, vertical longitudinal, and small), bucket-handle, and complex (multiplane combinations, flap, oblique, parrot beak, and degenerative).19 In addition, meniscal tears were graded according to the classification of Anderson and Anderson2 and Laible et al20 (grade 0, intact; grade 1, nonsurgical tear; grade 2, reparable tear of <50% thickness; grade 3, reparable bucket-handle tear; grade 4, irreparable tear of >50% thickness; and grade 5, irreparable bucket-handle tear).
Meniscal reparability was defined based on standard meniscal repair guidelines during ACLR. Simple or bucket-handle meniscal tears without degeneration were repaired, whereas complex or degenerative meniscal tears were partially resected. Reparable meniscal tears were fixed using the inside-out technique. For relatively small meniscal tears, such as ramp lesions of medial meniscus and popliteomeniscal fascicle tears of lateral meniscus, the FasT-Fix (Smith and Nephew Endoscopy) all-inside meniscal repair was preferred. Irreparable meniscal tears (classified as grades 4 and 5) were those unable to retain the entire normal (medial/lateral) meniscal shape at primary ACLR. Meniscal repair failure was defined as the need for additional meniscal surgery at the same location of the initial repair.
Rehabilitation
The same postoperative rehabilitation was carried out for all patients. A knee brace was applied for 1 week postoperatively. The patients were allowed partial weightbearing at 1 week and full weightbearing at 4 weeks. In patients with meniscal repairs, full weightbearing was allowed at 6 weeks. Vigorous sports activity was allowed at about 8 months postoperatively.
Postoperative Clinical Evaluation
The presence of meniscal tear at primary ACLR was collected from the analysis of surgical reports. The postoperative clinical evaluation was carried out at 6-month intervals until 24 months postoperatively or at the last follow-up (in patients with >24 months of follow-up). Age at ACLR, sex, BMI, TTS, preinjury Tegner score, ACL graft selection, and the follow-up period were obtained from medical records. Additional surgeries for meniscal tears and subsequent ACL injuries after ACLRs were investigated by analyzing medical records and surgical reports. Based on these data, the failure rate after meniscal repair was calculated to verify whether our treatment decisions and surgical treatments for meniscal tears were appropriate.
Statistical Analysis
The t test and chi-square test were used to compare continuous variables and categorical variables, respectively. To investigate the association of age, BMI, and Tegner score with the presence of meniscal injuries (tear grades 1-5) and irreparable meniscal tears (grades 4 and 5) during primary ACLRs, a fixed-effect multivariate logistic regression analysis was conducted. The analysis was separately performed on medial and lateral sides. The model was adjusted for characteristic data (patient sex) and potential confounding factors (TTS ≥3 months) in addition to age, BMI, and Tegner score. The cutoff value for TTS, used to predict patients with an increased risk for medial meniscal injuries, was evaluated using receiver operating characteristic (ROC) curve analysis. Statistical tests were considered significant at P < .05. All P values were 2-sided. All analyses were performed using SAS Version 9.4 (SAS Institute).
Results
Patient Characteristic Data
ACLR procedures were performed using bone–patellar tendon–bone autografts in 268 patients and hamstring autografts in 516 patients. The mean postoperative follow-up period of the 784 study patients was 33 months. The characteristic data of the 784 study patients are shown in Table 1.
Table 1.
Patient Characteristic Dataa
| Age, y | |
| Mean ± SD | 25.8 ± 10.1 |
| Median (range) | 22 (13-50) |
| Sex, male/female, n | 406/378 |
| BMI | |
| Mean ± SD | 23.1 ± 3.6 |
| Median (range) | 22.3 (15.8-41.7) |
| TTS, mo | |
| Mean ± SD | 11.6 ± 22.0 |
| Median (range) | 3 (1-120) |
| Preinjury Tegner score | |
| Mean ± SD | 7.1 ± 1.3 |
| Median (range) | 7 (3-9) |
| ACL graft, male/female, n | |
| BPTB autograft | 157/111 |
| Hamstring autograft | 250/266 |
| Follow-up period, mo | |
| Mean ± SD | 33.0 ± 27.6 |
| Median (range) | 24 (12-154) |
aACL, anterior cruciate ligament; BMI, body mass index; BPTB, bone–patellar tendon–bone; TTS, time to surgery.
Postoperative Clinical Evaluation
Medial meniscectomy was required in 15 patients at a mean of 32.7 months after ACLR. Of these, 9 patients experienced failure after medial meniscal repair at ACLR (the failure rate after medial meniscal repairs was 4.6%). Lateral meniscectomy was needed in 1 patient at 27 months after ACLR. In terms of subsequent ACL injuries, 43 patients experienced ACL graft ruptures at a mean of 32.3 months, and 56 patients had contralateral ACL injuries at a mean of 34.1 months (Table 2).
Table 2.
Results of Postoperative Clinical Evaluationa
| No. or Mean ± SD | |
|---|---|
| Medial meniscectomy | 15 |
| Time after primary ACLR, mo | 32.7 ± 26.0 |
| Failure of meniscal repair at primary ACLR | 9 |
| Lateral meniscectomy | 1 |
| Time after primary ACLR, mo | 27 |
| Failure of meniscal repair at primary ACLR | 0 |
| Subsequent ACL injury | |
| ACL graft rupture | 43 |
| Time after primary ACLR, mo | 32.3 ± 30.6 |
| BPTB autograft, M/F | 1/4 |
| Hamstring autograft, M/F | 22/16 |
| Contralateral ACL injury | 56 |
| Time after primary ACLR, mo | 34.1 ± 26.2 |
| BPTB autograft, M/F | 9/14 |
| Hamstring autograft, M/F | 11/22 |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BPTB, bone–patellar tendon–bone; F, female; M, male.
Meniscal Tear Characteristics
The meniscal tear patterns at surgery are listed in Table 3. There were 325 medial meniscal tears (41.5%) and 335 lateral meniscal tears (42.7%). Overall, 131 medial meniscal tears (40.3%) and 143 lateral meniscal tears (42.7%) were irreparable (tear grades 4 and 5) at ACLR.
Table 3.
Meniscal Tear Pattern and Gradinga
| Medial Meniscus | Lateral Meniscus | |
|---|---|---|
| Meniscal tear patternb | ||
| Intact | 459 | 449 |
| Simple tear | 176 | 184 |
| Bucket-handle tear | 68 | 21 |
| Complex tear | 81 | 130 |
| Meniscal tear gradec | ||
| 0 | 459 | 449 |
| 1 | 30 | 112 |
| 2 | 146 | 72 |
| 3 | 18 | 8 |
| 4 | 81 | 130 |
| 5 | 50 | 13 |
aValues are expressed as numbers of cases.
bAccording to Krych et al.19
ROC Curve Analysis
In the ROC curve analysis, TTS had an area under the curve of 0.683 (95% CI, 0.634-0.732) for predicting medial meniscal injuries. The distance from the top left corner of the ROC curve were used to determine the cutoff value. The optimal TTS cutoff value was 3 months (Figure 2).
Figure 2.
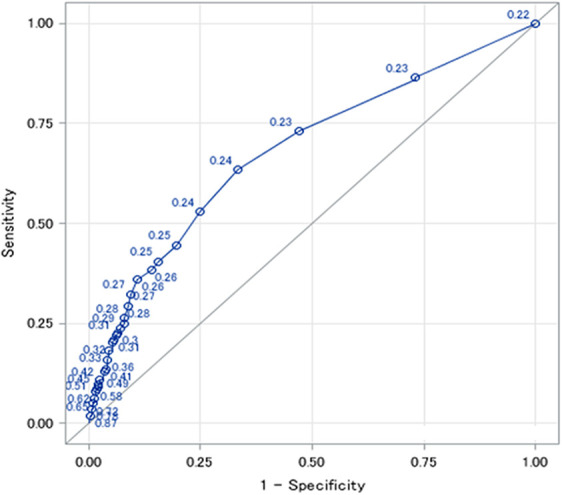
Receiver operating characteristic curve analysis for predicting medial meniscal injury.
Univariate Analyses
The results of univariate analyses for association with the presence of meniscal injuries and irreparable meniscal tears are shown in Table 4.
Table 4.
Univariate Analyses for Association With the Presence of Meniscal Injuries and Irreparable Meniscal Tearsa
| MM Injury | Irreparable MM Tear | |||||
|---|---|---|---|---|---|---|
| Variable | No (n = 459) | Yes (n = 325) | Pb | No (n = 194) | Yes (n = 131) | Pb |
| Age, y | 26.2 ± 10.4 | 25.1 ± 9.6 | .137 | 23.3 ± 8.9 | 27.9 ± 10.1 | <.001 |
| BMI | 22.9 ± 3.6 | 23.3 ± 3.6 | .140 | 22.9 ± 3.3 | 23.9 ± 3.8 | .012 |
| Male sex | 237 (52) | 169 (52) | .944 | 95 (49) | 74 (56) | .183 |
| TTS ≥3 mo | 71 (15) | 159 (48) | <.001 | 77 (37) | 82 (63) | <.001 |
| Preinjury Tegner score ≥7 | 288 (63) | 220 (68) | .172 | 137 (45) | 83 (63) | .170 |
| LM Injury | Irreparable LM Tear | |||||
| Variable | No (n = 449) | Yes (n = 335) | Pb | No (n = 192) | Yes (n = 143) | Pb |
| Age, y | 26.6 ± 10.3 | 24.7 ± 9.7 | .008 | 24.4 ± 9.7 | 25.0 ± 9.7 | .608 |
| BMI | 23.0 ± 3.6 | 23.2 ± 3.6 | .376 | 23.1 ± 3.7 | 23.4 ± 3.4 | .414 |
| Male sex | 227 (51) | 179 (53) | .425 | 96 (50) | 83 (58) | .144 |
| TTS ≥3 mo | 129 (29) | 101 (30) | .667 | 45 (23) | 56 (39) | .002 |
| Preinjury Tegner score ≥7 | 273 (61) | 235 (70) | .007 | 135 (70) | 100 (70) | .940 |
aData are presented as mean ± SD or n (%). Bolded P values indicate statistically significant difference between groups (P < .05). BMI, body mass index; LM, lateral meniscal; MM, medial meniscal; TTS, time to surgery.
bDetermined using t test or chi-square test.
Multivariate Analyses
Presence of Meniscal Injuries at ACLR
Multivariate analyses with age per 1-year increase, male sex, BMI per 1-unit increase, TTS ≥3 months, and preinjury Tegner score of ≥7 revealed that the risk factor for medial meniscal injuries was TTS ≥3 months (odds ratio [OR], 4.213; 95% CI, 3.104-5.719; P < .001). On multivariate analysis, none of the variables were significantly associated with lateral meniscal injuries (Table 5).
Table 5.
Multivariate Logistic Regression Analyses for Association With the Presence of Meniscal Injuriesa
| Variable | Medial Meniscus, OR (95% CI) | P | Lateral Meniscus, OR (95% CI) | P |
|---|---|---|---|---|
| Age per 1-y increase | 0.990 (0.973-1.007) | .250 | 0.985 (0.969-1.002) | .082 |
| Male sex | 1.112 (0.797-1.552) | .533 | 0.995 (0.728-1.360) | .976 |
| BMI per 1-unit increase | 1.042 (0.996-1.089) | .076 | 1.025 (0.982-1.070) | .253 |
| TTS ≥3 months | 4.213 (3.104-5.719) | <.001 | 1.099 (0.826-1.463) | .517 |
| Preinjury Tegner score ≥7 | 1.283 (0.884-1.864) | .190 | 1.323 (0.931-1.880) | .119 |
aBolded P value indicates statistical significance (P < .05). BMI, body mass index; OR, odds ratio; TTS, time to surgery.
Presence of Irreparable Meniscal Tears at ACLR
The presence of irreparable medial meniscal tears increased with older age (OR, 1.053; 95% CI, 1.024-1.084; P < .001), increased BMI (OR, 1.077; 95% CI, 1.003-1.156; P = .042), and TTS ≥3 months (OR, 1.794; 95% CI, 1.046-3.078; P = .034). The presence of irreparable lateral meniscal tears was not significantly associated with any factors (Table 6).
Table 6.
Multivariate Analyses for Association With the Presence of Irreparable Meniscal Tearsa
| Variable | Medial Meniscus, OR (95% CI) | P | Lateral Meniscus, OR (95% CI) | P |
|---|---|---|---|---|
| Age per 1-y increase | 1.053 (1.024-1.084) | <.001 | 0.997 (0.969-1.025) | .816 |
| Male sex | 0.818 (0.480-1.393) | .460 | 0.755 (0.452-1.263) | .285 |
| BMI per 1-unit increase | 1.077 (1.003-1.156) | .042 | 1.016 (0.948-1.089) | .658 |
| TTS ≥3 months | 1.794 (1.046-3.078) | .034 | 1.129 (0.711-1.794) | .607 |
| Preinjury Tegner score ≥7 | 1.242 (0.683-2.261) | .477 | 0.876 (0.479-1.601) | .666 |
aBolded P values indicate statistical significance (P < .05). BMI, body mass index; OR, odds ratio; TTS, time to surgery.
Discussion
The study results indicated that a delay in TTS of ≥3 months was strongly associated with the presence of medial meniscal injuries and irreparable medial meniscal tears at ACLR, whereas lateral meniscal injuries and irreparable lateral meniscal tears were not related to TTS. Additionally, older age and higher BMI affected the presence of irreparable medial meniscal tears at ACLR.
Age
Increased age was not related to the presence of medial meniscal injuries in this study. Similarly, Yoo et al47 reported no statistically significant relationship between changes in medial meniscal lesions and patient age in a preoperative magnetic resonance imaging study. Previous studies6,24,26 among adolescent patients have claimed that the presence of secondary meniscal injuries, defined as tears that develop after the initial ACL injury, was relatively high and the rate of medial meniscal injury increased with the delay in ACLR. In contrast to studies of young patients, Hagmeijer et al10 found a lower rate of secondary meniscal tears after ACL injury in older patients and suggested that the lower activity level of older patients might explain the lower rate of secondary meniscal injuries. Although increased age would lead to degenerative changes in menisci, older patients did not have medial meniscal injuries presumably because of the low risk of secondary meniscal injuries.
In terms of irreparable meniscal tears during primary ACLRs, increased age was a significant risk factor for the medial menisci in the current study. Chhadia et al5 investigated relationships between some variables (age, sex, and TTS) and meniscal repair rates and showed that increasing age was associated with a decreased rate of medial meniscal repair. Everhart et al7 also indicated that increased patient age was an independent predictor of a degenerative tear requiring meniscectomy. Increased age should lead to degenerative changes of the medial menisci and promote irreparable medial meniscal tears.
Patient Sex
Male sex was not a risk factor for the presence of medial meniscal injuries at primary ACLR in the current study, whereas previous studies3,5,9,30 have shown that male patients demonstrated higher rates of medial meniscal injury than did female patients. Investigators have suggested that the association between increased meniscal injury and sex (male) could be related to a higher activity level and higher energy trauma.3 In contrast, Slauterbeck et al38 and Chhadia et al5 pointed out that female patients having surgery were younger and had a shorter time from ACL injury to surgery. Using a binary logistic regression model to adjust the potential confounders, Chhadia et al5 showed that sex (male) was not associated with the presence of medial meniscal injury.
Sex (male) was not associated with irreparable tears of the medial menisci in the current study. Krutsch et al18 reported that the rate of prognostically disadvantageous medial meniscal resection in women increased >6 months after ACL injury. O’Connor et al30 showed that, when ACLR was performed >26 weeks after injury, both men and women had increased risk of meniscal injuries but the rate at which the risk increased was much higher for women. Compared with men, women generally have weaker muscles supporting the knees, and higher ligament laxity, which may explain their results.46 Although men had an overall higher risk of meniscal injuries across all time intervals, women tended to incur subsequent additional meniscal injuries, which were less likely to be preserved due to degenerative changes,5,10 at a higher rate over time.30 Thus, sex (male) might not contribute to irreparable medial meniscal tears.
Body Mass Index
In the current study, increased BMI was significantly related to irreparable medial meniscal tears. In general, obesity (increased BMI) is likely to have both biomechanical and biochemical links to osteoarthritis.35,45 In patients with ACL injuries, higher BMI was found to be a risk factor for radiographic osteoarthritis in the medial compartment after ACLR27 and was associated with medial compartment chondrosis at revision ACLR.4 Increased BMI accelerated degeneration of medial menisci and reduced repairability of medial meniscal tears in the current study. In contrast to our result regarding irreparable medial meniscal tear, Kluczynski et al17 reported that BMI was not significantly related to the management of medial meniscal injuries. However, those investigators categorized their patients into 3 groups (normal, overweight, and obese) according to BMI, and the apparent discrepancy may be due to differences in statistical methods.
Time to Surgery
In our ROC curve analysis, the optimal TTS cutoff value for predicting medial meniscal injuries was 3 months. In a multivariate analysis, TTS (≥3 months) was strongly associated with medial meniscal injuries. This result is similar to the results of previous studies reporting that increased TTS was a risk factor for increased medial meniscal injuries and a greater factor than was age.40,48 Although no consensus has been reached with regard to the ideal timing of ACLR in terms of reducing secondary meniscal injury in ACL-deficient knees,47 previous studies have reported that timelines for medial meniscal injuries were 6 months5,10,47,49 or 12 months3,25,36 after ACL injuries. Our TTS (≥3 months) for medial meniscal injuries was relatively earlier. This discrepancy regarding the relationship of TTS to increased medial meniscal injuries could be attributable to differences in physical activity level,3 the studies’ sample sizes, the number of surgeons participating in the studies, and the time periods into which the surgeries are grouped.25
The presence of irreparable medial meniscal tears in the current study was associated with TTS of ≥3 months, which was earlier compared with previous studies. Chhadia et al5 reported that the medial meniscal repair rate decreased with TTS beyond 12 months. Krutsch et al18 found a significantly higher number of prognostically favorable and reparable concomitant meniscal lesions in the first 6 months after ACL trauma compared with the second 6 months after ACL trauma. Similar to our results, Everhart et al7 reported that the delay of surgery beyond 8 weeks significantly increased the odds that a tear would require meniscectomy and significantly decreased the odds that a tear would require repair. However, their study included 78 (12.8%) patients who had previous non-ACL surgeries in ACL-injured knees, which could act as a confounder to their findings. In the present study, the OR of TTS ≥3 months for irreparable medial meniscal tear was higher compared with that of other factors. ACLR should be performed within 3 months after ACL injury to preserve medial meniscal health and normal knee kinematics and to reduce stress forces on the ACL graft.32
Preinjury Tegner Score
Preinjury Tegner score was not statistically associated with the presence of either medial meniscal injuries or irreparable medial meniscal tears, although we expected that some patients with high preinjury Tegner score would resume previous levels of activity after ACL injuries and that there would be an association between preinjury Tegner score and the presence of medial meniscal injuries. Ralles et al36 reported that medial meniscal injuries were significantly observed in less active patients. Kluczynski et al17 found that sports-related injuries predicted fewer medial meniscal injuries and medial meniscectomy. In particular, the number of instability episodes after ACL injury was correlated with medial meniscal tears.17 Therefore, medial meniscal injuries may be related to postinjury rather than preinjury activity level.
Lateral Meniscal Injury
The presence of lateral meniscal injuries was not associated with any factors (age, sex, BMI, TTS, and preinjury Tegner score) in this study. Similarly, previous studies5,25,36,47 have demonstrated that lateral meniscal injuries occurred more commonly at the time of the primary injury but not secondarily after the incident injury, whereas medial compartment injuries were caused by chronic stresses in an ACL-deficient knee.8,17 A possible reason for these results is that the lateral meniscus has a role in mobility and constraint1 whereas the medial meniscus is less mobile and less able to follow the increased anterior and rotational translation of the tibia, especially in dynamic situations in the absence of the ACL3; thus, the medial meniscus is more likely than the lateral meniscus to undergo shear stresses.21
The presence of irreparable lateral meniscal tears was not related to any factors examined in the current study. Similarly, Chhadia et al5 showed that the lateral meniscal repair rate did not have any statistically significant associations, although the medial meniscal repair rate decreased with TTS beyond 12 months and with increasing age.
Limitations
There are several limitations to our study. Unlike previous studies, which involved multiple surgeons or centers, primary ACLR was performed by a single surgeon in the current study. Accordingly, indications for meniscal repair depended on 1 surgeon’s experience, which might have biased the results. In addition, this study lacked cartilage data. Cartilage damage and meniscectomies are the most significant predictors of the development of osteoarthritis.16 It has been reported that at ACLR, meniscal injuries requiring resection increased the risk of cartilage loss.22,29 Therefore, the meniscus should be preserved to prevent cartilage damage.
The follow-up period in the current study was relatively short, and 17% of the patients did not have a 12-month follow-up. Westermann et al44 reported that the average time to meniscal repair failure was 2.1 years for medial repairs and 3.7 years for lateral repairs performed at the time of ACLR and the failure rate after meniscal repairs varied from 5.5% to 14%.39 Although the failure rate after medial meniscal repair was 4.6% in the current study, a longer follow-up may have resulted in a higher rate of failure. In addition, the postoperative follow-up can be completed by mail or telephone; however, to evaluate clinical findings correctly, we included only those patients who could be followed up in person. Furthermore, we excluded patients with TTS >120 months, which might have influenced our results. Finally, ACLR procedures were performed using bone–patellar tendon–bone autograft or hamstring autograft (double-bundle reconstruction). Differences in the ACL grafts might have affected the subsequent meniscal status, healing process, and postoperative knee stability.
Conclusion
Time from ACL injury to ACLR of ≥3 months was strongly associated with medial meniscal injuries and irreparable medial meniscal tears at primary ACLR. Furthermore, older age and increased BMI were also risk factors for the presence of irreparable medial meniscal tears at ACLR, whereas male sex and preinjury Tegner score were not related to the presence of irreparable medial meniscal tears.
Acknowledgment
The authors thank Yoshihide Kanaoka, MD, PhD, for English language editing.
Footnotes
Final revision submitted September 13, 2020; accepted October 9, 2020.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Shimada Hospital (ID No. 2019-018).
References
- 1. Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000;18:109–115. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:275–281. [DOI] [PubMed] [Google Scholar]
- 3. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43:2966–2973. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Haas AK, Huston LJ, Nwosu SK, MARS Group, Wright RW. Association of meniscal status, lower extremity alignment, and body mass index with chondrosis at revision anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:1616–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39:1894–1899. [DOI] [PubMed] [Google Scholar]
- 6. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40:2128–2133. [DOI] [PubMed] [Google Scholar]
- 7. Everhart JS, Kirven JC, Abouljoud MM, DiBartola AC, Kaeding CC, Flanigan DC. Effect of delayed primary anterior cruciate ligament reconstruction on medial compartment cartilage and meniscal health. Am J Sports Med. 2019;47:1816–1824. [DOI] [PubMed] [Google Scholar]
- 8. Ghodadra N, Mall NA, Karas V, et al. Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg. 2013;26:185–193. [DOI] [PubMed] [Google Scholar]
- 9. Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian national knee ligament registry. Am J Sports Med. 2009;37:955–961. [DOI] [PubMed] [Google Scholar]
- 10. Hagmeijer MH, Hevesi M, Desai VS, et al. Secondary meniscal tears in patients with anterior cruciate ligament injury: relationship among operative management, osteoarthritis, and arthroplasty at 18-year mean follow-up. Am J Sports Med. 2019;47:1583–1590. [DOI] [PubMed] [Google Scholar]
- 11. Hawkins RJ, Misamore GW, Merritt TR. Followup of the acute nonoperated isolated anterior cruciate ligament tear. Am J Sports Med. 1986;14:205–210. [DOI] [PubMed] [Google Scholar]
- 12. Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412–417. [DOI] [PubMed] [Google Scholar]
- 13. Indelicato PA, Bittar ES. A perspective of lesions associated with ACL insufficiency of the knee: a review of 100 cases. Clin Orthop Relat Res. 1985;198:77–80. [PubMed] [Google Scholar]
- 14. Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188–193. [PubMed] [Google Scholar]
- 15. Karlsson J, Kartus J, Magnusson L, Larsson J, Brandsson S, Eriksson BI. Subacute versus delayed reconstruction of the anterior cruciate ligament in the competitive athlete. Knee Surg Sports Traumatol Arthrosc. 1999;7:146–151. [DOI] [PubMed] [Google Scholar]
- 16. Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010;38:455–463. [DOI] [PubMed] [Google Scholar]
- 17. Kluczynski MA, Marzo JM, Bisson LJ. Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med. 2013;41:2759–2765. [DOI] [PubMed] [Google Scholar]
- 18. Krutsch W, Zellner J, Baumann F, Pfeifer C, Nerlich M, Angele P. Timing of anterior cruciate ligament reconstruction within the first year after trauma and its influence on treatment of cartilage and meniscus pathology. Knee Surg Sports Traumatol Arthrosc. 2017;25:418–425. [DOI] [PubMed] [Google Scholar]
- 19. Krych AJ, McIntosh AL, Voll AE, Stuart MJ, Dahm DL. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36:1283–1289. [DOI] [PubMed] [Google Scholar]
- 20. Laible C, Stein DA, Kiridly DN. Meniscal repair. J Am Acad Orthop Surg. 2013;21:204–213. [DOI] [PubMed] [Google Scholar]
- 21. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883–888. [PubMed] [Google Scholar]
- 22. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. [DOI] [PubMed] [Google Scholar]
- 23. Mascarenhas R, Tranovich M, Kropf E, Fu F, Harner C. Bone-patellar tendon-bone autograft versus hamstring autograft anterior cruciate ligament reconstruction in the young athlete: a retrospective matched analysis with 2-10 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2012;20:1520–1527. [DOI] [PubMed] [Google Scholar]
- 24. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18:955–959. [DOI] [PubMed] [Google Scholar]
- 25. Mok YR, Wong KL, Panjwani T, Chan CX, Toh SJ, Krishna L. Anterior cruciate ligament reconstruction performed within 12 months of the index injury is associated with a lower rate of medial meniscus tears. Knee Surg Sports Traumatol Arthrosc. 2019;27:117–123. [DOI] [PubMed] [Google Scholar]
- 26. Moksnes H, Engebretsen L, Risberg MA. Prevalence and incidence of new meniscus and cartilage injuries after a nonoperative treatment algorithm for ACL tears in skeletally immature children: a prospective MRI study. Am J Sports Med. 2013;41:1771–1779. [DOI] [PubMed] [Google Scholar]
- 27. MOON Knee Group; Jones MH, Oak SR, Andrish JT, et al. Predictors of radiographic osteoarthritis 2 to 3 years after anterior cruciate ligament reconstruction: data from the MOON on-site nested cohort. Orthop J Sports Med. 2019;7:2325967119867085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Murrell GA, Maddali S, Horovitz L, Oakley SP, Warren RF. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med. 2001;29:9–14. [DOI] [PubMed] [Google Scholar]
- 29. Nakamae A, Adachi N, Deie M, et al. Risk factors for progression of articular cartilage damage after anatomical anterior cruciate ligament reconstruction: a second-look arthroscopic evaluation. Bone Joint J. 2018;100-B:285–293. [DOI] [PubMed] [Google Scholar]
- 30. O’Connor DP, Laughlin MS, Woods GW. Factors related to additional knee injuries after anterior cruciate ligament injury. Arthroscopy. 2005;21:431–438. [DOI] [PubMed] [Google Scholar]
- 31. Osti L, Papalia R, Del Buono A, Amato C, Denaro V, Mafulli N. Good results five years after surgical management of anterior cruciate ligament tears, and meniscal and cartilage injuries. Knee Surg Sports Traumatol Arthrosc. 2010;18:1385–1390. [DOI] [PubMed] [Google Scholar]
- 32. Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29:226–231. [DOI] [PubMed] [Google Scholar]
- 33. Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1438–1444. [DOI] [PubMed] [Google Scholar]
- 34. Pattee GA, Fox JM, Del Pizzo W, Friedman MJ. Four to ten year followup of unreconstructed anterior cruciate ligament tears. Am J Sports Med. 1989;17:430–435. [DOI] [PubMed] [Google Scholar]
- 35. Rai MF, Sandell LJ. Inflammatory mediators: tracing links between obesity and osteoarthritis. Crit Rev Eukaryot Gene Expr. 2011;21:131–142. [DOI] [PubMed] [Google Scholar]
- 36. Ralles S, Agel J, Obermeier M, Tompkins M. Incidence of secondary intra-articular injuries with time to anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:1373–1379. [DOI] [PubMed] [Google Scholar]
- 37. Scavenius M, Bak K, Hansen S, Norring K, Jensen KH, Jorgensen U. Isolated total ruptures of the anterior cruciate ligament: a clinical study with long-term follow-up of 7 years. Scand J Med Sci Sports. 1999;9:114–119. [DOI] [PubMed] [Google Scholar]
- 38. Slauterbeck JR, Kousa P, Clifton BC, et al. Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am. 2009;91:2094–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Steadman JR, Matheny LM, Singleton SB, et al. Meniscus suture repair: minimum 10-year outcomes in patients younger than 40 years compared with patients 40 and older. Am J Sports Med. 2015;43:2222–2227. [DOI] [PubMed] [Google Scholar]
- 40. Tandogan RN, Taşer O, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262–270. [DOI] [PubMed] [Google Scholar]
- 41. Thoma LM, Grindem H, Logerstedt D, et al. Coper classification early after anterior cruciate ligament rupture changes with progressive neuromuscular and strength training and is associated with 2-year success: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2019;47:807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tomihara T, Hashimoto Y, Taniuchi M, et al. Shallow knee flexion angle during femoral tunnel creation using modified transtibial technique can reduce femoral graft bending angle in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:618–625. [DOI] [PubMed] [Google Scholar]
- 43. Tomihara T, Yoshida G, Hara Y, Taniuchi M, Shimada N. Transparent 3-dimensional CT in evaluation of femoral bone tunnel communication after ACL double-bundle reconstruction: comparison between outside-in and transportal technique. Knee Surg Sports Traumatol Arthrosc. 2014;22:1563–1572. [DOI] [PubMed] [Google Scholar]
- 44. Westermann RW, Wright RW, Spindler KP, Huston LJ, Wolf BR. Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med. 2014;42:2184–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wluka AE, Lombard CB, Cicuttini FM. Tackling obesity in knee osteoarthritis. Nat Rev Rheumatol. 2013;9:225–235. [DOI] [PubMed] [Google Scholar]
- 46. Wojtys EM, Ashton-Miller JA, Huston LJ. A gender-related difference in the contribution of the knee musculature to sagittal-plane shear stiffness in subjects with similar knee laxity. J Bone Joint Surg Am. 2002;84:10–16. [DOI] [PubMed] [Google Scholar]
- 47. Yoo JC, Ahn JH, Lee SH, Yoon YC. Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med. 2009;37:1478–1483. [DOI] [PubMed] [Google Scholar]
- 48. Yüksel HY, Erkan S, Uzun M. The evaluation of intraarticular lesions accompanying ACL ruptures in military personnel who elected not to restrict their daily activities: the effect of age and time from injury. Knee Surg Sports Traumatol Arthrosc. 2006;14:1139–1147. [DOI] [PubMed] [Google Scholar]
- 49. Zoller SD, Toy KA, Wang P, Ebramzadeh E, Bowen RE. Temporal relation of meniscal tear incidence, severity, and outcome scores in adolescents undergoing anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]



