Abstract
Background:
Patellar instability (PI) is a common problem among pediatric, adolescent, and young adult patients. Recent literature has shown a correlation between pathoanatomy and PI.
Purpose/Hypothesis:
The purpose of this study was to determine if there is any difference in patellar shape in patients with and without PI and if there is any association between the shape of the patella and the shape of the trochlea. Our hypothesis was that there would be no association between the shape of the patella and the likelinhood of having PI and that the shape of the trochlea would not be associated with patellar morphology.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Magnetic resonance imaging (MRI) scans were analyzed for 97 study patients with PI and 100 control patients with anterior cruciate ligament tears. Radiologic measurements of trochlear morphology were collected via MRI; 15 measurements of patellar morphology were then measured using axial MRI scans. Comparisons between the control and PI groups were performed using a 2-tailed t test. Regression analysis was performed to determine if associations existed between the 15 patellar morphology measurements and the trochlear dysplasia measurements.
Results:
There were no statistically significant differences between the PI and control groups for the majority of patellar morphology measurements. With regression analysis, there were no statistically significant associations between the majority of patellar morphology measurements and the trochlear dysplasia measurements.
Conclusion:
Patellar morphology is highly variable in knees with and without PI. There was a minimal association between measurements of patellar morphology and trochlear dysplasia.
Keywords: patellar instability, trochlear dysplasia, knee, patellar morphology
Patellar instability (PI) is a common problem among pediatric and adolescent patients. Commonly cited anatomic risk factors for PI include trochlear dysplasia, patella alta, genu valgum, femoral anteversion, and ligamentous laxity.†† While these risk factors have received appropriate attention, there has been sporadic research evaluating the shape of the patella and its role in PI.2,8,15,16,20 These studies have generally been small patient series examining variables such as medial and lateral facet angles, facet length, and overall patellar width on magnetic resonance imaging (MRI) scans. In general, these studies have shown either no consistent findings or that any morphologic changes in patients with PI were centered about the medial facet, which plays much less of a role in lateral PI.2,8,15 The largest study to date included 140 knees in 105 patients with PI and found a significant association between a convex medial patellar facet and a Dejour type C trochlea as well as increased patellar tilt. However, this study evaluated patellar shape based on axial radiographs, as opposed to MRI or computed tomography scans, and there was no control group.16 Thus, it is difficult to determine the validity or significance of these findings.
Ideally, any study examining patellar morphology in the setting of PI should help determine treatment algorithms and options. An example is whether altered or abnormal patellar shape would contraindicate a groove-deepening trochleoplasty, a question that arises among orthopaedic surgeons who manage patellofemoral pathology. Therefore, evaluation of the medial and lateral facets of the patella at multiple points is of importance to determine if any clinically relevant morphologic differences exist in patients with and without PI and, specifically, patients with and without trochlear dysplasia.
As such, the purpose of this study was to determine if there is any difference in patellar shape in patients with and without PI. Furthermore, we sought to determine if there is any association between the shape of the patella and the shape of the trochlea. Our hypothesis was that there would be no association between the shape of the patella and the likelihood for PI in patients and that the shape of the trochlea would not be associated with the shape of the patella.
Methods
After receiving institutional review board approval, we queried an institutional database for patients with PI between January 2014 and December 2018. All patients with PI who satisfied all clinically relevant inclusion criteria were identified. Patients were excluded from the study if there was insufficient imaging for evaluation or if the correct diagnosis could not be determined using clinical notes. Furthermore, patients were excluded if they had neuromuscular conditions or noted degenerative changes of joint space narrowing or osteophyte formation on imaging. From these patients, all who had available demographic and radiologic data via MRI were identified. Demographic data collected included age at first PI event, sex, body mass index (BMI), and laterality. Radiologic data collected via MRI were lateral trochlear inclination (LTI) angle,12 sulcus angle,1 lateral patellar inclination (LPI),11 proximal tibial tubercle–trochlear groove (pTT-TG) distance,4 and distal tibial tubercle–trochlear groove (dTT-TG) distance.4 A matched cohort of patients with anterior cruciate ligament tear and no history of PI was identified as a control group, and the same data were collected. After application of inclusion and exclusion criteria, 100 control patients and 97 patients with PI were identified.
Patellar Imaging Measurements
The following measurements were taken from axial MRI scans (≥1.5 T).
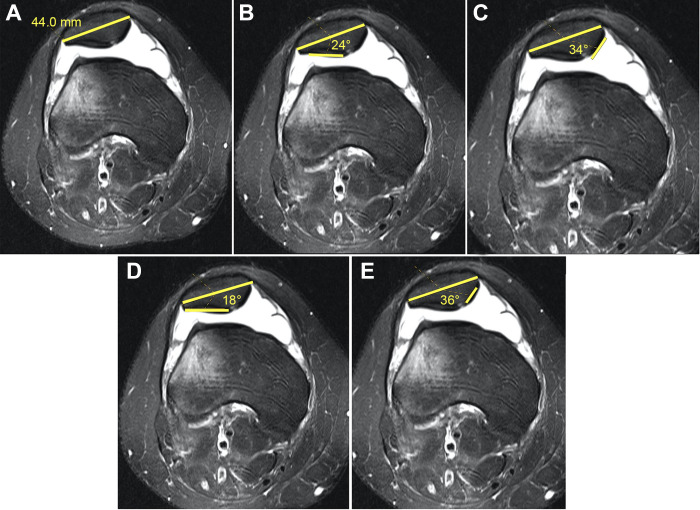
Width of patella: This is measured from the most medial and lateral aspects of the patella as described by Stäubli et al20 (Figure 1A).
Lateral facet angle of cartilage (L-FAC): This is the angle subtended between the axis of the most medial and lateral aspects of the patella and the chondral surface of the lateral facet (Figure 1B).
Medial facet angle of cartilage (M-FAC): This is the angle subtended between the axis of the most medial and lateral aspects of the patella and the chondral surface of the medial facet. In cases where there appeared to be a rather vertical odd facet, the medial facet angle was taken from the median ridge to the junction of the medial facet and odd facet (Figure 1C).
Lateral facet angle of bone (L-FAB): This is the angle subtended between the axis of the most medial and lateral aspects of the patella and the subchondral bone of the lateral facet (Figure 1D).
Medial facet angle of bone (M-FAB): This is the angle subtended between the axis of the most medial and lateral aspects of the patella and the subchondral bone of the medial facet. Similar to the M-FAC, in cases where there appeared to be a rather vertical odd facet, the medial facet angle was taken from the median ridge to the junction of the medial facet and odd facet (Figure 1E).
Figure 1.
Measurements made on axial T2-weighted magnetic resonance imaging sequence: (A) patellar width at its greatest diameter, (B) lateral facet angle of cartilage, (C) medial facet angle of cartilage, (D) lateral facet angle of bone, and (E) medial facet angle of bone.
These 5 measurements were taken at 3 points along the patella: (1) the most proximal aspect of the patella where both facets were visible and had visible chondral surfaces, (2) the point where the patella was widest, and (3) the most distal point where both facets were visible and had visible chondral surfaces. Thus, 15 measurements were taken for each patella. All patellar measurements were performed by 2 orthopaedic sports medicine fellows (A.E.J., B.J.L.) and 1 sports medicine fellowship–trained surgeon (J.L.P.). A random sample of 30 patients in the PI group and 30 in the control group were chosen for intra- and interrater reliability. Patellar morphology measurements were performed at least 2 weeks apart. The MRI scan readings were performed using the same protocol for the original readings (the readers were free to select their own MRI slices). Reliability of measurements was determined using intraclass correlation coefficients (ICCs). All other measurements (LTI, LPI, sulcus angle, pTT-TG, dTT-TG) had been collected on all patients as part of the institutional database.
Statistical Analysis
The Shapiro-Wilk test was used to test for normality of data of all continuous variables. Means and SDs were determined for all continuous variables with normal distributions. A 2-tailed heteroscedastic t test was performed to compare the control group with the PI group, with P values <.05 indicating significance. Intra- and interrater variability were assessed using ICCs. Two-way analysis of variance with Tukey post hoc analysis was performed to determine differences among variables at different measurement levels (ie, proximal, middle, and distal). The data were modeled using generalized multiple regression analysis with backward elimination to determine associations between measures of patellar morphology and measures of trochlear dysplasia. Inter- and intrarater ICC values were calculated for all study measurements. ICC values were graded as excellent (>0.9), good (>0.8-0.9), fair (>0.7-0.8), moderate (>0.5-0.7), and poor (≤0.5).
Results
A total of 97 patients with PI (mean ± SD; age, 14.5 ± 1.8 years; BMI, 25.5 ± 6.4; 53 male and 44 female) and 100 controls (age, 14.5 ± 1.9 years; BMI, 23.7 ± 5.7; 55 male and 45 female) were evaluated. Demographic data and trochlear measurements of the 2 groups are shown in Table 1. There was a significant difference in BMI between the groups (P = .04) as well as significant differences for all trochlear measurements (P < .001 for all).
Table 1.
Demographic Data and Trochlear Measurements of the PI and Control Groupsa
| Group, Mean ± SD or No. | |||
|---|---|---|---|
| Control (n = 100) | PI (n = 97) | P Value | |
| Age, y | 14.5 ± 1.9 | 14.5 ± 1.8 | .88 |
| Body mass index | 23.7 ± 5.7 | 25.5 ± 6.4 | .04 |
| Sex | |||
| Male | 55 | 53 | .96 |
| Female | 45 | 44 | .96 |
| Trochlear measurements | |||
| LTI, deg | 18.9 ± 5.8 | 5.8 ± 10.4 | <.001 |
| LPI, deg | 8.7 ± 6.3 | 20.9 ± 9.1 | <.001 |
| Sulcus angle, deg | 140.5 ± 6.4 | 158.4 ± 9.3 | <.001 |
| pTT-TG, mm | 9.2 ± 4.2 | 14.9 ± 4.3 | <.001 |
| dTT-TG, mm | 9.0 ± 3.7 | 15.4 ± 4.3 | <.001 |
aBold P values indicate statistically significant difference between groups (P < .05). dTT-TG, distal tibial tubercle–trochlear groove; LPI, lateral patellar inclination; LTI, lateral trochlear inclination; PI, patellar instability; pTT-TG, proximal tibial tubercle–trochlear groove.
ICC of Patellar Morphology Measurements
Intrarater ICC values ranged from poor to excellent. Notably, intrarater ICCs generally improved as measurements moved distally. Proximal measurements had the most poor intrarater ICCs (6 of 10), followed by middle measurements (2 of 10) and distal measurements (0 of 10). Of the 8 poor intrarater ICCs, 6 were calculated for measurements on the medial side of the patella.
Interrater ICC values ranged from moderate to excellent (>0.5). Patellar width (middle) and M-FAB (distal) had excellent ICC values (0.904 and 0.912, respectively). Patellar width (proximal), M-FAB (proximal), and M-FAC (proximal, middle, and distal) had good ICC values. Patellar width (distal), L-FAB (proximal), L-FAC (proximal), and M-FAB (middle) had fair ICC values. L-FAB (middle and distal) and L-FAC (middle and distal) had moderate ICC values. There were no measurements with poor ICC values. ICC values for all measurements are presented in Table 2.
Table 2.
ICC Values for Patellar Morphology Measurementsa
| Intrarater ICC | |||
|---|---|---|---|
| Variable | Rater 1 | Rater 2 | Interrater ICC |
| Proximal level | |||
| Width | 0.476 | 0.831 | 0.876 |
| M-FAB | 0.397 | 0.036 | 0.805 |
| L-FAB | 0.542 | 0.645 | 0.754 |
| M-FAC | 0.373 | 0.203 | 0.895 |
| L-FAC | 0.496 | 0.701 | 0.771 |
| Middle level | |||
| Width | 0.961 | 0.959 | 0.904 |
| M-FAB | 0.601 | 0.409 | 0.704 |
| L-FAB | 0.585 | 0.800 | 0.639 |
| M-FAC | 0.730 | 0.405 | 0.802 |
| L-FAC | 0.531 | 0.716 | 0.569 |
| Distal level | |||
| Width | 0.891 | 0.916 | 0.800 |
| M-FAB | 0.629 | 0.617 | 0.912 |
| L-FAB | 0.715 | 0.883 | 0.573 |
| M-FAC | 0.699 | 0.700 | 0.872 |
| L-FAC | 0.709 | 0.900 | 0.668 |
aICC, intraclass correlation coefficient; L-FAB, lateral facet angle of bone; L-FAC, lateral facet angle of cartilage; M-FAB, medial facet angle of bone; M-FAC, medial facet angle of cartilage.
Group Comparisons
There were no statistically significant differences between the groups with measurements of patellar width, L-FAB, or L-FAC at any level (proximal, middle, distal). There was no statistically significant difference between M-FAC at the proximal and middle levels, but the PI group had significantly smaller angles than did the control group at the distal level (PI, 17.1° ± 9.7°; control, 20.0° ± 8.4°; P = .027). The M-FAB was statistically significantly smaller in the PI group than the control group at the proximal level (PI, 11.8° ± 3.8°; control, 14.2° ± 6.3°; P = .002), middle level (PI, 11.1° ± 4.3°; control 12.5° ± 4.8°; P = .035), and the distal level (PI, 8.6° ± 3.9°; control, 10.9° ± 4.7°; P < .001). Group comparison means and SDs for all study measurements are presented in Table 3.
Table 3.
Group Comparisons Between PI and Control Groupsa
| Group, Mean ± SD | |||
|---|---|---|---|
| Variable | Control | PI | P Value |
| Proximal level | |||
| Width, mm | 39.7 ± 4.2 | 38.8 ± 4.1 | .175 |
| M-FAB, deg | 14.2 ± 6.3 | 11.8 ± 3.8 | .002 |
| L-FAB, deg | 26.1 ± 4.2 | 26.4 ± 4.3 | .735 |
| M-FAC, deg | 21.4 ± 7.2 | 20.2 ± 8.4 | .262 |
| L-FAC, deg | 19.3 ± 8.4 | 18.2 ± 8.2 | .391 |
| Middle level | |||
| Width, mm | 42.8 ± 3.9 | 42.0 ± 4.1 | .186 |
| M-FAB, deg | 12.5 ± 4.8 | 11.1 ± 4.3 | .035 |
| L-FAB, deg | 27.4 ± 4.7 | 26.8 ± 4.2 | .346 |
| M-FAC, deg | 20.3 ± 8.2 | 18.8 ± 8.5 | .189 |
| L-FAC, deg | 19.6 ± 9.2 | 18.4 ± 9.2 | .357 |
| Distal level | |||
| Width, mm | 40.3 ± 4.3 | 39.2 ± 3.7 | .074 |
| M-FAB, deg | 10.9 ± 4.7 | 8.6 ± 3.9 | <.001 |
| L-FAB, deg | 26.0 ± 5.9 | 25.9 ± 4.9 | .946 |
| M-FAC, deg | 20.0 ± 8.4 | 17.1 ± 9.7 | .027 |
| L-FAC, deg | 17.1 ± 9.7 | 17.2 ± 9.6 | .364 |
aBold P values indicate statistically significant difference between groups (P < .05). L-FAB, lateral facet angle of bone; L-FAC, lateral facet angle of cartilage; M-FAB, medial facet angle of bone; M-FAC, medial facet angle of cartilage; PI, patellar instability.
Level Comparisons
In the control group, patellar width was significantly larger at the middle level than the proximal level (middle, 42.8 ± 3.9 mm; proximal, 39.7 ± 4.2 mm; P < .001). The M-FAB was significantly smaller at the distal level as compared with the proximal level (distal, 10.9° ± 4.7°; proximal, 14.2° ± 6.3°; P < .001). The L-FAB was significantly larger at the middle level versus the distal level (middle, 27.4° ± 4.7°; distal, 26.0° ± 5.9°; P = .009). There were no statistically significant differences in M-FAC or L-FAC at any level. Control group–level comparisons can be found in Table 4.
Table 4.
Level Comparisons of the Control and PI Groupsa
| Level, Mean ± SD | ||||
|---|---|---|---|---|
| Variable | Proximal | Middle | Distal | P Value |
| Control group | ||||
| Width, mm | 39.7 ± 4.2 | 42.8 ± 3.9b | 40.3 ± 4.3 | <.001 |
| M-FAB, deg | 14.2 ± 6.3 | 12.5 ± 4.8 | 10.9 ± 4.7b | <.001 |
| L-FAB, deg | 26.1 ± 4.2 | 27.4 ± 4.7c | 26.0 ± 5.9 | .009 |
| M-FAC, deg | 21.4 ± 7.2 | 20.3 ± 8.2 | 20.0 ± 8.4 | .447 |
| L-FAC, deg | 19.3 ± 8.4 | 19.6 ± 9.2 | 17.1 ± 9.7 | .649 |
| PI group | ||||
| Width, mm | 38.8 ± 4.1 | 42.0 ± 4.1b,c | 39.2 ± 3.7 | <.001 |
| M-FAB, deg | 11.8 ± 3.8 | 11.1 ± 4.3c | 8.6 ± 3.9b | <.001 |
| L-FAB, deg | 26.4 ± 4.3 | 26.8 ± 4.2 | 25.9 ± 4.9 | .451 |
| M-FAC, deg | 20.2 ± 8.4 | 18.8 ± 8.5 | 17.1 ± 9.7 | .056 |
| L-FAC, deg | 18.2 ± 8.2 | 18.4 ± 9.2 | 17.2 ± 9.6 | .594 |
aBold P values indicate statistically significant difference (P < .05). L-FAB, lateral facet angle of bone; L-FAC, lateral facet angle of cartilage; M-FAB, medial facet angle of bone; M-FAC, medial facet angle of cartilage; PI, patellar instability.
bSignificant difference from proximal.
cSignificant difference from distal.
In the PI group, patellar width was significantly larger at the middle level as compared with the proximal and distal levels (proximal, 38.8 ± 4.1 mm; middle, 42.0 ± 4.1 mm; distal, 39.2 ± 3.7 mm; P < .001). The M-FAB was significantly larger at the proximal and middle levels than at the distal level (proximal, 11.8° ± 3.8°; middle, 11.1° ± 4.3°; distal, 8.6° ± 3.9°; P < .001). There were no statistically significant differences in L-FAB, M-FAC, or L-FAC at any level. PI group–level comparisons can be found in Table 4.
Regression Analysis
There was a statistically significant association between M-FAB (proximal, middle, and distal) and measures of increasing severity of trochlear dysplasia (LTI, LPI, dTT-TG, pTT-TG, sulcus angle); however, these differences were small. There was no association between M-FAC and trochlear measurements. There was an association between decreasing sulcus angle (flatter trochlea) and L-FAC (proximal), L-FAB (middle and distal), and M-FAC (distal). There was no significant association between the majority of patellar morphology measurements and the trochlear dysplasia measurements. Complete data for regression analysis are presented in Table 5.
Table 5.
Regression Analysis Between Patellar Morphology Measurements and Trochlear Dysplasia Measurementsa
| Level, P Value (β) | |||
|---|---|---|---|
| Variable | Proximal | Middle | Distal |
| Width | |||
| LTI | .284 | .986 | .722 |
| LPI | .108 | .346 | .412 |
| dTT-TG | .959 | .930 | .679 |
| pTT-TG | .957 | .888 | .638 |
| Sulcus | .758 | .587 | .484 |
| M-FAB | |||
| LTI | <.001 (0.527) | .008 (0.441) | <.001 (0.599) |
| LPI | <.001 (–0.582) | <.001 (–0.638) | <.001 (–0.548) |
| dTT-TG | .002 (–0.216) | .002 (–0.246) | .020 (–0.191) |
| pTT-TG | .020 (–0.163) | .013 (–0.200) | .018 (–0.194) |
| Sulcus | .001 (–0.524) | .033 (–0.400) | .002 (–0.597) |
| L-FAB | |||
| LTI | .107 | .268 | .074 |
| LPI | .095 | .067 | .114 |
| dTT-TG | .284 | .538 | .604 |
| pTT-TG | .704 | .602 | .485 |
| Sulcus | .389 | .008 (–0.513) | .046 (–0.317) |
| M-FAC | |||
| LTI | .259 | .067 | .013 (0.209) |
| LPI | .100 | .197 | .284 |
| dTT-TG | .711 | .185 | .283 |
| pTT-TG | .234 | .071 | .104 |
| Sulcus | .238 | .134 | .010 (–0.242) |
| L-FAC | |||
| LTI | .350 | .362 | .175 |
| LPI | .638 | .644 | .630 |
| dTT-TG | .258 | .210 | .691 |
| pTT-TG | .991 | .705 | .428 |
| Sulcus | .043 (–0.210) | .071 | .126 |
adTT-TG, distal tibial tubercle–trochlear groove; L-FAB, lateral facet angle of bone; L-FAC, lateral facet angle of cartilage; LPI, lateral patellar inclination; LTI, lateral trochlear inclination; M-FAB, medial facet angle of bone; M-FAC, medial facet angle of cartilage; pTT-TG, proximal tibial tubercle–trochlear groove.
Discussion
The main finding from this study is that patellar morphology in a young nonarthritic knee is variable in patients with and without PI. There was almost no association between measurements of trochlear dysplasia and patellar morphology. There was a statistically significant association between the M-FAB and measurements of trochlear dysplasia; however, this association was not seen between measurements of trochlear dysplasia and M-FAC. Furthermore, the association between the M-FAB and measurements of trochlear dysplasia was weak. Our findings were consistent with those reported in previous literature that has shown that any nonarthritic changes in patellar morphology in the setting of PI occur on the medial facet.2,8,16 While there was statistical significance achieved in some of the associations between medial patellar facet morphology and trochlear dysplasia, the absolute differences between the control and study groups were very small. Thus, this could represent a lowering of the SEM owing to the large sample sizes as opposed to anything that represents clinical significance.
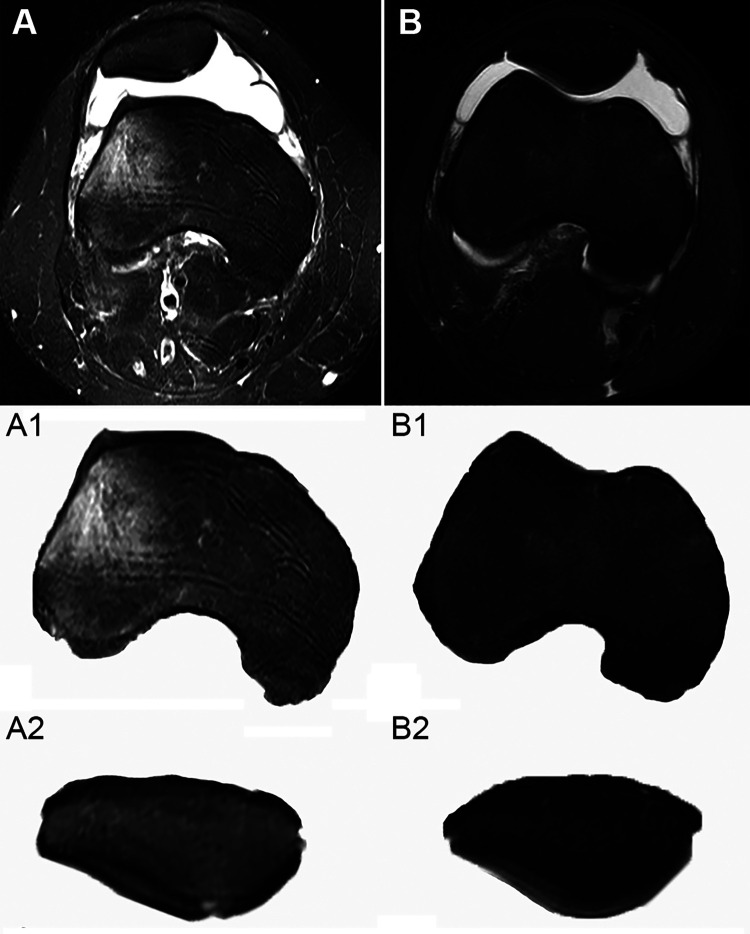
Of particular importance, there was no association between the lateral patellar facet angles and trochlear morphology. This lack of association calls into question the role that patellar morphology plays in instability. It is possible that the shape of the patella changes as the patellofemoral joint becomes arthritic, but primary patellar dysplasia appears to be a rare entity and not a regular phenomenon in the setting of trochlear dysplasia. The congruency between the lateral facet of the patella and the lateral trochlea is of central importance to patellar stability. Our study and previous studies have not established a difference for any measure of the lateral patellar facet between patients with instability and a control group. 2,8,16 Interestingly, in our study, the cartilaginous lateral patellar facet angles had mean values of 18.2° ± 8.2° (proximal), 18.4° ± 9.2° (middle), and 17.2° ± 9.6° (distal) in the PI group. This was congruent with the mean LTI angle present in the control group (18.9° ± 5.8°) but quite incongruous with the LTI angle in the PI group (5.8° ± 10.4°). These findings are contrary to the argument that a dysplastic trochlea causes a reactive “dysplastic congruency” of the patella (Figure 2). Thus, in the case of recurrent PI attributed to high-grade trochlear dysplasia, a trochleoplasty should not be routinely contraindicated for patellar morphology. We acknowledge and have seen highly dysplastic patellae that are concave, but these are rare, as evidenced in this study.
Figure 2.
Qualitative difference in patellotrochlear congruency between (A) dysplastic and (B) normal trochlea. Significant trochlear dysplasia seen in A1 as compared with B1. However, the corresponding patella of the dysplastic trochlea (A2) shows similar morphology to the patella of the normal trochlea (B2).
Our results are in line with those reported in recent literature on the topic. Otto et al15 performed a similar study evaluating the MRI scans of 50 patients with PI and 50 controls with anterior cruciate ligament tear. They found that patients with patellofemoral instability did not have a significantly smaller lateral patellar facet or relative patellar width as compared with the control group. Our study helps to build on this, and our measurements of proximal, middle, and distal patellar widths were not different between the case and control groups. Fucentese et al8 performed a similar comparative MRI study investigating patellar morphology and trochlear dysplasia. They compared a group of 22 patients with underlying trochlear dysplasia with 22 matched controls. The authors found only a few significant differences between the groups and that all differences were isolated to changes of the medial facet, which has a questionable role in the setting of PI.
Barnett et al2 published a similar article comparing the morphology of the patella in normal and dysplastic knees by retrospectively analyzing MRI scans of 25 patients with patellofemoral dysplasia and 10 controls to assess whether there was any change in the morphology of the patella along its vertical length. The authors showed that in the dysplastic patellofemoral articulation, the medial facet of the patella became smaller in relation to the lateral facet from proximal to distal. Stäubli et al20 studied cryosections from a cadaver knee and MRI scans of 30 nondysplastic knees. They found a difference in all knees between the geometry of the surface of the cartilage and the corresponding subchondral osseous anatomy of the femoral trochlea and patella. This supports the notion that the patella’s morphology is highly variable and not associated with PI. Previous studies2,8,16 have demonstrated morphologic differences in patellar morphology in patients with instability, but these have all been related to the medial facet, which likely has low clinical significance.
We recognize several study limitations. An a priori power analysis was not performed to determine if our study had an adequate sample size to test our hypothesis. Given the retrospective nature of the study, there is a possibility of selection bias, and the cohort included may not be representative of the general population of other practices, as our patients were almost exclusively adolescents. The patients selected were representative of our population of interest, and adolescents represent the bulk of patients with PI.7,9,18,19 Thus, despite the narrow age range, it is a clinically relevant representation of the typical patient with PI. In terms of imaging evaluation, observers could not be blinded to whether images were obtained in controls or patients with PI. In addition, our assessment of cartilage angles, particularly the medial facet, was difficult to determine in several cases. This was reflected in our poor intraobserver reliability in measuring the medial facet in the proximal aspect of the patella. Of note, poor intraobserver reliability was limited to the proximal and middle patella, with all measurements of the distal patella demonstrating moderate or better reliability.
In terms of the lateral facet, we demonstrated poor reliability at worst and excellent reliability at best using angular measurements. Given that the articulation between the lateral facet and the lateral trochlea is the key to stability, we are still able to derive clinically meaningful results from this study. Furthermore, this study provides the largest case and control groups on the topic in the literature, and rather than using the qualitative Dejour classification to evaluate trochlear dysplasia, we used the much more quantifiable and reliable 2-image LTI12 in conjunction with other quantifiable measures of trochlear dysplasia, both direct (sulcus angle) and indirect (LPI, pTT-TG, and dTT-TG). This allowed for robust statistical analysis of continuous variables to determine any significant associations. Further research on this topic is warranted to establish a more reliable measurement system of patellar morphology, particularly the medial facet, and to refine its role in instability.
Conclusion
Patellar morphology is highly variable in knees with and without PI. There was minimal association between measurements of patellar morphology and trochlear dysplasia. The role of patellar morphology in PI appears to be minimal, with primary patellar dysplasia being a rare phenomenon. Furthermore, a trochleoplasty for PI should rarely be contraindicated for patellar shape.
Footnotes
Final revision submitted September 3, 2020; accepted October 16, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.L.P. has received education payments from Arthrex; consulting fees from Arthrex, Ceterix, and Smith & Nephew; and nonconsulting fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Connecticut Children’s Medical Center (No. 18-015).
References
- 1. Arendt EA, Askenberger M, Agel J, Tompkins MA. Risk of redislocation after primary patellar dislocation: a clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med. 2018;46:3385–3390. [DOI] [PubMed] [Google Scholar]
- 2. Barnett AJ, Gardner RO, Lankester BJ, Wakeley CJ, Eldridge JD. Magnetic resonance imaging of the patella: a comparison of the morphology of the patella in normal and dysplastic knees. J Bone Joint Surg Br. 2007;89:761–765. [DOI] [PubMed] [Google Scholar]
- 3. Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–712. [DOI] [PubMed] [Google Scholar]
- 4. Brady JM, Sullivan JP, Nguyen J, et al. The tibial tubercle–to–trochlear groove distance is reliable in the setting of trochlear dysplasia, and superior to the tibial tubercle–to–posterior cruciate ligament distance when evaluating coronal malalignment in patellofemoral instability. Arthroscopy. 2017;33:2026–2034. [DOI] [PubMed] [Google Scholar]
- 5. Caton J. Method of measuring the height of the patella. Article in French. Acta Orthop Belg. 1989;55:385–386. [PubMed] [Google Scholar]
- 6. Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. 2017;45:2105–2110. [DOI] [PubMed] [Google Scholar]
- 7. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. [DOI] [PubMed] [Google Scholar]
- 8. Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schöttle PB. The patella morphology in trochlear dysplasia—a comparative MRI study. Knee. 2006;13:145–150. [DOI] [PubMed] [Google Scholar]
- 9. Hiemstra LA, Kerslake S, Lafave M. Assessment of demographic and pathoanatomic risk factors in recurrent patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2017;25:3849–3855. [DOI] [PubMed] [Google Scholar]
- 10. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop. 2017;37:484–490. [DOI] [PubMed] [Google Scholar]
- 11. Joseph S, Cheng C, Solomito M, Pace J. Lateral patellar inclination in children and adolescents: modified measurement technique to characterize patellar instability. Orthop J Sports Med. 2019;7(3)(suppl):2325967119S00091. [Google Scholar]
- 12. Joseph S, Cheng C, Solomito M, Pace J. Lateral trochlear inclination in children and adolescents: modified measurement technique to characterize patellar instability. Orthop J Sports Med. 2019;7(3)(suppl):2325967119S00146. [Google Scholar]
- 13. Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg. 2015;28:303–309. [DOI] [PubMed] [Google Scholar]
- 14. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41:575–581. [DOI] [PubMed] [Google Scholar]
- 15. Otto A, Tscholl PM, Pääsuke R, et al. Neither lateral patellar facet nor patellar size are altered in patellofemoral unstable patients: a comparative magnetic resonance imaging analysis. Knee Surg Sports Traumatol Arthrosc. 2020;28:1064–1071. [DOI] [PubMed] [Google Scholar]
- 16. Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19:663–670. [DOI] [PubMed] [Google Scholar]
- 17. Prakash J, Seon JK, Woo SH, Jin C, Song EK. Comparison of radiological parameters between normal and patellar dislocation groups in Korean population: a rotational profile CT-based study. Knee Surg Relat Res. 2016;28:302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1037–1043. [DOI] [PubMed] [Google Scholar]
- 19. Sanders TL, Pareek A, Johnson NR, Stuart MJ, Dahm DL, Krych AJ. Patellofemoral arthritis after lateral patellar dislocation: a matched population-based analysis. Am J Sports Med. 2017;45:1012–1017. [DOI] [PubMed] [Google Scholar]
- 20. Stäubli HU, Dürrenmatt U, Porcellini B, Rauschning W. Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg Br. 1999;81:452–458. [DOI] [PubMed] [Google Scholar]
- 21. Van Haver A, De Roo K, De Beule M, et al. The effect of trochlear dysplasia on patellofemoral biomechanics: a cadaveric study with simulated trochlear deformities. Am J Sports Med. 2015;43:1354–1361. [DOI] [PubMed] [Google Scholar]