Abstract
Thermal burns of the oral cavity usually arise from ingestion of hot foods or beverages. A 38-year-old female patient presented with two painful ulcerative erythematous patches of the palate. The patient was consulted on the same day lesions appeared. Medical history was unremarkable. Clinically significant self-inflicted injuries may result in wide ulcers in the mouth and usually do not take less than 2 weeks to heal, whereas our patient, treated with low-level laser therapy, had a complete response in day 4, after 2 days of treatment. The fact that multiple lesions were present signaled against the World Health Organization exclusion diagnosis of erythroplakia for red patches. A traumatic ulcer, regardless of its cause of origin, usually heals within 2 weeks, after the source of injury is resolved. A thermal burn in the oral cavity usually takes longer than that to heal, but whenever this time frame is not respected, the suspicion of a potentially malignant disorder should always arise, and a biopsy should be performed. The present case showed two painful thermal burns with great results in terms of speeding up the relieve of symptoms and healing time with soft laser as opposed to the traditional treatment with oral topical corticosteroid.
Keywords: Dentistry, thermal burns, palate, laser treatment, erythroplakia, oral mucosa
Introduction
Thermal burns of the oral cavity usually arise from ingestion of hot foods or beverages. In addition, microwave ovens have been associated with an increased frequency of thermal burns due to their ability to cook food that seems to be cool or at least edible on the exterior although extremely hot in the interior.1 The misuse of microwave ovens can be particularly hazardous to vulnerable individuals, such as infants, who can suffer palatal burns from microwave-heated infant’s milk;2 and the elderly, occasionally causing significant thermal injuries that may result in emergency scenarios such as laryngeal damage.3 Systemic diseases such as diabetes can be related to oral mucosal dysesthesia, which may predispose the occurrence of thermal burns in the mouth, causing significant more damage than what the patient actually feels.4 Microwave-heated food ingestion in two cases, one adult male and an elderly female, highlight the level of discomfort and morbidity that such condition may cause, with 6 weeks and 9 months of recovery time, respectively. The latter only being able to eat semi-solid food after 6 weeks post-injury.5 Sommer and collaborators recently pointed out that many of the current models used to interpret the photon–cell interaction in low-level laser therapy (LLLT) mechanism of action are flawed. They have presented heavy criticism on the cytochrome c oxidase (COX) model and confirmed the hypothesis of the read to near infrared (R-NIR) photons model.6 Regardless of the mitochondrial conundrum, LLLT biological robustness affects cell proliferation, connective tissue transforming growth factor beta/small mothers against decapentaplegic (TGF-β/Smad) pathway, angiogenesis and cytokines, apoptosis and even micro ribonucleic acid (micro-RNA) modification with the stimulation of mesenchymal stem cells.7 These mechanisms of action provide a positive influence in several clinical outcomes, including lesions that require a faster wound healing such as thermal burns, for a better quality of life of the patient and to avoid secondary infections.
Case report
A 38-year-old female patient presented with two painful ulcerative erythematous patches of the palate. The patient was consulted on the same day lesions appeared. Medical history was unremarkable. Laboratory exams revealed no thrombocytopenia, anemia, or any white blood cells deviation. Another differential diagnosis that was ruled out was erythroplakia, for which a biopsy should be undertaken in case any lesion does not heal in 2 weeks. The fact that multiple lesions were present signaled against the exclusion of premalignant lesion for a red patch that does not have a defined clinical diagnosis, as prescribed by the World Health Organization (WHO). The provisional diagnosis was of thermal burns from microwave-heated food consumption. Given the lack of success reported by the patient in previous thermal burns with conventional topical corticosteroid treatment, the prominent LLLT was suggested as a therapeutic approach for the palatal burns. Both lesions were dried before laser therapy with a gauze when bleeding was noted. Nevertheless, there was no prior spontaneous bleeding. Patient was laser-zapped on day 1 (Figure 1) with a GaAlAs diode laser (Laser (DUO®—MMOptics Ltda, São Carlos, Brazil), with 100 mW, 3.2 J, 106 J/cm2, a spot size of 0.03 cm2, emitting a continuous light at 808 nm, for 32 s (standard dose), twice for the larger lesion (one anterior and one posterior zap) and once for the midline palate lesion centrally. On day 2 (Figure 2), the larger and midline palate lesions were laser-zapped with standard doses. Finally, the treatment was finished on the third day with standard doses for lateral palate lesion with a single application again (Figure 3). All sessions had 24 h intervals between each laser therapy. Using a visual analog pain scale graded from 0 to 10, patient reported an improvement from 10 to 5, from day 1 to day 2. Patient reported only minor discomfort on day 3 (grade 2 on the pain scale) and no more symptoms from day 4 onward (grade 0). Patient returned on day 6 for a clinical exam, in which there was no remnant lesion observed (Figure 4).
Figure 1.
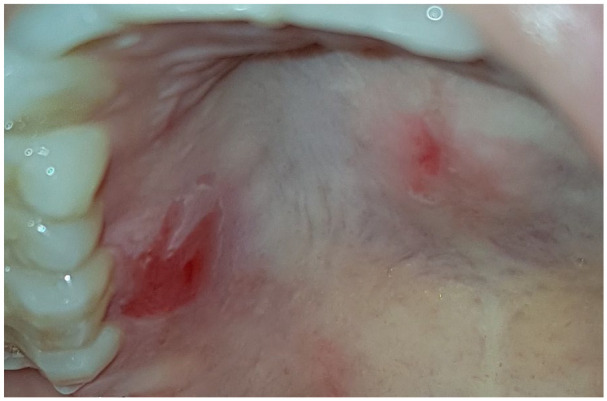
Day 1, laser zapped with standard dose twice for the larger lesion and once for the midline palate lesion centrally.
Figure 2.
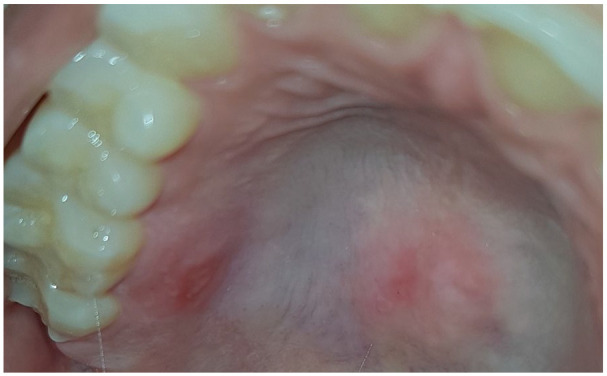
Day 2, larger lesion, and midline palate lesion were laser zapped with standard dose once.
Figure 3.
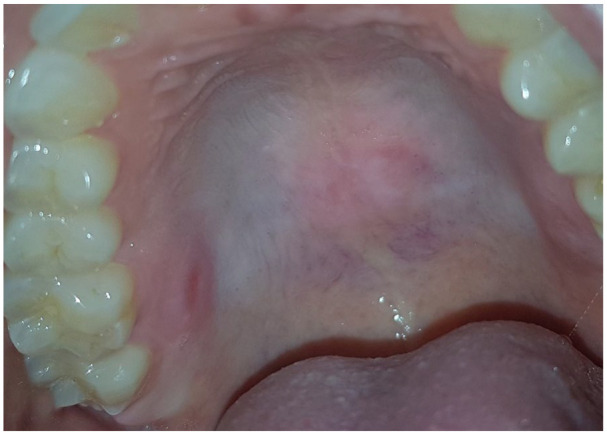
Day 3, almost resolved, laser zapped with standard dose once for larger lesion only.
Figure 4.
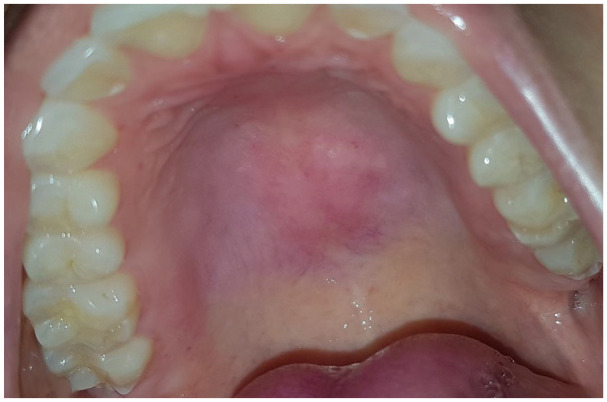
Day 6, posttreatment control with complete healing.
Discussion
Clinically significant self-inflicted injuries may result in wide ulcers in the mouth and usually do not take less than 2 weeks to heal,8 whereas our patient, treated with LLLT, had a complete recovery after 3 days of treatment. To the best of our knowledge, this is the first report involving wide traumatic ulcer laser treatment in the mouth. Ahad and collaborators presented a palatal self-inflicted burn treatment due to a matchstick. Infrared soft laser (810 nm) with 1 W in continuous mode was applied 5 times with 48 h interval between sessions. Complete healing occurred only on the 12th day.9 The longer interval between applications could explain the inferior result as compared with our case. A microwave-heated pizza burn was reported to heal within a week with the application of triamcinolone in Orabase and a bland diet.10 This report shows that use of topical corticosteroid seems not only to heal the burn slower but also relies on the adherence of the patient to treatment, since laser zapping is a more controlled therapy modality, performed by the clinician. Similar lesions may also take a long time to heal, which is the case for the differential diagnosis of thermal burns. The impact of LLLT to prevent oral mucositis in head and neck cancer patients treated with chemotherapy is remarkable, revealing survival improvement of cancer patients compared with placebo.11 A reactive ulceration in self-inflicted lesions called Riga-Fede Disease (RFD) is rare and usually present in newborn or children related to teething, but also observed in teenagers, adults, or removable prosthetic appliances users. Anesthetic based gel is an alternative to treat RFD, as reported for an 11-month-old girl,12 although LLLT might be a potential therapeutic agent for such pathology, with fewer risks of side effects, especially in pediatric patients. When exophytic traumatic lesions are observed, the association of low- and high-power laser devices may prove to be a good treatment of choice.13 If special-needs patients present with self-inflicted lesions of the mouth, in addition to laser therapy and oral appliances to separate oral tissues from trauma origin, botulinum toxin to neuromuscular block may be considered to prevent self-injurious behavior.14
Conclusion
A traumatic ulcer, regardless of its cause of origin, usually heals within 2 weeks, after the source of injury is resolved. A thermal burn in the oral cavity usually takes longer than that to heal, but whenever this time frame is not respected, the suspicion of a potentially malignant disorder should always arise, and a biopsy should be performed. The present case showed two painful thermal burns with great results in terms of speeding up the relief of symptoms and healing time with soft laser as opposed to the traditional treatment with oral topical corticosteroid.
Acknowledgments
The authors acknowledge the Clinical Research Division of the National Cancer Institute of Brazil (INCA) and Dr. Leonardo Weiss Cohen, PhD, for his excellent contributions with regard to text editing and English revision.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Leblon Medical Center does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iDs: Daniel Cohen Goldemberg  https://orcid.org/0000-0002-0089-1910
https://orcid.org/0000-0002-0089-1910
Andreia Cristina de Melo  https://orcid.org/0000-0002-1201-4333
https://orcid.org/0000-0002-1201-4333
References
- 1. Neville BW, Damn DD, Allen CM, et al. Physical and chemical injuries. In: Oral and maxillofacial pathology. St. Louis, MO: Elsevier Inc., 2015, pp. 259–302. Available at: https://www.elsevier.com/books/oral-and-maxillofacial-pathology/neville/978-1-4557-7052-6/. [Google Scholar]
- 2. Hibbard RA, Blevins R. Palatal burn due to bottle warming in a microwave oven. Pediatrics 1988; 82(3): 382–384. [PubMed] [Google Scholar]
- 3. Hyo Y, Fukutsuji K, Fukushima H, et al. Two cases of thermal burns of the larynx in older men. Auris Nasus Larynx 2017; 44(5): 620–623. [DOI] [PubMed] [Google Scholar]
- 4. Kannan S, Chandrasekaran B, Muthusamy S, et al. Thermal burn of palate in an elderly diabetic patient. Gerodontology 2014; 31(2): 149–152. [DOI] [PubMed] [Google Scholar]
- 5. Wakefield Y, Pemberton MN. Oro-facial thermal injury caused by food heated in a microwave oven. Dent Update 2009; 36(1): 26–27. [DOI] [PubMed] [Google Scholar]
- 6. Sommer AP, Schemmer P, Pavláth AE, et al. Quantum biology in low level light therapy: death of a dogma. Ann Transl Med 2020; 8(7): 440–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sonis ST, Hashemi S, Epstein JB, et al. Could the biological robustness of low level laser therapy (photobiomodulation) impact its use in the management of mucositis in head and neck cancer patients. Oral Oncol 2016; 54: 7–14. [DOI] [PubMed] [Google Scholar]
- 8. Politis C, Schoenaers J, Jacobs R, et al. Wound healing problems in the mouth. Front Physiol 2016; 7: 507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ahad A, Tasneem S, Lamba AK, et al. Healing of self-inflicted thermal injury of palatal mucosa by low-level laser therapy. Spec Care Dentist 2017; 37(6): 314–317. [DOI] [PubMed] [Google Scholar]
- 10. Nahlieli O, Eliav E, Shapira Y, et al. Central palatal burns associated with the eating of microwaved pizzas. Burns 1999; 25(5): 465–466. [DOI] [PubMed] [Google Scholar]
- 11. Antunes HS, Herchenhorn D, Small IA, et al. Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis. Oral Oncol 2017; 71: 11–15. [DOI] [PubMed] [Google Scholar]
- 12. Çavuş Ş, Özmen B. Riga-Fede disease in the upper jaw in an infant. Dermatol Ther 2017; 30(5): e12517. [DOI] [PubMed] [Google Scholar]
- 13. Santos MTBR, de Souza Merli LA, Guare RO, et al. The association of low and high laser treatments. Photomed Laser Surg 2010; 28(4): 565–568. [DOI] [PubMed] [Google Scholar]
- 14. Santos MTBR, Manzano FS, Genovese WJ. Different approaches to dental management of self-inflicted oral trauma: oral shield, botulinum toxin type A neuromuscular block, and oral surgery. Quintessence Int 2008; 39(2): e63–e69. [PubMed] [Google Scholar]


