Abstract
Inflammatory myofibroblastic tumor (IMT) is an extremely rare disease composed of myofibroblast cells and inflammatory infiltrates. There are different sites of the urogenital system affected by IMT-bladder, prostate and kidney.
We report a case of a 59-year-old male patient presented with abdominal pain, gross hematuria and a renal mass treated with partial nephrectomy. The final diagnosis was renal inflammatory myofibroblastic tumor. Despite recent improvements in imaging technology, preoperative diagnosis of IMT remains a dilemma. It is therefore mandatory to carry out clinical interpretation, careful histologic examination, and immunohistochemical studies which will generally determine the appropriate diagnosis and patient management.
Keywords: Inflammatory tumor, Kidney, Partial nephrectomy
Introduction
Inflammatory myofibroblastic tumor (IMT) is an extremely rare disease composed of myofibroblast cells and inflammatory infiltrates. There is no prevalence in rates regarding age and gender. The first case of BMI was described in 1937 and affected the lungs. Subsequent reports have published other extrapulmonary localizations of this disease 1, 2. There are different sites of the urogenital system affected by IMT-bladder, prostate and rarely the kidney 3, 4. Because of its rare occurrence, it is possible that it is not considered by the physician, and the fact that it usually mimics renal cell carcinoma can potentially lead to be overdiagnosed as a malignancy both clinically and pathologically. In the time of the “nephron-sparing” surgery it is very important to report such rare benign renal tumors to determine their reliable characteristics, and avoid performing unnecessary radical interventions.
We report a case of renal inflammatory myofibroblastic tumor where our patient was presented with a renal mass and was treated with partial nephrectomy.
Case presentation
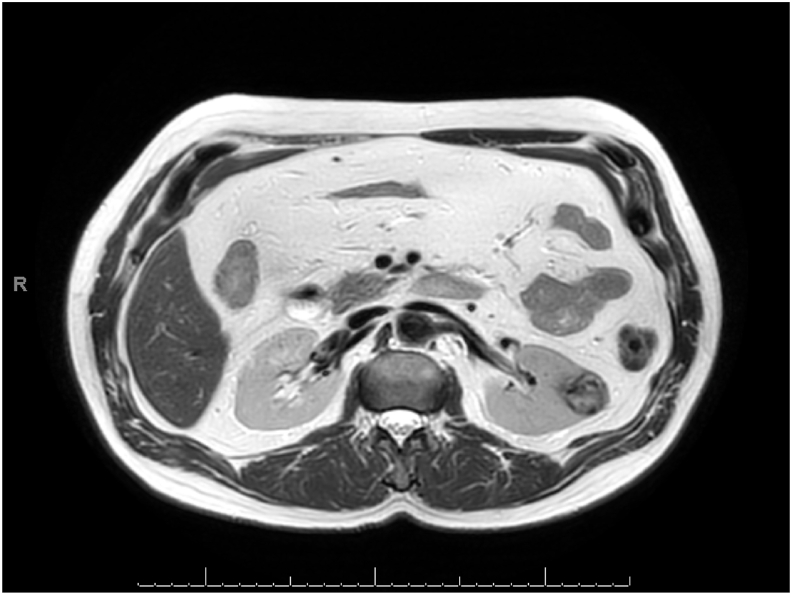
A 59-year-old male patient was presented with abdominal pain and gross hematuria. There was no past or family history of a kidney disease or renal trauma, only arterial hypertension as a comorbidity. The patient was a smoker-a pack of cigarettes per day. Basic laboratory examinations of complete blood count, and serum biochemistry were normal. Initially, to be found the source of the abdominal pain a CT scan and a complementary MRI were performed (Fig. 1).
Fig. 1.
MRI of a tumor mass at the left kidney.
They revealed the presence of a left medial renal atypical cystic lesion on the convexity measured at 30 mm with description of a hemorrhagic component and an enhanced tissue component. Also, the information about hematuria combined with smoking obliged us to take under account, and not underestimate endo-vesical lesion. For that reason a cystoscopy was performed with a removal of urinary cytology at the beginning of the procedure. There was an absence of visible suspicious endo-vesical lesions and increased prostate volume. Concerning the renal lesion, the case was presented to the multidisciplinary meeting of onco-urology and after a discussion the diagnostic therapeutic strategies were defined. A chest CT scan was performed and excluded the metastatic extension of the renal tumor. The preoperative MRI gave us the following conclusion: “left renal mass, average polar measuring 38 × 22 mm over a height of 29 mm. It has fluid, hemorrhagic, tissue, and necrotic components, as well as heterogeneous early enhancement. The whole evokes on first hypothesis as a primary renal lesion compatible with tubulo-papillary carcinoma of type 2. No argument for a metastatic attack”.
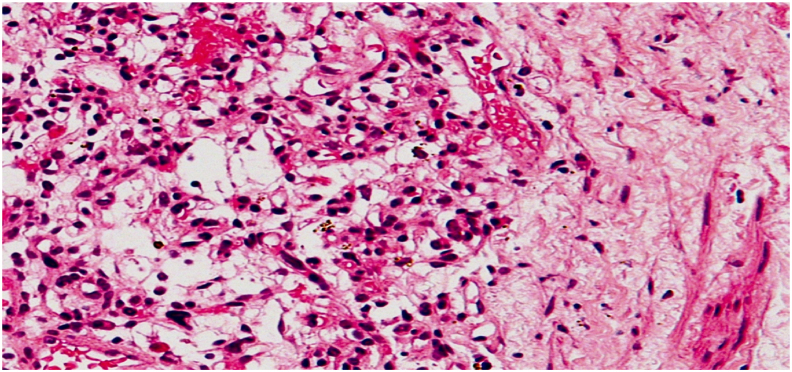
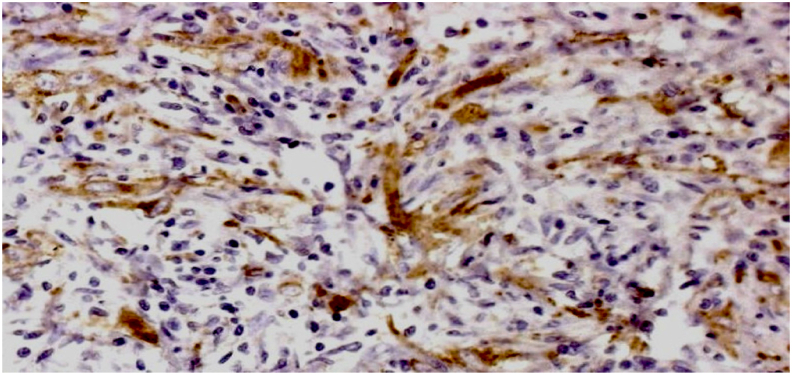
Partial left nephrectomy by lumbotomy was performed with any complications, and the patient was discharged on the third day after the intervention. Histopathology examination resulted in a lesion consisting of spindle-shaped, elongated cells with no marked cytonuclear atypia; fibroblasts; myofibroblasts; lymphocytes; histiocytes loaded with hemosiderin pigments, and also vascular contingent made essentially of capillary vessels (Fig. 2). Immunohistochemical study carried out there is a positivity of SMA (Smooth Muscle Actine) and a negativity of ALK (Anaplastic Lymphoma Kinase) as well as Cytokeratin AE1/AE3 and EMA (Fig. 3). As a conclusion the histological aspect was in favor of an inflammatory myofibroblastic tumor (inflammatory pseudotumor).
Fig. 2.
Classic histological finding.
Fig. 3.
SMA positivity.
Discussion
Inflammatory myofibroblastic tumor of the kidney is a rare benign disease of the kidney which is characterized with mass forming proliferation of myofibroblasts, fibroblasts, histiocytes, and plasma cells in the affected portion of the kidney 3. In addition to the first case of lung involvement, BMI can be localized in many other organs. As for the urogenital system, the rates of kidney involvement are extremely low 2. There's no noteworthy distinction between sex and age. The origin of IMT is very disputable and the focus of the discussion is the question: “Whether it is a truly neoplastic or a post inflammatory process?“. Presumed and described in the literature etiological factors are: Epstein Barr virus (EBV), Human herpes virus (HHV8), and over expression of interleukin IL-6 4. Recent studies suggest that BMI is a neoplasm rather than an inflammatory process due to available cytogenetic clonality, aggressive local behavior, and manifestations of metastases 1. Common clinical features for this entity are lumbar pain and hematuria. Physical examinations and radiological investigations are often inconclusive. The radiographic image of IMT depends on the type of examination. In ultrasound examination it is hypo- or heteroechogenic mass, in Doppler-hypoechoic mass with intra-tumor vascularization, in CT-mass with low attenuation and in MRI-hypovascular lesion 3. Also, the histological changes make the diagnosis difficult. It is composed of spindle cells with variable inflammatory component 4. There are 3 histologic patterns for IMT: a myxoid and vascular pattern with inflammatory infiltrate (same as our case), compact spindle cell proliferation, and hypocellular fibrous pattern 2. Preoperative diagnosis of IMT is only confirmed by nephrectomy and pathologic assessment 3. Differential diagnoses include malignant tumors such as renal cell carcinoma, sarcomatoid renal cell carcinoma, inflammatory fibrosarcoma, malignant fibrous histiocytoma, low grade neurogenic tumor, myxoid leimyosarcoma and non-malignant tumors such as angiomyolipoma, xanthogranuloma pyelonephritis and plasma cell granuloma 5. In rare cases, local recurrence or malignant transformation may be observed, presumably due to non-radical resection 1.
Conclusions
Despite recent improvements in imaging technology, preoperative diagnosis of IMT remains a dilemma, and final diagnosis is predicated on histopathologic evaluation of the involved tissue. In the present case, a partial left nephrectomy was carried out as the disease was presumed to be a tubulo-papillary carcinoma of type 2. Histological examination of the specimen confirmed IMT. It is therefore, mandatory to carry out clinical interpretation, careful histologic examination, and immunohistochemical studies which will generally determine the appropriate diagnosis and patient management.
Declaration of competing interest
The authors declare that they have no competing interests.
Contributor Information
A.S. Ivanov, Email: dratanasivanov@yahoo.bg.
P.A. Antonov, Email: p_antonov@abv.bg.
Z.R. Chitalov, Email: chitalov63@gmail.com.
References
- 1.Coffin C.M., Watterson J., Priest J.R., Dehner L.P. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995;19:859–872. doi: 10.1097/00000478-199508000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Pungpapong S., Geiger X.J., Raimondo M. Inflammatory myofibroblastic tumor presenting as a pancreatic mass: a case report and review of the literature. JOP. 2004;5:360–367. [PubMed] [Google Scholar]
- 3.Kapusta L.R., Weiss M.A., Ramsay J., Lopez-Beltran A., Srigley J.R. Inflammatory myofibroblastic tumors of the kidney: a clinicopathologic and immunohistochemical study of 12 cases. Am J Surg Pathol. 2003;27:658–666. doi: 10.1097/00000478-200305000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Tarhan F., Gul A.E., Karadayi N., Kuyumcuoglu U. Inflammatory pseudotumor of the kidney: a case report. Int Urol Nephrol. 2004;36(2):137–140. doi: 10.1023/b:urol.0000034662.23919.0b. [DOI] [PubMed] [Google Scholar]
- 5.Larbcharoensub N., Chobpradit N., Kijvikai K., Chalermsanyakorn P. Primary renal inflammatory myofibroblastic tumor. Urol Int. 2006;76:94–96. doi: 10.1159/000089745. [DOI] [PubMed] [Google Scholar]