Abstract
BACKGROUND
Nonagenarians (NG), individuals aged ≥ 90 years, constitute an increasing proportion of hospitalizations presenting with atrial fibrillation (AF). However, not much is known about demographics, clinical outcomes, and trends of hospitalizations. Therefore, we analyzed data about hospitalizations and clinical outcomes among NGs with AF over ten years from 2005 to 2014 using a publically available database, the National Inpatient Sample.
METHODS
All hospitalizations and major outcomes of subjects ≥ 90 years with a primary diagnosis of AF (ICD-9-CM code 427.31) over a ten-year period were assessed in this study by multivariate logistic regression analysis.
RESULTS
There were more females than males (176,268 females, 51,384 males) in this analysis. The number of hospitalizations for AF among NG increased by 50% (17,295 in 2005 to 25,830 in 2014). Males were more likely to undergo cardioversion (6.14% of males vs. 5.06% of females, P < 0.0001). Over this period, in-hospital mortality declined from 3.21% in 2005 to 2.38% in 2014 ( P = 0.0041), with higher in-hospital mortality in males (3.23% in males vs. 2.76% in females, P = 0.0138), mean length of hospitalization decreased from 4.53 days to 4.13 days (P < 0.0001), the prevalence of congestive heart failure fell from 0.48% to 0.23% ( P = 0.0257), and the use of anticoagulation increased from 6.09% to 14.54% (P < 0.0001). In a multivariate analysis, hospital admission on the weekend, Elixhauser comorbidity index, CHA 2DS2VASc score, acute respiratory failure, and the length of hospital stay were associated with a higher risk of in-hospital mortality.
CONCLUSIONS
From 2005 to 2014, AF-related hospitalizations among NGs increased, more so in in females population, mortality trends improved, rates of anticoagulation increased, and cardioversions increased. Despite the decreasing trend of in-hospital mortality since 2005, the relatively high mortality rate in males warrants further studies.
Atrial fibrillation (AF), the most common sustained arrhythmia, is associated with significant morbidity and an enormous economic burden to society.[1] The prevalence of AF in the general population continues to rise. It is well recognized that the prevalence of AF increases with age. However, the literature on AF in the subjects older than 90 years, also called nonagenarians (NG), is limited. The present study aimed to investigate AF hospitalization trends, gender-specific outcomes, and factors associated with in-hospital mortality in the NG population using a large publically available database, the National Inpatient Sample (NIS).
METHODS
A detailed description of the NIS database has been reported in prior studies.[2,3] The NIS represents the largest, all-payer database of inpatient hospitalizations in the United States that is maintained by the Agency for Health Care Quality and Research (AHRQ). The NIS includes a random 20% sample of all inpatient hospitalizations from forty-six states in the United States from 1998 to 2014. Each observation in the NIS represents an individual hospitalization with a primary diagnosis, up to twenty-nine secondary diagnoses, and up to fifteen procedure codes. All discharge diagnoses and procedures were coded using the International Classification of Disease, 9th revision, clinical modification (ICD-9-CM) codes.
Hospitalizations in the NIS reflect two different sampling strategies: (1) before 2012, the NIS included all discharges from a random sample of 20% of acute care hospitals in the United States, stratified by bed size, region, and location; and (2) starting in 2012, the NIS included a random sample of 20% of discharges from all acute care hospitals in the United States; this effort reduced the margin of error by 50%, and national estimates decreased by 4.3%. From 1998 to 2011, discharge weights are provided by the AHRQ after a validation process, and they are used to calculate national estimates. As recommended by the AHRQ, to account for the differences in sampling strategy from 2012 to 2014 compared with before 2012, revised discharge weights termed “trend weights” are used for 2011 and all preceding years, while computing national estimates to ensure comparability across years and to facilitate trend analysis from 1998 to 2014.
Study Population
The study protocol was reviewed by the University of Arkansas for Medical Sciences, Little Rock, Arkansas, Institutional Review Board, and was exempted from review as it includes only de-identified, publicly available data. For our analysis, we only used NIS data from 2005 to 2014. Like previous studies, we used the ICD-9-CM code 427.31 to identify hospitalizations involving principal diagnosis of AF.[4] Starting in 2012, the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project has reported the age as ‘90’ for all the hospitalizations of age greater than or equal to 90 years.
Outcomes Assessment
From the study cohort, we abstracted demographic data, payment type, and co-morbid diseases. Anticoagulated hospitalizations with AF were identified using the ICD-9-CM code V58.61, which represents a long-term and current use of anticoagulants. ICD-9-procedure codes 9961, 9962, and 9969 were used to identify hospitalizations undergoing cardioversion. We then abstracted length of stay (days) data for all the hospitalizations.
Statistical Analysis
As recommended by the AHRQ, we used survey analysis methods to account for the clustering and stratification of hospitalizations for all continuous and categorical variables. SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA) software was used to perform statistical analysis. We used sampling weights to estimate trends and national estimates to account for the change in sampling design as recommended by the AHRQ. Pearson’s chi-square test for categorical variables and student t-test was used to evaluate the differences in the demographics among males and females. Multivariate logistic regression analysis (proc surveylogistic) was used to create a regression model for evaluating the predictors of in-hospital mortality after the major covariates were considered for adjustment. Like previous studies, trends in hospitalization demographics, co-morbid diseases, weekend hospitalizations with AF, length of hospitalization, in-hospital mortality were evaluated using the logistic models after creating the dummy variables for each outcome of interest. A two-sided P-value < 0.05 was considered statistically significant. The trends for the cost of hospitalization were adjusted for inflation. [5] The checklist provided by NIS was used to ensure the appropriateness of data analysis as recommended by AHRQ.[6]
RESULTS
From January 2005 to December 2014, there were 227,652 hospitalizations for AF aged 90 years and older (Table 1). Among the subjects, there were 51,384 males and 176,268 females. 88.47% of subjects were Caucasians. Gender differences were noted among Caucasians and Blacks and Hispanics.
1. Demographic characteristics of nonagenarian hospitalizations admitted with atrial fibrillation.
| Total | Male | Female | P-value | |
| Data are presented as n or %. *Refers to express as percentage of the weighted hospitalizations in the respective column. | ||||
| Unweighted index admissions | 47,026 | 10,582 | 36,444 | |
| Weighted index admissions | 227,652 | 51,384 | 176,268 | |
| CHA2DS2VASc score (mean) | 3.83 | 3.03 | 4.06 | < 0.0001 |
| Disposition of the hospitalization* | < 0.0001 | |||
| Routine* | 38.71% | 42.41% | 37.64% | |
| Transfer to short-term hospital* | 1.42% | 1.96% | 1.27% | |
| Skilled nursing facility or Intermediate care facility* | 35.49% | 31.25% | 36.74% | |
| Home health care* | 21.26% | 20.73% | 21.42% | |
| Left against medical advice* | 0.2% | 0.40% | 0.14% | |
| Died in hospital* | 2.86% | 3.23% | 2.76% | |
| Discharged alive, destination unknown* | 0.03% | 0.03% | 0.04% | |
| Length of hospital stay*, days | 0.2260 | |||
| 0−7* | 88.67% | 88.77% | 88.64% | |
| 8−14* | 9.80% | 9.54% | 9.87% | |
| > 14* | 1.52% | 1.68% | 1.48% | |
| Mean length of stay | 4.24 | 4.14 | 4.27 | 0.0001 |
| Primary expected payer* | < 0.0001 | |||
| Medicare* | 94.77% | 93.92% | 95.03% | |
| Medicaid* | 0.55% | 0.63% | 0.53% | |
| Private insurance* | 3.82% | 4.21% | 3.72% | |
| Self-pay* | 0.28% | 0.26% | 0.29% | |
| Other* | 0.55% | 0.98% | 0.44% | |
| Race* | < 0.0001 | |||
| White* | 88.47% | 88.04% | 88.60% | |
| Black* | 4.55% | 3.64% | 4.83% | |
| Hispanic* | 3.7% | 4.48% | 3.48% | |
| Asian* | 1.25% | 1.65% | 1.14% | |
| Other* | 2.00% | 2.18% | 1.96% | |
| Cost of hospitalizations (mean) | 7168.5 | 7573.3 | 7050.8 | < 0.0001 |
| Hospital location and teaching status | 0.035 | |||
| Rural* | 16.42% | 15.59% | 16.67% | |
| Urban non-teaching* | 44.98% | 45.79% | 44.75% | |
| Urban teaching* | 38.59% | 38.61% | 38.58% | |
| Comorbidities* | ||||
| Alcohol abuse* | 0.29% | 0.83% | 0.13% | < 0.0001 |
| Congestive heart failure* | 0.45% | 0.55% | 0.43% | 0.1131 |
| Depression* | 7.65% | 5.6% | 8.25% | < 0.0001 |
| Diabetes with chronic complications* | 1.42% | 1.99% | 1.26% | < 0.0001 |
| Hypertension (combine uncomplicated and complicated)* | 70.30% | 64.33% | 72.04% | < 0.0001 |
| Liver disease* | 0.28% | 0.32% | 0.27% | 0.4017 |
| Obesity* | 1.38% | 1.06% | 1.48% | < 0.0013 |
| Peripheral vascular disorder* | 7.91% | 10.34% | 7.20% | < 0.0001 |
| Renal failure* | 19.01% | 25.73% | 17.05% | < 0.0001 |
| Uncomplicated diabetes* | 12.97% | 14.3% | 12.58% | < 0.0001 |
| In-hospital mortality* | 2.86% | 3.22% | 2.76% | 0.0138 |
| Cardioversion rates* | 5.30% | 6.14% | 5.06% | < 0.0001 |
Compared to females, males had higher prevalence of complicated and uncomplicated diabetes (1.99% vs. 1.26% & 14.3% vs. 12.58%, respectively), alcohol abuse (0.83% vs. 0.13%), peripheral vascular disease (10.34% vs. 7.20%), and renal failure (25.73% vs. 17.05%). Females had higher prevalence of depression (8.25% vs. 5.6%), hypertension (72.04% vs. 64.33%), and obesity (1.48% vs. 1.06%) when compared to males (Table 1).
The mean length of stay was marginally higher among females (4.24 days in females vs. 4.14 days in males, P = 0.0001). Medicare was the primary expected payer for 94.77% of hospitalizations, most hospitalizations were 0−7 days (88.67%), and most subjects were hospitalized in large and urban non-teaching hospitals. Male subjects had higher utilization of cardioversion (6.14% in malesvs. 5.06% in females) and higher in-hospital mortality (3.23% in males vs. 2.76% in females).
38.7% of subjects were discharged to home (or self-care) and 35.4% of subjects to care facilities (skilled nursing or intermediate care), and 21.2% of subjects to home health care. A higher proportion of females were discharged to skilled nursing or intermediate care facilities (36.7% in females vs. 31.2% in males).
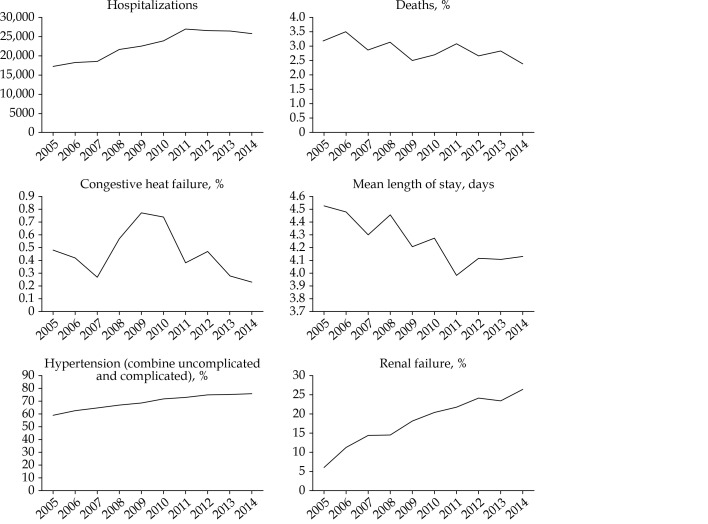
Trends of hospitalizations, outcomes, and associated comorbidities among NGs with AF from 2005 to 2014 are shown in Figure 1 and Table 2. Hospitalizations for AF among NG increased by almost 50% (from 17,295 to 25,830), and in-hospital mortality declined from 3.21% to 2.38% (P = 0.0041). Female hospitalizations were consistently higher during all the years. The majority of hospitalizations were Caucasians (91.6% in 2005 to 87.7% in 2014). The mean length of hospitalization gradually declined from 4.53 days in 2005 to 4.13 days in 2014 (Ptrend-value < 0.0001). There was a gradual trend of increase in hospitalization in urban-teaching hospitals from 2005 to 2014. There was a higher number of hospitalizations in the urban non-teaching hospitalizations during the early years of our study.
1.
Trends of hospitalizations, outcomes, and associated comorbidities among nonagenarians with atrial fibrillation from 2005 to 2014.
2. Year-wise baseline demographics and comorbidities in nonagenarians subjects with atrial fibrillation.
| Years | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Ptrend-value |
| Data are presented as n or %. *Refers to express as percentage of the total hospitalizations in the respective column. | |||||||||||
| Weighted hospitalizations | 17,295 | 18,217 | 18,548 | 21,538 | 22,474 | 23,784 | 26,973 | 26,554 | 26,434 | 25,830 | |
| Indicator of sex* | |||||||||||
| Male* | 22% | 22.88% | 22.56% | 21.9% | 23.05% | 23.1% | 21.86% | 22.73% | 23.25% | 22.3% | 0.6453 |
| Female* | 78% | 77.12% | 77.44% | 78.1% | 76.95% | 76.9% | 78.14% | 77.27% | 76.75% | 77.7% | |
| Admission day* | |||||||||||
| Weekday* | 77.84% | 79.24% | 77.35% | 76.56% | 77.46% | 77.5% | 77.1% | 76.61% | 76.39% | 77.04% | 0.0132 |
| Weekend* | 22.16% | 20.76% | 22.65% | 23.44% | 22.54% | 22.5% | 22.9% | 23.39% | 23.61% | 22.96% | |
| Died during hospitalization* | |||||||||||
| Did not die* | 96.79% | 96.48% | 97.12% | 96.84% | 97.48% | 97.29% | 96.91% | 97.34% | 97.16% | 97.62% | 0.0041 |
| Died* | 3.21% | 3.52% | 2.88% | 3.16% | 2.52% | 2.71% | 3.09% | 2.66% | 2.84% | 2.38% | |
| Race* | |||||||||||
| White* | 91.61% | 88.52% | 88.37% | 88.7% | 86.73% | 88.79% | 89.12% | 88.67% | 87.73% | 87.7% | < 0.0001 |
| Black* | 3.97% | 4.91% | 4.65% | 3.82% | 4.32% | 4.99% | 4.53% | 4.65% | 4.98% | 4.42% | 0.0002 |
| Hispanic* | 2.42% | 3.81% | 3.38% | 3.76% | 4.07% | 3% | 4.04% | 3.46% | 4.09% | 4.32% | 0.0002 |
| Asian or Pacific Islander* | 1.01% | 1.45% | 1.62% | 1.06% | 1.73% | 0.83% | 0.8% | 1.25% | 1.39% | 1.52% | 0.0946 |
| Other* | 1% | 1.31% | 1.98% | 2.65% | 3.13% | 2.38% | 1.52% | 1.97% | 1.81% | 2.04% | 0.0104 |
| Length of stay*, days | |||||||||||
| 0−3* | 49.12% | 51.33% | 50.24% | 49.64% | 51.17% | 50.83% | 53.96% | 53.8% | 53.1% | 52.39% | < 0.0001 |
| 4−6* | 31.8% | 30.39% | 32.22% | 32.09% | 32.27% | 32.54% | 31.92% | 30.42% | 31.37% | 32.51% | 0.8685 |
| 7−9* | 11.12% | 11.41% | 11.36% | 11.55% | 10.8% | 11.08% | 9.36% | 10.79% | 10.08% | 10.05% | 0.0012 |
| 10−12* | 4.22% | 3.72% | 3.25% | 3.9% | 3.67% | 3.14% | 2.74% | 2.9% | 3.31% | 2.79% | < 0.0001 |
| ≥ 12* | 3.74% | 3.15% | 2.93% | 2.82% | 2.09% | 2.41% | 2.01% | 2.09% | 2.14% | 2.27% | < 0.0001 |
| Mean length of stay, days | 4.53 | 4.48 | 4.3 | 4.46 | 4.21 | 4.28 | 3.98 | 4.12 | 4.11 | 4.13 | < 0.0001 |
| Hospital location and teaching status* | |||||||||||
| Rural* | 20.08% | 19.92% | 18.99% | 15.64% | 15.29% | 16.89% | 15.75% | 16% | 15.74% | 12.74% | < 0.0001 |
| Urban non-teaching* | 49.43% | 44.31% | 48.27% | 48.54% | 50.05% | 48.5% | 45.86% | 44.61% | 42.63% | 31.49% | < 0.0001 |
| Urban teaching* | 30.49% | 35.77% | 32.74% | 35.82% | 34.66% | 34.62% | 38.39% | 39.39% | 41.63% | 55.77% | < 0.0001 |
| Comorbidities* | |||||||||||
| Alcohol abuse* | 0.31% | 0.32% | 0.36% | 0.28% | 0.33% | 0.13% | 0.34% | 0.23% | 0.32% | 0.37% | 0.9622 |
| Congestive heart failure* | 0.48% | 0.42% | 0.27% | 0.57% | 0.77% | 0.74% | 0.38% | 0.47% | 0.28% | 0.23% | 0.0257 |
| Depression* | 5.83% | 6.51% | 7.51% | 7.54% | 6.95% | 7.46% | 7.92% | 8.6% | 8.61% | 8.44% | < 0.0001 |
| Diabetes with chronic complications* | 1.06% | 0.81% | 0.89% | 1.27% | 1.53% | 1.36% | 1.65% | 1.6% | 1.66% | 1.96% | < 0.0001 |
| Hypertension (combine uncomplicated and complicated)* | 59.08% | 62.54% | 64.79% | 67.12% | 68.63% | 72.09% | 73.17% | 75.15% | 75.71% | 76.23% | < 0.0001 |
| Liver disease* | 0.17% | 0.14% | 0.24% | 0.31% | 0.33% | 0.25% | 0.41% | 0.28% | 0.26% | 0.39% | 0.0263 |
| Obesity* | 0.7% | 0.86% | 0.64% | 1.11% | 1.14% | 1.04% | 1.55% | 1.73% | 1.87% | 2.5% | < 0.0001 |
| Peripheral vascular disorder* | 5.5% | 6.34% | 6.94% | 7.45% | 7.98% | 7.61% | 8.18% | 9.19% | 8.95% | 9.31% | < 0.0001 |
| Renal failure* | 6.03% | 11.3% | 14.46% | 14.68% | 18.21% | 20.48% | 21.77% | 24.31% | 23.49% | 26.5% | < 0.0001 |
| Uncomplicated diabetes* | 10.05% | 10.12% | 12.39% | 11.43% | 12.72% | 13.83% | 14.11% | 14.2% | 14.3% | 14.29% | < 0.0001 |
| Cardioversion rates* | 4.35% | 4.48% | 4.09% | 4.78% | 5.17% | 5.19% | 5.71% | 5.95% | 5.77% | 6.52% | < 0.0001 |
| Anticoagulation* | 6.09% | 7.25% | 6.99% | 7.93% | 9.8% | 9.92% | 11.53% | 11.37% | 12.73% | 14.54% | < 0.0001 |
| CHA2DS2VASc score (mean) | 3.66 | 3.69 | 3.75 | 3.78 | 3.81 | 3.85 | 3.89 | 3.9 | 3.9 | 3.91 | < 0.0001 |
| Cost of hospitalization (adjusted for inflation), $ | 7,518.5 | 7,740.8 | 7,869.8 | 8,035.6 | 7,734.0 | 7,852.2 | 7,562.4 | 7,659.4 | 7,716.3 | 7,692.4 | < 0.0001 |
The prevalence of depression, hypertension, liver disease, diabetes with chronic complications, peripheral vascular disorder, psychoses, and obesity increased by 1.5 to 2-fold, while the prevalence of renal failure increased by 4-fold (6.03% in 2005 to 23.49 in 2014, Ptrend-value < 0.0001). In contrast, prevalence of congestive heart failure decreased by 50% (0.48% in 2005 to 0.23% in 2014, Ptrend-value = 0.0257).
The rates of utilization of cardioversion increased over the years (4.35% in 2005 to 6.52% in 2014, Ptrend-value < 0.0001). The anticoagulation rates also increased by almost 2-fold during these years (6.09% in 2005 to 14.54% in 2014, Ptrend-value < 0.0001).
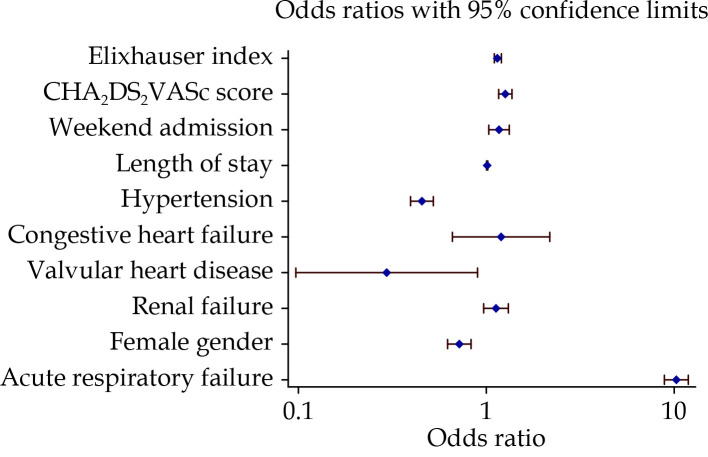
Multivariate logistic regression analysis was performed to assess the estimates for in-hospital mortality. After adjusting for significant covariates and taking the complex sampling of clusters and strata into account, we identified that weekend hospitalization [odds ratio (OR) = 1.161, 95% confidence interval (CI): 1.025–1.316, P = 0.0191], length of stay (OR = 1.011, 95% CI: 1.004−1.018,P = 0.003), CHA2DS2VASc score (OR = 1.26, 95% CI: 1.163−1.365,P ≤ 0.0001), and Elixhauser comorbidity index (OR = 1.147, 95% CI: 1.095−1.201,P ≤ 0.0001) were independently associated with in-hospital mortality. The data are shown in Table 3 (univariate analysis, unadjusted OR) and Figure 2, and Table 4 (multivariate analysis, adjusted OR).
3. Univariate-unadjusted odds ratio for factors associated with in-hospital mortality.
| Odds ratio | 95% Confidence interval | P-value | |
| Weekend admission | 1.19 | 1.05−1.34 | 0.0043 |
| Hypertension | 0.67 | 0.59−0.75 | < 0.0001 |
| Congestive heart failure | 2.92 | 1.77−4.81 | < 0.0001 |
| Valvular heart disease | 0.92 | 0.29−2.88 | 0.8865 |
| Renal failure | 1.47 | 1.29−1.66 | < 0.0001 |
| Female gender | 0.85 | 0.74−0.96 | 0.0138 |
| Acute respiratory failure | 11.7 | 10.18−13.44 | < 0.0001 |
| > or = 7 Chronic conditions | 1.24 | 1.11−1.39 | 0.0001 |
2.
Multivariate logistic regression analysis with adjusted odds ratio for in-hospital mortality.
The adjusted odds ratio, 95% confidence interval, and their P-value represent the odds of in-hospital mortality after adjusting for the covariates listed in Table 4. The blue dots indicate the adjusted odds ratio for the named variable, and the red lines indicate 95% confidence interval. Odds ratio to the right of midline (where odds ratio = 1) indicate higher odds of in-hospital mortality, while odds ratio to the left of the midline indicate lower odds of in-hospital mortality.
4. Multivariate logistic regression analysis for factors associated with in-hospital mortality.
| Effect | Point estimate | 95% Confidence limits | P-value |
| Elixhauser comorbidity index | 1.147 | 1.095−1.201 | < 0.0001 |
| CHA2DS2VASc score | 1.26 | 1.163−1.365 | < 0.0001 |
| Weekend admission | 1.161 | 1.025−1.316 | 0.0191 |
| Length of stay | 1.011 | 1.004−1.018 | 0.003 |
| Hypertension | 0.453 | 0.394−0.521 | < 0.0001 |
| Congestive heart failure | 1.195 | 0.658−2.17 | 0.5574 |
| Valvular heart disease | 0.292 | 0.095−0.894 | 0.031 |
| Renal failure | 1.124 | 0.969−1.303 | 0.1234 |
| Female gender | 0.716 | 0.616−0.832 | < 0.0001 |
| Acute respiratory failure | 10.243 | 8.872−11.825 | < 0.0001 |
DISCUSSION
The main findings of this study are as follows: (1) AF-related hospitalizations among NG have increased from 2005 to 2014; (2) there are higher AF hospitalization rates in females; (3) males has higher rates of in-hospital mortality; (4) proportion of hospitalized NGs with AF receiving anticoagulation has increased; (5) there is a 4-fold increase in the presence of renal failure; and (6) CHA2DS2VASc score, Elixhauser comorbidity index, length of stay, and weekend hospitalizations has an association with the increased risk of in-hospital mortality.
Published studies among the NG population with AF are limited, although the earliest mention was in 2006.[7] Prior studies focused on the incidence of stroke (Berlin-Atrial Fibrillation registry),[8] bleeding outcomes after left atrial appendage closure with the Watchman device,[9] and prognostic significance of new-onset AF after acute myocardial infarction.[10]
In our study, a higher prevalence of hospitalized females was noted. This is not unexpected because it is well recognized that longevity is more common in women compared to men.[11,12–14] Higher percentage of NG females with AF is similar to the NG population reported in the United States census.[15] White race comprised most of the hospitalizations; however, gender-differences were also noted in the Blacks and the Hispanic AF population. These differences point out that fewer Black men and fewer Hispanic women constitute the overall cohort, which is likely related to gender-related discrepancies in treatment for AF among these groups early on in life, which warrants further studies.
The reason for the higher mortality among hospitalized men observed in our analysis can be explained to a certain extent by the higher prevalence of complicated and uncomplicated diabetes, alcohol abuse, peripheral vascular disease, and renal failure. Whether this relates to long-standing AF requiring aggressive rhythm control strategy, as can be inferred from a higher rate of utilization of electrical cardioversion procedures in men comparing to women in our cohort warrants further scrutiny.
A higher proportion of females were discharged to skilled care facilities may be partly explained by higher frequency of obesity and depression resulting in deconditioning requiring physical therapy and rehabilitation.
Although the use of anticoagulation has increased over the recent years in our cohort, it continues to be lower than anticipated based on the age and prevalence of comorbidities. In our sample, only 14.54% of hospitalizations received anticoagulation in 2014. This is despite the high prevalence of significant comorbidities known to be associated with increased risk of stroke in hospitalizations with AF, such as hypertension, diabetes, and renal failure. A one-point mean difference in females versus males in the CHA2DS2VASc score is very likely explained by attributing the extra point for female gender in the scoring. The mean CHA2DS2VASc score in our cohort was 3.83 ± 0.91. Wutzler, et al.[8] also observed that oral anticoagulation therapy was attempted only in 26.5% of subjects. The reasons for improving rates of anticoagulation among NGs can be explained by better awareness of the benefit of anticoagulation in the elderly, incorporation of CHA2DS2VASc score that emphasizes advanced age (over 75-year-old) as an essential incremental risk factor for AF-associated stroke, and recent advancements with widespread use in ambulatory monitoring techniques (event and holter monitors) to facilitate detection of commonly asymptomatic or minimally symptomatic AF in this population.
The ratio of the weekend and weekday hospitalization across ten-year appears to be consistent with prior studies on this topic among AF hospitalizations.[16] The trend towards shorter length of hospital stay from 2005 to 2014 may be an indirect consequence of improved rates of cardioversion, thereby, cardioverting to sinus rhythm and sooner hospital discharge. The observed trends toward decreasing prevalence of congestive heart failure among hospitalized nonagenarian AF population and increasing prevalence of renal failure over the studied period are not completely clear. One potential explanation could be that recent advancements in the primary and secondary prevention of other heart diseases (example: coronary artery disease) simply uncover other competing comorbidities due to less development of heart failure and thus, improved survival.
The weekend hospitalizations in AF are likely associated with poor outcomes due to limited staff availability as reported in the prior studies on weekend hospitalizations for AF.[2,4,16] Acute respiratory failure has very high odds of in-hospital mortality signifies that it is not well tolerated in this population, likely due to underlying comorbidities on top of the AF. Why females and those with hypertension have lower odds of in-hospital mortality after adjusting for comorbidities is poorly understood.
LIMITATIONS
Though our study had the essential strengths of including a large sample, our study is subject to some limitations. On the one hand, the NIS relies on claims data, which can incur inaccurate billing and underestimation of covariates of interest, thus leading to coding bias. Missing values in our data prevented us from including certain variables in the multivariate analysis. On the other hand, we did not evaluate the causes that could have accounted for this difference that are not patient-related but related to the hospital (e.g., staffing differences on weekends).
CONCLUSIONS
Findings of this population-based nationwide study in the United States suggest that AF-related hospitalizations among NG continue to increase. Although in-hospital mortality remains nontrivial, there is a trend towards lowered mortality over recent years. The increased risk of death appears to be primarily associated with underlying medical conditions. The relatively high mortality rate in males as compared to females warrants further study. While the prevalence of AF in this population continues to increase, controlling the AF burden, improving the quality of life, and prevention of stroke in this population continue to pose challenges in the future.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
References
- 1.Chugh SS, Blackshear JL, Shen WK, et al Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001;37:371–378. doi: 10.1016/S0735-1097(00)01107-4. [DOI] [PubMed] [Google Scholar]
- 2.Voruganti DC, Subash Shantha GP, Deshmukh A, et al Outcomes of hospitalizations with atrial fibrillation-flutter on a weekday versus weekend: an analysis from a 2014 nationwide inpatient sample. PeerJ. 2019;7:e6211. doi: 10.7717/peerj.6211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voruganti DC, Shantha G, Dugyala S, et al Temporal trends and factors associated with increased mortality among atrial fibrillation weekend hospitalizations: an insight from National Inpatient Sample 2005–2014. BMC Res Notes. 2019;12:398. doi: 10.1186/s13104-019-4440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deshmukh A, Pant S, Kumar G, et al Comparison of outcomes of weekend versus weekday admissions for atrial fibrillation. Am J Cardiol. 2012;110:208–211. doi: 10.1016/j.amjcard.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 5.United States Bureau of Labor Statistics. United States Bureau of Labor Statistics of CPI Inflation Calculator Web site. https://www.bls.gov/data/inflation_calculator.htm (accessed October 20, 2020).
- 6.Agency for Health Care Quality and Research. Overview of the National (Nationwide) Inpatient Sample (NIS) Web site. https://www.hcup-us.ahrq.gov/nisoverview.jsp (accessed October 20, 2020).
- 7.Formiga F, Ferrer A, Henríquez E, et al [Low percentage of oral anticoagulation in nonagenarians with atrial fibrillation] Rev Clin Esp. 2006;206:410–411. [In Spanish]. doi: 10.1157/13090516. [DOI] [PubMed] [Google Scholar]
- 8.Wutzler A, von Ulmenstein S, Attanasio P, et al Treatment of nonagenarians with atrial fibrillation: insights from the Berlin Atrial Fibrillation (BAF) Registry. J Am Med Dir Assoc. 2015;16:969–972. doi: 10.1016/j.jamda.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 9.Ramos Tuarez FJ, Pino JE, Alrifai A, et al Long-term quality of life in octogenarians and nonagenarians with nonvalvular atrial fibrillation following WATCHMANTM device implantation . Catheter Cardiovasc Interv. 2019;93:1138–1145. doi: 10.1002/ccd.28020. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-Sellés M, Datino T, Figueiras-Graillet LM, et al New-onset atrial fibrillation and prognosis in nonagenarians after acute myocardial infarction. Neth Heart J. 2013;21:499–503. doi: 10.1007/s12471-013-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waldron I Why do women live longer than men? Soc Sci Med. 1976;10:349–362. doi: 10.1016/0037-7856(76)90090-1. [DOI] [PubMed] [Google Scholar]
- 12.Silman AJ Why do women live longer and is it worth it? Br Med J (Clin Res Ed) 1987;294:1311–1312. doi: 10.1136/bmj.294.6583.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austad SN Why women live longer than men: sex differences in longevity. Gend Med. 2006;3:79–92. doi: 10.1016/S1550-8579(06)80198-1. [DOI] [PubMed] [Google Scholar]
- 14.Hazzard WR Why do women live longer than men? Biologic differences that influence longevity. Postgrad Med. 1989;85:271–283. doi: 10.1080/00325481.1989.11700672. [DOI] [PubMed] [Google Scholar]
- 15.United States Census Bureau. 2010 United States Census Special Reports Web site. https://www.census.gov/prod/cen2010/reports/c2010sr-03.pdf (accessed October 20, 2020).
- 16.Weeda ER, Hodgdon N, Do T, et al Association between weekend admission for atrial fibrillation or flutter and in-hospital mortality, procedure utilization, length-of-stay and treatment costs. Int J Cardiol. 2016;202:427–429. doi: 10.1016/j.ijcard.2015.09.053. [DOI] [PubMed] [Google Scholar]