Key Points
Question
Is the STOP-Bang (snoring, tiredness, observed apnea, blood pressure, body mass index, age, neck size, gender) questionnaire a valid obstructive sleep apnea screening tool for patients referred to sleep clinics in different geographical populations?
Findings
This systematic review and meta-analysis of 47 studies including 26 547 individuals found that the STOP-Bang questionnaire has adequate sensitivity and diagnostic accuracy for detecting moderate to severe obstructive sleep apnea across geographic regions.
Meaning
These findings suggest that the STOP-Bang questionnaire can be used as a screening tool in different geographical regions for triaging patients suspected of having obstructive sleep apnea who are referred to sleep clinics.
This systematic review and meta-analysis evaluates the utility of the STOP-Bang (snoring, tired, observed apnea, blood pressure, body mass index, age, neck size, gender) questionnaire in the sleep clinic setting to screen for and stratify the risk of obstructive sleep apnea among populations from different geographical regions.
Abstract
Importance
Obstructive sleep apnea (OSA) is a highly prevalent global health concern and is associated with many adverse outcomes for patients.
Objective
To evaluate the utility of the STOP-Bang (snoring, tiredness, observed apnea, blood pressure, body mass index, age, neck size, gender) questionnaire in the sleep clinic setting to screen for and stratify the risk of OSA among populations from different geographical regions.
Data Sources and Study Selection
MEDLINE, MEDLINE In-process, Embase, EmCare Nursing, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, PsycINFO, Journals@Ovid, Web of Science, Scopus, and CINAHL electronic databases were systematically searched from January 2008 to March 2020. This was done to identify studies that used the STOP-Bang questionnaire and polysomnography testing in adults referred to sleep clinics.
Data Extraction and Synthesis
Clinical and demographic data were extracted from each article independently by 2 reviewers. The combined test characteristics were calculated using 2 × 2 contingency tables. Random-effects meta-analyses and metaregression with sensitivity analyses were performed. The Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guideline was followed.
Main Outcomes and Measures
The combined test characteristics and area under summary receiver operating characteristic curves (AUCs) were used to compare STOP-Bang questionnaire accuracy with polysomnography testing.
Results
A total of 47 studies with 26 547 participants (mean [SD] age, 50 [5] years; mean [SD] body mass index, 32 [3]; 16 780 [65%] men) met the criteria for the systematic review. Studies were organized in different geographic regional groups: North America, South America, Europe, Middle East, East Asia, and South or Southeast Asia. The prevalence rates for all OSA, moderate to severe OSA, and severe OSA were 80% (95% CI, 80%-81%), 58% (95% CI, 58%-59%), and 39% (95% CI, 38%-39%), respectively. A STOP-Bang score of at least 3 had excellent sensitivity (>90%) and high discriminative power to exclude moderate to severe and severe OSA, with negative predictive values of 77% (95% CI, 75%-78%) and 91% (95% CI, 90%-92%), respectively. The diagnostic accuracy of a STOP-Bang score of at least 3 to detect moderate to severe OSA was high (>0.80) in all regions except East Asia (0.52; 95% CI, 0.48-0.56).
Conclusions and Relevance
The results of this meta-analysis suggest that the STOP-Bang questionnaire can be used as a screening tool to assist in triaging patients with suspected OSA referred to sleep clinics in different global regions.
Introduction
Obstructive sleep apnea (OSA) is an increasingly prevalent health condition globally. Its prevalence varies depending on geographic and demographic factors.1 Nevertheless, worldwide, an estimated 425 million individuals aged 30 to 69 years have moderate to severe OSA,2 and in the general adult population, 80% to 90% of OSA is untreated and undiagnosed.3 Unrecognized OSA is a significant health concern,4 associated with various diseases,5,6 public safety hazards,7 and all-cause mortality.8 Thus, it is imperative to consider strategies focusing on early diagnosis and treatment of OSA.
The criterion-standard test for OSA diagnosis is laboratory polysomnography (PSG), but it is costly and inconvenient. Home sleep apnea testing (HSAT) is an acceptable alternative; however, accessibility is lacking in resource-limited areas. Since waitlists are long for patient assessment at a sleep clinic, an effective screening tool is necessary to triage patients.9
The STOP-Bang questionnaire was developed as an OSA screening tool consisting of 4 self-reportable (STOP: snoring, tiredness, observed apnea, and high blood pressure) and 4 demographic (Bang: body mass index [BMI; calculated as weight in kilograms divided by height in meters squared], age, neck circumference, and gender) items. In the initial validation study, at a score of at least 3, the STOP-Bang questionnaire demonstrated a sensitivity of 84%, 93%, and 100% to detect all OSA (apnea-hypopnea index [AHI] ≥5), moderate OSA (AHI ≥15), and severe OSA (AHI ≥30), respectively.10 Because of its high diagnostic accuracy, ease of use, and clear thresholds for risk stratification,10,11 the STOP-Bang questionnaire has been used worldwide. Two STOP-Bang questionnaire items, BMI and neck circumference, are influenced by region-specific body characteristics, which may affect the performance of STOP-Bang questionnaire in different geographic areas. The objective of this systematic review and meta-analysis was to determine the utility of the STOP-Bang questionnaire as an OSA screening tool to assist in triaging patients referred to sleep clinics in different global regions.
Methods
Literature Search and Data Sources
The protocol of this systematic review and meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42020196952) and followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.12 One of us, a medical information specialist (M.E.), designed a literature search strategy using free-text and index terms (ie, stop-bang or stopbang) and systematically searched the following databases from January 2008 to March 2020 with no language restrictions: MEDLINE, MEDLINE In-process, Embase, EmCare Nursing, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, PsycINFO and Journals@Ovid with full-text searching using the Ovid search interface; Web of Science (Clarivate Analytics), Scopus (Elsevier), and CINAHL. A Web of Science citation search was run on the initial STOP-Bang validation article to capture publications in which it has been cited.10 A manual citation search was performed. Continued literature surveillance was done through August 2020. The electronic search strategy appears in eTable 1 in the Supplement.
Inclusion Criteria and Study Selection
Two of us (B.P. and L.C.) independently screened titles and abstracts of identified studies. After initial exclusion, full-text articles were assessed for the following inclusion criteria: (1) assessment of the STOP-Bang questionnaire to screen for OSA in adults (age ≥18 years); (2) patients referred to sleep clinic; (3) laboratory PSG or HSAT results confirmed the OSA diagnosis; and (4) AHI or respiratory disturbance index (RDI) was used to diagnose and grade the severity of OSA. Exclusion criteria were (1) pregnant populations; (2) use of a modified STOP-Bang questionnaire; (3) no analysis of test characteristics at a STOP-Bang score of at least 3; and (4) inadequate description of methods (ie, no report of PSG device used and OSA diagnosed without an AHI cutoff) or insufficient data for meta-analysis. Disagreements were resolved by discussion and consensus among 4 of us (B.P., L.C., M.N., and F.C.).
Data Extraction and Synthesis
Two of us (B.P. and L.C.) independently extracted clinical and demographic data using a predesigned form. Internal and external validity of the included studies was assessed independently according to the Cochrane Methods group’s guidelines on screening and diagnostic tests.13 Discrepancies were addressed with another author (M.N.).
Defining Geographic Regional Groups
Studies were organized into groups dependent on their geographical location (ie, North America, South America, Europe, Middle East, East Asia, South or Southeast Asia). Asian countries were separated into East Asia and South or Southeast Asia to match population demographic characteristics and mitigate factors affecting OSA prevalence (ie, craniofacial characteristics and body habitus differences).2,14
Statistical Analysis
Meta-analysis was performed using Review Manager version 5.3 (The Cochrane Collaboration) and Stata/SE version 14.2 (StataCorp). Summary statistics were computed for all variables of interest. Mean and standard deviation were used as appropriate for descriptive statistics. When applicable, frequencies and percentages were reported. Sample size was considered when calculating the means and standard deviations for age and BMI from individual studies.
The following AHI cutoffs were adopted: all OSA (AHI ≥5), moderate to severe OSA (AHI ≥15), and severe OSA (AHI ≥30). A STOP-Bang score of 3 or greater was adopted as a threshold. A 2 × 2 contingency table was reconstructed for each AHI cutoff at a STOP-Bang score of 3 or greater for each study. The random-effects bivariate analysis model was used to combine results from individual studies to obtain the following log-transformed summary estimates with 95% CIs: sensitivity, specificity, and log scale diagnostic odds ratio (DOR).15,16,17 This method analyzed paired outcomes, ie, sensitivity and specificity values from individual studies, while incorporating correlations between outcomes. For cells with a 0 value, a correction factor of 0.5 was added to prevent problems associated with sensitivity and specificity equaling.18 The following test characteristics were recalculated with 95% CIs: prevalence, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and log scale DOR. The summary area under the receiver operating characteristic (AUC) curves were calculated by logistic regression. Combined test characteristics were recalculated for each regional group at each OSA severity cutoff. Forest plots were designed using a random-effects model, while log scale DOR and AUC curve analysis were presented to assess diagnostic ability. Heterogeneity (I2) was assessed using the χ2 test, with P < .05 indicating that heterogeneity was present.
To determine the association between STOP-Bang score and probability of moderate to severe and severe OSA, posttest probabilities were calculated as previously described and combined from studies that assessed the performance of the STOP-Bang questionnaire at scores from 3 to 8. Results were produced as a bar graph.
Metaregression and sensitivity analyses were performed on various subgroups for each factor at each OSA severity using the Open MetaAnalyst software16 for continuous variables (ie, age, sex, BMI, neck circumference, and prevalence) and categorical variables (sample size, study design, validation tool, OSA criteria, and regional/ethnic groups). This aimed to measure these variables’ associations with the combined estimates of sensitivity, specificity, and log scale DOR. Robustness of the combined estimates was checked by leave-one-out meta-analysis to assess individual study association with the combined estimates and heterogeneity. A 2-tailed P < .05 was considered statistically significant.
Results
Search Results and Study Characteristics
Study characteristics and demographic data are summarized in Table 1 and eTable 3 in the Supplement, respectively.19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65 The initial search yielded 3871 studies, with 162 additional studies identified through citations (eFigure 1 in the Supplement). After screening titles and abstracts, 2309 articles were excluded, and 58 full-text articles were assessed for eligibility. Forty-seven studies, with 26 547 participants, were included. Mean (SD) age and BMI among participants were 50 (5) years and 32 (3), respectively, with 16 780 (65%) men. Reasons for article exclusion are listed in eTable 2 in the Supplement. Results of internal and external study validity assessment are presented in eTable 4 and eTable 5 in the Supplement. Included studies showed low to moderate risk of bias after validity assessment and were used to answer our review question. Studies were organized into 6 groups: (1) North America (9 studies,19,20,21,22,23,24,25,26,27 3507 participants); (2) South America (6 studies,28,29,30,31,32,33 10 709 participants); (3) Europe (10 studies,34,35,36,37,38,39,40,41,42,43 5679 participants); (4) the Middle East (11 studies,44,45,46,47,48,49,50,51,52,53,54 3468 participants); (5) East Asia (4 studies,55,56,57,58 1665 participants); and (6) South or Southeast Asia (7 studies,59,60,61,62,63,64,65 1519 participants).
Table 1. Demographic Data of Patients Using STOP-Bang Questionnaire.
| Source | Study location | Sample size | Study type | Validation tool | Age, mean (SD), y | Men, No. (%) | Mean (SD) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI | Neck circumference, cm | STOP-Bang score | AHI, events/h | Minimum Spo2 (%) | |||||||
| North America | |||||||||||
| Boynton et al,19 2013 | US | 219 | Prospective | Laboratory PSG | 46 (14) | 99 (45) | 33 (9) | 40 (5) | 4 (2) | NR | NR |
| Farney et al,20 2011 | US | 1424 | Retrospective | Laboratory PSG | 50 (15) | 812 (57) | 34 (8) | 41 (5) | 4 (2) | 32 (30) | NR |
| McMahon et al,21 2017 | US | 338 | Retrospective | Laboratory PSG | 40 (10) | 257 (76) | 29 (4) | 40 (9) | 4 (1) | 13 (16) | NR |
| Miller et al,22 2018 | US | 142 | Cross-sectional | HSAT (ApneaLink Air) and Laboratory PSG | 55 (15) | 74 (52) | NR | NR | NR | NR | NR |
| Mou et al,23 2019 | US | 935 | Prospective | Laboratory PSG | NR | 533 (57) | 36 (10) | NR | 5 (2) | NR | NR |
| Orbea et al,24 2020 | US | 66 | Retrospective | HSAT and Laboratory PSG | 54 (6) | 0 | 33 (8) | NR | 3 (1) | 8 (8) | NR |
| Pereira et al,25 2013 | Canada | 128 | Prospective | HSAT (Sandman Elite SD32+) | 50 (12) | 84 (66) | 31 (7) | 41 (4) | NR | 33 (28) | NR |
| Sangkum et al,26 2017 | US | 208 | Cross-sectional | Laboratory PSG | 53 (1) | 75 (36) | 37 (1) | 41 (0) | NR | 19 (22) | NR |
| Vana et al,27 2013 | US | 47 | Cross-sectional | Laboratory PSG | 46 (13) | 16 (34) | 36 (9) | 38 (5) | 5 (2) | 29 (23) | NR |
| South America | |||||||||||
| Andrade et al,28 2020 | Brazil | 35 | Cross-sectional | Laboratory PSG | NR | 17 (49) | 33 (5) | 40 (5) | NR | 36 (27) | NR |
| Baldini et al,29 2017 | Argentina | 327 | Retrospective | Laboratory PSG | 50 | 170 (52) | 39 | 44 | NR | NR | NR |
| Duarte et al,30 2017 | Brazil | 456 | Prospective | Laboratory PSG | 43 (13) | 292 (64) | 32 (8) | 41 (4) | 4 (2) | 25 (25) | NR |
| Duarte et al,31 2020 | Brazil | 7377 | Cross-sectional | Laboratory PSG | 46 (15) | 3984 (54) | 33 (8) | 41 (5) | NR | 28 (28) | 82 (9) |
| Saldias Peñafiel et al,32 2018 | Chile | 1050 | Prospective | HSAT (Embletta Gold, Embletta MPR) | 56 (15) | 714 (68) | 31 (6) | 42 (4) | NR | 26 (22) | 79 (10) |
| Saldias Peñafiel et al,33 2019 | Chile | 1464 | Prospective | Laboratory PSG | 54 (15) | 951 (65) | 31 (6) | 41.6 (4) | NR | NR | NR |
| Europe | |||||||||||
| Bille et al,34 2015 | Denmark | 43 | Prospective | HSAT | 54 (14) | 34 (79) | 29 | NR | 5 | 13 | NR |
| Christensson et al,35 2018 | Sweden | 449 | Prospective | HSAT (Embletta, NOX T3) | 54 (14) | 274 (61) | 30 (6) | NR | 4 (1) | 12 (15) | NR |
| Cowan et al,36 2014 | UK | 129 | Prospective | HSAT (SOMNOmedics) | 49 (11) | 83 (64) | 33 (2) | NR | NR | NR | NR |
| Kørvel-Hanquist et al,37 2018 | Denmark | 208 | Prospective | HSAT (NOX T3) | 53 (13) | 152 (73) | 35 (8) | NR | 5 (1) | 35 (20) | NR |
| Kuczyński et al,38 2019 | Poland | 1123 | Retrospective | Laboratory PSG | 52 (12) | 842 (75) | 32 (6) | NR | NR | 20 (6) | NR |
| Pataka et al,39 2014 | Greece | 1853 | Retrospective | Laboratory PSG | 52 (14) | 1371 (74) | 33 (7) | 42 (4) | 5 (2) | 33 (27) | NR |
| Pataka et al,40 2019 | Greece | 700 | Retrospective | Laboratory PSG | 60 (11) | 455 (65) | 35 (8) | 42 (8) | 5 (2) | 34 (24) | NR |
| Pataka et al,41 2020 | Greece | 700 | Prospective | Laboratory PSG | 53 (14) | 350 (50) | 30 (9) | 39 (11) | 4 (1) | 25 (24) | NR |
| Rebelo-Marques et al,42 2018 | Portugal | 259 | Prospective | HSAT (NOX T3, Stardust II, Embletta X100, Alice PDx); Laboratory PSG | 55 (12) | 184 (71) | 31 (5) | 41 (3) | 5 (2) | 39 (18) | NR |
| Reis et al,43 2015 | Portugal | 215 | Prospective | Laboratory PSG | 54 (13) | 135 (63) | 29 | 40 (4) | 4 (2) | 16.7 | NR |
| Middle East | |||||||||||
| Acar et al,44 2013 | Turkey | 110 | Prospective | Laboratory PSG | 44 (12) | 103 (94) | 30 (4) | NR | NR | 28 (25) | NR |
| Alhouqani et al,45 2015 | United Arab Emirates | 193 | Prospective | Laboratory PSG | 43 (12) | 151 (78) | 35 (9) | 40 (4) | NR | 35 (31) | 78 (13) |
| Amra et al,46 2018 | Iran | 400 | Cross-sectional | Laboratory PSG | 50 (10) | 236 (59) | 32 (7) | 41 (3) | NR | NR | NR |
| Arslan et al,47 2020 | Turkey | 1003 | Cross-sectional | Laboratory PSG | 51 (11) | 702 (70) | NR | NR | NR | NR | NR |
| Avincsal et al,48 2017 | Turkey | 162 | Retrospective | Laboratory PSG | 50 (1) | 113 (70) | 34 (0) | 41 (0) | NR | 39 (63) | NR |
| BaHammam et al,49 2015 | Saudi Arabia | 100 | Prospective | Laboratory PSG | 47 (14) | 61 (61) | 34 (8) | 38 (4) | 4 (2) | 50 (37) | NR |
| Bingol et al,50 2016 | Turkey | 196 | Prospective | Laboratory PSG | NR | 90 (46) | NR | NR | NR | NR | NR |
| El-Sayed,51 2012 | Egypt | 234 | Prospective | Laboratory PSG | 50 (11) | 199 (85) | 38 (10) | 42 (4) | 6 (2) | 46 (33) | NR |
| Kashaninasab et al,52 2017 | Iran | 250 | Cross-sectional | Laboratory PSG | 48 (12) | 190 (76) | NR | 40 (4) | NR | 44 (3) | NR |
| Mergen et al,53 2019 | Turkey | 217 | Retrospective | Laboratory PSG | 50 (10) | 158 (73) | 36 (4) | 43 (3) | NR | NR | NR |
| Sadeghniiat-Haghighi et al,54 2015 | Iran | 603 | Cross-sectional | Laboratory PSG | 46 (13) | 452 (75) | 29 (6) | 40 (4) | 4 (1) | NR | 70 (28) |
| East Asia | |||||||||||
| Byun et al,55 2020 | South Korea | 778 | Cross-sectional | Laboratory PSG | 49 (13) | 591 (76) | 27 (4) | 38 (4) | NR | 28 (39) | 80 (11) |
| Hu et al,56 2019 | China | 196 | Prospective | Laboratory PSG | NR | 161 (82) | 27 (4) | 40 (4) | 4 (2) | 48 (22) | NR |
| Luo et al,57 2014 | China | 212 | Prospective | Laboratory PSG | 45 (12) | 189 (89) | 28 (4) | 41 (3) | 4 (1) | 44 (28) | 74 (13) |
| Peng et al,58 2018 | China | 479 | Retrospective | Laboratory PSG | 49 (14) | 373 (78) | 26 (4) | 37 (4) | 3 (1) | 20 (23) | 80 (14) |
| South or Southeast Asia | |||||||||||
| Abdullah et al,59 2018 | Malaysia | 134 | Cross-sectional | Laboratory PSG | 41 (13) | 84 (63) | NR | NR | NR | NR | NR |
| Banhiran et al,60 2014 | Thailand | 303 | Cross-sectional | Laboratory PSG | NR | 184 (61) | NR | NR | NR | NR | NR |
| Chakrabarti et al,61 2019 | India | 80 | Retrospective | Laboratory PSG | 49 (112) | 57 (71) | 28 (5) | NR | 5 (1) | 34 (23) | NR |
| Loh et al,62 2018 | Singapore | 591 | Retrospective | Laboratory PSG | 46 (14) | 437 (74) | 28 (6) | 40 (4) | NR | 25 (29) | NR |
| Ong et al,63 2010 | Singapore | 319 | Prospective | Laboratory PSG | 47 (15) | 226 (71) | 28 (6) | 40 (4) | 4 (2) | 26 (27) | 82 (13) |
| Perumalsamy et al,64 2017 | India | 62 | Cross-sectional | Laboratory PSG | 53 (12) | 37 (60) | NR | NR | NR | NR | NR |
| Vulli et al,65 2019 | India | 35 | Prospective | Laboratory PSG | 54 (6) | 28 (80) | 35 (3) | 41 (1) | NR | NR | NR |
Abbreviations: AHI, apnea-hypopnea index; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HSAT, home sleep apnea testing; NR, not reported; PSG, polysomnography; Spo2, oxyhemoglobin saturation.
Test Characteristics of the STOP-Bang Questionnaire in All Included Studies
The combined test characteristics in the sleep clinic at a STOP-Bang threshold of 3 or greater are presented in Figure 1, Table 2, and eFigure 2 in the Supplement. The prevalence rates of all OSA, moderate to severe OSA, and severe OSA were 80% (95% CI, 80%-81%), 58% (95% CI, 58%-59%), and 39% (95% CI, 38%-39%), respectively. A STOP-Bang score of at least 3 had excellent sensitivity (combined sensitivity, 91.4; 95% CI, 86.4-94.6) to detect all severities of OSA. The false-negative rate was 8% (6%-11%). Moreover, the STOP-Bang questionnaire demonstrated a high discriminative power, indicated by NPVs, to exclude moderate to severe (77%, 95% CI, 75%-78%) and severe (91%, 95% CI, 90%-92%) OSA. Moderately low specificity was seen, with 28% (95% CI, 22%-34%) for moderate to severe OSA and 24% (95% CI, 19%-30%) for severe OSA.
Figure 1. Forest Plot for Combined Sensitivity and Specificity for All Obstructive Sleep Apnea for All Included Studies in the Sleep Clinic.
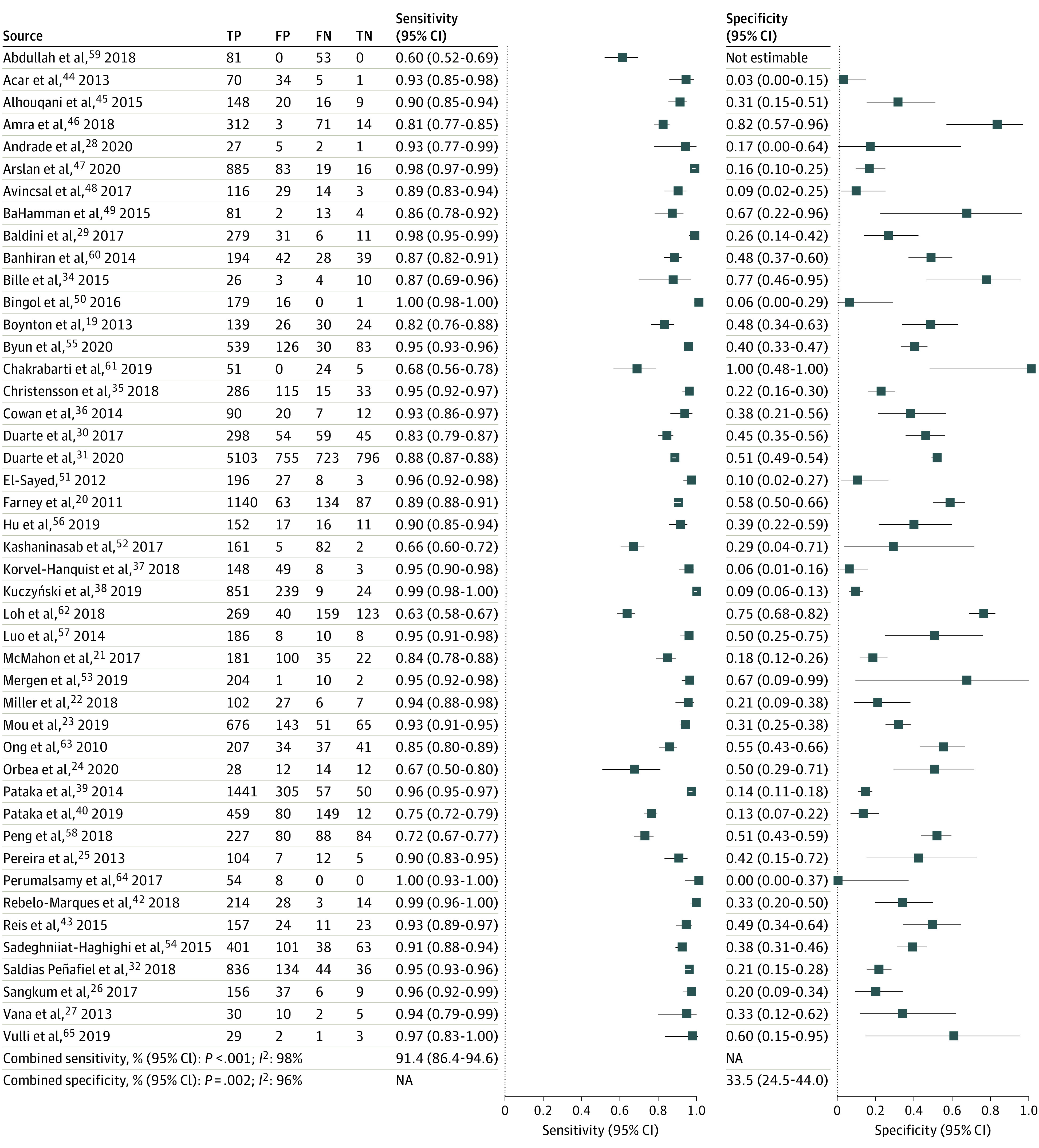
FN indicates false-negative; FP, false-positive; NA, not applicable; TN, true-negative; TP, true-positive.
Table 2. Combined Test Characteristics of a STOP-Bang Score of 3 or Greater.
| Test characteristic | All OSA, ie, AHI ≥5, % (95% CI) | Moderate to severe OSA, ie, AHI ≥15, % (95% CI) | Severe OSA, ie, AHI ≥30, % (95% CI) |
|---|---|---|---|
| All regions | |||
| Studies, No. (participants, No.) | 45 (24 192) | 38 (23 811) | 29 (17 984) |
| Prevalence | 80 (80 to 81) | 58 (58 to 59) | 39 (38 to 39) |
| Sensitivity | 92 (89 to 94) | 95 (93 to 96) | 97 (95 to 98) |
| Specificity | 33 (26 to 41) | 28 (22 to 34) | 24 (19 to 30) |
| PPV | 86 (85 to 86) | 66 (65 to 66) | 46 (45 to 47) |
| NPV | 47 (45 to 49) | 77 (75 to 78) | 91 (90 to 92) |
| Log scale DOR (95% CI) | 1.74 (0.88 to 2.59) | 1.91 (1.62 to 2.21) | 2.08 (1.72 to 2.43) |
| AUC (95% CI) | 0.76 (0.72 to 0.80) | 0.76 (0.72 to 0.80) | 0.72 (0.68 to 0.76) |
| North America | |||
| Studies, No. (participants, No.) | 9 (3507) | 9 (3507) | 8 (3460) |
| Prevalence | 81 (80 to 82) | 54 (53 to 56) | 32 (31 to 34) |
| Sensitivity | 90 (84 to 93) | 94 (93 to 96) | 96 (94 to 97) |
| Specificity | 34 (24 to 45) | 24 (18 to 33) | 20 (14 to 27) |
| PPV | 86 (84 to 87) | 60 (58 to 62) | 36 (34 to 38) |
| NPV | 45 (41 to 49) | 78 (74 to 81) | 91 (88 to 93) |
| Log scale DOR (95% CI) | 1.21 (–0.81 to 3.24) | 1.93 (1.40 to 2.47) | 1.59 (1.12 to 2.07) |
| AUC (95% CI) | 0.72 (0.68 to 0.76) | 0.89 (0.85 to 0.91) | 0.89 (0.86 to 0.91) |
| South America | |||
| Studies, No. (participants, No.) | 5 (9245) | 4 (9624) | 3 (8160) |
| Prevalence | 80 (79 to 81) | 58 (57 to 59) | 37 (36 to 38) |
| Sensitivity | 93 (87 to 96) | 96(91 to 98) | 96 (96 to 97) |
| Specificity | 33 (21 to 48) | 25(15 to 38) | 30 (28 to 31) |
| PPV | 87 (86 to 88) | 66 (65 to 67) | 44 (43 to 46) |
| NPV | 52 (49 to 54) | 78 (76 to 80) | 93 (92 to 94) |
| Log scale DOR, 95% CI | 4.09 (1.18 to 7.00) | 1.62 (1.27 to 1.97) | 2.36 (2.16 to 2.55) |
| AUC, 95% CIa | 0.76 (0.72 to 0.79) | 0.74 | 0.66 |
| Europe | |||
| Studies, No. (participants, No.) | 9 (4979) | 10 (5679) | 6 (3278) |
| Prevalence | 79 (78 to 80) | 60 (58 to 61) | 46 (45 to 48) |
| Sensitivity | 95 (90 to 97) | 97 (93 to 99) | 99 (97 to 99) |
| Specificity | 24 (13 to 39) | 25 (14 to 40) | 22 (12 to 36) |
| PPV | 81 (80 to 82) | 67 (66 to 69) | 56 (54 to 58) |
| NPV | 41 (36 to 46) | 78 (75 to 81) | 96 (94 to 98) |
| Log scale DOR, 95% CI | 2.81 (1.03 to 4.59) | 1.93 (1.60 to 2.26) | 3.00 (1.99 to 4.01) |
| AUC, 95% CI | 0.78 (0.74 to 0.81) | 0.81 (0.78 to 0.84) | 0.96 (0.93 to 0.97) |
| Middle East | |||
| Studies, No. (participants, No.) | 11 (3468) | 7 (2545) | 6 (1542) |
| Prevalence | 87 (86 to 88) | 67 (65 to 68) | 48 (46 to 51) |
| Sensitivity | 93 (87 to 96) | 95 (89 to 98) | 94 (85 to 98) |
| Specificity | 24 (12 to 44) | 28 (13 to 50) | 33 (17 to 54) |
| PPV | 90 (88 to 91) | 71 (69 to 73) | 55 (52 to 57) |
| NPV | 30 (26 to 35) | 66 (61 to 72) | 78 (73 to 83) |
| Log scale DOR, 95% CI | 0.75 (–1.27 to 2.78) | 2.24 (1.11 to 3.37) | 1.96 (1.48 to 2.45) |
| AUC, 95% CI | 0.77 (0.73 to 0.80) | 0.83 (0.79 to 0.86) | 0.78 (0.74 to 0.81) |
| East Asia | |||
| Studies, No. (participants, No.) | 4 (1665) | 4 (1665) | 3 (887) |
| Prevalence | 75 (73 to 77) | 56 (54 to 59) | 40 (37 to 43) |
| Sensitivity | 90 (81 to 96) | 93(84 to 97) | 90 (87 to 93) |
| Specificity | 44 (37 to 50) | 33 (27 to 41) | 30 (26 to 34) |
| PPV | 83 (81 to 85) | 64 (62 to 67) | 46 (43 to 50) |
| NPV | 56 (51 to 62) | 76 (71 to 81) | 82 (76 to 87) |
| Log scale DOR, 95% CI | 1.38 (–0.19 to 2.97) | 2.01 (1.24 to 2.77) | 1.89 (0.74 to 3.03) |
| AUC. 95% CIa | 0.56 (0.52 to 0.60) | 0.52 (0.48 to 0.56) | 0.41 |
| South or Southeast Asia | |||
| Studies, No. (participants, No.) | 7 (1519) | 4 (791) | 3 (657) |
| Prevalence | 75 (73 to 78) | 56 (52 to 59) | 34 (30 to 38) |
| Sensitivity | 81 (68 to 89) | 89 (73 to 96) | 96(93 to 98) |
| Specificity | 60 (46 to 73) | 45 (30 to 61) | 33 (28 to 37) |
| PPV | 86 (84 to 89) | 65 (61 to 69) | 42 (38 to 47) |
| NPV | 46 (41 to 51) | 70 (63 to 76) | 95 (89 to 98) |
| Log scale DOR, 95% CI | 1.36 (0.21 to 2.52) | 2.04 (1.12 to 2.96) | 2.54 (1.91 to 3.17) |
| AUC, 95% CIa | 0.76 (0.72 to 0.80) | 0.70 (0.66 to 0.74) | 0.89 |
Abbreviations: AHI, apnea-hypopnea index; AUC, area under the summary receiver operating characteristic curve; DOR, diagnostic odds ratio; NPV, negative predictive value; OSA, obstructive sleep apnea; PPV, positive predictive value.
For groups with fewer than 5 studies, 95% CIs for AUC values are not reported due to software output.
Test Characteristics of the STOP-Bang Questionnaire for All OSA in Different Geographic Regional Groups
For all OSA, the combined prevalence ranged between 75% (95% CI, 73%-77%) in East Asia and 87% (95% CI, 86%-88%) in the Middle East (Table 2; eFigure 3 and eTable 6 in the Supplement). The combined sensitivities were excellent in all regions (>90%) and combined specificity values were moderately low, except in South or Southeast Asia (sensitivity: 81%; 95% CI, 68%-89%; specificity: 60%; 95% CI, 46%-73%). Similarly, PPVs were consistently high among all regional groups, ranging between 81% (95% CI, 80%-82%) in Europe and 87% (95% CI, 86%-88%) in South America. The AUC curves ranged between 0.72 (95% CI, 0.68-0.76) in North America and 0.78 (95% CI, 0.74-0.81) in Europe, with an exception in East Asia (0.56; 95% CI, 0.52-0.60).
Test Characteristics of the STOP-Bang Questionnaire for Moderate to Severe OSA in Different Geographic Regional Groups
For moderate to severe OSA, the STOP-Bang questionnaire demonstrated an excellent combined sensitivity (>93%; eg, North America, 94%; 95% CI, 93%-96%) and low specificity (<33%) in North America, South America, Europe, and the Middle East. In East Asian, sensitivity was 93% (95% CI, 84%-97%); in South or Southeast Asia, sensitivity was 89% (95% CI, 73%-96%). In South or Southeast Asia, specificity was 45% (95% CI, 30%-61%) (Table 2; eFigure 3 and eTable 6 in the Supplement). A STOP-Bang score of at least 3 had a moderate discriminative power to exclude moderate to severe OSA, with NPVs ranging between 66% (95% CI, 65%-67%) in South America and 78% (95% CI, 74%-81%) in North America. DOR values were comparable across groups for moderate to severe OSA, ranging from 1.62 (95% CI, 1.27-197) in South America to 2.24 (95% CI, 1.11-3.37) in the Middle East. The diagnostic accuracy of a STOP-Bang score of at least 3 to detect moderate to severe OSA indicated by the AUC curve was high in North America, Europe, and the Middle East (eg, North America: 0.89; 95% CI, 0.85-0.91) but lower in the East Asian (0.52; 95% CI, 0.48-0.56) and South or Southeast Asian (0.70; 95% CI, 0.66-0.74) groups.
Test Characteristics of the STOP-Bang Questionnaire for Severe OSA in Geographic Regional Groups
The STOP-Bang questionnaire demonstrated an excellent combined sensitivity, ranging between 90% (95% CI, 87%-93%) in East Asia and 99% (95% CI, 97%-99%) in Europe, with lower combined specificities (Table 2; eFigure 3 and eTable 6 in the Supplement). The STOP-Bang questionnaire demonstrated a high discriminative power to exclude severe OSA in all regional groups, as NPVs ranged between 82% (95% CI, 76%-87%) in East Asia and 96% (95% CI, 94%-98%) in Europe. The AUC curve value was highest in the European group (0.96, 95% CI, 0.93-0.97).
Metaregression and Sensitivity Analysis of Various Subgroups
Metaregression and sensitivity analysis of continuous variables slightly changed the combined estimates but did not affect overall inference of the results (Table 3; eTable 7 in the Supplement). Similarly, analysis of the categorical variables slightly changed the combined estimates but did not impact the final inference of our results. Leave-one-out meta-analysis showed no individual study greatly affected the results.
Table 3. Metaregression and Sensitivity Analysis of the STOP-Bang Questionnaire for Various Subgroups According to the Severity of OSA.
| Covariate (studies, No.) | Sensitivity | Log scale diagnostic odds ratio | ||||||
|---|---|---|---|---|---|---|---|---|
| Point estimate (95% CI) | I2, % | Coefficient (SE) | P value | Point estimate (95% CI) | I2, % | Coefficient (SE) | P value | |
| Apnea-hypopnea index ≥5 (45) | ||||||||
| Age (42) | 91.0 (85.6 to 94.5) | 98 | 0.064 (0.057) | .26 | 1.72 (0.82 to 2.62) | 98 | 0.115 (0.105) | .28 |
| Gender (45) | 91.4 (86.4 to 94.6) | 98 | –0.010 (0.014) | .46 | 1.74 (0.88 to 2.59) | 97 | –0.022 (0.024) | .36 |
| BMI (41) | 91.1 (85.7 to 94.6) | 98 | 0.109 (0.075) | .15 | 1.71 (0.79 to 2.64) | 98 | 0.171 (0.142) | .23 |
| Neck circumference (34) | 90.2 (83.6 to 94.3) | 98 | 0.34 (0.191) | .07 | 1.52 (0.47 to 2.57) | 98 | 0.505 (0.378) | .18 |
| Sample size | ||||||||
| >200 (30) | 89.6 (82.2 to 94.1) | 98 | –0.425 (0.482) | .38 | 1.28 (0.25 to 2.31) | 98 | –1.453 (0.839) | .08 |
| <200 (15) | 94.1 (87.6 to 97.3) | 95 | NA | NA | 2.77 (1.37 to 4.16) | 91 | NA | NA |
| Study type | ||||||||
| Prospective (19) | 93.6 (87.9 to 96.7) | 97 | NA | NA | 2.18 (0.71 to 3.64) | 98 | NA | NA |
| Retrospective (12) | 85.5 (74.6 to 92.2) | 98 | 0.779 (0.564) | .17 | 0.85 (–0.48 to 2.20) | 97 | 1.646 (0.965) | .09 |
| Cross-sectional (14) | 91.9 (79.4 to 97.1) | 99 | –0.403 (0.594) | .50 | 1.87 (0.52 − 3.23) | 96 | –0.526 (1.033) | .61 |
| Validation tool | ||||||||
| Lab PSG (39) | 91.2 (85.7 to 94.8) | 98 | –0.990 (0.792) | .21 | 1.79 (0.84 to 2.73) | 98 | –2.732 (1.373) | .047 |
| HSAT (6) | 92.1 (80.6 to 97.1) | 94 | NA | NA | 1.45 (–0.36 to 3.27) | 92 | NA | NA |
| OSA criteria | ||||||||
| AHI ≥5 (44) | 91.1 (85.9 to 94.5) | 98 | 0.734 (1.651) | .66 | 1.71 (0.84 to 2.58) | 97 | –0.311 (2.791) | .91 |
| RDI ≥5 (1)a | 97.9 (95.4 to 99.1) | NA | NA | NA | NA | NA | NA | |
| Prevalence (45) | 91.4 (86.4 to 94.6) | 98 | 0.003 (0.025) | .92 | 1.74 (0.88 to 2.59) | 97 | –0.013 (0.045) | .78 |
| Region | ||||||||
| North America (9) | 85.7 (70.7 to 93.7) | 97 | NA | NA | 1.21 (–0.81 to 3.24) | 97 | NA | NA |
| South America (5) | 97.8 (95.0 to 99.1) | 91 | 0.149 (0.698) | .83 | 4.09 (1.18 to 7.00) | 98 | 0.011(1.225) | .99 |
| Europe (9) | 95.7 (88.4 to 98.5) | 97 | 1.890 (0.883) | .03 | 2.81 (1.03 to 4.59) | 96 | 2.529 (1.542) | .10 |
| Middle East (11) | 91.2 (73.9 to 97.4) | 99 | 1.489 (0.733) | .04 | 0.75 (–1.27 to 2.78) | 96 | 1.973 (1.284) | .12 |
| East Asia (4) | 82.7 (57.5 to 94.4) | 98 | 0.308 (0.689) | .66 | 1.38 (–0.19 to 2.97) | 96 | –1.248 (1.231) | .31 |
| South/Southeast Asia (7) | 83.8 (72.5 to 91.0) | 92 | 0.167 (0.871) | .85 | 1.36 (0.21 to 2.52) | 87 | 0.234 (1.518) | .88 |
| Apnea-hypopnea index ≥15 (38) | ||||||||
| Age (35) | 94.4 (92.3 to 96.0) | 94 | 0.064 (0.043) | .13 | 1.92 (1.60 to 2.25) | 88 | –0.014 (0.038) | .71 |
| Gender (38) | 94.4 (92.4 to 95.8) | 93 | 0.021 (0.015) | .166 | 1.91 (1.62 to 2.21) | 87 | 0.011 (0.015) | .44 |
| BMI (33) | 94.4 (92.4 to 95.9) | 93 | 0.025 (0.053) | .65 | 1.95 (1.62 to 2.28) | 88 | –0.007 (0.049) | .89 |
| Neck circumference (26) | 94.3 (92.1 to 95.9) | 93 | 0.040 (0.048) | .41 | 1.96 (1.58 to 2.34) | 91 | 0.018 (0.054) | .73 |
| Sample size | ||||||||
| >200 (27) | 94.9 (92.9 to 96.4)94 | 94 | 0.345 (0.416) | .41 | 1.93 (1.60 to 2.26) | 89 | –0.029 (0.412) | .94 |
| <200 (11) | 92.5 (84.8 to 96.5) | 87 | NA | NA | 1.90 (1.19 to 2.61) | 68 | NA | NA |
| Study type | ||||||||
| Prospective (19) | 95.5 (92.5 to 97.3) | 91 | NA | NA | 1.95 (1.70 to 2.20) | 96 | NA | NA |
| Retrospective (9) | 93.2 (87.2 to 96.5) | 95 | –0.022 (0.405) | .96 | 1.51 (0.44 to 2.59) | 96 | –0.037 (0.393) | .92 |
| Cross-sectional (10) | 93.5 (87.6 to 96.7) | 95 | –0.527 (0.534) | .32 | 2.01 (1.77 to 2.24) | 25 | –0.700 (0.526) | .18 |
| Validation tool | ||||||||
| Lab PSG (33) | 94.0 (91.7 to 95.6) | 94 | 0.418 (0.720) | .56 | 1.89 (1.57 to 2.20) | 88 | –0.106 (0.710) | .88 |
| HSAT (5) | 96.6 (93.5 to 98.3) | 24 | NA | NA | 2.04 (1.41 to 2.67) | 0 | NA | NA |
| OSA criteria | ||||||||
| AHI≥5 (37) | 94.1 (92.1 to 95.7) | 93 | 2.652 (1.255) | .04 | 1.89 (1.60 to 2.19) | 87 | 1.827 (1.227) | .14 |
| RDI≥5 (1)a | 99.1 (96.4 to 99.8)- | NA | NA | NA | NA | NA | NA | NA |
| Prevalence (38) | 94.4 (92.4 to 95.8) | 93 | 0.005 (0.018) | .76 | 1.91 (1.62 to 2.21) | 87 | 0.015 (0.015) | .33 |
| Region | ||||||||
| North America (9) | 93.5 (91.4 to 95.1) | 36 | NA | NA | 1.62 (1.27 to 1.97) | 36 | NA | NA |
| South America (4) | 95.4 (90.6 to 97.8) | 93 | 1.354 (0.670) | .04 | 1.93 (1.60 to 2.26) | 48 | 0.174 (0.647) | .79 |
| Europe (10) | 96.5 (91.8 to 98.5) | 96 | 0.810 (0.701) | .25 | 2.24 (1.11 to 3.37) | 95 | –0.017 (0.660) | .98 |
| Middle East (7) | 94.9 (86.7 to 98.2) | 95 | 1.362 (0.689) | .048 | 2.01 (1.24 to 2.77) | 78 | 0.585 (0.662) | .38 |
| East Asia (4) | 93.2 (78.4 to 98.1) | 95 | 0.904 (0.574) | .12 | 2.04 (1.12 to 2.96) | 87 | 0.087(0.565) | .88 |
| South/Southeast Asia (4) | 88.5 (66.8 to 96.7) | 93 | 0.612 (0.679) | .37 | 1.93 (1.40 to 2.47) | 28 | 0.655 (1.831) | .91 |
| Apnea-hypopnea index ≥30 (29) | ||||||||
| Age (26) | 95.6 (93.0 to 97.2)89 | 89 | 0.053 (0.052) | .31 | 2.07 (1.67 to 2.47) | 79 | 0.031 (0.044) | .49 |
| Gender (29) | 95.7 (93.5 to 97.1) | 88 | 0.029 (0.015) | .05 | 2.08 (1.72 to 2.43) | 77 | 0.013 (0.013) | .32 |
| BMI (26) | 95.9 (93.8 to 97.3) | 86 | 0.094 (0.065) | .15 | 2.08 (1.69 to 2.48) | 79 | 0.057 (0.059) | .33 |
| Neck circumference (23) | 95.8 (93.3 to 97.3) | 90 | 0.600 (0.124) | <.001 | 2.15 (1.75 to 2.55) | 80 | 0.340 (0.128) | .008 |
| Sample size | ||||||||
| >200 (20) | 96.4 (94.3 to 97.8) | 89 | 0.013 (0.977) | .28 | 2.20 (1.77 to 2.63) | 82 | –0.086 (0.359) | .81 |
| <200 (9) | 92.9 (84.1 to 97.0) | 78 | NA | NA | 1.72 (1.26 to 2.18) | 0 | NA | NA |
| Study type | ||||||||
| Prospective (15) | 96.5 (93.4 to 98.2) | 78 | NA | NA | 2.12 (1.81 to 2.44) | NA | NA | NA |
| Retrospective (8) | 94.2 (86.1 to 97.7) | 93 | –0.250 (0.416) | .55 | 1.78 (0.74 to 2.81) | 93 | –0.175 (0.278) | .53 |
| Cross-sectional (6) | 95.8 (89.3 to 98.4) | 92 | –0.181 (0.415) | .66 | 2.31 (2.13 to 2.50) | 0 | 0.235 (0.304) | .44 |
| Validation tool | ||||||||
| Lab PSG (26) | 95.5 (93.1 to 97.1) | 89 | –0.293 (0.815) | .72 | 2.08 (1.71 to 2.46) | 79 | –0.627 (0.708) | .38 |
| HSAT (3) | 97.2 (92.2 to 99.0) | 0 | NA | NA | 1.19 (0.45 to 1.94) | 0 | NA | NA |
| OSA criteria | ||||||||
| AHI ≥5 (28) | 95.5 (93.2 to 97.0) | 88 | 3.177 (1.610) | .048 | 2.06 (1.70 to 2.42) | 77 | 1.714 (1.488) | .25 |
| RDI ≥5 (1)a | 99.7 (95.3 to 1.0)- | NA | NA | NA | NA | NA | NA | NA |
| Prevalence (29) | 95.7 (93.5 to 97.1) | 88 | 0.008 (0.025) | .75 | 2.08 (1.72 to 2.43) | 77 | 0.036 (0.020) | .07 |
| Region | ||||||||
| North America (8) | 94.9 (91.7 to 96.9) | 48 | NA | NA | 1.59 (1.12 to 2.07) | 33 | NA | NA |
| South America (3) | 96.3 (93.5 to 97.9) | 42 | 1.645 (0.583) | .005 | 2.36 (2.16 to 2.55) | 0 | 0.393 (0.463) | .40 |
| Europe (6) | 98.3 (96.9 to 99.1) | 32 | 1.145 (0.583) | .049 | 3.00 (1.99 to 4.01) | 69 | 0.557 (0.364) | .13 |
| Middle East (6) | 93.4 (83.8 to 97.5) | 90 | 2.126 (0.615) | <.001 | 1.96 (1.48 to 2.45) | 30 | 1.738 (0.450) | <.001 |
| East Asia (3) | 93.5 (70.5 to 98.9) | 92 | 0.682 (0.544) | .21 | 1.89 (0.74 to 3.03) | 83 | 0.187 (0.423) | .66 |
| South/Southeast Asia (3) | 96.2 (92.6 to 98.0) | 0 | 0.995 (1.586) | .09 | 2.54 (1.91 to 3.17) | 0 | 0.676 (0.460) | .14 |
Abbreviations: AHI, apnea-hypopnea index; BMI, body mass index; HSAT, home sleep apnea testing; NA, not applicable; OSA, obstructive sleep apnea; PSG, polysomnogram; RDI, respiratory disturbance index.
No heterogeneity or log scale diagnostic odds ratio available for groups with fewer than 5 studies.
Predictive Performance and Predictive Probability of STOP-Bang Scores of 3 to 8
For all OSA, as the STOP-Bang score increased from 3 to 8, the specificity increased from 40.6% (95% CI, 39.3%-42.0%) to 99.7% (95% CI, 99.0%-99.9%), while sensitivity decreased from 89.2% (95% CI, 88.7%-89.6%) to 3.6% (95% CI, 3.0%-4.3%) (eTable 8 in the Supplement). The PPVs and NPVs showed similar trends. This was similar for moderate to severe OSA and severe OSA.
In all included studies, as the STOP-Bang score increased from 3 to 6, the probability of moderate to severe OSA increased from 65% to 75% (Figure 2). Similarly, the probability of having severe OSA with a STOP-Bang score of 3 was 45%, and with a score of 6, it was 57%.
Figure 2. Association Between STOP-Bang Scores of 3 to 8 and Probability of Obstructive Sleep Apnea (OSA).
Discussion
This systematic review and meta-analysis found that the STOP-Bang questionnaire was a useful screening tool to triage patients with suspected OSA in sleep clinics in different geographic regions. Its high sensitivity would help to identify those at risk for all, moderate to severe, and severe OSA, while high NPVs would allow clinicians to rule out severe OSA in individuals with a STOP-Bang score of 2 or less. The AUC was clinically significant at each AHI threshold, indicative of its global screening utility.
The prevalence for all, moderate to severe, and severe OSA at sleep clinics globally was high at 80% (95% CI, 80%-81%), 58% (95% CI, 58%-59%), and 39% (95% CI, 38-39). Patients referred to sleep clinics are already suspected of having OSA, which explains the high prevalence and diagnostic accuracy in our study. In this setting, the STOP-Bang questionnaire fulfills the role of a screening tool that may allocate resource-limited care according to severity. While STOP-Bang scores of 3 to 5 had similar posttest probabilities (ie, 65%-66%), individuals who scored 6 or greater had a 75% posttest probability of being diagnosed with moderate to severe OSA and should be investigated more urgently. The implications of our findings are that the STOP-Bang questionnaire is a helpful tool when triaging patients who were referred to sleep clinics.
Groups were organized relative to country and geographic proximity. Asian countries were separated into East Asia and South or Southeast Asia to minimize external factors that influence OSA prevalence (ie, sleep clinic referral patterns and burden of other comorbidities)2 as well as population-specific anatomic and phenotypic features that influence OSA development and severity. Although OSA is prevalent globally, certain regions report higher prevalences, ie, China, the United States, Brazil, and India.2 These differences influence prevalence-dependent variables, such as pretest and posttest probabilities. We have addressed this by organizing studies based on geography to accurately represent OSA prevalence in each global region. Moreover, DOR values, which are independent of prevalence, were comparable across groups for moderate-to-severe OSA, ranging from 1.62 (95% CI, 1.27-197) in South America to 2.24 (95% CI, 1.11-3.37) in the Middle Eastern group.
The North American group showed a high sensitivity of 94% (95% CI, 93%-96%) and AUC of 0.89 (95% CI, 0.85-0.91) to detect moderate to severe OSA with lower specificities. Similar results were found for the South American, European, and the Middle Eastern groups. Asian groups showed lower sensitivity and AUC values at the same AHI cutoff, ie, 93% (95% CI, 84%-97%) and 0.52 (95% CI, 0.48-0.56) in the East Asian group; 89% (95% CI, 73%-96%) and 0.70 (95% CI, 0.66-0.74) in the South or Southeast Asian group; both groups had higher specificities.
Variation in the STOP-Bang questionnaire performance among these geographic groups may be explained by obesity and craniofacial characteristics. Obesity prevalence and patterns of adiposity vary among ethnic groups. In European, North American, South American, and Asian populations, AHI increases with BMI; however, BMI is most associated with OSA severity in the latter 2 regions.66,67 In Asian populations, higher body fat percentages and visceral fat are associated with a lower BMI.66,68,69 This fat distribution pattern is associated with increased tongue size and lower lung volumes that may contribute to nocturnal upper airway collapse,70 such that Asians present with OSA at lower BMIs and are more sensitive to BMI increases.71 Changing the STOP-Bang BMI cutoff to 30, closer to the obesity cutoff for Asian populations, has shown increases in sensitivity without compromising specificity for OSA detection.57,60,61
The craniofacial features are important in OSA pathogenesis and are unique depending on location. Chinese individuals have a smaller, narrower retropalatal airway and soft tissues with greater susceptibility to pharyngeal collapse.72 Differences are found between ethnic groups, such that Asian populations have more craniofacial restriction,73 while European groups have larger upper airway soft tissues (ie, larger tongue and parapharyngeal fat pads)73 with smaller airway dimensions.14 Similarly, North American and South American populations also showed increased neck circumference, which is associated with greater odds of a higher Mallampati class, indicative of oropharyngeal crowding, while Asian groups do not.66 This may explain the excellent clinical utility seen in each regional group other than the East Asian population. Further research is necessary to investigate the contribution of ethnic and genetic factors to OSA prevalence and severity.
Ideally, a diagnostic test has high sensitivity with sufficient specificity, is inexpensive, and allows for early disease identification. High sensitivity is helpful to rule out OSA and/or to prioritize patients referred to sleep clinics; however, it is an incomplete study estimate, especially in the presence of study heterogeneity and bias. False-negativity is a component of sensitivity that provides a robust summary estimate and may be considered independent of prevalence. In our meta-analysis, the false-negative rate was 8% (6%-11%). Considering specificity may improve accuracy. A moderate to low specificity at a STOP-Bang score of at least 3 may subject patients to false-positive results, increasing unnecessary costs and caseloads at sleep clinics. Nevertheless, with the goal of diagnosing and preventing mortality and morbidity associated with OSA as well as the low risk of investigating potential OSA, false-positives are of secondary importance.
Limitations
This study has limitations. First, included studies used various laboratory PSG and HSAT devices to diagnose OSA. Although often comparable, some inconsistences may exist. Second, risk of bias for internal validity was occasionally unclear, specifically whether PSG and STOP-Bang results were masked and interpreted independent of clinical information. Third, metaregression analysis showed positive confounders contributing to differences between groups, thus enhancing combined estimates of our results. Some confounders were related to components of the STOP-Bang questionnaire (age, sex), while others were not (OSA definition). Next, although the STOP-Bang questionnaire had high NPVs for moderate to severe and severe OSA, it is possible to miss patients with OSA who have lower AHIs because of lower NPVs in patients with mild OSA. Additionally, our results are unique to the sleep clinic and do not apply to other populations owing to inflated OSA prevalence, given that patients were screened before referral for further OSA investigation. Furthermore, moderate-to-high heterogeneity exists. This may be attributed to methodological heterogeneity and variability in study location; however, all studies were grouped with efforts to unify populations. A random-effects model for meta-analysis was performed because of the suspicion of high heterogeneity. Despite these limitations, our study provides an interpretation of the available literature on the STOP-Bang questionnaire as an OSA screening tool among different global populations in the sleep clinic setting.
Conclusions
In this study, the STOP-Bang questionnaire showed high sensitivity and NPVs at all AHI cutoffs. These findings indicate that it is a useful OSA screening tool for triaging patients in sleep clinics in various global regions.
eFigure 1. Study Flow Diagram
eFigure 2. Forest Plot for Combined Sensitivity and Specificity for Moderate to Severe OSA and Severe OSA for All Included Studies in the Sleep Clinic
eFigure 3. Forest Plots for Combined Sensitivity and Specificity for Various OSA Severities in Different Geographic Regional Groups
eTable 1. Search Strategy
eTable 2. Excluded Studies and Reasons for Exclusion
eTable 3. Characteristics of Included Studies
eTable 4. Appraisal of Included Studies Based on Criteria for Internal Validity
eTable 5. Appraisal of Included Studies Based on Criteria for External Validity
eTable 6. Tables Describing the 2 × 2 Contingency Values and Test Characteristics of Individual Studies for All OSA (AHI ≥5), Moderate to Severe OSA (AHI ≥15), and Severe OSA (AHI ≥30)
eTable 7. Specificity Analysis of the STOP-Bang Questionnaire for Various Subgroups According to the Severity of OSA
eTable 8. Test Characteristics of the Various STOP-Bang Score Cutoffs for the Different Severity of Apnea-Hypopnea Index in the Sleep Clinic Setting
References
- 1.Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70-81. doi: 10.1016/j.smrv.2016.07.002 [DOI] [PubMed] [Google Scholar]
- 2.Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687-698. doi: 10.1016/S2213-2600(19)30198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705-706. doi: 10.1093/sleep/20.9.705 [DOI] [PubMed] [Google Scholar]
- 4.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi: 10.1093/aje/kws342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rezaeitalab F, Moharrari F, Saberi S, Asadpour H, Rezaeetalab F. The correlation of anxiety and depression with obstructive sleep apnea syndrome. J Res Med Sci. 2014;19(3):205-210. [PMC free article] [PubMed] [Google Scholar]
- 6.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182(2):269-277. doi: 10.1164/rccm.200911-1746OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung F. Asleep at the controls and a potential problem in flights: is obstructive sleep apnea a public safety concern? Sleep Med. 2020;S1389-9457(20)30375-0. doi: 10.1016/j.sleep.2020.08.016 [DOI] [PubMed] [Google Scholar]
- 8.Marshall NS, Wong KKH, Liu PY, Cullen SRJ, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079-1085. [PMC free article] [PubMed] [Google Scholar]
- 9.Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169(6):668-672. doi: 10.1164/rccm.200308-1124PP [DOI] [PubMed] [Google Scholar]
- 10.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-821. doi: 10.1097/ALN.0b013e31816d83e4 [DOI] [PubMed] [Google Scholar]
- 11.Chung F, Abdullah HR, Liao P. STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149(3):631-638. doi: 10.1378/chest.15-0903 [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Shamseer L, Clarke M, et al. ; PRISMA-P Group . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labarca G, Valdivia G, Oñate A, et al. Prevalence of STOP BANG questionnaire and association with major cardiovascular events in hospitalized population: is it enough with currently used cardiovascular risk measurements? Sleep Med. 2019;61:82-87. doi: 10.1016/j.sleep.2019.02.019 [DOI] [PubMed] [Google Scholar]
- 14.Hnin K, Mukherjee S, Antic NA, et al. The impact of ethnicity on the prevalence and severity of obstructive sleep apnea. Sleep Med Rev. 2018;41:78-86. doi: 10.1016/j.smrv.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 15.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Soft. 2010;1(3):1-48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 16.Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Soft. 2012;49(5):15. doi: 10.18637/jss.v049.i05 [DOI] [Google Scholar]
- 17.Reitsma JB, Glas AS, Rutjes AWS, Scholten RJPM, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58(10):982-990. doi: 10.1016/j.jclinepi.2005.02.022 [DOI] [PubMed] [Google Scholar]
- 18.Walter SD. Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med. 2002;21(9):1237-1256. doi: 10.1002/sim.1099 [DOI] [PubMed] [Google Scholar]
- 19.Boynton G, Vahabzadeh A, Hammoud S, Ruzicka DL, Chervin RD. Validation of the STOP-BANG questionnaire among patients referred for suspected obstructive sleep apnea. J Sleep Disord Treat Care. 2013;2(4). doi: 10.4172/2325-9639.1000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farney RJ, Walker BS, Farney RM, Snow GL, Walker JM. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7(5):459-65B. doi: 10.5664/JCSM.1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McMahon MJ, Sheikh KL, Andrada TF, Holley AB. Using the STOPBANG questionnaire and other pre-test probability tools to predict OSA in younger, thinner patients referred to a sleep medicine clinic. Sleep Breath. 2017;21(4):869-876. doi: 10.1007/s11325-017-1498-1 [DOI] [PubMed] [Google Scholar]
- 22.Miller JN, Kupzyk KA, Zimmerman L, et al. Comparisons of measures used to screen for obstructive sleep apnea in patients referred to a sleep clinic. Sleep Med. 2018;51:15-21. doi: 10.1016/j.sleep.2018.06.007 [DOI] [PubMed] [Google Scholar]
- 23.Mou J, Pflugeisen BM, Crick BA, et al. The discriminative power of STOP-Bang as a screening tool for suspected obstructive sleep apnea in clinically referred patients: considering gender differences. Sleep Breath. 2019;23(1):65-75. doi: 10.1007/s11325-018-1658-y [DOI] [PubMed] [Google Scholar]
- 24.Orbea CAP, Lloyd RM, Faubion SS, Miller VM, Mara KC, Kapoor E. Predictive ability and reliability of the STOP-BANG questionnaire in screening for obstructive sleep apnea in midlife women. Maturitas. 2020;135:1-5. doi: 10.1016/j.maturitas.2020.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pereira EJ, Driver HS, Stewart SC, Fitzpatrick MF. Comparing a combination of validated questionnaires and level III portable monitor with polysomnography to diagnose and exclude sleep apnea. J Clin Sleep Med. 2013;9(12):1259-1266. doi: 10.5664/jcsm.3264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sangkum L, Klair I, Limsuwat C, Bent S, Myers L, Thammasitboon S. Incorporating body-type (apple vs. pear) in STOP-BANG questionnaire improves its validity to detect OSA. J Clin Anesth. 2017;41:126-131. doi: 10.1016/j.jclinane.2016.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vana KD, Silva GE, Goldberg R. Predictive abilities of the STOP-Bang and Epworth Sleepiness Scale in identifying sleep clinic patients at high risk for obstructive sleep apnea. Res Nurs Health. 2013;36(1):84-94. doi: 10.1002/nur.21512 [DOI] [PubMed] [Google Scholar]
- 28.Andrade JdS, Capeloni JRB, Rocha MP, de Souza FX, Barbosa ALG, Brandão AdS. Correlation of clinical aspects and sleep questionnaires with polysonographic findings in patients with obstructive sleep apnea. Article in Portuguese. Revista Eletrônica Acervo Saúde. 2020;12(3):e2851. [Google Scholar]
- 29.Baldini M, Chiapella MN, Fernández MA, Guardia S. STOP-BANG, a useful and easy tool for the screening of obstructive sleep apnea. Article in Spanish. Medicina (B Aires). 2017;77(3):191-195. [PubMed] [Google Scholar]
- 30.Duarte RLM, Fonseca LBM, Magalhães-da-Silveira FJ, Silveira EAD, Rabahi MF. Validation of the STOP-Bang questionnaire as a means of screening for obstructive sleep apnea in adults in Brazil. J Bras Pneumol. 2017;43(6):456-463. doi: 10.1590/s1806-37562017000000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duarte RL, Magalhães-da-Silveira FJ, Oliveira-E-Sá TS, Silva JA, Mello FC, Gozal D. Obstructive sleep apnea screening with a 4-item instrument, named GOAL questionnaire: development, validation and comparative study with No-Apnea, STOP-Bang, and NoSAS. Nat Sci Sleep. 2020;12:57-67. doi: 10.2147/NSS.S238255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saldías Peñafiel F, Gassmann Poniachik J, Canelo López A, Uribe Monasterio J, Díaz Patiño O.. Accuracy of sleep questionnaires for obstructive sleep apnea syndrome screening. Article in Spanish. Rev Med Chil. 2018;146(10):1123-1134. doi: 10.4067/s0034-98872018001001123 [DOI] [PubMed] [Google Scholar]
- 33.Saldías Peñafiel F, Salinas Rossel G, Cortés Meza J, et al. Gender differences in clinical features and performance of sleep questionnaires in adults with obstructive sleep apnea syndrome. Article in Spanish. Rev Med Chil. 2019;147(10):1291-1302. doi: 10.4067/s0034-98872019001001291 [DOI] [PubMed] [Google Scholar]
- 34.Bille J, Bille-Hasselstrøm C, Petersen CG. Translation and validation of the Stop-Bang Questionnaire for obstructive sleep apnoea into Danish. Dan Med J. 2015;62(12):A5158. [PubMed] [Google Scholar]
- 35.Christensson E, Franklin KA, Sahlin C, et al. Can STOP-Bang and pulse oximetry detect and exclude obstructive sleep apnea? Anesth Analg. 2018;127(3):736-743. doi: 10.1213/ANE.0000000000003607 [DOI] [PubMed] [Google Scholar]
- 36.Cowan DC, Allardice G, Macfarlane D, et al. Predicting sleep disordered breathing in outpatients with suspected OSA. BMJ Open. 2014;4(4):e004519. doi: 10.1136/bmjopen-2013-004519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kørvel-Hanquist A, Andersen IG, Lauritzen E, Dahlgaard S, Moritz J. Validation of the Danish STOP-Bang obstructive sleep apnoea questionnaire in a public sleep clinic. Dan Med J. 2018;65(1):A5434. [PubMed] [Google Scholar]
- 38.Kuczyński W, Mokros Ł, Stolarz A, Białasiewicz P. The utility of STOP-BANG questionnaire in the sleep-lab setting. Sci Rep. 2019;9(1):6676. doi: 10.1038/s41598-019-43199-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pataka A, Daskalopoulou E, Kalamaras G, Fekete Passa K, Argyropoulou P. Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic. Sleep Med. 2014;15(7):776-781. doi: 10.1016/j.sleep.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 40.Pataka A, Kalamaras G, Daskalopoulou E, Argyropoulou P. Sleep questionnaires for the screening of obstructive sleep apnea in patients with type 2 diabetes mellitus compared with non-diabetic patients. J Diabetes. 2019;11(3):214-222. doi: 10.1111/1753-0407.12835 [DOI] [PubMed] [Google Scholar]
- 41.Pataka A, Kotoulas S, Kalamaras G, et al. Gender differences in obstructive sleep apnea: the value of sleep questionnaires with a separate analysis of cardiovascular patients. J Clin Med. 2020;9(1):E130. doi: 10.3390/jcm9010130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rebelo-Marques A, Vicente C, Valentim B, et al. STOP-Bang questionnaire: the validation of a Portuguese version as a screening tool for obstructive sleep apnea (OSA) in primary care. Sleep Breath. 2018;22(3):757-765. doi: 10.1007/s11325-017-1608-0 [DOI] [PubMed] [Google Scholar]
- 43.Reis R, Teixeira F, Martins V, et al. Validation of a Portuguese version of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea: analysis in a sleep clinic. Rev Port Pneumol (2006). 2015;21(2):61-68. doi: 10.1016/j.rppnen.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 44.Acar HV, Kaya A, Yücel F, et al. Validation of the STOP-Bang questionnaire: an obstructive sleep apnoea screening tool in Turkish population. Turk J Anaesth Reanim. 2013;41:115-120. Accessed January 28, 2021. https://turkjanaesthesiolreanim.org/en/validation-of-the-stop-bang-questionnaire-an-obstructive-sleep-apnoea-screening-tool-in-turkish-population-13546 [Google Scholar]
- 45.Alhouqani S, Al Manhali M, Al Essa A, Al-Houqani M. Evaluation of the Arabic version of STOP-Bang questionnaire as a screening tool for obstructive sleep apnea. Sleep Breath. 2015;19(4):1235-1240. doi: 10.1007/s11325-015-1150-x [DOI] [PubMed] [Google Scholar]
- 46.Amra B, Javani M, Soltaninejad F, et al. Comparison of Berlin Questionnaire, STOP-Bang, and Epworth Sleepiness Scale for diagnosing obstructive sleep apnea in Persian patients. Int J Prev Med. 2018;9:28. doi: 10.4103/ijpvm.IJPVM_131_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arslan BO, Hoşgör ZZU, Orman MN. Which screening questionnaire is best for predicting obstructive sleep apnea in the sleep clinic population considering age, gender, and comorbidities? Turk Thorac J. 2020;21(6):383-389. doi: 10.5152/TurkThoracJ.2019.19024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Avincsal MO, Dinc ME, Ulusoy S, Dalgic A, Ozdemir C, Develioglu ON. Modified Mallampati score improves specificity of STOP-BANG Questionnaire for obstructive sleep apnea. J Craniofac Surg. 2017;28(4):904-908. doi: 10.1097/SCS.0000000000003513 [DOI] [PubMed] [Google Scholar]
- 49.BaHammam AS, Al-Aqeel AM, Alhedyani AA, Al-Obaid GI, Al-Owais MM, Olaish AH. The validity and reliability of an Arabic version of the STOP-Bang Questionnaire for identifying obstructive sleep apnea. Open Respir Med J. 2015;9:22-29. doi: 10.2174/1874306401509010022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bingol Z, Pıhtılı A, Kıyan E. Modified STOP-BANG questionnaire to predict obesity hypoventilation syndrome in obese subjects with obstructive sleep apnea. Sleep Breath. 2016;20(2):495-500. doi: 10.1007/s11325-015-1213-z [DOI] [PubMed] [Google Scholar]
- 51.El-Sayed IH. Comparison of four sleep questionnaires for screening obstructive sleep apnea. Egyptian J of Chest Dis Tuberc. 2012;61(4):433-441. doi: 10.1016/j.ejcdt.2012.07.003 [DOI] [Google Scholar]
- 52.Kashaninasab F, Alavi K, Farhadi M, Salehi M, Ghaleh Bandi MF. A comparative study of four Persian versions of sleep questionnaires for screening obstructive sleep apnea syndrome (OSAS). Med J Islam Repub Iran. 2017;31:122. doi: 10.14196/mjiri.31.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mergen H, Altındağ B, Zeren Uçar Z, Karasu Kılıçaslan I. The predictive performance of the STOP-Bang questionnaire in obstructive sleep apnea screening of obese population at sleep clinical setting. Cureus. 2019;11(12):e6498. doi: 10.7759/cureus.6498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sadeghniiat-Haghighi K, Montazeri A, Khajeh-Mehrizi A, et al. The STOP-BANG questionnaire: reliability and validity of the Persian version in sleep clinic population. Qual Life Res. 2015;24(8):2025-2030. doi: 10.1007/s11136-015-0923-9 [DOI] [PubMed] [Google Scholar]
- 55.Byun J-I, Kim D-H, Kim J-S, Shin WC. Usefulness of using alternative body-mass index and neck circumference criteria for STOP-Bang questionnaire in screening South Korean obstructive sleep apnea patients. Sleep Med Res. 2020;11(1):38-43. doi: 10.17241/smr.2020.00591 [DOI] [Google Scholar]
- 56.Hu YY, Yu Y, Wang ZB, Liu C, Cui YH, Xiao WM. Reliability and validity of simplified Chinese STOP-BANG questionnaire in diagnosing and screening obstructive sleep apnea hypopnea syndrome. Curr Med Sci. 2019;39(1):127-133. doi: 10.1007/s11596-019-2010-x [DOI] [PubMed] [Google Scholar]
- 57.Luo J, Huang R, Zhong X, Xiao Y, Zhou J. STOP-Bang questionnaire is superior to Epworth Sleepiness Scales, Berlin questionnaire, and STOP questionnaire in screening obstructive sleep apnea hypopnea syndrome patients. Chin Med J (Engl). 2014;127(17):3065-3070. [PubMed] [Google Scholar]
- 58.Peng M, Chen R, Cheng J, Li J, Liu W, Hong C. Application value of the NoSAS score for screening sleep-disordered breathing. J Thorac Dis. 2018;10(8):4774-4781. doi: 10.21037/jtd.2018.07.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdullah B, Idris AI, Mohammad ZW, Mohamad H. Validation of Bahasa Malaysia STOP-BANG questionnaire for identification of obstructive sleep apnea. Sleep Breath. 2018;22(4):1235-1239. doi: 10.1007/s11325-018-1663-1 [DOI] [PubMed] [Google Scholar]
- 60.Banhiran W, Durongphan A, Saleesing C, Chongkolwatana C. Diagnostic properties of the STOP-Bang and its modified version in screening for obstructive sleep apnea in Thai patients. J Med Assoc Thai. 2014;97(6):644-654. [PubMed] [Google Scholar]
- 61.Chakrabarti S, Singh M, Kumar R, Gupta N, Rathi V, Ish P.. Comparison of Epworth Sleepiness Scale and STOP-BANG Questionnaire for diagnosing obstructive sleep apnea at a tertiary care centre in North India: a retrospective study. Indian J of Sleep Med. 2019;14(3):46-50. [Google Scholar]
- 62.Loh JM-R, Toh S-T. Rethinking neck circumference in STOP-BANG for Asian OSA. Proc Singapore Healthcare. 2018;28(2):105-109. doi: 10.1177/2010105818810272 [DOI] [Google Scholar]
- 63.Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu AA. Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath. 2010;14(4):371-376. doi: 10.1007/s11325-010-0350-7 [DOI] [PubMed] [Google Scholar]
- 64.Perumalsamy P, Charles AK, Reddy G, Chokkalingam C, Balakrishnan R. Comparison of three sleep questionnaires in screening obstructive sleep apnea. J Evol Med Dent Sci. 2017;6(88):6132-6136. doi: 10.14260/jemds/2017/1332 [DOI] [Google Scholar]
- 65.Vulli V, Balla P, Vasu P. Predictive ability of STOPBANG scale and Epworth Sleepiness Scale in identifying obstructive sleep apnoea. IOSR J Dent Med Sci. 2019;18(6):1-7. doi: 10.9790/0853-1806160107 [DOI] [Google Scholar]
- 66.Sutherland K, Lee RW, Cistulli PA. Obesity and craniofacial structure as risk factors for obstructive sleep apnoea: impact of ethnicity. Respirology. 2012;17(2):213-222. doi: 10.1111/j.1440-1843.2011.02082.x [DOI] [PubMed] [Google Scholar]
- 67.Hsu PP, Tan AK, Chan YH, Lu PK, Blair RL. Clinical predictors in obstructive sleep apnoea patients with calibrated cephalometric analysis--a new approach. Clin Otolaryngol. 2005;30(3):234-241. doi: 10.1111/j.1365-2273.2005.00983.x [DOI] [PubMed] [Google Scholar]
- 68.Ko GT, Tang J, Chan JC, et al. Lower BMI cut-off value to define obesity in Hong Kong Chinese: an analysis based on body fat assessment by bioelectrical impedance. Br J Nutr. 2001;85(2):239-242. doi: 10.1079/BJN2000251 [DOI] [PubMed] [Google Scholar]
- 69.Lim U, Ernst T, Buchthal SD, et al. Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes. 2011;1(5):e6. doi: 10.1038/nutd.2011.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Van de Graaff WB. Thoracic traction on the trachea: mechanisms and magnitude. J Appl Physiol (1985). 1991;70(3):1328-1336. doi: 10.1152/jappl.1991.70.3.1328 [DOI] [PubMed] [Google Scholar]
- 71.Lyons MM, Bhatt NY, Pack AI, Magalang UJ. Global burden of sleep-disordered breathing and its implications. Respirology. 2020;25(7):690-702. doi: 10.1111/resp.13838 [DOI] [PubMed] [Google Scholar]
- 72.O’Driscoll DM, Landry SA, Pham J, et al. The physiological phenotype of obstructive sleep apnea differs between Caucasian and Chinese patients. Sleep. 2019;42(11):zsz186. doi: 10.1093/sleep/zsz186 [DOI] [PubMed] [Google Scholar]
- 73.Xu L, Keenan BT, Wiemken AS, et al. Differences in three-dimensional upper airway anatomy between Asian and European patients with obstructive sleep apnea. Sleep. 2020;43(5):zsz273. doi: 10.1093/sleep/zsz273 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Study Flow Diagram
eFigure 2. Forest Plot for Combined Sensitivity and Specificity for Moderate to Severe OSA and Severe OSA for All Included Studies in the Sleep Clinic
eFigure 3. Forest Plots for Combined Sensitivity and Specificity for Various OSA Severities in Different Geographic Regional Groups
eTable 1. Search Strategy
eTable 2. Excluded Studies and Reasons for Exclusion
eTable 3. Characteristics of Included Studies
eTable 4. Appraisal of Included Studies Based on Criteria for Internal Validity
eTable 5. Appraisal of Included Studies Based on Criteria for External Validity
eTable 6. Tables Describing the 2 × 2 Contingency Values and Test Characteristics of Individual Studies for All OSA (AHI ≥5), Moderate to Severe OSA (AHI ≥15), and Severe OSA (AHI ≥30)
eTable 7. Specificity Analysis of the STOP-Bang Questionnaire for Various Subgroups According to the Severity of OSA
eTable 8. Test Characteristics of the Various STOP-Bang Score Cutoffs for the Different Severity of Apnea-Hypopnea Index in the Sleep Clinic Setting



