Abstract
Deep venous thrombosis (DVT) of the upper extremities is usually secondary to inflammatory processes, malignancy, immobility from trauma, and inherited or acquired thrombophilias. This is a case of a young man who presented to our facility complaining of upper extremity pain and swelling. Imaging results showed thrombosis in the deep venous system of the left upper extremity, consistent with Paget-Schroetter syndrome.
Keywords: paget-schroetter syndrome, thrombosis, thrombolysis, deep vein thrombosis, dvt
Introduction
Paget-Schroetter syndrome is an acute, effort-induced thrombosis of the deep veins of the upper extremity, occurring after intense physical use such as sporting activities [1]. It makes up 1%-4% of all cases of deep venous thrombosis (DVT) [2]. Usually, there is an anatomical factor which contributes to the etiology and progression of this syndrome, such as, a cervical rib or hypertrophied cervical and upper shoulder muscles. This begins a cascade of endothelial injury with eventual thrombus formation [1]. Upper extremity DVT especially in younger patients should raise suspicion of this syndrome.
Case presentation
A 24-year-old healthy male with no medical history presented to the ED complaining of acute-onset, moderate pain in his left upper extremity, involving his shoulder. This began while he was lifting weights at the gym. He also complained of dependent edema and cyanotic discoloration which improved with elevation of the extremity. He denied any symptoms in the right upper extremity, neck, chest, or head.
His vital signs were stable at presentation. On physical examination, left upper extremity appeared cyanotic with 1+ non-pitting edema. Pulses were intact (2+) and equal on palpation of both radial and brachial arteries. Cyanosis improved with elevation of the left arm. Laboratory findings were within normal limits including a complete blood count and comprehensive metabolic panel. He had a slightly prolonged prothrombin time of 14.4 s (reference range 10.3--12.9 s), and an INR of 1.2 (reference range 0.9-1.1).
A CT-angiogram of his left upper extremity showed no abnormalities, and a venous ultrasound demonstrated extensive acute occlusive DVT of the left subclavian, axillary and brachial veins.
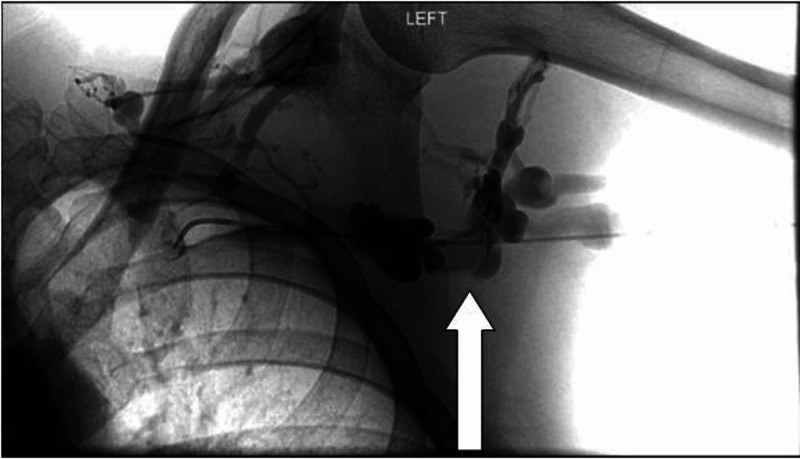
He received systemic anticoagulation with heparin infusion, and also underwent catheter-directed thrombolysis after venography confirmed presence of DVT, as can be seen in Figure 1.
Figure 1. Left upper extremity venogram.
Arrow showing thrombosis in the deep venous system before intervention.
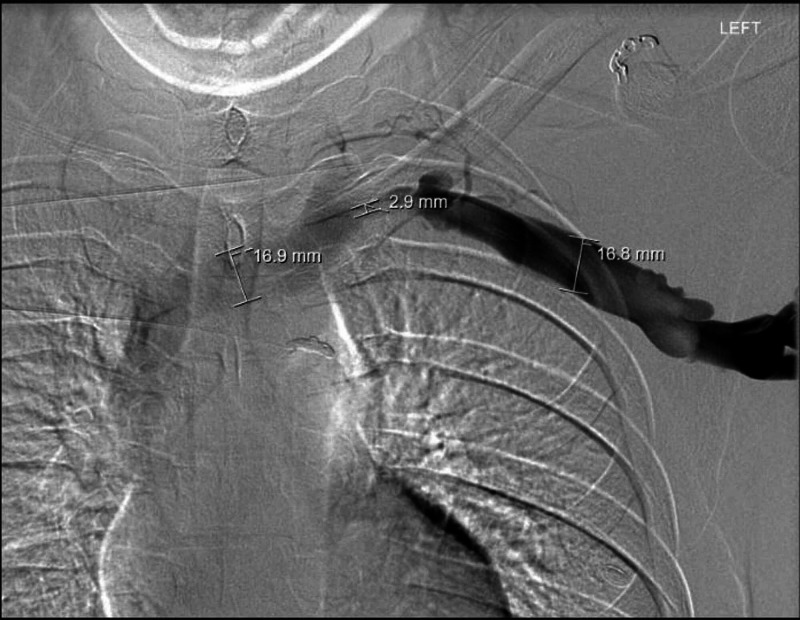
After thrombolysis, venogram showed good results without residual venous thrombosis in the left upper extremity and central veins. However, severe stenosis of the left brachiocephalic vein at the level of the sternoclavicular junction was present. This is seen in Figure 2.
Figure 2. Post-thrombolysis venogram.
Observed flow through the vein, and provided dimensions show stenosis at the area of the sternoclavicular junction.
The patient agreed to undergo first rib resection for definitive treatment, which was scheduled for a later date. He was transitioned to rivaroxaban, with plans to follow up for scheduled outpatient surgical management. Prior to discharge, the pain, swelling, and discoloration had improved. Investigation of thrombophilia was subsequently negative.
Discussion
Paget-Schroetter syndrome typically occurs in young and healthy patients who are physically active [1]. It makes up to 1%-4% of all DVTs and repetitive activity causing significant muscle hypertrophy and thoracic outlet obstruction, or other anatomical obstructions are usually associated risk factors [2].
Patients will usually present with complaints of post-workout pain, swelling, heaviness, and upper extremity discoloration [3]. Often, patients are able to relate onset of symptoms to physical activity. On inspection, these signs are apparent and it is extremely important to rule out arterial disease by physical examination and imaging studies, if uncertain. This will help prevent complications of arterial disease that could eventually lead to loss of limb when delayed.
Imaging modalities such as ultrasonography, catheter-directed venography, CT venography, and MR angiography are useful in making the diagnosis [4]. Treatment involves symptomatic management such as elevation of the extremity and pain management. Thrombolytic therapy followed by thoracic outlet decompression such as first rib resection is definitive management [5]. Prompt diagnosis and management are essential to avoid fibrosis and permanent disability [6].
Conclusions
This case describes a typical presentation of Paget-Schroetter syndrome, highlights diagnosis, clinical course, and management in a young, otherwise healthy patient. It is vital to consider this diagnosis in patients presenting with upper extremity symptoms who are clinically consistent with DVT.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Paget-Schroetter syndrome: review of pathogenesis and treatment of effort thrombosis. Alla VM, Natarajan N, Kaushik M, Warrier R, Nair CK. https://pubmed.ncbi.nlm.nih.gov/21079709/ West J Emerg Med. 2010;11:358–362. [PMC free article] [PubMed] [Google Scholar]
- 2.Upper extremity deep venous thrombosis. Kommareddy A, Zaroukian MH, Hassouna HI. Semin Thromb Hemost. 2002;28:89–99. doi: 10.1055/s-2002-20567. [DOI] [PubMed] [Google Scholar]
- 3.Paget-Schroetter syndrome: a review of effort thrombosis of the upper extremity from a sports medicine perspective. Mall NA, Van Thiel GS, Heard WM, Paletta GA, Bush-Joseph C, Bach BR Jr. Sports Health. 2013;5:353–356. doi: 10.1177/1941738112470911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paget-Schroetter syndrome: treatment of venous thrombosis and outcomes. Hangge P, Rotellini-Coltvet L, Deipolyi AR, Albadawi H, Oklu R. Cardiovasc Diagn Ther. 2017;7:0. doi: 10.21037/cdt.2017.08.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Surgery remains the most effective treatment for Paget-Schroetter syndrome: 50 years‘ experience. Urschel HC, Jr Jr, Patel AN. Ann Thorac Surg. 2008;86:254–260. doi: 10.1016/j.athoracsur.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Protocols for Paget-Schroetter syndrome and late treatment of chronic subclavian vein obstruction. Molina JE, Hunter DW, Dietz CA. Ann Thorac Surg. 2009;87:416–422. doi: 10.1016/j.athoracsur.2008.11.056. [DOI] [PubMed] [Google Scholar]