ABSTRACT
Mycetoma is an infrequent subcutaneous infection caused by true fungi (eumycetoma) or aerobic actinomycetes (actinomycetoma). We report the case of a 62-year-old man with eumycetoma involving the left foot and ankle. Skin biopsy revealed black-brown grains, and in culture, a white colony fungus grew at day 8. Molecular sequencing using ITS1-ITS4 primers identified the species as Aspergillus sydowii. The patient was treated with itraconazole 200 mg twice daily and terbinafine 250 mg daily for 8 months, with complete response and no recurrence after 2.5 years of follow-up. Aspergillus sydowii is a saprotrophic fungus that rarely causes skin or nail disease. No cases of eumycetoma caused by this agent have been previously reported. As its geographic distribution continues to expand, it may increasingly be recognized as a cause of human disease.
INTRODUCTION
Mycetoma is a chronic subcutaneous infection caused by true fungi (eumycetoma) or aerobic actinomycetes (actinomycetoma). It is considered a neglected tropical disease and, although most cases occur in the “mycetoma belt” (area 15° latitude south and 30° latitude north that includes Sudan, Mexico, Senegal, and India), sporadic autochthonous cases are reported worldwide, including the United States and Europe.1 Aspergillus sydowii is a saprotrophic and cosmopolitan fungus that causes devastating aspergillosis in coral reefs, but seldom affects humans.2 Herein, we report a case of A. sydowii eumycetoma successfully treated with systemic antifungals.
CASE PRESENTATION
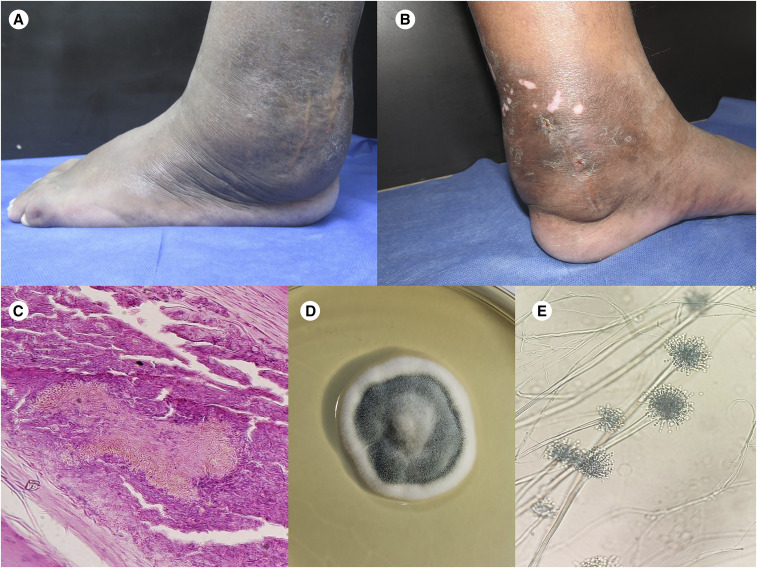
A previously healthy 62-year-old man presented to the dermatology outpatient clinic with a 14-year evolution of left foot and ankle swelling. Clinical examination revealed firm, painless swelling with foot deformity, nodules, and fistulae that drained a seropurulent discharge (Figure 1A and B). He had received previous treatment with antibiotics for years without improvement. Direct microscopic examination of the exudate did not reveal microorganisms. Histopathological examination showed granulomatous inflammation surrounding black-brown grains. Culturing of the skin biopsy in Sabouraud agar, added of chloramphenicol and cycloheximide, resulted in the isolation of a white, velvety colony with a greenish center on day 8. Microscopic examination of the colony showed septate hyphae with conidiophores ending in a vesicle with round conidia suggestive of Aspergillus spp. (Figure 1C–E). Two subsequent biopsy specimens grew a colony with the same characteristics. Molecular sequencing using ITS1-ITS4 primers identified the species as A. sydowii (100% identity; GenBank accession number MT625245). Eumycetoma caused by A. sydowii was diagnosed. Treatment with itraconazole 200 mg twice daily and terbinafine 250 mg daily combination for 8 months achieved complete resolution without recurrence after 2.5 years of follow-up. No liver function tests abnormalities or other adverse events were identified during treatment.
Figure 1.
Clinical, histopathological, and microbiological characteristics of eumycetoma by Aspergillus sydowii. (A and B) Left foot painless swelling with deformity, nodules, and fistulae that drained a seropurulent discharge. (C) Histopathological examination (hematoxylin and eosin; original magnification ×100) revealing a black-brown grain. (D) Fungal culture of the skin biopsy showing a white, velvety colony with a greenish center. (E) Microscopic examination of the colony showed septate hyphae with conidiophores ending in a vesicle with round conidia suggestive of Aspergillus spp. This figure appears in color at www.ajtmh.org.
DISCUSSION
Aspergillus spp. eumycetomas are very rare.3,4 They have infrequently been reported to cause white-grain or black-grain cases. As many Aspergillus species are ubiquitous in the environment, their geographic distribution is more widespread than other mycetoma agents that present distinctive endemicity. Aspergillus sydowii is a cosmopolitan and saprotrophic fungus that has been reported to cause disease in humans, animals, and plants. Particularly, it is responsible for aspergillosis in corals, which has caused important deterioration of coral reefs in the Caribbean Sea. Aspergillus sydowii is a terrestrial fungus, but it is also capable of surviving and reproducing in water, even with high salinity; it is considered a halophilic fungus capable of thriving in hypersaline environments.5 Dust storms may play a role in the worldwide dissemination of A. sydowii.2 Aspergillus spp. are hyalohyphomycetes that habitually produce white-grain eumycetoma.6 Exceptionally, some species have been reported to produce black mycetoma grains.3
Aspergillus sydowii is a very infrequent cause of human disease. We performed a systematic review of human infections of the skin, hair, or nails caused by A. sydowii. We searched the PubMed (Medline) database (May 25, 2020) using the keywords “A. sydowii” and screened results in English, French, or Spanish that reported human infections by A. sydowii confirmed by molecular techniques. We excluded cases that did not involve the skin, hair, or nails; that were in other languages; that only had morphological confirmation; or that did not specify the type of infection.
After screening the 159 results retrieved, 26 were evaluated for inclusion. We excluded 10 because they lacked specification of the type of infection, five because they involved infections in other sites, three because of lack of molecular species confirmation, and three because of language. We included five reports of nine patients (Table 1).7–11 The infections predominantly involved the nails.7–11 No mycetoma cases were recorded. Only one case detailed the treatment and outcome of the infection.11
Table 1.
Aspergillus sydowii infections affecting the skin, nails, or hair
| Author, country | N | Gender | Age (years) | Comorbidities | Type of infection | Site of infection | Treatment | Outcome | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| Borgohain et al.,7 India | 1 | Male | 33 | HIV infection | Onychomycosis and superficial skin infection | Right-hand thumb and widespread skin involvement | NA | NA | NA |
| Zhu et al.,8 China | 1 | Male | 58 | Onychomycosis and tinea pedis | Hyperkeratosis-like lesions | Right foot | NA | NA | NA |
| Tsang et al.,9 Hong Kong | 4 | 3 females, one male | 28, 38, 49, and 56 | 1: gouty arthritis, 1: diabetic nephropathy, hypertension, gout, hepatitis B infection | Onychomycosis | Toenails | NA | NA | NA |
| Nouripour-Sisakht et al.,10 Iran | 2 | NA | NA | NA | Onychomycosis | NA | NA | NA | NA |
| Takahata et al.,11 Japan | 1 | Female | 33 | None | Onychomycosis | Right first toenail | Surgical removal of the nail | Cure | 6 |
| Vera-Cabrera et al. (current report), Mexico | 1 | Male | 62 | None | Eumycetoma | Left foot and ankle | Terbinafine and itraconazole | Cure | 30 |
NA = not available.
In conclusion, we present a case of A. sydowii mycetoma successfully treated with systemic antifungal treatment. Aspergillus sydowii is an infrequent cause of human infection but, as its geographic distribution continue to expand, more cases may be detected in coming years.
REFERENCES
- 1.Cardenas-de la Garza JA, Welsh O, Cuellar-Barboza A, Suarez-Sanchez KP, De la Cruz-Valadez E, Cruz-Gomez LG, Gallardo-Rocha A, Ocampo-Candiani J, Vera-Cabrera L, 2020. Clinical characteristics and treatment of actinomycetoma in northeast Mexico: a case series. PLoS Negl Trop Dis 14: e0008123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hallegraeff G, Coman F, Davies C, Hayashi A, McLeod D, Slotwinski A, Whittock L, Richardson AJ, 2014. Australian dust storm associated with extensive Aspergillus sydowii fungal “bloom” in coastal waters. Appl Environ Microbiol 80: 3315–3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawatkar GU, Narang T, Shiva Prakash MR, Daroach M, Sharma M, Nahar Saikia U, Dogra S, 2017. Aspergillus: an uncommon pathogen of eumycetoma. Dermatol Ther 30: e12411. [DOI] [PubMed] [Google Scholar]
- 4.Bonifaz A, Tirado-Sanchez A, Calderon L, Saul A, Araiza J, Hernandez M, Gonzalez GM, Ponce RM, 2014. Mycetoma: experience of 482 cases in a single center in Mexico. PLoS Negl Trop Dis 8: e3102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung D, Kim H, Choi HS, 2019. Fungi in salterns. J Microbiol 58: 915–925. [DOI] [PubMed] [Google Scholar]
- 6.Estrada R, Chávez-López G, Estrada-Chávez G, López-Martínez R, Welsh O, 2012. Eumycetoma. Clin Dermatol 30: 389–396. [DOI] [PubMed] [Google Scholar]
- 7.Borgohain P, Barua P, Dutta PJ, Shaw D, Rudramurthy SM, 2019. Onychomycosis associated with superficial skin infection due to Aspergillus sydowii in an immunocompromised patient. Mycopathologia 184: 683–689. [DOI] [PubMed] [Google Scholar]
- 8.Zhu CX, Li X, Tan X, Wu G, 2019. Zombie cells, composite cells of fungal-human keratinocytes of plantar hyperkeratosis-like lesions. Mycopathologia 184: 597–605. [DOI] [PubMed] [Google Scholar]
- 9.Tsang CC, et al. 2016. Genetic diversity of Aspergillus species isolated from onychomycosis and Aspergillus hongkongensis sp. nov., with implications to antifungal susceptibility testing. Diagn Microbiol Infect Dis 84: 125–134. [DOI] [PubMed] [Google Scholar]
- 10.Nouripour-Sisakht S, Mirhendi H, Shidfar MR, Ahmadi B, Rezaei-Matehkolaei A, Geramishoar M, Zarei F, Jalalizand N, 2015. Aspergillus species as emerging causative agents of onychomycosis. J Mycol Med 25: 101–107. [DOI] [PubMed] [Google Scholar]
- 11.Takahata Y, Hiruma M, Sugita T, Muto M, 2008. A case of onychomycosis due to Aspergillus sydowii diagnosed using DNA sequence analysis. Mycoses 51: 170–173. [DOI] [PubMed] [Google Scholar]